Abstract
Background:
Higher maternal and neonatal deaths are common in low- and middle-income countries; due to less access to skilled help. Adequate knowledge and skills on maternal and newborn care (MNC) of community health workers can improve maternal and newborn health.
Aims:
To identify the knowledge of primary level health workers on some components of MNC.
Subjects and Methods:
Respondents were selected using simple random sampling method. For collecting the data, enumerators visited health institutions for 2 months from 1st October to 31st November 2012, and structured interview schedule was used to gather the information. A cross-sectional study was conducted in a total of one hundred and thirty-seven primary level health workers in Kapilvastu district, Nepal. The Chi-square test was employed to examine the association between the knowledge of health workers on MNC and designation and work experience. Data were analyzed using SPSS version 17.
Results:
In a total of 137 primary level health workers, more than half 53.2% (73/137) were senior auxiliary health workers/health assistant. Health workers having correct knowledge on contents of MNC were-registration 32.1% (44/137), major components of antenatal care 57.7% (79/137), danger signs of pregnancy 39.4% (54/137), five cleans 59.1% (81/137), postnatal health problems 54.0% (74/137), majority to health action to newborn care, newborn bath and meaning of exclusive breastfeeding. There was a statistical association between designation of health workers and above-mentioned components of MNC (P < 0.05).
Conclusions:
The differentials in the knowledge of MNC among primary level health suggest improving knowledge of the grass root level health workers with appropriate training and development programs.
Keywords: Knowledge, Maternal and newborn care, Primary level health workers
Introduction
Mostly, maternal deaths occur in developing countries and higher majority of four million annual neonatal deaths is also seen in developing countries.[1,2] The risk of maternal death as a result of pregnancy or childbirth during her lifetime is about one in six in the poorest parts of the world compared with about one in 30,000 in developed countries.[3] Globally, more than half a million newborns are estimated to die each year from serious neonatal infections, accounting for about 15% of all neonatal deaths.[2]
According to the latest report, Nepal has a higher maternal deaths of 170 per hundred thousand live births and neonatal death of 33 per thousand live births.[4] Many of these deaths could be avoided with the help of skilled care.[5] Access to quality care during pregnancy and delivery is an important factor in reducing maternal and neonatal morbidity and mortality, yet many women in low- and middle-income countries have lesser access to skilled help.[6,7] In low-income countries, about 60% of births occur without a skilled help.[8]
According to the National Health Policy 1991 of Nepal community health workers need to provide a wide range of primary health care services, both preventive and curative, including maternal, newborn, and child health interventions.[9] The high maternal and newborn mortality rates in Nepal are attributable to the scarcity of trained skilled birth attendants and paucity of resources. Improvement of health care providers with adequate knowledge and skills can serve as a tool for change. Till date, to the best of our knowledge, no research has been conducted in these matters in Nepal. With this background, the current research was conducted to assess the knowledge of maternal and newborn care (MNC) among primary level health workers of Kapilvastu district of Nepal.
Subjects and Methods
Study setting
This study was conducted in Kapilvastu district, Nepal, a Terai area with the population of 571,936 during 1st October to 31st November 2012. The study area is situated in Western Development Region of Nepal. District is the major administrative unit of Nepal. Kapilvastu district is administratively divided into 77 Village Development Committees (VDC), 16 illakas, five electoral constituencies, and one municipality. VDC is the lowest administrative unit of Nepal whereas illakas consists of 3-4 VDCs.[10] As of 2008/2009, the utilization of four antenatal care (ANC) services was only (53.26%), assistance of deliveries by health workers (31.14%), and institutional deliveries were low in the district as well as higher numbers of unnecessary deaths of children occurred in the district.[11,12]
According to the National Health Policy of Nepal 1991, each VDC has a sub-health post (SHP), health post (HP) at each illaka level, and Primary Health Care Center (PHCC) for each electoral constituency to provide primary health care services. SHP is staffed by an auxiliary health worker (AHW), a female maternal and child health worker (MCHW), and a village health worker (VHW). MCHW and VHW are recently upgraded as auxiliary nurse midwives and upgraded AHW (UAHW), respectively. AHW is the in-charge of the SHP. An HP is staffed with health assistant (HA) as in-charge, AHW, ANM, and VHW whereas medical officer (MO) is the in-charge of PHCC and other staffs under MO are HA, AHW, ANM, and staff nurse. HA and AHW are upgraded as public health inspector (PHI) after 10 years of work experience and senior auxiliary health worker (SAHW) after 5 years work experience in governmental sector, respectively. In addition, SAHW and HA have the same level of authority.[9,13]
Study design and sampling
A descriptive cross-sectional study was carried out in the primary level health workers working under the government health care delivery system; particularly PHI, SAHW/HA, AHW, and UAHW using a simple random sampling of the health institutions. A total of 137 primary level of health workers working under the government health care delivery system of the district including 7 PHI, 73 HA/SHW, 6 AHW, and 51 UAHW of various health institutions constituted the sample size of the study. Sample size was calculated using formula  , where P is taken as 0.07 (proportion of primary level health workers with adequate knowledge in prenatal and newborn care was 7.1% in a cross sectional study in Masindi, Uganda).[14] The permissible margin of error in the estimated value was taken as 5% with degree of assurance as 95% confidence level and also, assuming 10% non-response rate, we obtained 111 as the sample size. Taking all the primary level health workers available during the survey in health institutions, the total number of health workers included in this study became 137 as the final sample.
, where P is taken as 0.07 (proportion of primary level health workers with adequate knowledge in prenatal and newborn care was 7.1% in a cross sectional study in Masindi, Uganda).[14] The permissible margin of error in the estimated value was taken as 5% with degree of assurance as 95% confidence level and also, assuming 10% non-response rate, we obtained 111 as the sample size. Taking all the primary level health workers available during the survey in health institutions, the total number of health workers included in this study became 137 as the final sample.
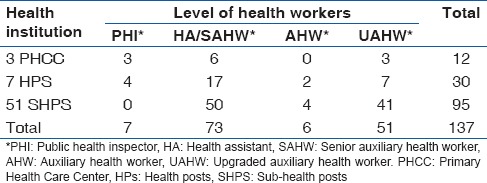
For the sampling health institutions, all the SHPs (66) of Kapilvastu were listed first. Then, 51 SHPs were selected by a simple random method using a random table. In the case of HPs and PHCCs, all the institutions in the district were included for the study. Health workers of different levels were interviewed from selected health institutions as shown in the Table 1 below.
Table 1.
Number of health workers in different level of selected health institutions in Kapilvastu District
Data collection
The face-to-face interview was conducted using structured questionnaire. The English version of the questionnaire was translated to Nepali and back translated to English to increase the reliability of the tool. The Nepali version of the questionnaire was pretested in a neighboring district named Rupandehi in the similar group of health workers to ensure cultural adaptability. The questionnaires have been adapted from maternal and neonatal health counseling package “Jeevan Suraksha” developed by U.S. Agency for International Development USAID and job description of health workers of Nepal.[13,14]
The questionnaire consisted of two parts: (i) Selected general characteristics of the respondents and (ii) knowledge on some components of registration of MNC, selected antenatal, natal, and postnatal services including newborn care. Seven medical students who were trained in interviewing and pretesting conducted the interview.
Ethics
The research proposal was approved by the Research Committee of the Sanjeevani College of Medical Sciences, Rupandehi, Nepal, and the written approval letter was obtained from District Health Office of Kapilvastu, Nepal. Health workers were provided written consent before the interview. The personal identifiers were removed before data analysis.
Definition of variables
The variables of the study were knowledge of MNC specifically; registration system of MNC, antenatal, natal, and postnatal services including newborn care, perceived problems of MNC services, designation, experience and technical education of health workers, age, sex, and marital status. Age of the respondents was coded as 20-29 years, 30-39 years, 40-49 years, and 50 and above years’ age group; sex as male and female. Marital status was coded as married and unmarried. Designation of health workers as PHI, SAHW/HA, AHW, and UAHW as mentioned job description of health workers of Nepal.[13] Technical education as HA having 3 years medical education, community medical assistants (CMAs) with 1–6 months training of medical education and UAHW with only 6th month training based on components of primary health care and total years of work experience was coded as ≤10 years and more than 10 years.
Statistical analysis
The knowledge on selected components of MNC and perceived problem in providing MNC services was expressed in frequency and percentage. In addition, all the participants were divided into two groups: PHI and SAHWs/HA, and UAHWs based on their similarity of the job description with their years of working experience to assess the differentials in the knowledge of MNC. The association between the independent variables and dependent variables was identified by using Chi-square test and also P ≤ 0.05 was considered statistically significant. Data were analyzed using Statistical Package for Social Sciences (SPSS) Statistics for Windows, Version 17.0. Chicago: SPSS Inc.
Results
The general characteristics of the respondents are presented in Table 2. Most of the respondents 91.2% (125/137) were male and married 98.5% (135/137). More than 50% 53.2% (73/137) were SAHW/HA followed by UAHW 37.2% (51/137), PHI 5.1% (7/137), and AHW 4.4% (6/137). More than half of them 57.6% (79/137) had technical education CMA, followed by VHW (38% 52/137). Only 4.4% (6/137) were HA, which level is considered as relatively more competent human resources among middle-level health workers. Majority of health workers 61.3% (84/137) were of 30-50 years of age. Most of them 85.4% (117/137) had more than 10 years of experience.
Table 2.
General characteristics of the respondents (n=137)
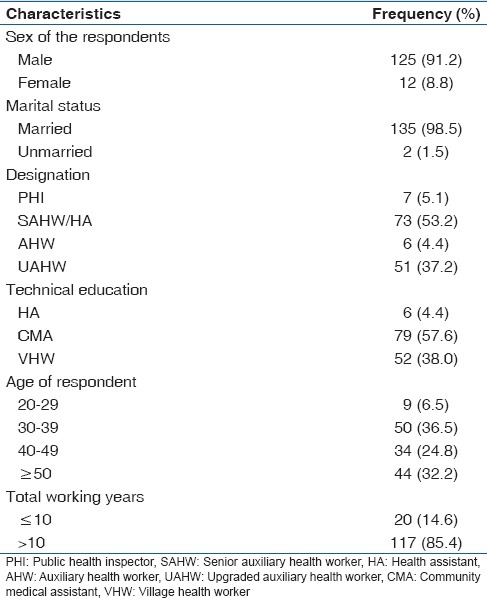
Table 3 presents the knowledge of selected components of MNC of the respondents. Few of health workers 32.1% (44/137) reported the correct number of Health Management Information System (HMIS) used in their health institution. More than half of them 57.7% (79/137) recalled the three major components of ANC. Nearly, two-fifth 39.4% (54/137) of the respondents recalled the danger signs of pregnancy. Two-fifth of the respondents 40.1% (55/137) correctly reported that extra meal is needed during pregnancy. Most of the health workers 82.5% (113/137) reported the time needed for rest and sleep during pregnancy. More than half 59.1% (81/137) of the respondents were known about the five cleans to be maintained during the intra-natal period and more than half 54.0% (74/137) recalled at least three postnatal health problems. Most 88.3% (121/137) of them correctly reported the most important health action to newborn care. Majority of them correctly reported the time for newborn bath and meaning of exclusive breastfeeding.
Table 3.
Knowledge of the respondents on selected components of maternal and newborn care (n=137)
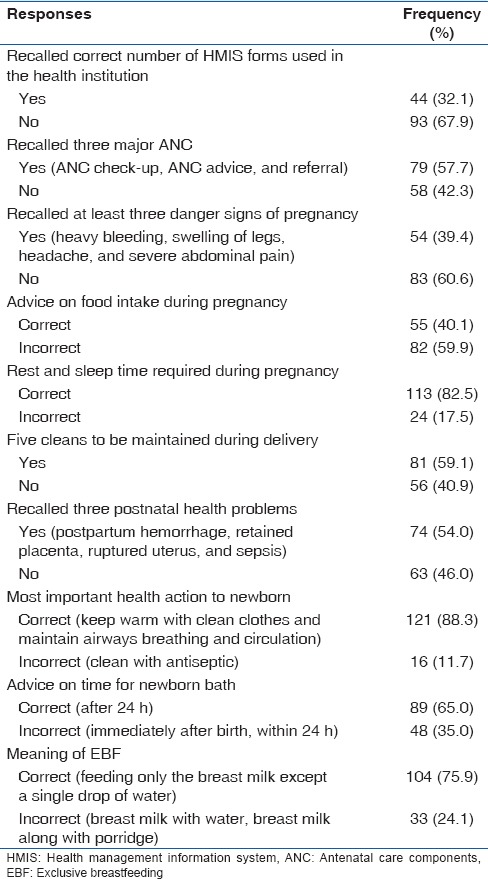
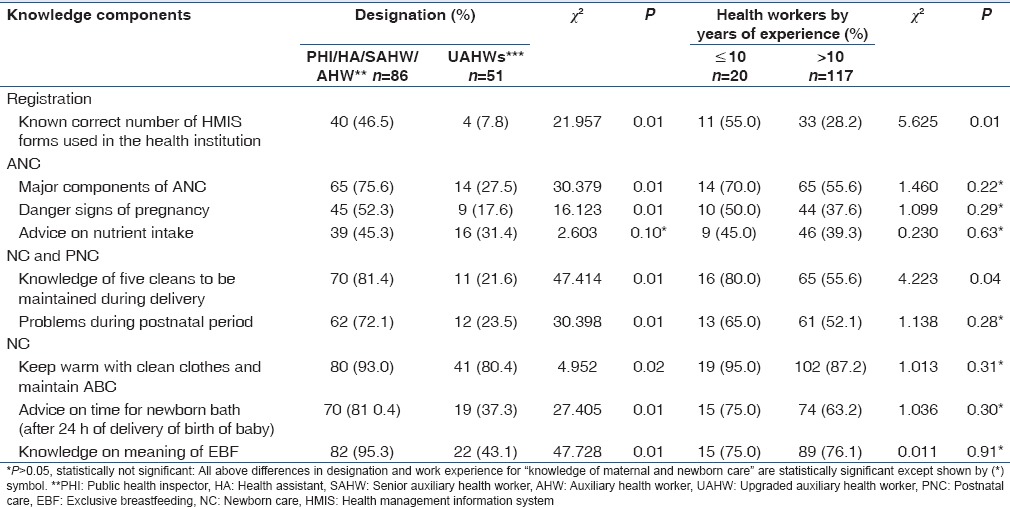
Table 4 shows differentials in the designation of paramedical staffs, their work experience, and how these differentials affect on knowledge of selected MNC components. There was statistical association between the designation of health workers and the entire knowledge components (P = 0.01). However, the designation of health worker and knowledge to the correct advice on nutrient intake during ANC was not statistically significant (P = 0.10). There was also the statistical association between the number of years of experience of health workers and some components of knowledge of MNC, particularly the number of HMIS forms used in health institution (P = 0.01) and knowledge about the five cleans to be maintained during delivery (P = 0.04).
Table 4.
Differentials in knowledge of maternal and newborn care of the respondents
Discussion
Appropriate maternal and newborn care is vital in the reduction of maternal and child morbidity and mortality. A recently published research performed in Kapilvastu district of Nepal revealed that only two-fifth of the postnatal mother attended any postnatal care (PNC) and only about 14% attended PNC within 24 h of delivery. More importantly, only 19% postnatal mothers sought PNC service from health workers in the same area. The antenatal, delivery service, and child health services in the same district were poor.[15,16] This situation of the district demands to have an insight on MNC. Knowledge of peripheral level health worker is key to change the situation. In this study, we had a total of 137 primary level health workers, in whom only 32% recalled the correct number of HMIS forms used in health institution indicating a lack of knowledge on the health management information system. The knowledge of registration to the designation and years of experience of health workers (PHI/HA/SAHW vs. UAHWs) was statistically significant. On contrary to this, a study conducted to determine the accuracy of monthly reports submitted by lady health workers of national program for family planning and primary health care in Lahore, Pakistan found that 80% had good knowledge, 15% had satisfactory knowledge, while 5% had unsatisfactory knowledge regarding data recording and reporting tools.[17] This calls for appropriate in-service and refresher training to the community health workers in particular, to the UAHWs to improve the knowledge of health workers on registration in the concerned district.
The study also revealed that more than half of the respondents could recall at least three major components of ANC but only 40% could recall at least three danger signs of pregnancy and correct advice for appropriate nutrient intake during pregnancy. However, most of the respondents reported correctly regarding total number of hours within 24 h required or rest and sleep during pregnancy. The statistical association between ANC contents, particularly recalling the major components of ANC and danger signs during pregnancy to the designation of health worker was observed. A similar Ethiopian study showed that more than half (54%) of the health extension workers had poor knowledge on contents of ANC counseling, and the majority (88%) had poor knowledge on danger symptoms, danger signs, and complications in pregnancy.[18] Primary level health worker needs coaching for improving the knowledge and skills of antenatal counseling.
Majority of the respondents reported five cleans (clean hands, clean surface, clean cord cutting instruments, clean tie, and clean stumps) to be maintained during delivery and more than half could recall at least three postnatal problems. The knowledge of both of these natal and postnatal contents by designation was statistically significant. Interestingly, an association was also found between the knowledge of five cleans to be maintained during delivery to the years of work experience of the health workers. This study differs with the cross-sectional survey conducted in Bubi district, Matabeleland North Province, Zimbabwe reported that nine of the ten nurses interviewed were not aware of a PNC policy.[19]
Knowledge of newborn care contents by designation of health workers was statistically significant but not significant by years of work experience in this study. Most of the respondents reported keeping the baby with warm clean clothes and maintain ABC is the most important health action to newborn care. Majority of them reported newborn bath to be done only after 24 h. More than three-fourth of the respondents reported the correct meaning of exclusive breastfeeding. The knowledge of newborn care in this study found higher than the study among 1358 skilled birth attendants of Nicaragua where only 44.8% professional nurses had 39.0% Auxiliary nurses had immediate newborn care knowledge.[20] Despite, several efforts with policy, strategies and programs in response to the improvement of MNC in Nepal, still need to educate and train primary level health workers to improve maternal and newborn health.[12,21,22]
This study has several strengths as it has provided much of the information about the knowledge of MNC of primary level of health workers in Kapilvastu district of Nepal which may serve as the basis for improving the knowledge of primary level health workers and this study will serve as useful baseline information for future research in the district. Although the author has collected as much information as possible in order to fulfill the research goal, the study still has some limitations. First, it is a cross-sectional study conducted in only one district; our results might not be representative of the whole country. Second, the attribution of in-service training has not been analyzed to assess the level of knowledge among health workers in the components of maternal and newborn care.
Conclusions
This study found the gap in the knowledge on maternal and newborn care among primary level health workers despite several efforts of Nepal. Inadequate knowledge on MNC among more than one-third of health workers demands interventions such as appropriate education and training and development programs to improve the health of mother and newborn in addition to existing training and developmental programs.
Financial support and sponsorship
International Fellowship Nepal, Kapilvastu Branch, Nepal.
Conflicts of interest
There are no conflicts of interest
Acknowledgments
Our special thanks goes to our research assistants and the respondents who participated in this study.
We are grateful to Dr. Nimal Kasturiaratchi, FAIRMED, Nepal, for his valuable suggestions in conducting this research and Mr. Karna Bahadur Gurung, Chief, International Nepal Fellowship, Nepal (INF), Kapilvastu for his continuous financial support during the research work as well as all the respondents who were participated in this study.
References
- 1.Hill K, Thomas K, AbouZahr C, Walker N, Say L, Inoue M, et al. Estimates of maternal mortality worldwide between 1990 and 2005: An assessment of available data. Lancet. 2007;370:1311–9. doi: 10.1016/S0140-6736(07)61572-4. [DOI] [PubMed] [Google Scholar]
- 2.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet. 2010;375:1969–87. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 3.Ronsmans C, Graham WJ. Lancet Maternal Survival Series steering group. Maternal mortality: Who, when, where, and why. Lancet. 2006;368:1189–200. doi: 10.1016/S0140-6736(06)69380-X. [DOI] [PubMed] [Google Scholar]
- 4.Annual Report 2011/2012. Kathmandu: Ministry of Health and Population Nepal, Department of Health Services; 2012. Ministry of Health and Population (MOHP) [Google Scholar]
- 5.Gabrysch S, Campbell OM. Still too far to walk: Literature review of the determinants of delivery service use. BMC Pregnancy Childbirth. 2009;9:34. doi: 10.1186/1471-2393-9-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Filippi V, Ronsmans C, Campbell OM, Graham WJ, Mills A, Borghi J, et al. Maternal health in poor countries: The broader context and a call for action. Lancet. 2006;368:1535–41. doi: 10.1016/S0140-6736(06)69384-7. [DOI] [PubMed] [Google Scholar]
- 7.Faundes A, Rosenfield A, Pinotti JA. Maternity care in developing countries: Relevance of new technological advances. Int J Gynaecol Obstet. 1988;26:349–54. doi: 10.1016/0020-7292(88)90328-1. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO) WHO Statistical Information System (WHOSIS) 2009. [Last accessed on 2014 Apr 03]. Available from: http://www.who.int/whosis/en/index.html .
- 9.National Health Policy of Nepal 1991. Kathmandu, Nepal: Ministry of Health; 1991. Ministry of Health and Population (MOHP) [Google Scholar]
- 10.District Health Office (DHO), Kapilvastu. District Health Profile of Kapilvastu District. District Health Office, Kapilvastu, Ministry of Health and Population. 2011/2012 [Google Scholar]
- 11.District Health Office (DHO), Kapilvastu. District Health Profile of Kapilvastu District. District Health Office, Kapilvastu, Ministry of Health and Population. 2009/2010 [Google Scholar]
- 12.Annual Report 2010/2011. Kathmandu: Department of Health Services and Ministry of Health and Population; 2011/2012. Department of Health Service, Population MoHa. [Google Scholar]
- 13.Ministry of Health and Population (MOHP) Department of Health Service, Kathmandu, Nepal: Job Description of Employees. Ministry of Health and Population. 1997 [Google Scholar]
- 14.Ayiasi RM, Criel B, Orach CG, Nabiwemba E, Kolsteren P. Primary healthcare worker knowledge related to prenatal and immediate newborn care: a cross sectional study in Masindi, Uganda. BMC health services research. 2014;14:1. doi: 10.1186/1472-6963-14-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khanal S, Sharma J, GC VS, Dawson P, Houston R, Khadka N, et al. Community health workers can identify and manage possible infections in neonates and young infants: MINI - A model from Nepal. J Health Popul Nutr. 2011;29:255–64. doi: 10.3329/jhpn.v29i3.7873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paudel M, Khanal V, Acharya B, Adhikari M. Determinants of postnatal service utilization in a Western District of Nepal: Community based cross sectional study. J Women's Health Care. 2013;2:126. [Google Scholar]
- 17.Mahmood S, Ayub M. Accuracy of primary health care statistics reported by community based lady health workers in district Lahore. J Pak Med Assoc. 2010;60:649–53. [PubMed] [Google Scholar]
- 18.Medhanyie A, Spigt M, Dinant G, Blanco R. Knowledge and performance of the Ethiopian health extension workers on antenatal and delivery care: A cross-sectional study. Hum Resour Health. 2012;10:44. doi: 10.1186/1478-4491-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sibanda JQ, Saungweme I, Nleya C, Mutyambizi MP, Rutgers RA. Post natal care in Bubi district deserves more attention. Cent Afr J Med. 2001;47:103–8. [PubMed] [Google Scholar]
- 20.Harvey SA, Blandón YC, McCaw-Binns A, Sandino I, Urbina L, Rodríguez C, et al. Are skilled birth attendants really skilled. A measurement method, some disturbing results and a potential way forward? Bull World Health Organ. 2007;85:783–90. doi: 10.2471/BLT.06.038455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Planning Commission. Nepal Millennium Development Goals: Progress Report 2005. National Planning Commission and United Nations Development rogramme, Kathmandu, Nepal. 2005 [Google Scholar]
- 22.National Planning Commission, Three Year Interim Plan 2013-2016, Government of Nepal, Kathmandu. 2007 [Google Scholar]


