Abstract
Persistent left superior vena cava (PLSVC) with absence of right SVC (isolated PLSVC) is a rare congenital anomaly that occurs as a result of a degenerative condition in the left anterior cardinal vein. It is generally an incidental finding while performing invasive procedures such as antiarrhythmic device implantation. We report on a rare case of permanent pacemaker implantation in a patient with this anomaly from right subclavian route, albeit most of the earlier reported cases are from left subclavian approach. A wide spectrum of clinicians should be aware of this anomaly, its variations, and possible complications.
Keywords: Device implantation, pacemaker, persistent left superior vena cava
INTRODUCTION
Persistent left superior vena cava (PLSVC) is a structural, asymptomatic, and infrequent anomaly, present in 0.3% of the general population and in 4.3% of congenital heart disease.[1] Typically, the diagnosis reveals itself unexpectedly at the time of device implantations. Isolated PLSVC (PLSVC with absent right SVC [RSVC]) is usually asymptomatic, but it can pose difficulties with central venous access, device implantation, and cardiothoracic surgery. This condition is also associated with an increased incidence of congenital heart disease, arrhythmias, and conduction disturbances. Successful implantation of a permanent pacemaker from right subclavian route was done in a 70-year-old male patient with isolated PLSVC.
CASE REPORT
A 70-year-old male was admitted in our institution with a complaint of recurrent syncope for 10 days duration. A 12-lead electrocardiography revealed complete heart block (CHB). The probable etiology of CHB was kept as degenerative, after ruling out reversible causes. Temporary pacemaker lead was inserted uneventfully by femoral route. As per the government's funding scheme, the only option for permanent pacemaker implantation was single chamber VVI. Due to large experience of our institution, right subclavian approach was used. After puncture of right subclavian vein, it was impossible to advance a guidewire into the normal expected course of SVC, under fluoroscopy, the wire always being seen to coil in the left subclavian vein (LSCV) and guidewire to pass through left-sided SVC. A 9-French pacemaker sheath was inserted by modified Seldinger technique. On lead insertion, circuitous course of the lead via left mediastinum (PLSVC), instead of the expected right side, was noted [Figure 1]. Right upper limb venography from right antecubital vein demonstrated contrast from right subclavian vein via the bridging vein into the left-sided SVC and absence of the RSVC [Figure 1]. Passive fixation pacemaker lead could be successfully placed with acceptable parameters (threshold 0.6V, impedance 560Ω). Fluoroscopic anteroposterior view showed the characteristic alpha configuration [Figure 2]. Transthoracic echocardiography revealed dilated coronary sinus (CS) and agitated saline injected from both right and left arm that showed opacification of CS before right atrium (RA) [Figure 3]. Multiple detector computed tomography (MDCT) and CT venography showed a bridging vein draining the right jugular and right subclavian veins into PLSVC, which descended at the left side of the mediastinum and left atrium before draining into the RA via a dilated CS [Figures 4 and 5]. The RSVC was absent. At 3-month follow-up, the patient was asymptomatic with acceptable lead parameters at pacemaker interrogation and fluoroscopically appropriate lead position.
Figure 1.
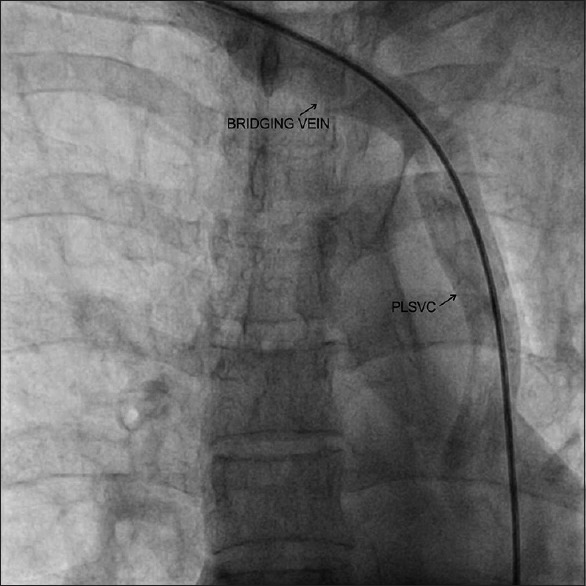
Right upper limb venography showing absence of right superior vena cava and drainage of right subclavian vein into left superior vena cava via bridging vein
Figure 2.
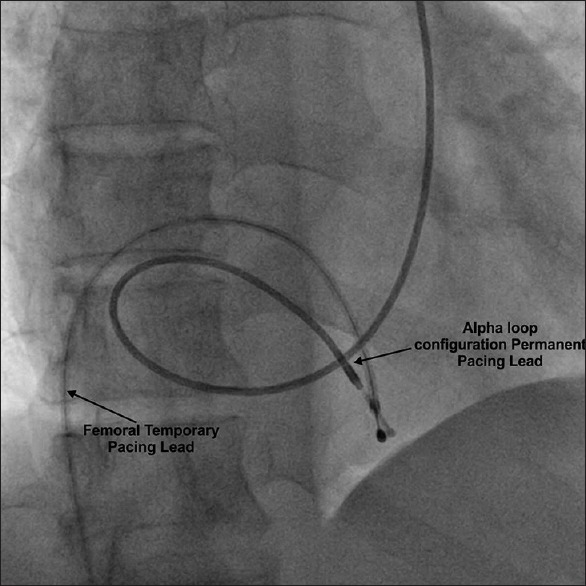
Passive fixation of permanent pacemaker lead at right ventricle apex with alpha loop configuration
Figure 3.
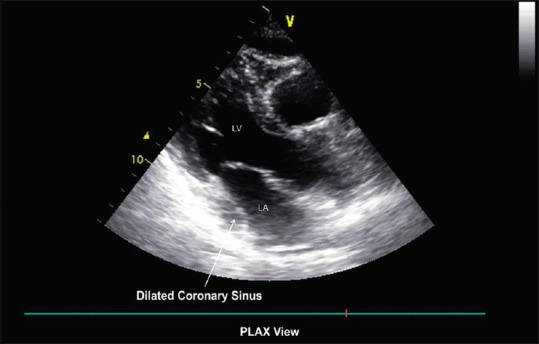
Transthoracic echocardiography in parasternal long-axis view demonstrating dilated coronary sinus
Figure 4.
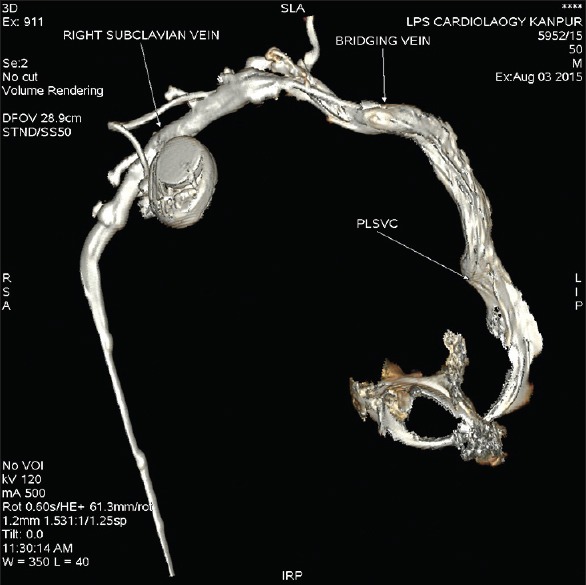
Computed tomography venography showing absence of right superior vena cava and drainage of right subclavian vein into left superior vena cava via bridging vein
Figure 5.

Computed tomography venography showing absence of right superior vena cava and drainage of right subclavian vein into left superior vena cava via bridging vein
DISCUSSION
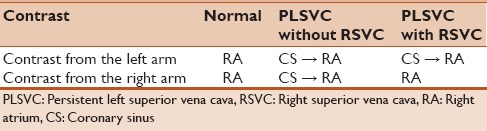
PLSVC is a structural, asymptomatic, and infrequent anomaly, present in 0.3% of the general population and in 4.3% of congenital heart disease.[1] PLSVC with absence of RSVC occurs in only 10–20% cases of PLSVC. In most patients with left SVC, RSVC is present which is called bilateral SVC or double venous system and drains into RA via a dilated CS. During normal fetal development, the left-sided anterior venous cardinal system regresses, leaving the CS and the ligament of Marshall. Failure of the closure of the left anterior cardinal vein results in PLSVC.[2] It is a rare anomaly with only a handful of cases reported to date. The first case of PLSVC with absence of RSVC was reported in 1862. Either isolated or associated with RSVC, this venous malformation itself causes no hemodynamic disturbance and is usually diagnosed incidentally.[3,4,5] However, it has several clinical implications. A PLSVC can cause problems during pacemaker implantation such as difficulty in obtaining a stable lead position and sustained capture due to the circuitous route of the pacemaker lead.[6] Therefore, long lead lengths are needed to reach right ventricle due to circuitous course of the ventricular lead. The complete anomaly is encountered via right subclavian approach; as by left subclavian approach, it is only possible to suspect PLSVC. When compared to double venous system, it is much easier to cross the tricuspid valve level in isolated PLSVC because there is no right-sided vena cava entering the RA as a second “exit” for the lead. Echocardiography will reveal a dilated CS and finding as described in Table 1.[7,8] However, it is the contrast echocardiography which will diagnose whether RSVC is present or not.
Table 1.
Echocardiographic diagnosis of persistent left superior vena cava and its possible variation with contrast application
CT (MDCT and venography) will confirm the diagnosis.[5] Finally, a wide spectrum of clinicians (interventional cardiologists, radiologists, intensivists, anesthesiologists, and cardiothoracic surgeons) should be aware of PLSVC and its variations to avoid possible complications. In cases of isolated PLSVC, if the right subclavian approach fails, then options which remain viable are the following:
LSCV approach: Advantage of this approach being avoidance of long lead length due to less circuitous route and thereby conferring a stable lead position
Inferior vena cava (IVC) approach: This approach is preferred in cases where there is a loss of SVC and RA continuity, for example, post-Glenn shunt in single ventricle. The site of implantation of pulse generator is in the anterior abdominal wall
Transcatheter pacing system (leadless pacemaker): Micra transcatheter pacemaker is a fully self-contained, miniaturized pacemaker delivered via catheter through the IVC and positioned inside the right ventricle. It obviates the surgical pocket under the skin for pulse generator
Epicardial pacemaker: This approach is typically used in infants and children with complex congenital heart disease and complicated anatomy. In addition, this approach has applicability in older people, particularly if they are undergoing cardiac surgeries in view of postarrhythmias. In cases where right ventricular endocardial pacing is not feasible like patient with tricuspid mechanical valve prosthesis, epicardial pacing offers an alternative.
CONCLUSION
Isolated PLSVC is a rare congenital anomaly, usually diagnosed incidentally, and a wide variety of operators must be aware of this venous anomaly that may technically complicate the procedures. An interventional cardiologist must keep in this mind, this rare anomaly which comes across while implanting intra-cardiac devices from right subclavian approach and must know the technical difficulties and measures to escape from them.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Guray Y, Yelgec NS, Guray U, Yylmaz MB, Boyaci A, Korkmaz S. Left-sided or transposed inferior vena cava ascending as hemiazygos vein and draining into the coronary sinus via persistent left superior vena cava: Case report. Int J Cardiol. 2004;93:293–5. doi: 10.1016/S0167-5273(03)00154-2. [DOI] [PubMed] [Google Scholar]
- 2.Nsah EN, Moore GW, Hutchins GM. Pathogenesis of persistent left superior vena cava with a coronary sinus connection. Pediatr Pathol. 1991;11:261–9. doi: 10.3109/15513819109064763. [DOI] [PubMed] [Google Scholar]
- 3.Shyamkumar NK, Brown R. Double superior vena cava with a persistent left superior vena cava: An incidental finding during peripherally inserted central catheter placement. Australas Radiol. 2007;51(Suppl (4)):B257–9. doi: 10.1111/j.1440-1673.2007.01796.x. [DOI] [PubMed] [Google Scholar]
- 4.Antretter H, Cottogni M, Oberhauser A, Lhotta K, Furtwängler W. Pacemaker implantation via a persistent left superior vena cava in atresia of the true superior vena cava. Dtsch Med Wochenschr. 1992;117:1394–8. doi: 10.1055/s-2008-1062456. [DOI] [PubMed] [Google Scholar]
- 5.Heye T, Wengenroth M, Schipp A, Johannes Dengler T, Grenacher L, Werner Kauffmann G. Persistent left superior vena cava with absent right superior vena cava: Morphological CT features and clinical implications. Int J Cardiol. 2007;116:e103–5. doi: 10.1016/j.ijcard.2006.08.067. [DOI] [PubMed] [Google Scholar]
- 6.Recupero A, Pugliatti P, Rizzo F, Carerj S, Cavalli G, de Gregorio C, et al. Persistent left-sided superior vena cava: Integrated noninvasive diagnosis. Echocardiography. 2007;24:982–6. doi: 10.1111/j.1540-8175.2007.00509.x. [DOI] [PubMed] [Google Scholar]
- 7.Chan KL, Abdulla A. Images in cardiology. Giant coronary sinus and absent right superior vena cava. Heart. 2000;83:704. doi: 10.1136/heart.83.6.704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uçar O, Pasaoglu L, Ciçekçioglu H, Vural M, Kocaoglu I, Aydogdu S. Persistent left superior vena cava with absent right superior vena cava: A case report and review of the literature. Cardiovasc J Afr. 2010;21:164–6. [PMC free article] [PubMed] [Google Scholar]


