Abstract
The incidence of epidermoid tumors is between 1% and 2% of all intracranial tumors. The usual locations of epidermoid tumor are the parasellar region and cerebellopontine angle, and it is less commonly located in sylvian fissure, suprasellar region, cerebral and cerebellar hemispheres, and lateral and fourth ventricles. Epidermoid cysts located in the posterior fossa usually arise in the lateral subarachnoid cisterns, and those located in the brain stem are rare. These epidermoids contain cheesy and flaky white soft putty like contents. Epidermoid cysts are very slow growing tumors having a similar growth pattern of the epidermal cells of the skin and develop from remnants of epidermal elements during closure of the neural groove and disjunction of the surface ectoderm with neural ectoderm between the third and fifth weeks of embryonic life. We are presenting an interesting case of intrinsic brainstem epidermoid cyst containing milky white liquefied material with flakes in a 5-year-old girl. Diffusion-weighted imaging is definitive for the diagnosis. Ideal treatment of choice is removal of cystic components with complete resection of capsule. Although radical resection will prevent recurrence, in view of very thin firmly adherent capsule to brainstem, it is not always possible to do complete resection of capsule without any neurological deficits.
Keywords: Brainstem, dermoid, diffusion-weighted imaging, epidermoid, epidermoid cyst, intrinsic, pons
Introduction
Epidermoids are very slow growing congenital tumors, and were initially described by French pathologist Cruveilhier as the “most beautiful tumors of all the tumors” based on their pearly nature.[1] The incidence of epidermoid tumors is between 1% to 2% of all intracranial tumors.[2,3,4,5,6,7] The usual locations of epidermoid tumor are parasellar region and cerebellopontine angle[7,8,9,10,11] and is less commonly located in sylvian fissure, suprasellar region, cerebral[12,13,14] and cerebellar hemispheres,[12,14,15] and lateral and fourth ventricles.[7,12,14,15,16,17,18] Epidermoid cysts located in the posterior fossa usually arise in the lateral subarachnoid cisterns,[9,14,19] and those located in the brain stem are rare.[2,5,19,20,21,22] As far as our literature search, there were only 22 cases of epidermoid tumors reported[5,13,19,20,21,22,23,24,25,26,27,28,30,31,32,33,34,35,36] Growth rate of epidermoid tumors was similar to epidermal cells of the skin and they grow along the cisternal spaces with very few exceptions of infiltrating the surrounding parenchyma of brain.[37] These epidermoids contain cheesy and flaky white soft putty like contents. We are presenting an interesting case of an intrinsic brainstem epidermoid cyst containing milky white liquefied material with flakes in a 5-year-old girl. The presentation, radiological imaging, differential diagnosis, and surgical management are discussed, along with a review of the reported cases in the literature.
Case Example
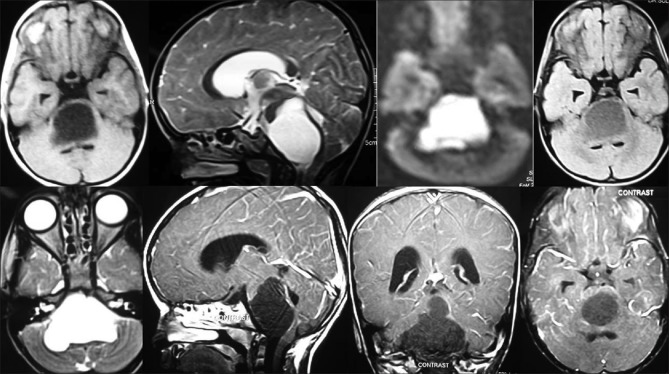
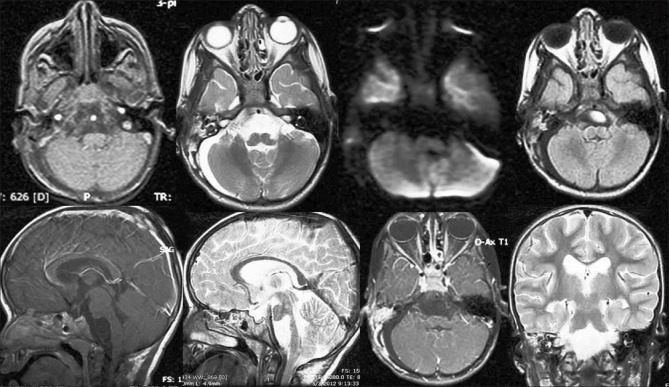
A 5-year-old girl was admitted to our services with insidious onset gradually progressive headache, mild low grade fever on and off for 1 year along with difficulty in swallowing for 1 month. She was fully conscious; alert and oriented, fundi were normal, have lower cranial nerve deficits with impaired gag. Her gait was typically ataxic. Laboratory investigations were within normal limits. Magnetic resonance (MR) imaging showed a well-defined, intra-axial mass lesion in pons and medulla, measuring 40 × 35 × 40 mm in diameter with signal intensities hypointense on T1-weighted images, iso-intense to CSF on T2-weighted images, hyperintense with uniform restriction on diffusion-weighted images, and no enhancement on gadolinium administration with hydrocephalus [Figure 1]. The MRI showed thinned out brainstem around the cystic lesion. The patient was operated with initial presumptive diagnosis of the epidermoid based on imaging. A left retromastoid retrosigmoid/suboccipital craniotomy and microsurgical aspiration of the cystic lesion with excision of the tumor capsule were done. Shortly following cerebellar retraction, a thinned out bulging pontomedullary region was noted. The whole lesion is intrinsic to the brainstem without any extra-axial or exophytic component. Upon myelotomy at the most thinned part of the brainstem, white-milky fluid with flakes drained from the lesion cavity. Microsurgical subtotal excision of the tumor capsule with drainage of the all the contents was done. Small bits of tumor capsule densely adherent to the brainstem were left behind. At the end, the cavity was irrigated with a hydrocortisone solution with Ringer lactate to prevent aseptic meningitis. The postoperative course was uneventful with immediate improvement of all the symptoms and normalization of the lower cranial nerves. Histopathological examination of tumor tissue was compatible with the epidermoid cyst. Postoperative MRI scans revealed complete excision of the tumor [Figure 2]. The patient was discharged on the 10th postoperative day. On follow up at 11 months, she was doing well and the repeat MRI showed small recurrence of the lesion [Figure 3].
Figure 1.
T1 hypointense, T2 FLAIR hyperintense, restriction on diffusion-weighted image with no enhancement on contrast in the region of brainstem suggestive of brainstem epidermoid cyst
Figure 2.
Post-operative image showing the complete absence of restriction in diffusion-weighted imaging along with completion of aspiration of the contents
Figure 3.
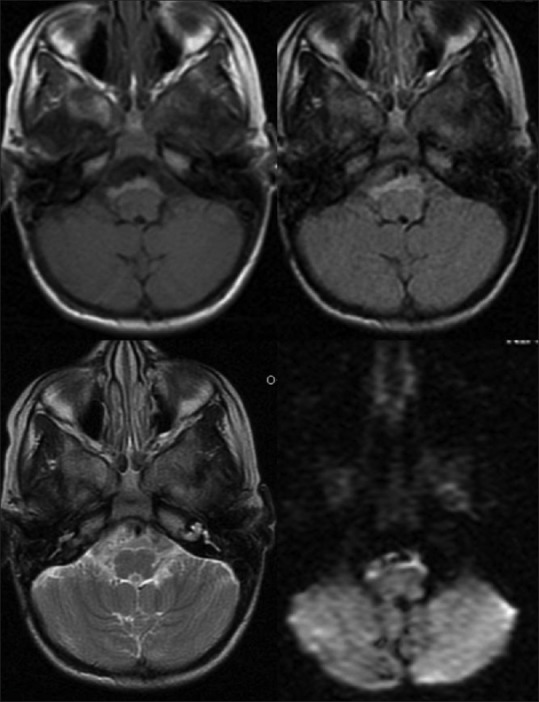
Post-operative image showing small recurrence with restriction in diffusion-weighted imaging
Discussion
Epidermoid cysts are very slow growing tumors with a similar growth pattern to the epidermal cells of the skin and develop from remnants of epidermal elements during closure of the neural groove and disjunction of the surface ectoderm with neural ectoderm between the third and fifth weeks of embryonic life.[9,14,37,38,39,40,41] Most of the epidermoids cysts have lateral preference in extra-axial space due to proliferation of transplanted epithelial cell remnants moved with migration of otic vesicles or developing neurovasculature;[14,16] few of the intrinsic intra-axial median located epidermoid tumors occur with separation of neuroectoderm from the cutaneous counterpart. Those located in the brainstem occur very rarely, and purely intrinsic lesions without exophytic extensions have been reported previously in six cases only [Table 1].[20,22,29,31,32,33] The epidermoid cyst consists of an outer capsule, an epithelial layer, and, in some cases, an inner cystic fluid.[9,40] Enlargement of the tumor is mainly attributed to accumulation of breakdown products of desquamated epithelial cells which leads to Keratin and cholesterol accumulation in the subarachnoid space and give the milky-white or pearly appearance.[14,39,40] This characteristic pearly appearance was lost when the epidermoid gets infected and the cyst contents become liquefies.[42] The other theory that may cause the liquefaction of the cyst contents was due to loss of vascularity.[42] Previously, only Caldarelli et al. and Ziyal et al. reported that the cyst content was a milky fluid at the surgery.[2,42]
Table 1.
List of reported Brainstem epidermoid cysts in the literature till date
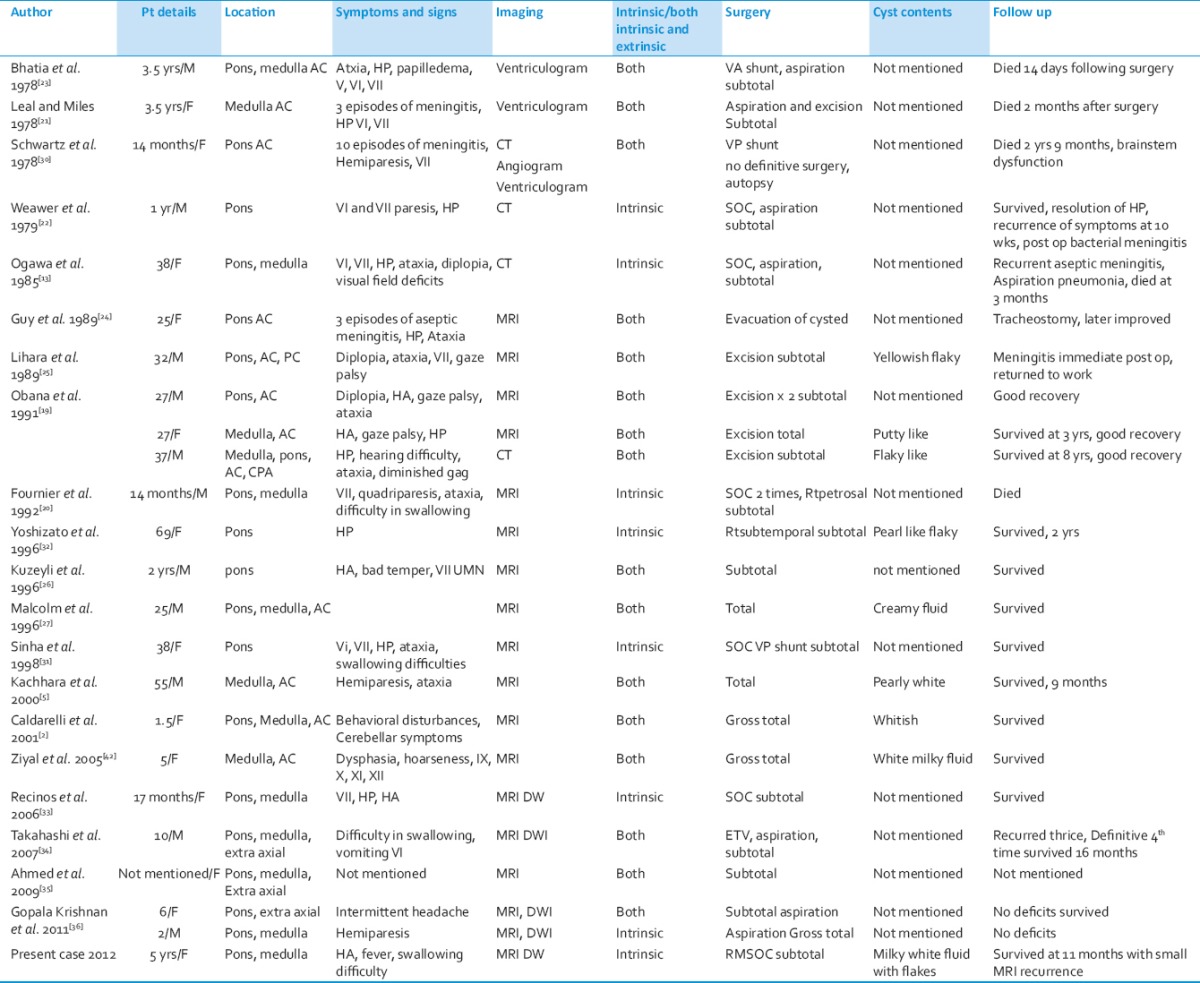
Epidermoids are commonly symptomatic during the adulthood and present during the 4th decade[7] and very few were presented during childhood due to their slow nature of the growth.[2,20,21,22,23,26,30] We divided the tumors into two groups based on whether they are purely intrinsic or have an extra axial component along with intrinsic part. Even though there is no difference in the mean age at presentation between the intrinsic and intrinsic with extra axial lesions, median age at presentation is less compared to the intrinsic with extra axial lesions.[33] Epidermoids usually cause symptoms by compression of the surrounding neural structures and symptomatology depends on the location of the cyst. Among the 20 reported cases, the most common signs included hemiparesis, seventh cranial nerve palsy, sixth cranial nerve palsy, and gait ataxia. Other notable signs included aseptic meningitis and increased intracranial pressure. Recurrent episodes of aseptic meningitis are due to rupture or leakage of cyst contents spontaneously.[21,24,27,30] Even though the tumors are very large in size, they present with minimal clinical symptoms and signs due to the slow growth of the tumor along with the plasticity of the neural architecture, although there may be severe radiological compression of important neural structures like in our patient. Although drainage of epidermoid cyst fluid into the subarachnoid space has been shown to produce aseptic meningitis, no sign of meningeal irritation was noted in this case.
On computed tomography (CT) scan, the tumor appears hypodense or isodense or sometimes spontaneous hyperdense due to protein, lipid, calcium, and hemosiderin content[43] along with occasional calcification (more in dermoids). MRI scan is the modality of choice for the diagnosis. The lesion is hypointense on T1-weighted, hyperintense on T2-weighted, FLAIR with hyperintense restriction on diffusion-weighted imaging (DWI)[2] without any contrast enhancement.[5,44,45] If contrast enhancement occurs, it is usually at the margins of the tumor.[14] In intrinsic lesions, the absence of the tumor edema distinguishes from the gliomas. In extrinsic locations, DWI is useful to differentiate from the arachnoid cyst and abscess.[46,47] DWI is useful to know the remnant by its restriction, differentiation from abscess, and arachnoid cyst.[33]
During the natural course, the epidermoid cyst spontaneously regresses due to rupture into arachnoid cyst with waning of the symptoms, over a period of time the symptoms will recur due to the development of the aseptic meningitis. Ideal treatment of choice is removal of cystic components with complete resection of capsule.[6,24,40] These tumors should be removed with the aim of radical resection without compromising the patient's neurological condition. Although the cyst content can be aspirated easily,[28] radical removal of the total tumor is not always possible because capsule is usually adherent to surrounding neurovascular structures.[2,13,19,20,22,25,26,30] Treatment of intrinsic brain stem epidermoid cysts consists of simple aspiration or subtotal excision of the tumor may be performed due to adherence of the tumor capsule to the surrounding vital brainstem tissue. An aggressive approach leads to disastrous complications.[12,21] Avoidance of aseptic meningitis in the post-operative period can be done with prevention of the spillage of cyst components into the surrounding subarachnoid space, which was encountered in 2% to 50% in previously reported cases.[2,4,7,11,13,22,25,30,48,49,50] Perioperative administration of steroid agents with copious irrigation with hydrocortisone has been shown to help prevent aseptic meningitis.[7,9,11,14,31,49,51] Of all reported 20 cases of brain stem epidermoid cysts in the literature, 6 patients died due to the postoperative progressive deterioration.[5,13,20,21,23,30] Good long-term outcomes with minor morbidity have been achieved with a more conservative approach to difficult cases.[19] Although radical resection will prevent recurrence, in view of very thin firmly adherent capsule to brainstem, it is not always possible to do complete resection capsule without any neurological deficits.
Tancredi et al. reported that prognosis does not influenced by type of excision or preoperative tumor size.[7] The recurrence rate is between 1% and 54% and may be avoided to devitalize the remnant of capsule fragments during the operation.[9,11,14,29,49,51] Reoperation should be performed when the patient becomes symptomatic again, because no dissection plane between the capsule and the arachnoid during the second operation. The reoperation is usually performed for decompression. Malignant degeneration was reported for recurrent epidermoid tumors.[10,40,49,52,53]
Conclusion
Epidermoid cysts located in the posterior fossa usually arise in the lateral subarachnoid cisterns, and those located in the brain stem are rare. Epidermoid cysts are very slow growing tumors with a similar growth pattern of the epidermal cells of the skin and develop from remnants of epidermal elements during closure of the neural groove and disjunction of the surface ectoderm with neural ectoderm between the third and fifth weeks of embryonic life. Diffusion-weighted imaging is definitive for the diagnosis. Ideal treatment of choice is removal of cystic components with complete resection of capsule. Although radical resection will prevent recurrence, in view of very thin firmly adherent capsule to brainstem, it is not always possible to do complete resection of capsule without any neurological deficits. As the capsule is firmly adherent to the brainstem, second surgery for recurrence is only for decompression to relieve symptoms.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Cruveilhier J. Paris: Baillere; 1829. Anatomie pathologique du corps humain. Vol 1, book 2. [Google Scholar]
- 2.Caldarelli M, Colosimo C, Di Rocco C. Intra-axial dermoid/epidermoid tumors of the brainstem in children. Surg Neurol. 2001;56:97–105. doi: 10.1016/s0090-3019(01)00542-0. [DOI] [PubMed] [Google Scholar]
- 3.Caldarelli M, Massimi L, Kondageski C, Di Rocco C. Intracranial midline dermoid and epidermoid cysts in children. J Neurosurg. 2004;100:473–80. doi: 10.3171/ped.2004.100.5.0473. [DOI] [PubMed] [Google Scholar]
- 4.Guidetti B, Gagliardi FM. Epidermoid and dermoid cysts: Clinical evaluation and late surgical results. J Neurosurg. 1977;47:12–8. doi: 10.3171/jns.1977.47.1.0012. [DOI] [PubMed] [Google Scholar]
- 5.Kachhara R, Bhattacharya RN, Radhakrishnan VV. Epidermoid cyst involving the brain stem. Acta Neurochir (Wien) 2000;142:97–100. doi: 10.1007/s007010050013. [DOI] [PubMed] [Google Scholar]
- 6.Rubin G, Scienza R, Pasqualin A, Rotsa L, Da Pian R. Craniocerebral epidermoids and dermoids. Acta Neurochir (Wien) 1989;97:1–16. doi: 10.1007/BF01577734. [DOI] [PubMed] [Google Scholar]
- 7.Tancredi A, Fiume D, Gazzeri G. Epidermoid cysts of the fourth ventricle: Very long follow up in 9 cases and review of the literature. Acta Neurochir (Wien) 2003;145:905–11. doi: 10.1007/s00701-003-0008-3. [DOI] [PubMed] [Google Scholar]
- 8.Altschuler EM, Jungreis CA, Sekhar LN, Jannetta PJ, Sheptak PE. Operative treatment of intracranial epidermoid cysts and chlosterol granulomas: Report of 21 cases. Neurosurgery. 1990;26:606–4. doi: 10.1097/00006123-199004000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Berger MS, Wilson CB. Epidermoid cysts of the posterior fossa. J Neurosurg. 1985;62:214–9. doi: 10.3171/jns.1985.62.2.0214. [DOI] [PubMed] [Google Scholar]
- 10.Netsky MG. Epidermoid tumors. Review of the literature. Surg Neurol. 1988;29:477–83. doi: 10.1016/0090-3019(88)90144-9. [DOI] [PubMed] [Google Scholar]
- 11.Yamakawa K, Shitara N, Genka N, Kanaka S, Takakura K. Clinical course and surgical prognosis of 33 cases of intracranial epidermoid tumors. Neurosurgery. 1989;24:568–73. doi: 10.1227/00006123-198904000-00013. [DOI] [PubMed] [Google Scholar]
- 12.Grant FC, Austin GM. Epidermoids: Clinical evaluation and surgical results. J Neurosurg. 1950;7:190–8. doi: 10.3171/jns.1950.7.3.0190. [DOI] [PubMed] [Google Scholar]
- 13.Ogawa T, Sekino H, Fuse T, Nakamura N. Multiple intracranial epidermoids located in the brain stem and the middle cranial fossa: Case report. Neurol Med Chir (Tokyo) 1985;25:393–7. doi: 10.2176/nmc.25.393. [DOI] [PubMed] [Google Scholar]
- 14.Yasargil MG, Abernathey CD, Sarioglu AÇ. Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989;24:561–7. doi: 10.1227/00006123-198904000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Sabin HI, Bordi LT, Symon L. Epidermoid cysts and cholesterol granulomas centered on the posterior fossa: 20 years of diagnosis and management. Neurosurgery. 1987;21:789–805. doi: 10.1227/00006123-198712000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Eekhof JL, Thomeer RT, Bots GT. Epidermoid tumor in the lateral ventricle. Surg Neuro l. 1985;23:189–92. doi: 10.1016/0090-3019(85)90344-1. [DOI] [PubMed] [Google Scholar]
- 17.Fiume D, Gazzeri G, Spallone A, Santucci N. Epidermoid cysts of the fourth ventricle. Surg Neurol. 1988;29:178–82. doi: 10.1016/0090-3019(88)90002-x. [DOI] [PubMed] [Google Scholar]
- 18.Yamaki T, Takeda M, Takayama H, Nakagaki Y. Double intracranial tumours of mal developmental originteratoma at the pineal region and an epidermoid cyst in the fourth ventricle. Neurochirurgia (Stuttg) 1990;33:88–90. doi: 10.1055/s-2008-1053563. [DOI] [PubMed] [Google Scholar]
- 19.Obana WG, Wilson CB. Epidermoid cyst of the brain stem. Report of three cases. J Neurosurg. 1991;74:123–8. doi: 10.3171/jns.1991.74.1.0123. [DOI] [PubMed] [Google Scholar]
- 20.Fournier D, Mercier P, Menei P, Pouplard F, Rizk T, Guy G. Recurrent intrinsic brain stem epidermoid cyst. Childs Nerv Syst. 1992;8:471–4. doi: 10.1007/BF00274412. [DOI] [PubMed] [Google Scholar]
- 21.Leal O, Miles J. Epidermoid cyst in the brain stem. Case report. J Neurosurg. 1978;48:811–3. doi: 10.3171/jns.1978.48.5.0811. [DOI] [PubMed] [Google Scholar]
- 22.Weawer EN, Jr, Coulon RA., Jr Excision of a brain stem epidermoid cyst. Case report. J Neurosurg. 1979;51:254–7. doi: 10.3171/jns.1979.51.2.0254. [DOI] [PubMed] [Google Scholar]
- 23.Bhatia R, Shankar SK, Tandon PN. Pre-pontineepidermoid traversing the brain stem: A case report. Neurol India. 1978;26:76–8. [PubMed] [Google Scholar]
- 24.Guy G, Jan M, Guegan Y. Leslesionschirurgicales du tronc cerebral. Neuochiurgie. 1989;35(Suppl 1):99–101. [Google Scholar]
- 25.Iihara K, Kikuchi H, Ishikawa M, Nagasawa S. Epidermoid cyst traversing the pons into the fourth ventricle. Case report. Surg Neurol. 1989;32:377–81. doi: 10.1016/0090-3019(89)90143-2. [DOI] [PubMed] [Google Scholar]
- 26.Kuzeyli K, Duru S, Cakir E, Pekince A, Ceylan S, Aktürk F. Epidermoid cyst of the brain stem. Case report. Neurosurg Rev. 1996;19:179–81. doi: 10.1007/BF00512049. [DOI] [PubMed] [Google Scholar]
- 27.Malcolm GP, Gibson R, Ironside JW, Whittle IR. Microsurgical excision of a pontomedullary epidermoid cyst with prepontine extension. Case report. Neurosurgery. 1996;38:579–83. doi: 10.1097/00006123-199603000-00032. [DOI] [PubMed] [Google Scholar]
- 28.Netsky MG. Epidermoid tumors. Review of the literature. Surg Neurol. 1988;29:477–83. doi: 10.1016/0090-3019(88)90144-9. [DOI] [PubMed] [Google Scholar]
- 29.Samii M, Tatagiba M, Piquer J, Carvalho GA. Surgical treatment of epidermoid cysts of the cerebellopontine angle. J Neurosurg. 1996;84:14–9. doi: 10.3171/jns.1996.84.1.0014. [DOI] [PubMed] [Google Scholar]
- 30.Schwartz JF, Balentine JD. Recurrent meningitis due to an intracranial epidermoid. Neurology. 1978;28:124–9. doi: 10.1212/wnl.28.2.124. [DOI] [PubMed] [Google Scholar]
- 31.Sinha AK. Brain stem epidermoid cyst. Surg Neurol. 1999;51:687–8. [PubMed] [Google Scholar]
- 32.Yoshizato K, Kai Y, Kuratsu J, Ushio Y. Intramedullary epidermoid cyst in the brain stem. Case report. Surg Neurol. 1996;45:537–40. doi: 10.1016/0090-3019(95)00470-x. [DOI] [PubMed] [Google Scholar]
- 33.Recinos PF, Roonprapunt C, Jallo GI. Intrinsic brainstem epidermoid cyst. Case report and review of the literature. J Neurosurg. 2006;104:285–9. doi: 10.3171/ped.2006.104.4.285. [DOI] [PubMed] [Google Scholar]
- 34.Takahashi M, Paz Paredes A, Scavarda D, Lena G. Brainstem epidermoid cyst in a child. Case report. Neurol Med Chir (Tokyo) 2007;47:140–4. doi: 10.2176/nmc.47.140. [DOI] [PubMed] [Google Scholar]
- 35.Ahmed I, Auguste KI, Vachhrajani S, Dirks PB, Drake JM, Rutka JT. Neurosurgical anagement of intracranial epidermoid tumors in children. J Neurosurg Pediatr. 2009;4:91–6. doi: 10.3171/2009.4.PEDS08489. [DOI] [PubMed] [Google Scholar]
- 36.Gopalakrishnan CV, Dhakoji A, Nair S. Epidermoid cyst of the brainstem in children: Case-based update. J Child Neurol. 2012;27:105–12. doi: 10.1177/0883073811414709. [DOI] [PubMed] [Google Scholar]
- 37.Ulrich J. Intracranial epidermoids. A study on their distribution and spread. J Neurosurg. 1964;21:1051–8. doi: 10.3171/jns.1964.21.12.1051. [DOI] [PubMed] [Google Scholar]
- 38.Tan TI. Epidermoids and dermoids of the central nervous system.(With two exceptional cases not represented in the literature) ActaNeurochir (Wien) 1972;26:13–24. doi: 10.1007/BF01413529. [DOI] [PubMed] [Google Scholar]
- 39.Toglia JU, Netsky MG, Alexander E., Jr Epithelial (epidermoid) tumors of the cranium. Their common nature and pathogenesis. J Neurosurg. 1965;23:384–93. doi: 10.3171/jns.1965.23.4.0384. [DOI] [PubMed] [Google Scholar]
- 40.Cobbs CS, Pitts LH, Wilson CB. Epidermoid and dermoid cysts of the posterior fossa. Clin Neurosurg. 1997;44:511–28. [PubMed] [Google Scholar]
- 41.Toglia JU, Netsky MG, Alexander E., Jr Epithelial (epidermoid) tumors of the cranium. Their common nature and pathogenesis. J Neurosurg. 1965;23:384–93. doi: 10.3171/jns.1965.23.4.0384. [DOI] [PubMed] [Google Scholar]
- 42.Ziyal IM, Bilginer B, Bozkurt G, Cataltepe O, Tezel GG, Akalan N. Epidermoid cyst of the brain stem symptomatic in childhood. Childs Nerv Syst. 2005;21:1025–9. doi: 10.1007/s00381-005-1172-y. [DOI] [PubMed] [Google Scholar]
- 43.Braun IF, Naidich TP, Leeds NE, Koslow M, Zimmerman HM, Chase NE. Dense intracranial epidermoid tumors: Computed tomographic observations. Radiology. 1977;122:717–9. doi: 10.1148/122.3.717. [DOI] [PubMed] [Google Scholar]
- 44.Doll A, Abu Eid M, Kehrli P, Esposito P, Gillis C, Bogorin A, et al. Aspect of FLAIR sequences, 3D-CISS and diffusion weight MR imaging of intracranial epidermoid cysts. J Neuroradiol. 2000;27:101–6. [PubMed] [Google Scholar]
- 45.Karantanas AH. MR imaging of intracranial epidermoid tumors: Specific diagnosis with turbo-FLAIR pulse sequence. Comput Med Imaging Graph. 2001;25:249–55. doi: 10.1016/s0895-6111(00)00069-0. [DOI] [PubMed] [Google Scholar]
- 46.Bergui M, Zhong J, Bradac GB, Sales S. Diffusion-weighted images of intracranial cyst-like lesions. Neuroradiology. 2001;43:824–9. doi: 10.1007/s002340100595. [DOI] [PubMed] [Google Scholar]
- 47.Tsuruda JS, Chew WM, Moseley ME, Norman D. Diffusion weighted MR imaging of the brain: Value of differentiating between extraaxial cysts and epidermoid tumors. AJNR Am J Neuroradiol. 1990;11:925–34. [PMC free article] [PubMed] [Google Scholar]
- 48.Fiume D, Gazzeri G, Spallone A, Santucci N. Epidermoid cysts of the fourth ventricle. Surg Neurol. 1988;29:178–82. doi: 10.1016/0090-3019(88)90002-x. [DOI] [PubMed] [Google Scholar]
- 49.Salazar J, Vaquero J, Saucedo G, Bravo G. Posterior fossa epidermoid cysts. Acta Neurochir (Wien) 1987;85:34–9. doi: 10.1007/BF01402367. [DOI] [PubMed] [Google Scholar]
- 50.Zhou LF. Intracranial epidermoidtumours: Thirty-seven years of diagnosis and treatment. Br J Neurosurg. 1990;4:211–6. doi: 10.3109/02688699008992726. [DOI] [PubMed] [Google Scholar]
- 51.Rubin G, Scienza R, Pasqualin A, Rotsa L, Da Pian R. Craniocerebral epidermoids and dermoids. Acta Neurochir (Wien) 1989;97:1–16. doi: 10.1007/BF01577734. [DOI] [PubMed] [Google Scholar]
- 52.Dubois PJ, Sage M, Luther JS, Burger PC, Heinz ER, Drayer BP. Malignant change in an epidermoid intracranial epidermoid cyst. J Comput Assist Tomogr. 1981;5:433–5. doi: 10.1097/00004728-198106000-00025. [DOI] [PubMed] [Google Scholar]
- 53.Goldman SA, Gandy SE. Squamous cell carcinoma as a late complication of intra cerebroventricular epidermoid cyst. J Neurosurg. 1987;66:618–20. doi: 10.3171/jns.1987.66.4.0618. [DOI] [PubMed] [Google Scholar]