Abstract
Objective:
The aim of this study was to discuss the technique of midsagittal splitting laminoplasty and to compare its short-term follow-up results with laminectomy in cases of compressive cervical spinal cord myelopathy.
Materials and Methods:
Exclusion criteria were as follows: Intramedullary compressive lesions, kyphotic cervical spine, previous spinal surgeries, and defective anterior vertebral column. Twenty patients (10 each of laminoplasty and laminectomy groups) were prospectively studied from 2005 to 2008. After clinico-radiological assessment, laminoplasty or laminectomy was performed in patients aged <50 years and >50 years, respectively. The laminoplasty was performed by splitting the excised lamina in midline up to the tip of spinous process. Follow-up was done by neurosurgical cervical spine scoring, Nurick's grading, and the final outcome was determined by Odom's criteria.
Results:
The mean operative time and blood loss in laminoplasty and laminectomy was 100 ± 0.87 (range 90-140 min), 80 ± 0.67 (range 75-100 min) P = 0.04; and 65 ± 0.07 (range 60-90 ml) and 68 ± 0.61 (range 65-80 ml) P = 0.09, respectively. There were no intraoperative accidents, and no postoperative neurological deterioration/recurrence of symptoms. One patient who underwent laminectomy alone developed progressive kyphosis of the spine, whereas one having rheumatoid arthritis and long symptom duration didn’t improve. 85% (17/20 patients) had sustained excellent to fair outcome (improvement by at least one Nurick's grade).
Conclusions:
The technique used by us was simple, effective, and inexpensive. There was no minimal postoperative morbidity, although long-term results are awaited.
Keywords: Cervical spondylitis, compressive spinal myelopathy, laminectomy, laminoplasty
Introduction
Cervical canal stenosis may be developmental, traumatic, secondary to multisegmental cervical spondylosis, or due to ossification of the posterior longitudinal ligament.[1,2] The cervical spondylitis is a common cause of compressive spinal myelopathy (CSM).[3] The laminoplasty provides adequate decompression of the spinal canal and, at the same time, reduces instability by preserving and reconstructing posterior vertebral elements of the spine [Table 1].[3,4,5,6] The stability of posterior vertebral elements also prevents the kyphosis and swan-neck deformity in long term.[3,4,5,6,7] Here, we performed a newer technique of laminoplasty to expand the antero-posterior diameter of cervical spine canal. The technique and its short-term follow-up results were compared to laminectomy.
Table 1.
Indications and contraindications of laminoplasty[3]
Materials and Methods
All patients having cervical spondylitis as the cause of CSM were prospectively analyzed from January 2005 to January 2008 at the university hospital. We excluded patients who previously underwent any kind of cervical spine surgery, patients having intramedullary lesion as the cause of myelopathy, associated kyphotic deformity of the cervical spine, or defective anterior column of cervical vertebra (due to trauma, tuberculosis, and or malignancy). The ethical approval was taken from the ethical committee of the university along with informed written consent from the patients.
The patient's neck was first immobilized by application of hard cervicalcollar. Clinical examination, neurosurgical cervical spine scoring (NCSS), Nurick's grading, X-ray cervical spine (antero-posterior and lateral views), and magnetic resonance imaging (MRI) of cervical spine were done [Tables 2 and 3]. The comorbid conditions (diabetes mellitus, rheumatoid arthritis, and hypertension) were managed simultaneously. The patients were divided into two groups according to the age, one who underwent laminoplasty (age <50 years), and other who underwent laminectomy alone (age >50 years). The demographic data, imaging findings, NCSS, and Nurick's grades were analyzed in the follow-up. The final outcome was determined by Odom's criteria [Table 4].
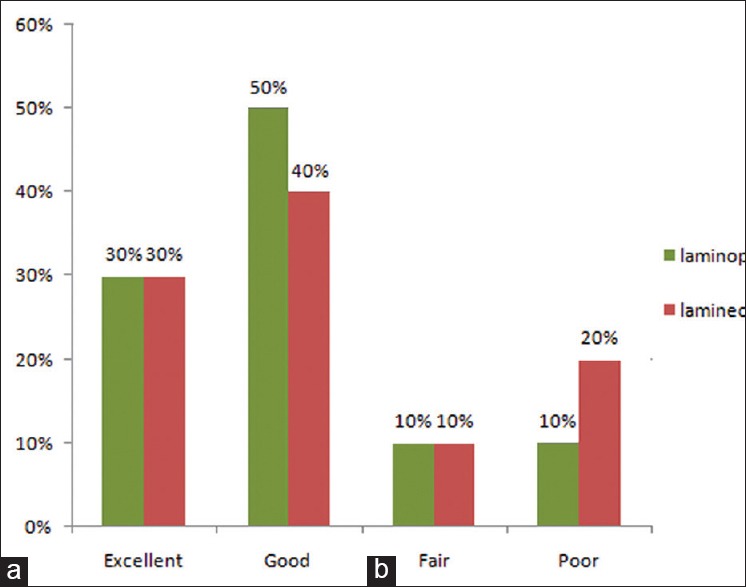
Table 2.
Nurick's classification of disability
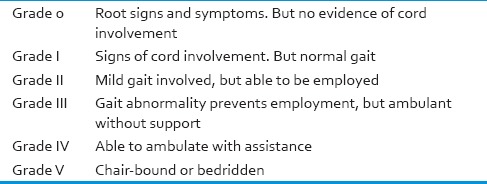
Table 3.
Neurosurgical cervical spine scoring
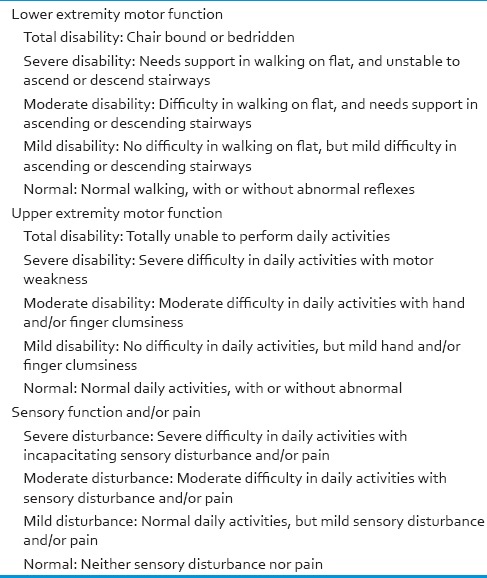
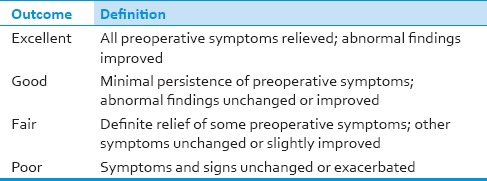
Table 4.
Odom's criteria for final outcome
Operative procedure
The surgery was done under general anesthesia. The patients positioned prone and the head was supported on a horseshoe-shaped pad in the neutral position. Midline longitudinal incision was made from two vertebras above to the two vertebras below of the diseased vertebras. Following exposure of appropriate lamina, the spinous processes of diseased vertebras along with one healthy vertebra above and below were tried to excised enblock with their spino-ligamentous complex. The lateral portion of laminas left in situ adjacent to the facet joint were drilled deeply to form gutters via the microspeed power system, having a 1.4 mm diamond shape burr (Aesculap B/BRAUN, Germany) [Figures 1 and 2]. The inside table of excised lamina was splited in midline up to the tip of spinous process. This portion serves the basis for the enlargement of cervical canal. A tunnel extending into the inferior articular process was made bilaterally on the excised lamina via the microspeed power system. Another tunnel was created into the corresponding portion of lamina left in situ. The excised lamina after splitting in midline was replaced to their position and secured via silk (2, 0) round body needle suture/22 gauge stainless steel wire passing into the tunnels created on adjacent laminas. If enblock excision of laminas was not successful, individual lamina excised and repositioned after midline splitting, as described above. Thus, antero-posterior diameter of the reconstructed neocanal was increased [Figure 3]. Suction drain was placed and wound closed in three layers via absorbable sutures. The compressive dressing was done. During surgery average blood loss, time of operation, and intraoperative accidents (excessive bleeding, fracture of lamina during excision and/or during drilling, injury to spinal cord and/or nerve roots, failed laminoplasty due to any reason) were noticed.
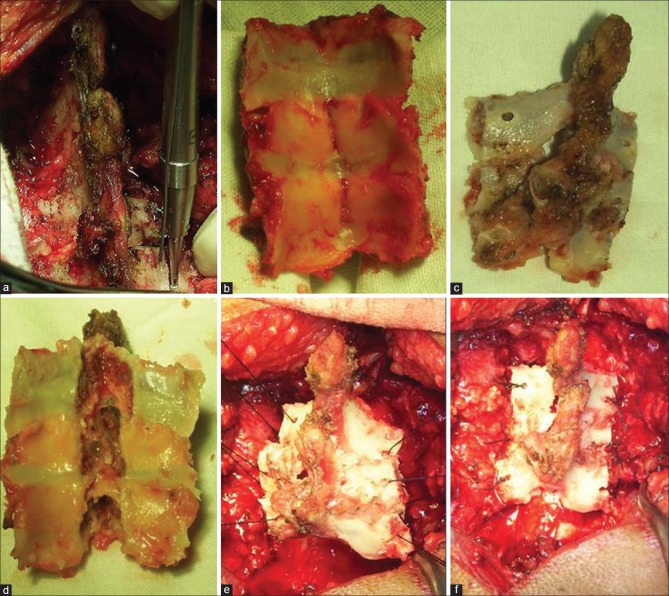
Figure 1.
(a) Exposed diseased cervical vertebras. (b) Laminas were excised enblock with a spino-ligamentous complex. (c) Tunnels were drilled into adjacent laminas on either side. (d) Midline saggital splitting of the inner table of lamina up to the tip of spinous process. (e) Splitted laminas were repositioned with a nonabsorbable suture. (f) Completed laminoplasty
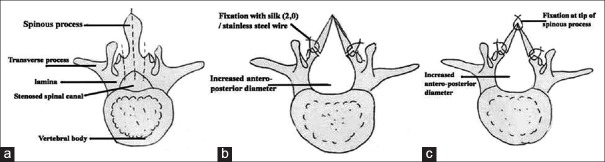
Figure 2.
(a) The inner table of individual lamina was splitted by either chesal and hammer, or (b, c) via microspeed power burr. (d) Individual lamina splitted in the midline. (e) Splitted laminas were repositioned with steel wires
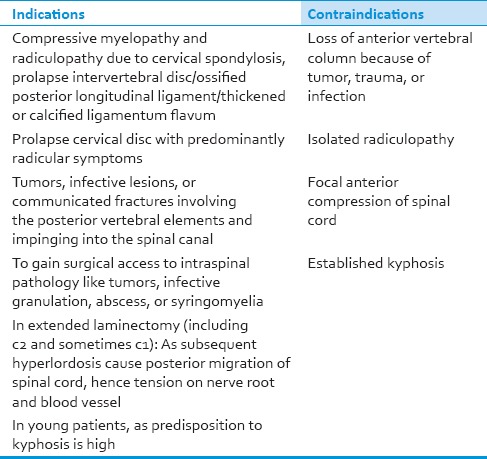
Figure 3.
Pictoreal diagram showing basis of the technique (dotted line denotes line of laminectomy). (a) Preoperative narrow antero-posterior spinal diameter. (b) Increased antero-posterior diameter of the spinal canal after laminoplasty
In the postoperative period, intravenous antibiotics amoxicillin clavulanic acid 1.2 gm 6 hourly and amikacin 500 mg 12 hourly was administered for 5 days. The patients were ambulated from bed on the next day of surgery with application of a hard cervical collar. We have not used any other external orthosis for neck immobilization. The patients were discharged on the sixth to eighth postoperative day with proper advice and follow-up. The patients were advised to wear a hard cervical collar for 3-4 weeks following surgery. The patients were reexamined in follow up at outdoor visits at 3 months interval for at least 2 years.
Statistics
The data were analyzed through SPSS software, version 17.0. The continuous variables were expressed as mean values and ranges (minimum to maximum), as well as in percentages. The analysis was performed using the Pearson χ2 for categorical variables and Student's t-test for continuous variables. The non-parametric analysis was done with the Wilcoxon signed rank test. The P <0.05 was considered as significant while <0.005 as highly significant.
Results
A total of 25 patients having CSM were admitted at the department of university hospital over a 3 year period. Five patients were excluded from the study (kyphotic deformity in one, previous spinal surgery in two, cervical spinal cord tumor in one, and intradural neurofibroma in one). The mean age at surgery was 58 ± 0.24 years (ranged 45-67 years). The male to female ratio was 19:1. The mean symptom duration was 18 ± 0.04 months (ranged 4-36 months). Three patients had diabetes mellitus. All patients had mixed sensory-motor symptomatology. The paraparasis was the most common presentation (65%, 13/20 patients) followed by monoparasis (20%, 4/20 patients) and quadriparasis (15%, 3/20 patients). Cervical mechanical changes (restricted neck movements and cervical pain) were present in 55% (11/20 patients) of patients. Muscle wasting was present in 15% (3/20) patients, which was related to their long symptom duration (P = 0.05). 35% (7/20) of patients had bladder and bowel involvement. 65% (13/20) of patients could not perform their jobs (Nurick's grade III).
On radiological assessment C5-C6-C7 vertebras were most commonly involved. All patients showed radiological changes of spondylitis in X-ray cervical spine and 90.4% (19/20) of these changes disappeared at the end of 2 years of follow-up [Figure 4]. It was observed that if patients had a symptom duration of less than 5 months, there were no changes in the intensity of spinal cord on either T1- or T2-weighted MRI images (P = 0.08). However, as the duration of symptoms increased, the signal intensity of spinal cord in MRI images also increased (suggestive of dysplastic changes). The first noticeable change on MRI is on T2-weighted MRI images, and these images are also more sensitive for predicting outcome. The patients having signal changes on only T2-weighted images (85%, 17/20 patients) had better outcome in the postoperative period compared to those having altered signal on both T1- and T2-weighted MRI images (P = 0.04). One patient who underwent laminectomy alone had developed kyphosis after 6 months of surgery, which further progressed in the follow-up.
Figure 4.
(a) Preoperative X-ray: Lateral view of cervical spine showing loss of cervical lordosis, anterior and posterior osteophytosis suggestive of cervical spondylosis. (b) Postoperative X-ray showing loss of posterior osteophytes and slight regain of lordosis
The laminoplasty/laminectomy was done from C4 to C7 in most of the cases. In six patients, the laminoplasty was done enblock, while in four it was done by repositioning of individual lamina. In authors’ opinion, it takes longer time with the later technique, but had not affected the final outcome. The mean operative time in laminoplasty and laminectomy was 100 ± 0.87 (range 90 − 140 min) and 80 ± 0.67 (range 75-100 min) P = 0.04. The average blood loss in laminoplasty and laminectomy was 65 ± 0.07 ml (range 60-90 ml) and 68 ± 0.61 (range 65-80 ml) P = 0.09.
There were no intraoperative accidents. The most common complication in the postoperative period was cerebrospinal fluid leak 15% (3/20 patients) followed by wound infection 10% (2/20 patients). Both the above complications were managed conservatively by prolonged use of intravenous antibiotics, regular dressings, and strict control of blood sugar in diabetic patients.
The follow-up was done at outdoor visits, questionnaires by mail, or on telephone calls. The symptom that improved earliest was radicular pain. The range of neck movements improved in both groups and compared between both laminectomy and laminoplasty groups.
On comparing Nurick's grade at the end of 2 years, it was found that within the laminoplasty group: One patient having grade V improved to grade IV and lost to follow-up at 1 year. Seven patients having grade IV of which five improved to grade III, one to grade II, and one did not improved at 6 months. All these patients improved further to one grade of Nurick's at the end of 2 years. Two patients of grade III improved to grade II at 6 months and further to grade I after 2 years. Among the laminectomy group, two patients of grade V improved to grade IV. One patient had lost to follow-up at 1 year, while the second patient remained in grade IV at 1 year of follow-up. Out of six patients having grade IV Nurick's, three had improved to grade III, two to grade II, while one remained in grade IV at 6 months of follow-up. These five patients had further improved to grade I at 2 years. The patient, who had not improved in follow-up after 6 months, had lost to follow-up. Out of two patients having grade III Nurick's, one improved to grade II at 6 months and grade I at 2 year. One patient deteriorated in the postoperative period up to Nurick's grade I, who acquired kyphotic deformity of the neck [Table 5].
Table 5.
Preoperative and follow up Nurick's grades
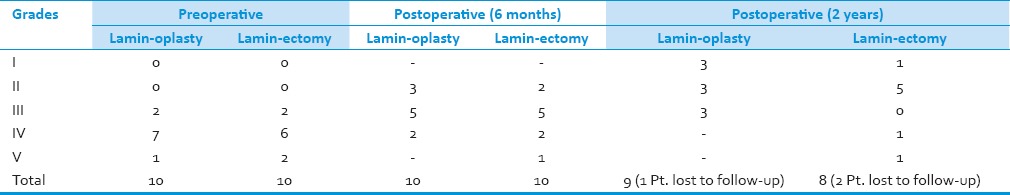
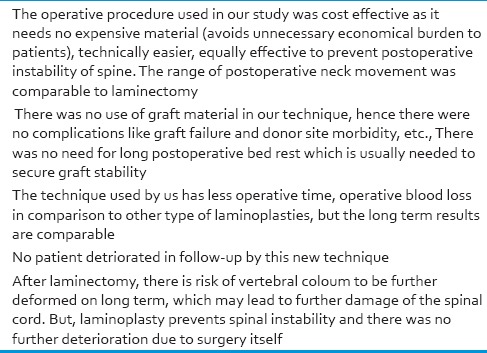
In both groups, the mean NCSS scoring improved significantly in the postoperative period (non-parametric analysis with the Wilcoxon signed rank test) [Table 6]. In 2 years of follow-up, neither patient deteriorated nor had recurrence of symptoms, except one who developed progressive kyphosis of cervical spine after laminectomy alone. One patient having both diabetes mellitus and rheumatoid arthritis along with the long duration of symptoms did not improve at all. The final outcome based on Odom's criteria is shown in Figure 5.
Table 6.
Comparison of NCSS scores at the end of 2 years
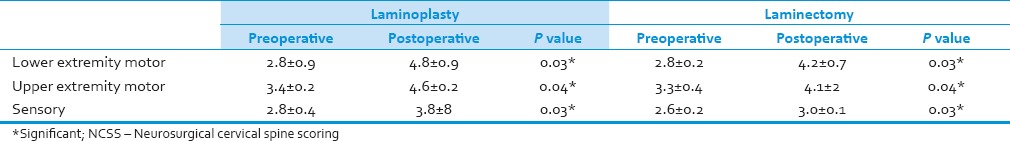
Figure 5.
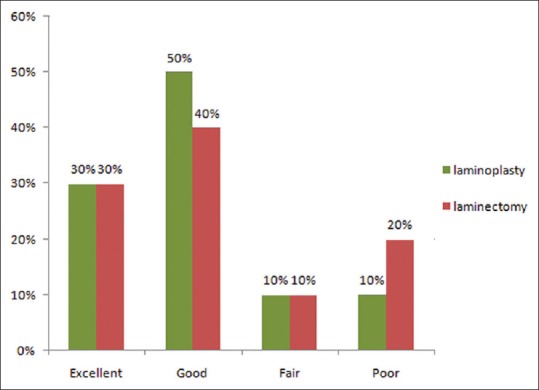
Outcome at the end of 2 years (Odoms’ criteria) in both laminoplasty and laminectomy groups
Discussion
Stookey advocated the removal of cartilaginous nodules of degenerate disk material for cervical spondylotic myelopathy.[8,9] Cervical spondylosis with multiple osteophytes better responds by extensive posterior decompression compared to limited laminectomy, so Aboulker et al. introduced total laminectomy from C-1 to D-1.[8,9,10] However, after laminectomy spinal deformity has been reported in 10-15% of the cases.[11,12] As in elder patients with poor muscular tone lack of cervical spine support lead to the development of cervical instability and kyphosis.[13] The laminoplasty is the procedure of choice in CSM, especially when multiple vertebras involve in young age.[14,15,16] In laminoplasty, the dura is covered by the bone; thus, restrangulation by the postlaminectomy membrane does not occur.[18,28,29] But laminoplasty does not have good results in aged >65 years, myelopathy of >2 year duration, spinal canal stenosis of >60%, and kyphotic cervical spine curvature.[17,18]
Omaya and Hattori et al. described expansive lamina Z plasty.[7,17,19] Since then, several modifications such as use of wires, iliac bone graft, rib allografts, ceramic/apatite beads, mid-longitudinal bone graft, tension band laminoplasty, vascularized pedicled laminoplasty, vascularized pedicle on supraspinous, interspinous, and interlaminor ligaments, expensive midline T-saw laminoplasty, CG-Clip-assisted laminoplasty, etc., have been described.[20,21,22,23,24,25,26] All these procedures were technically demanding and cause some economic burden to the patients. But the technique described by us was not expensive.
We observed that it takes about 5 months for the CSM to produce signal changes in the spinal cord on MRI. The preoperative MRI may help to predict the postoperative outcome of surgery as signal changes on both T1- and T2-weighted MRI images showed poor outcome compared to the signal changes on T2-weighted MRI images only.[3,6]
We had used Nurick's grade because of its simplicity (gait disturbances) which can be obtained by mail or telephonic questionnaire.[27] NCSS scoring provides objective assessment of sensory − motor functions.[3] Odom's criteria are the simplest and most widely used for outcome assessment.[3,27] Based on Odom's criteria, 85% (17/20) of patients had sustained excellent to fair results (improvement by at least one Nurick's grade), despite initial advanced disease (Nurick's Grade IV/V).
Our technique increased the diameter of spinal canal which enhances neurological recovery because of canal enlargement and improvement in the circulation of the spinal cord and nerve roots.[18,28,29] The re-stenosis of the spinal canal is supposed to be the most common complication of our technique, but the authors did not encounter it in any patients till date; however, long-term results are still awaited. Other complications reported in the literature, like transient C5-6 root paresis, severe neck pain with or without paresthesias, and under riding of the lamina at the hinged side had not occurred in any of our patients.[13] The technique is cost effective (need no expansive material), simple, effective to prevent postoperative instability, but technically demanding. There were no risk of graft failure, donor site morbidity, and neurological deterioration [Table 7]. There was no need for prolonged bed rest to secure graft stability. The technique needed less operative time, less blood loss contrary to what had been reported in the literature, but with comparable results.[3]
Table 7.
Conclusions drawn from our study
To conclude midsaggital splitting, the laminoplasty technique was effective for the treatment of CSM, although long-term results of the technique is still awaited.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Samii M, Völkening D, Sepehrnia A, Penkert G, Baumann H. Surgical treatment of myeloradiculopathy in cervical spondylosis. A report on 438 operations. Neurosurg Rev. 1989;12:285–90. doi: 10.1007/BF01780841. [DOI] [PubMed] [Google Scholar]
- 2.Nikolaidis I, Fouyas IP, Sandercock PA, Statham PF. Surgery for cervical radiculopathy or myelopathy. Cochrane Database Syst Rev. 2010;20:CD001466. doi: 10.1002/14651858.CD001466.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agrawal D, Sharma BS, Gupta A, Mehta VS. Efficacy and results of expansive laminoplasty in patients with severe cervical myelopathy due to cervical canal stenosis. Neurol India. 2004;52:54–8. [PubMed] [Google Scholar]
- 4.Herkowitz HN. A comparison of anterior cervical fusion, cervical laminectomy, and cervical laminoplasty for the surgical management of multiple level spondylotic radiculopathy. Spine (Phila Pa 1976) 1988;13:774–80. doi: 10.1097/00007632-198807000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Iwasaki M, Kawaguchi Y, Kimura T, Yonenobu K. Long-term results of expansive laminoplasty for ossification of the posterior longitudinal ligament of the cervical spine: Morethan 10 yearsfollowup. J Neurosurg. 2002;96(2 Suppl):180–9. [PubMed] [Google Scholar]
- 6.Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976) 1981;6:354–64. doi: 10.1097/00007632-198107000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Kawai S, Sunago K, Doi K, Saika M, Taguchi T. Cervical laminoplasty (Hattori's method). Procedure and follow-up results. Spine (Phila Pa 1976) 1988;13:1245–50. [PubMed] [Google Scholar]
- 8.Stoops WL, King RB. Neural complications of cervical spondylosis: Their response to laminectomy and foramenotomy. J Neurosurg. 1962;19:986–99. doi: 10.3171/jns.1962.19.11.0986. [DOI] [PubMed] [Google Scholar]
- 9.Patchell RA, Tibbs PA, Young AB, Clark DB, Alban G. Smith and the beginnings of spinal surgery. Neurology. 1987;37:1683–4. doi: 10.1212/wnl.37.10.1683. [DOI] [PubMed] [Google Scholar]
- 10.Piepgras DG. Posterior decompression for myelopathy due to cervical spondylosis: Laminectomy alone versus laminectomy with dentate ligament section. Clin Neurosurg. 1977;24:508–15. doi: 10.1093/neurosurgery/24.cn_suppl_1.508. [DOI] [PubMed] [Google Scholar]
- 11.Mikawa Y, Shikata J, Yamamuro T. Spinal deformity and instability after multilevel cervical laminectomy. Spine (Phila Pa 1976) 1987;12:6–11. doi: 10.1097/00007632-198701000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Alvisi C, Borromei A, Cerisoli M, Giulioni M. Long-term evaluation of cervical spine disorders following laminectomy. J NeurosurgSci. 1988;32:109–12. [PubMed] [Google Scholar]
- 13.Praharaj SS, Vasudev MK, Kolluri VR. Laminoplasty: An evaluation of 24 cases. Neurol India. 2000;48:249–54. [PubMed] [Google Scholar]
- 14.Skowroński J, Bielecki M. The results of laminectomy and laminoplasty in cervical myeloradiculopathy. RoczAkad Med Bialymst. 1992;37:71–3. [PubMed] [Google Scholar]
- 15.Tsuji H. Laminoplasty for patients with compressive myelopathy due to so-called spinal canal stenosis in cervical and thoracic regions. Spine (Phila Pa 1976) 1982;7:28–34. doi: 10.1097/00007632-198200710-00002. [DOI] [PubMed] [Google Scholar]
- 16.Wang MY, Shah S, Green BA. Clinical outcomes following cervical laminoplasty for 204 patients with cervical spondylotic myelopathy. Surg Neurol. 2004;62:487–92. doi: 10.1016/j.surneu.2004.02.040. [DOI] [PubMed] [Google Scholar]
- 17.Itoh T, Tsuji H. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine (Phila Pa 1976) 1985;10:729–36. doi: 10.1097/00007632-198510000-00007. [DOI] [PubMed] [Google Scholar]
- 18.Kohno K, Kumon Y, Oka Y, Matsui S, Ohue S, Sakaki S. Evaluation of prognostic factors following expansive laminoplasty for cervical spinal stenotic myelopathy. Surg Neurol. 1997;48:237–45. doi: 10.1016/s0090-3019(97)00166-3. [DOI] [PubMed] [Google Scholar]
- 19.Kawai S, Sunago K, Doi K, Saika M, Taguchi T. Cervical laminoplasty (Hattori's method). Procedure and follow-up results. Spine (Phila Pa 1976) 1998;13:1245–50. [PubMed] [Google Scholar]
- 20.Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8:693–9. doi: 10.1097/00007632-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Lee TT, Manzano GR, Green BA. Modified open-door cervical expansive laminoplasty for spondylotic myelopathy: Operative technique, outcome, and predictors for gait improvement. J Neurosurg. 1997;86:64–8. doi: 10.3171/jns.1997.86.1.0064. [DOI] [PubMed] [Google Scholar]
- 22.Asano T, Tsuzuki N. Surgical management of ossification of posterior longitudinal ligament. In: Schmidek HH, Sweet WH, editors. Operative Neurosurgical Techniques. Philadelphia: W.B.Saunders; 1995. pp. 1825–8. [Google Scholar]
- 23.Goel A. Vascularised pedicled laminoplasty. Surg Neurol. 1997;48:442–5. doi: 10.1016/s0090-3019(97)00292-9. [DOI] [PubMed] [Google Scholar]
- 24.Nakano K, Harata S, Suetsuna F, Araki T, Itoh J. Spinous process-splitting laminoplasty using hydroxyapatite spinous process spacer. Spine (Phila Pa 1976) 1992;17(3 Suppl):41–3. doi: 10.1097/00007632-199203001-00009. [DOI] [PubMed] [Google Scholar]
- 25.Koyama T, Iwasaki K, Watanabe K, Handa J. Osteoplastic laminectomy using hydroxyapatite ceramic implants. No ShinkeiGeka. 1986;14:151–9. [PubMed] [Google Scholar]
- 26.Kihara S, Umebayashi T, Hoshimaru M. Technical improvements and results of open-door expansive laminoplasty with hydroxyapatite implants for cervical myelopathy. Neurosurgery. 2005;57(4 Suppl):348–56. doi: 10.1227/01.neu.0000176646.88909.82. [DOI] [PubMed] [Google Scholar]
- 27.Nurick S. The natural history and the results of surgical treatment of the spinal disorders associated with cervical spondylosis. Brain. 1972;95:101–8. doi: 10.1093/brain/95.1.101. [DOI] [PubMed] [Google Scholar]
- 28.Kawaguchi Y, Kanamori M, Ishihara H, Kikkawa T, Matsui H, Tsuji H, et al. Clinical and radiographic results of expansive lumbar laminoplasty in patients with spinal stenosis. J Bone Joint Surg Am. 2005;87(Suppl 1):292–9. doi: 10.2106/JBJS.E.00211. [DOI] [PubMed] [Google Scholar]
- 29.Baba H, Uchida K, Maezawa Y, Furusawa N, Wada M, Imura S. Three-dimensional computed tomography for evaluation of cervical spinal canal enlargement after en-bloc open-door laminoplasty. Spinal Cord. 1997;35:674–9. doi: 10.1038/sj.sc.3100473. [DOI] [PubMed] [Google Scholar]