Abstract
Background and Objective:
Cervical spinal cord injury (CSCI) with a stable spine has been increasing as the elderly population is dramatically increasing all over the world. In this study, we evaluated the neurological outcome of decompression surgery (laminoplasty) for these patients.
Materials and Methods:
Forty-one patients with CSCI with stable spine who underwent decompression surgery (laminoplasty) were retrospectively studied. Inclusion criteria were as follows: CSCI without instability, spinal cord contusion in magnetic resonance image (MRI), spinal cord compression rate more than 20%, neurologic deficit American Spinal Cord Injury Association ([ASIA] scale from A to D), and follow-up of at least 12 months. Preoperative neurological state, clinical outcome, and neurological function were measured using the ASIA impairment scale, Japanese Orthopaedic Association (JOA) grading scale, and Hirabayashi recovering rate, respectively.
Results:
Thirty-three (80.4%) patients showed improvement in ASIA grade at 12-month follow-up. Four (9.7%) patients in ASIA Grade A and 4 (9.7%) patients in ASIA Grade D remain unchanged. The mean JOA score improved from 8.4 ± 6.1 points preoperatively to 11.2 ± 5.4 points at 12 months postoperatively. Improvement in JOA was statistically significant (P < 0.05). The mean Hirabayashi recovery rate was 37.4 ± 25.3%.
Conclusion:
Surgical decompression (laminoplasty) is helpful in relieving cord compromise and neurological deficit in CSCI with stable spine.
Keywords: Laminoplasty, outcome, spinal injury, surgical decompression
Introduction
Spinal cord injuries occur approximately 14,000/year in North America, and most involve the cervical spine region. Patients who sustain cervical spinal cord injuries usually have lasting, often devastating, neurological deficits and disabilities.[1,2] Management can affect the outcome in these patients; therefore, clinicians worldwide strive to provide the best conservative or surgical approach.
Although surgery has become the preferred method of management of traumatic unstable cervical spine injury, the treatment of spinal cord injury (SCI) without instability such as fracture, dislocation, and ligamentous injury, however, remains controversial.[3] In addition, the controversy surrounding the role and timing of surgery in SCI with stable spine remains unresolved.[4] Mirza et al. examined 43 patients and stated that early surgical (<72 h) intervention may improve recovery.[5] Advocates of conservative treatment, however, have claimed results at least as good with a low incidence of neurological deterioration.[6] However, faced with a patient with neurologic dysfunction and magnetic resonance image (MRI) evidence of cervical spinal cord compression, decompressive surgery is a practical treatment option. Laminoplasty is usually reserved for patients with multiple-level spinal cord compression.[7] It is safe and easily performed. In this study, we evaluated the efficacy of laminoplasty in the management of SCI with stable spine.
Materials and Methods
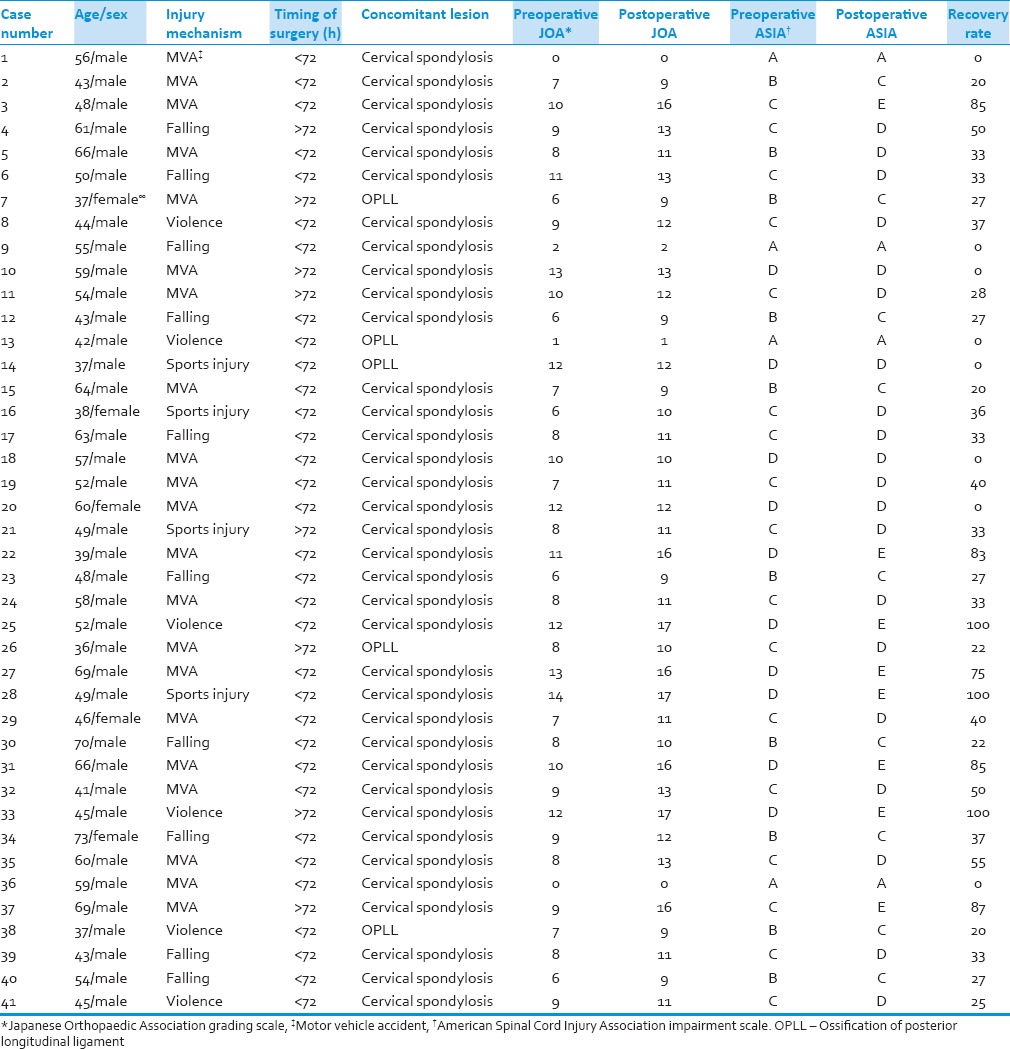
The study population in this retrospective study (an observational study using analytic retrospective study cohort design) consisted of 41 consecutive patients of cervical SCI (CSCI) with stable spine who had undergone cervical laminoplasty (Hirabayashi Technique) by senior surgeon in our institute between August 2006 and August 2010. The mean patient age was 52.1 ± 11.3 years (range, 36–73 years) [Table 1]. There were 36 men and 5 women. The mean follow-up period was 15.5 ± 9.3 months (range, 12–36 months).
Table 1.
Summary of patients data
According to the time of surgery, the patients were classified into two groups: Early surgical group (surgery within 72 h) and delayed surgical group (surgery after 72 h).
Imaging findings in favor of cervical spondylosis (disc prolapse, osteophyte, and hypertrophy of ligamentum flavum) and ossification of posterior longitudinal ligament (OPLL) were also recorded.
The inclusion criteria were as follows: CSCI without instability, spinal cord contusion in MRI, spinal cord compression rate more than 20%, neurologic deficit American SCI Association ([ASIA] scale from A to D), and follow-up of at least 12 months. Patients who had CSCI with instability, kyphosis, or neurologically intact patients were excluded from the study.
The rate of spinal cord compression was measured by sagittal view MRI. The spinal cord diameter was measured at both the intact level and the injured level on T1-weighted MRI sequences and was calculated by the following method:
(X–Y)/X × 100%
Where X is the diameter of the cervical cord at the intact level and Y is the diameter of the cervical cord at the injured level. A rate of 20% was defined as a cut-off point for the spinal cord compression rate.
Instability was defined by failure or loss of function of anterior or posterior elements, relative translation of vertebra in sagittal plane more than 3.5 mm and angulation >11°.
Cervical instability was assessed by plain film, dynamic view (flexion and extension), computed tomography, and MRI.
Preoperative neurological state, clinical outcome, and neurological function were measured using the ASIA impairment scale, Japanese Orthopaedic Association (JOA) grading scale, and Hirabayashi recovering rate ([postoperative JOA score – preoperative JOA scores]/[17 – preoperative JOA score] × 100%), respectively. Those assessments were made at admission and at 12-month follow-up.
The data obtained were statistically analyzed using SPSS (SPSS for Windows Release 12.0, Chicago, Illinois, USA). Fisher exact test and repeated measures ANOVA were used for data analysis. Statistical significance was set at P ≤ 0.05.
Results
Changes in the ASIA grade were evaluated from admission to 1-year after the injury. Thirty-three (80.4%) patients showed improvement in ASIA grade at 12-month follow-up. Four (9.7%) patients in ASIA Grade A and 4 (9.7%) patients in ASIA Grade D remain unchanged. The mean JOA score improved from 8.4 ± 6.1 points preoperatively to 11.2 ± 5.4 points at 12 months postoperatively. Improvement in JOA was statistically significant (P < 0.05). The mean Hirabayashi recovery rate was 37.4 ± 25.3%.
Mechanisms of injury were as follows: Motor vehicle accident (35%), falls (25%), violence (15%), and sports injury (9%).
Thirty-three (80.4%) patients underwent surgery within 72 h of injury and 8 (19.5%) patients underwent surgery after 72 h. There was no significant difference between these two groups (P > 0.05).
In this study, 30 patients had spinal cord compression rate <50% and 11 patients had spinal cord compression rate >50%. A group with compression rate <50% showed better neurologic outcome; however, this just failed to reach significance (P > 0.05).
Concomitant pathologic conditions such as cervical spondylosis and OPLL were noted in all patients. Thirty-six (87.8%) patients had cervical spondylosis and 5 (12.2%) had OPLL. Patients with cervical spondylosis had higher Hirabayashi recovery rate than patients with OPLL (P < 0.05).
No major complication occurred in patients after surgery.
Discussion
There is no absolute consensus regarding the best treatment modality (surgical or conservative management) of SCI without instability. Chen et al. reported decompression surgery to be associated with an immediate neurologic improvement and a better long-term neurologic outcome than for conservative treatment.[8] Lenehan et al. concluded that it is reasonable and safe to consider early surgical decompression in patients with neurologic deficit and persistent spinal cord compression due to CSCI without fracture or instability.[9] However, Katoh and el Masry reported that conservative treatment remains a good option for patients with cervical spinal cord injuries.[10]
This study showed that surgical decompression (laminoplasty) delivered good neurologic outcome in CSCI with stable spine.
In the study performed by Kawano et al.,[11] patients with either ASIA A or D were excluded from the study because patients with ASIA A showed a very poor general condition and surgical treatment was thought to have a negative effect on their general condition. Either patients with ASIA A or D did not show significant neurologic improvement after surgery. In our study, patients with ASIA A remain unchanged, but improvement of patients with ASIA D was statistically significant after surgery. Therefore, surgical decompression in patients with ASIA D is a logical choice.
There is considerable uncertainty regarding the role of the timing of surgical decompression of the spinal cord in the management of patients with SCI. Some researchers believe that early surgical stabilization may improve the neurological outcome.[12,13,14] In our study, no significant difference was observed in neurologic improvement between the early surgical group (<72 h) and delayed surgical group (>72 h) (P > 0.05).
In our series, comparison of Hirabayashi recovery rates in patients having cervical spondylosis versus OPLL showed that patients with preexisting cervical spondylosis had higher recovery rate than patients with preexisting OPLL. This finding may provide guidance for counseling and determining the prognosis of SCI patients after laminoplasty operations.
Recent studies have shown that there are wide variations in the choice of surgical approach for decompression of the cervical spine based on an individual surgeon's preferences.[15] Studies, including the recent AOS pine International multicenter prospective study, have also shown that the majority of the spine surgeons prefer the anterior approach in 51–60% of cases, posterior approach in about 35%, and a combined approach in the remaining cases. This is mainly due to the variations in the clinical and radiological parameters and to some extent due to surgeons’ preferences.[16,17] Laminoplasty was popularized in the late 1970s by Japanese spine surgeons who recognized the complications of standalone laminectomy.[18] The advantages of laminoplasty include: (1) It is a motion-preserving procedure, (2) the disadvantage of laminectomy, namely the development of postlaminectomy membrane is avoided, (3) unlike in laminectomy because the posterior bony elements are preserved, revision posterior surgery is not compromised by the exposed dura. Currently, the commonly accepted indications for laminoplasty include patients with preserved cervical lordosis if they have: (1) Multilevel cervical stenotic myelopathy (≥3-level disease), (2) cervical canal stenosis, and (3) posterior cord compression at multiple levels. Consequently, we performed laminoplasty for our patients due to aforementioned criteria.
The degree of spinal cord compression did not affect patients’ neurologic outcome in our study. Although good neurologic outcome was observed at <50% cord compression rate, neurologic outcome according to the degree of spinal cord compression was failed to reach significance (P > 0.05). However, Yoo et al., reported neurologic deterioration after trauma, and outcome after surgery depended on the diameter of the residual spinal canal.[19]
Some limitations in this study include: This study was a retrospective, nonrandomized study. The number of patients was small. Control group were needed to compare the treatment outcomes following conservative treatment and laminoplasty.
Conclusion
Acknowledging its numerous limitations, this retrospective study supports surgical intervention (laminoplasty) in the setting of SCI with stable spine as a safe and helpful management option. Improved ASIA grades were identified in those patients managed surgically. A prospective, randomized controlled trial is needed to definitively compare surgical versus conservative management in the setting of SCI with stable spine.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Pickett W, Simpson K, Walker J, Brison RJ. Traumatic spinal cord injury in Ontario, Canada. J Trauma. 2003;55:1070–6. doi: 10.1097/01.TA.0000034228.18541.D1. [DOI] [PubMed] [Google Scholar]
- 2.Cripps RA, Lee BB, Wing P, Weerts E, Mackay J, Brown D. A global map for traumatic spinal cord injury epidemiology: Towards a living data repository for injury prevention. Spinal Cord. 2011;49:493–501. doi: 10.1038/sc.2010.146. [DOI] [PubMed] [Google Scholar]
- 3.Chikuda H, Ohtsu H, Ogata T, Sugita S, Sumitani M, Koyama Y, et al. Optimal treatment for spinal cord injury associated with cervical canal stenosis (OSCIS): A study protocol for a randomized controlled trial comparing early versus delayed surgery. Trials. 2013;14:245. doi: 10.1186/1745-6215-14-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fehlings MG, Perrin RG. The role and timing of early decompression for cervical spinal cord injury: Update with a review of recent clinical evidence. Injury. 2005;36(Suppl 2):B13–26. doi: 10.1016/j.injury.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 5.Mirza SK, Krengel WF, 3rd, Chapman JR, Anderson PA, Bailey JC, Grady MS, et al. Early versus delayed surgery for acute cervical spinal cord injury. Clin Orthop Relat Res. 1999;359:104–14. doi: 10.1097/00003086-199902000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Lauweryns P. Role of conservative treatment of cervical spine injuries. Eur Spine J. 2010;19(Suppl 1):S23–6. doi: 10.1007/s00586-009-1116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steinmetz MP, Resnick DK. Cervical laminoplasty. Spine J. 2006;6(6 Suppl):274S–81S. doi: 10.1016/j.spinee.2006.04.023. [DOI] [PubMed] [Google Scholar]
- 8.Chen TY, Dickman CA, Eleraky M, Sonntag VK. The role of decompression for acute incomplete cervical spinal cord injury in cervical spondylosis. Spine (Phila Pa 1976) 1998;23:2398–403. doi: 10.1097/00007632-199811150-00007. [DOI] [PubMed] [Google Scholar]
- 9.Lenehan B, Fisher CG, Vaccaro A, Fehlings M, Aarabi B, Dvorak MF. The urgency of surgical decompression in acute central cord injuries with spondylosis and without instability. Spine (Phila Pa 1976) 2010;35(21 Suppl):S180–6. doi: 10.1097/BRS.0b013e3181f32a44. [DOI] [PubMed] [Google Scholar]
- 10.Katoh S, el Masry WS. Neurological recovery after conservative treatment of cervical cord injuries. J Bone Joint Surg Br. 1994;76:225–8. [PubMed] [Google Scholar]
- 11.Kawano O, Ueta T, Shiba K, Iwamoto Y. Outcome of decompression surgery for cervical spinal cord injury without bone and disc injury in patients with spinal cord compression: A multicenter prospective study. Spinal Cord. 2010;48:548–53. doi: 10.1038/sc.2009.179. [DOI] [PubMed] [Google Scholar]
- 12.Fehlings MG, Rabin D, Sears W, Cadotte DW, Aarabi B. Current practice in the timing of surgical intervention in spinal cord injury. Spine (Phila Pa 1976) 2010;35(21 Suppl):S166–73. doi: 10.1097/BRS.0b013e3181f386f6. [DOI] [PubMed] [Google Scholar]
- 13.Fehlings MG, Vaccaro A, Wilson JR, Singh A, Cadotte DW, Harrop JS, et al. Early versus delayed decompression for traumatic cervical spinal cord injury: Results of the surgical timing in acute spinal cord injury study (STASCIS) PLoS One. 2012;7:e32037. doi: 10.1371/journal.pone.0032037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Furlan JC, Noonan V, Cadotte DW, Fehlings MG. Timing of decompressive surgery of spinal cord after traumatic spinal cord injury: An evidence-based examination of pre-clinical and clinical studies. J Neurotrauma. 2011;28:1371–99. doi: 10.1089/neu.2009.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Irwin ZN, Hilibrand A, Gustavel M, McLain R, Shaffer W, Myers M, et al. Variation in surgical decision making for degenerative spinal disorders. Part II: Cervical spine. Spine (Phila Pa 1976) 2005;30:2214–9. doi: 10.1097/01.brs.0000181056.76595.f7. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham MR, Hershman S, Bendo J. Systematic review of cohort studies comparing surgical treatments for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2010;35:537–43. doi: 10.1097/BRS.0b013e3181b204cc. [DOI] [PubMed] [Google Scholar]
- 17.Ghogawala Z, Coumans JV, Benzel EC, Stabile LM, Barker FG., 2nd Ventral versus dorsal decompression for cervical spondylotic myelopathy: Surgeons’ assessment of eligibility for randomization in a proposed randomized controlled trial: Results of a survey of the Cervical Spine Research Society. Spine (Phila Pa 1976) 2007;32:429–36. doi: 10.1097/01.brs.0000255068.94058.8a. [DOI] [PubMed] [Google Scholar]
- 18.Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine (Phila Pa 1976) 1983;8:693–9. doi: 10.1097/00007632-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Yoo DS, Lee SB, Huh PW, Kang SG, Cho KS. Spinal cord injury in cervical spinal stenosis by minor trauma. World Neurosurg. 2010;73:50–2. doi: 10.1016/j.surneu.2009.05.021. [DOI] [PubMed] [Google Scholar]


