INTRODUCTION
Multiple myeloma (MM) pathogenesis may broadly be defined as a malignancy of terminally differentiated B cells that produce a complete and/or partial (light chain) monoclonal immunoglobulin protein.1 Although clinical manifestations may present in diverse ways, the cardinal signs—hypercalcemia, renal in sufficiency, anemia, and bone lesions (collectively known as “CRAB” signs)—are quite common and result from end-organ damage caused by myeloma mass effect or inflammatory proteins.2 MM represents 1.6% of all new cancer cases in the United States, comprising approximately 10% of hematological malignancies.3 Despite research and development, MM remains largely incurable, with a five-year survival rate of 46.6%.2,3
Carfilzomib (Kyprolis, Amgen) is a proteasome inhibitor indicated for the treatment of patients with relapsed or refractory MM.4 The Food and Drug Administration (FDA) awarded carfilzomib accelerated approval in July 2012 as monotherapy.5 The medication is now indicated for use as a single agent in patients with relapsed or refractory MM who have received one or more lines of therapy.4 In July 2015, the FDA approved carfilzomib as a component of combination therapy.6 It is currently indicated with dexamethasone or with lenalidomide (Revlimid, Celgene) plus dexamethasone for the treatment of relapsed or refractory MM in patients who have received one to three lines of prior treatment.4
MECHANISM OF ACTION
Carfilzomib is a modified epoxyketone that selectively targets the proteasome enzymes within the cell. It irreversibly binds to the active sites of the 20S proteasome, as well as the core component within the 26S proteasome. By selectively and irreversibly inhibiting these proteasomes, carfilzomib has the ability to delay proliferation and induce apoptosis to malignant plasma cells.7
Proteasomes have various roles in eukaryotic cell development, such as protein degradation, regulation of DNA repair, and proliferation. The 20S proteasome functions in several peptidase actions as well as proteolysis involving a threonine-binding site. The 26S proteasome is a complex containing both 20S and 19S proteasomes. It is responsible for the degradation of ubiquitinated proteins and several binding protein substrates. Thus, selectively inhibiting their function will induce cell-cycle arrest and lead to apoptosis of malignant plasma cells in the bone marrow.8,9
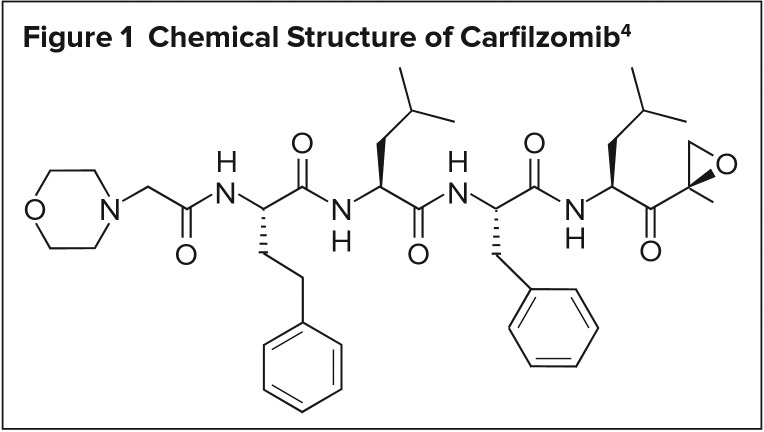
A tetrapeptide epoxyketone epoxide that is isolated as the crystalline free base, carfilzomib is essentially insoluble in water and very slightly soluble in acidic conditions. Kyprolis is available in 60-mg single-dose vials. It appears as a white to off-white lyophilized cake or powder.4,7 Its chemical structure is shown in Figure 1.
Figure 1.
Chemical Structure of Carfilzomib4
PHARMACOKINETICS
When carfilzomib is administered via intravenous (IV) infusion at the recommended starting dose of 20 mg/m2, the maximum plasma concentration (Cmax) is reached within minutes, and systemic exposure (area under the curve) is reached within less than one hour. At the recommended dose escalation of carfilzomib, it has been observed that the plasma concentration is dose-dependent.4,7 Carfilzomib penetrates all tissues extensively (excluding the brain). A dose of 20 mg/m2 on day 1 has demonstrated a mean volume of distribution of 28 L. Carfilzomib is highly protein-bound, approximating 97%.4,7
Carfilzomib is rapidly and extensively metabolized extra hepatically. The two main pathways of metabolism are peptidase cleavage and epoxide hydrolysis, demonstrating in active metabolites that were found to be peptide fragments and the diol metabolite of carfilzomib. The cytochrome P450 (CYP 450) metabolic system had minimal effect. Carfilzomib is rapidly eliminated by biliary and renal excretion with a half-life of less than one hour on day 1 of the recommended dose, resulting in less than 1% of the drug remaining intact. Within 24 hours, 25% of carfilzomib is excreted as the inactive metabolites.4,7,9
CLINICAL TRIALS
Phase 2 Monotherapy Trial
A phase 2, multicenter, open-label, single-arm study with 30 centers in the U.S. and Canada evaluated carfilzomib monotherapy in patients with relapsed or refractory MM. The study’s inclusion criteria are listed in Table 1.10
Table 1.
Patient Inclusion Criteria in Phase 2 Trial10
|
Carfilzomib was administered over two to 10 minutes on days 1, 2, 8, 9, 15, and 16 of each 28-day cycle for up to 12 cycles. Dosing of 20 mg/m2 was based on phase 1 studies. Response assessments were conducted on day 15 of cycle 1, on day 1 of cycles 2 to 12, and at the end of the study. The primary efficacy endpoint was overall response rate (ORR), including stringent complete response, complete response, very good partial response, and partial response (PR) based on study investigator assessments and subsequent adjudication by an independent review committee. Secondary endpoints included clinical benefit rate (CBR), duration of response (DOR), progression-free survival (PFS), and overall survival (OS). The study was deemed successful if the lower boundary of the two-sided 95% confidence interval (CI) about the ORR was more than 10%.10
From July 2008 to October 2009, 266 patients were enrolled in the study, with a data cutoff for analysis on February 11, 2011. Nine patients were excluded due to missing baseline and/or post-baseline disease assessment. The median patient age was 63 years and 58% were male. The MM diagnosis was a median of 5.4 years prior to study entry, and patients had received a median of five lines of therapy for MM, with 82% receiving more than four lines of therapy. Seventy-three percent of patients were refractory to bortezomib (Velcade, Millenium Pharmaceuticals) in any prior line, and 45% were refractory in their most recent line; 80% of patients (n = 214) were refractory to or intolerant of both bortezomib and lenalidomide.10
The median duration of carfilzomib treatment was three months, with 31% of patients completing more than six cycles and 12% continuing beyond 12 cycles in an extension protocol. Ninety-seven patients discontinued therapy due to progressive disease (59%) or adverse events (12%). The ORR was 23.7% and the CBR was 37%. As expected, the ORR in patients whose disease was refractory to bortezomib and/or lenalidomide was lower compared with those who were not refractory.10 In the 61 patients who achieved at least PR, the median DOR was 7.8 months, and was similar in those refractory to both bortezomib and lenalidomide.10
The mean dose per patient was 23.1 mg/m2 and the median dose was 23.5 mg/m2, with a median cumulative dose of 470 mg/m2 (range, 20–2,647 mg/m2). The most common treatment-emergent adverse events (AEs) were fatigue and anemia. The most common AEs of grade 3 or higher were fatigue and nausea. Of note, peripheral neuropathy was considered related to treatment in 8.3%. In comparison, up to 53% of patients receiving bortezomib and more than 70% of patients receiving thalidomide experience treatment-related peripheral neuropathy.10 It is believed that carfilzomib’s lack of neurodegeneration in vitro and lower neurotoxicity in animal studies bolster this clinical observation. This study concluded that treatment with carfilzomib produced clinically significant responses with an acceptable safety profile in heavily pretreated patients with relapsed and refractory MM.10
Phase 3 Combination Trial
Carfilzomib’s approval for use in patients with relapsed MM in combination with lenalidomide and dexamethasone was based on a phase 3, randomized, open-label, multicenter study.11 The trial evaluated the safety and efficacy of carfilzomib with lenalidomide and weekly dexamethasone compared with lenalidomide and weekly dexamethasone alone in patients with relapsed MM. The study was conducted from July 2010 through March 2012; 792 patients underwent randomization in North America, Europe, and the Middle East.11 Inclusion and exclusion criteria appear in Table 2.
Table 2.
Patient Selection Criteria in Phase 3 Trial11
Inclusion Criteria
|
Exclusion Criteria
|
The primary endpoint was PFS, and the secondary endpoints were OS, ORR, DOR, health-related quality of life, and safety. The endpoints were assessed in the intention-to-treat population. Safety was assessed in all patients who received at least one dose of study therapies: 392 patients in the carfilzomib group and 389 patients in the control group.11
Patients were randomly assigned in a 1:1 ratio to receive carfilzomib with lenalidomide and dexamethasone (the carfilzomib group) or lenalidomide and dexamethasone alone (the control group) within 28 days of therapy until disease progression, intolerable toxic effects, or withdrawal from the study. The phase 3 trial began with an initial dose of 20 mg/m2 and titrated the dose to 27 mg/m2. Patients were randomized based on previous therapy with bortezomib or lenalidomide and their B2 microglobulin level.11
Therapy in the carfilzomib group was conducted on days 1, 2, 8, 9, 15, and 16 of the 28-day cycle, with carfilzomib administered as a 10-minute infusion on two consecutive days. On days 1 and 2, carfilzomib was administered at 20 mg/m2, and the dose was escalated to reach 27 mg/m2 on days 15 and 16. During cycles 13 through 18, carfilzomib was administered only on days 1, 2, 15, and 16, and it was discontinued after 18 cycles. Lenalidomide was administered on days 1 through 21 as a 25-mg dose, and dexamethasone was administered on days 1, 8, 15, and 22 as a 40-mg dose. Adequate hydration was provided before and after cycle 1; subsequent cycles did not require pretreatment or post-treatment. Lenalidomide and dexamethasone therapy was continued beyond the 18th cycle if the patient experienced disease progression. Patients also received antiviral and antithrombotic prophylaxis.11
Disease progression or overall response to treatment was assessed on day 1 of every cycle according to the International Myeloma Working Group (IMWG) Uniform Response Criteria. Upon discontinuation or completion of the study, patients were observed every three months for up to one year, with follow-up every six months for survival data. Safety was assessed according to the National Cancer Institute Common Terminology Criteria for Adverse Events every 30 days from the last administered dose. Quality of life was measured using the European Organization for Research and Treatment of Cancer Quality of Life Core Module (QLQ-C30) questionnaire.11
The study met its objective primary endpoint of PFS with 431 events, demonstrating a median PFS of 26.3 months (95% CI, 23.3–30.5) in the carfilzomib group in comparison to 17.6 months (95% CI, 15.0–20.6) in the control group. In addition, it was determined that the hazard ratio (HR) for progression or death in the carfilzomib group was 0.69 (95% CI, 0.57–0.83; P = 0.0001). The benefit of carfilzomib in combination with lenalidomide and dexamethasone was observed among all subpopulations.11
OS was assessed according to a Kaplan-Meier graph demonstrating significant superiority in the carfilzomib group with a 73.3% rate (95% CI, 68.6–77.5) compared with a 65.0% rate (95% CI, 59.9–69.5) in the control group. The median follow-up periods were 32.3 months for the carfilzomib group and 31.5 months for the control group. The HR for death was 0.79 (95% CI, 0.63–0.99; P = 0.04), favoring carfilzomib.11
Further analysis demonstrated a complete response or greater in 31.8% of patients in the carfilzomib group and 9.3% of patients in the control group in the intention-to-treat population (P < 0.001). ORRs were 87.1% (95% CI, 83.4–90.3) and 66.7% (95% CI, 61.8–71.3), respectively (P < 0.001). Health-related quality of life was enhanced during the 18 cycles of treatment in the carfilzomib group (P < 0.001). The mean DOR was 28.6 months in the carfilzomib group with an average time to response of 1.6 months, compared with a 21.2-month DOR in the control group with an average time to response of 2.3 months.11 In the QLQ-C30 questionnaire used to measure patients’ quality of life, there was a five-point difference between the two groups, which is clinically of minimal impact. Changes of more than 20 points in the scores are correlated with greater toxicity, fatigue, and insomnia; however, quality-of-life score changes of 10 to 20 points are not associated with a negative effect on the quality of life.12
Initially, the study called for 526 events of disease progression or death to provide 90% power to determine a 25% reduction in these events. As of June 16, 2014, 305 deaths had occurred (approximately 60% of the specified 526 events required for the final analysis). An interim analysis was performed with a cutoff date of June 16, 2014. As of this date, 118 patients (29.8%) in the carfilzomib group and 86 patients (21.7%) in the control group were still receiving treatment.11
The median duration of treatment was approximately 88.0 weeks in the carfilzomib group and 57.0 weeks in the control group. AEs resulted in a carfilzomib dose reduction in 11% of patients and a lenalidomide dose reduction in 43.4% of patients in that group; in addition, 39.1% of patients in the control group experienced a lenalidomide dose reduction. The data showed that 69.9% of carfilzomib patients and 77.9% of control patients discontinued treatment due to disease progression (39.8% and 50.1%) or AEs (15.3% and 17.7%).11
There was a 5% increase in the incidence of common AEs such as hypokalemia, cough, upper respiratory tract infection, diarrhea, pyrexia, hypertension, thrombocytopenia, nasopharyngitis, and muscle spasms in patients in the carfilzomib group in comparison with the control group. AEs of grade 3 or higher were reported in 83.7% and 80.7% of patients in the two groups. AEs of particular interest, such as cardiac failure, were reported in 3.8% of patients in the carfilzomib group and 1.8% of patients in the control group, along with ischemic heart disease (3.3% versus 2.1%) and acute renal failure (3.3% versus 3.1%). Fourteen deaths (six in the carfilzomib group and eight in the control group) were attributed to treatment-related events, such as myocardial infarction, sepsis, and cardiac failure.11
SAFETY PROFILE
Adverse Events
Analysis of pooled monotherapy data yields a rate of serious AEs of 50%, irrespective of causality.4 The phase 3 trial provides data on AEs related to the use of carfilzomib in a combination treatment protocol. Table 3 provides a summary of important safety data from both monotherapy and combination therapy studies. AE data is mainly derived from those two clinical trials, although post-market reporting is beginning to produce new occurrences, including dehydration, tumor lysis syndrome (TLS), and posterior reversible encephalopathy syndrome (PRES).4
Table 3.
Carfilzomib Safety Data
| Adverse Event | Combination Data11 (%) | Monotherapy Data10 (%) |
|---|---|---|
| Incidence ≥ 10% | ||
| Anemia | 42.6 | 22 |
| Neutropenia | 37.8 | 15 |
| Thrombocytopenia | 29.1 | 29 |
| Fatigue | 32.9 | 37 |
| Diarrhea | 42.3 | 24 |
| Pyrexia | 28.6 | 15 |
| Hypokalemia | 27.6 | N/A |
| Hypertension | 14.3 | N/A |
| Incidence < 10% | ||
| Acute renal failure | 8.4 | 1.5 |
| Cardiac failure | 6.4 | 3.8 |
| Deep vein thrombosis | 6.6 | N/A |
| Hypophosphatemia | N/A | 7.1 |
Warnings and Precautions
The product labeling for carfilzomib includes warnings for several potential AEs, including cardiac toxicity, acute renal failure, TLS, pulmonary toxicity, dyspnea, pulmonary hypertension, hypertensive crisis, venous thrombosis, infusion reactions, thrombocytopenia, hepatic toxicity, thrombotic microangiopathy, PRES, and embryo-fetal toxicity.4
As of January 2016, no contraindications were listed in the product labeling.4
Use in Specific Populations
Pregnancy and Lactation
No data are available on the use of carfilzomib in pregnant or breastfeeding women. Doses administered to pregnant rats or rabbits were not found to be teratogenic. However, in rabbits, there was an increase in pre- and post-implantation loss (loss of embryos during the first trimester of pregnancy), an increase in fetal resorption causing early death to the embryo, and a decrease in fetal weight.
Based on evaluation of the animal studies, it is recommended that women use effective contraception at least two weeks prior to starting carfilzomib therapy and that they avoid breastfeeding due to potential AEs.4
Geriatric and Pediatric Use
Phase 3 clinical trials of carfilzomib in combination with lenalidomide and high-dose dexamethasone included 185 patients (46%) who were 65 years of age or older. A greater incidence of grade 3 or higher AEs was observed in patients at least 65 years of age (70%).4
No adequate studies have been conducted in pediatric patients.4
Renal and Hepatic Impairment
Carfilzomib was shown to have no effect on patients with mild, moderate, or severe renal impairment, so no dosing adjustments are needed. In phase 2 carfilzomib studies, patients receiving dialysis treatment were evaluated and no effects on baseline renal impairment were observed; however, it is recommended that the drug be administered after dialysis treatment due to the lack of data on the kinetics of carfilzomib after dialysis.4
Patients with hepatic impairment were not evaluated in the studies, so no conclusive evidence is available.
Cardiac Patients
Patients with recent myocardial infarctions or New York Heart Association Class III or IV heart failure were excluded from the clinical studies, so safety and efficacy data for this patient population are not available.4,7
Drug–Drug Interactions
Carfilzomib is metabolized primarily by peptidase and epoxide hydrolase activity. Thus, it is unlikely that drugs commonly processed through the CYP450 enzyme system will affect, or be affected by, carfilzomib pharmacokinetics.4
DOSAGE AND ADMINISTRATION
Kyprolis is packaged in single-use vials designed to provide 60 mg of carfilzomib at a concentration of 2 mg/mL after reconstitution. The reconstituted product is stable for 24 hours under refrigeration (2° to 8° C) and four hours at room temperature (15° to 30° C).4
In a combination regimen of carfilzomib, lenalidomide, and dexamethasone, carfilzomib is administered as a 10-minute IV infusion on two consecutive days per week for three weeks (on days 1, 2, 8, 9, 15, and 16), followed by a 12-day rest period. Each cycle is 28 days long. Cycle 1 dosing consists of carfilzomib 20 mg/m2 on days 1 and 2. If the patient tolerates week 1 dosing, an escalation to a target of 27 mg/m2 may be considered, starting on day 8 of cycle 1. Days 8 and 9 of carfilzomib should be discontinued at the onset of cycle 13, and complete discontinuation should follow cycle 18. Lenalidomide is dosed at 25 mg orally on days 1 to 21. Dexamethasone is dosed at 40 mg IV or orally on days 1, 8, 15, and 22 of each cycle.4
As an alternative dosing schedule in combination with dexamethasone, carfilzomib is administered as a 30-minute infusion on two consecutive days each week for three weeks followed by a 12-day rest period in a 28-day cycle. The carfilzomib dose is 20 mg/m2 on days 1 and 2 of cycle 1, and if tolerated, is escalated to 56 mg/m2 on day 8 of cycle 1. Dexamethasone 20 mg, oral or IV, is used on days 1, 2, 8, 9, 15, 16, 22, and 23 of each cycle. Dexamethasone is administered 30 minutes to four hours before carfilzomib.4
For relapsed refractory multiple myeloma as a single agent, carfilzomib may be administered as 10-minute or 30-minute infusions. The 10-minute infusion starts with 20 mg/m2 on days 1 and 2, then escalates to 27 mg/m2 on day 8 of cycle 1, if tolerated. The 30-minute infusion also begins with 20 mg/m2 on days 1 and 2, but escalates to 56 mg/m2 on day 8 of cycle 1, if tolerated. Carfilzomib monotherapy is administered on the same schedule as the combination regimen but may continue until disease progression or unacceptable toxicity occurs.4
Adequate hydration is required prior to the initiation of cycle 1, especially if the patient is identified as high risk for TLS or renal toxicity. Hydration may be continued as needed for subsequent cycles. Premedicating with dexamethasone to reduce infusion reactions is required 30 minutes to four hours prior to all carfilzomib doses in cycle 1. Dosing modifications are indicated in the presence of hematological and renal toxicities, in which case dosing is held until acceptable recovery of relevant biomarkers occurs.4
COST
Carfilzomib is supplied as a 60-mg single-use vial, which upon reconstitution yields a concentration of 2 mg/mL. The average wholesale price is $2,234. While the dose depends on body surface area, most patients will require the use of one vial (with any leftover portion discarded). With dosing of 20 mg/m2 on days 1 and 2, followed by titration to 27 mg/m2 for four more doses in cycle 1, six doses in cycles 2 to 13, and four doses in cycles 13 to 18, the cost of therapy would be approximately $214,464 for 72 weeks.13 This does not include coadministered medications.
P&T COMMITTEE CONSIDERATIONS
Carfilzomib is an FDA-approved agent indicated as either monotherapy or combination therapy with dexamethasone or with lenalidomide plus dexamethasone for the treatment of relapsed or refractory MM in patients who have received one to three lines of prior treatment.4 Clinical studies have evaluated the safety and efficacy of carfilzomib in comparison to standard treatment of care (lenalidomide with dexamethasone), demonstrating the significant benefit of carfilzomib in combination with lenalidomide and dexamethasone among all subpopulations.11 Carfilzomib is available as a 60-mg vial at a concentration of 2 mg/mL after reconstitution. The cost for carfilzomib therapy is comparable to current FDA-approved refractory lines of therapy.
Multiple myeloma is a progressive cancer for which there is no cure, and often patients experience periods of disease relapse. Based on clinical data and efficacy of carfilzomib, it is recommended that clinicians consider carfilzomib as a significant salvage therapy for refractory and relapsed MM patients.
CONCLUSION
Carfilzomib is an irreversible, selective proteasome inhibitor approved for the treatment of relapsed multiple myeloma in combination with lenalidomide and dexamethasone. This novel agent has shown positive efficacy and safety outcomes in phase 2 and 3 trials—despite disease refractory to such agents as bortezomib and lenalidomide. Although efficacy outcomes remain objectively low (spanning months), such results are relatively impressive given the fact that relapsed multiple myeloma is an incredibly difficult and deadly disease to manage, with low overall survival rates. As a robust salvage therapy option, carfilzomib offers improved survival outcomes and minimized safety risks for patients.
Footnotes
Disclosure: The authors report no commercial or financial interests in regard to this article.
REFERENCES
- 1.Kuehl MW, Bergsagel LP. Molecular pathogenesis of multiple myeloma and its premalignant precursor. J Clin Invest. 2012;122(10):3456–3463. doi: 10.1172/JCI61188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Rhee F, Anaissie E, Angtuaco E, et al. Chapter 109: Myeloma. In: Lichtman MA, Kipps TJ, Seligsohn U, et al., editors. Williams Hematology. 8th ed. New York, New York: McGraw-Hill; 2010. [Google Scholar]
- 3.National Cancer Institute, Surveillance Epidemiology, and End Results Program SEER cancer statistics review, 1975–2006. Available at: http://seer.cancer.gov/csr/1975_2006/results_merged/sect_18_myeloma.pdf. Accessed November 2, 2015.
- 4.Kyprolis (carfilozomib) prescribing information. Thousand Oaks, California: Amgen; Jan, 2016. [Google Scholar]
- 5.Food and Drug Administration Carfilzomib. Jul 20, 2012. Available at: www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm312945.htm. Accessed March 4, 2016.
- 6.Food and Drug Administration Carfilzomib/Kyprolis. Jul 24, 2015. www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm455873.htm. Accessed March 4, 2016.
- 7.Carfilzomib . Lexi-Drugs Online. Hudson, Ohio: Lexi-Comp, Inc.; Updated October 19, 2015. Available at: http://online.lexi.com. Accessed November 2, 2015. [Google Scholar]
- 8.Coux O, Tanaka K, Goldberg AL. Structure and functions of the 20S and 26S proteasomes. Annu Rev Biochem. 1996;65:801–47. doi: 10.1146/annurev.bi.65.070196.004101. [DOI] [PubMed] [Google Scholar]
- 9.Kortuem KM, Stewart AK. Carfilzomib. Blood. 2013;121(6):893–897. doi: 10.1182/blood-2012-10-459883. [DOI] [PubMed] [Google Scholar]
- 10.Siegel DS, Martin T, Wang M, et al. A phase 2 study of single-agent carfilzomib (PX-171-003-A1) in patients with relapsed and refractory multiple myeloma. Blood. 2012;120(14):2817–2825. doi: 10.1182/blood-2012-05-425934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stewart AK, Rajkumar SV, Dimopoulos MA, et al. Carfilzomib, lenalidomide, and dexamethasone for relapsed multiple myeloma. N Engl J Med. 2015;372(2):142–152. doi: 10.1056/NEJMoa1411321. [DOI] [PubMed] [Google Scholar]
- 12.Arraras Urdaniz JI, Vera García R, Martínez Aguillo M, et al. Quality of Life assessment through the EORTC questionnaires of colorectal cancer patients in advanced disease stages. Clin Transl Oncol. 2006;8(9):664–671. doi: 10.1007/s12094-006-0036-6. [DOI] [PubMed] [Google Scholar]
- 13.Red Book Online. Ann Arbor, Michigan: Truven Health Analytics; Accessed April 8, 2016. [Google Scholar]