INTRODUCTION
In the United States, colorectal cancer is the third most common malignancy in both men and women, following prostate and lung/bronchus cancer in men, and breast and lung/bronchus cancer in women.1 The American Cancer Society predicts that more than 130,000 new cases of colorectal cancer will be diagnosed in 2016 and that 49,000 people will die from the disease.1 Five-year survival rates for colorectal cancer diagnosed at the local stage are 90%, but that survival rate drops to 13% for those diagnosed with metastatic disease. Approximately 20% of patients are diagnosed at the metastatic stage. Among patients diagnosed at earlier stages, 50% to 60% eventually go on to develop colorectal metastases.2,3 Initial treatment usually involves a combination of surgery, radiation, and chemotherapy tailored to the characteristics of each patient’s disease.3
Fluoropyrimidine-based therapies have served as the backbone of colorectal cancer treatment for decades, and combination-based therapies with this drug class have led to significant reductions in mortality. Unfortunately, tumor cells can develop resistance to fluoropyrimidine-mediated damage, leaving clinicians with few options for heavily pretreated patients.4 The combination of trifluridine and tipiracil (TFD/TPI) has shown clinical activity in patients resistant to 5-flurorouracil (5-FU) and offers a viable alternative for pretreated individuals with metastatic colorectal cancer. Upon administration, the TFD component is incorporated directly into the replicating DNA strand, leading to tumor-cell damage, while the TPI component inhibits the secretion of angiogenic factors and endothelial cell growth.5–7
In September 2015, the Food and Drug Administration approved TFD/TPI (Lon-surf, Taiho Oncology, Inc.) for use in patients with metastatic colorectal cancer who have been treated with fluoropyrimi-dine-, oxaliplatin-, and irinotecan-based chemotherapy, an anti-vascular endothelial growth factor (VEGF) biological therapy, and—if RAS wild-type—an anti-epidermal growth factor receptor (EGFR) therapy.8,9
The only other medication with this indication is regorafenib (Stivarga, Bayer HealthCare), a tyrosine kinase inhibitor approved in September 2012.10,11
MECHANISM OF ACTION
TFD is a nucleoside analog; it is incorporated into replicating DNA strands, where it inhibits DNA synthesis and further cellular proliferation. TPI is an inhibitor of the enzyme thymidine phosphorylase, which is responsible for the breakdown of the active trifluridine component; thus, TPI boosts the levels of TFD. The two components are combined in a molar ratio of 1:0.5 in each formulation of TDF/TPI.9 In addition, thymidine phosphorylase promotes the migration of endothelial cells and angiogenesis in tumors. It has been suggested that the inhibition of this enzyme by TPI may also contribute to the latter’s antitumor activity.6,12
The chemical structures of TFD and TPI are shown in Figure 1.9
Figure 1.
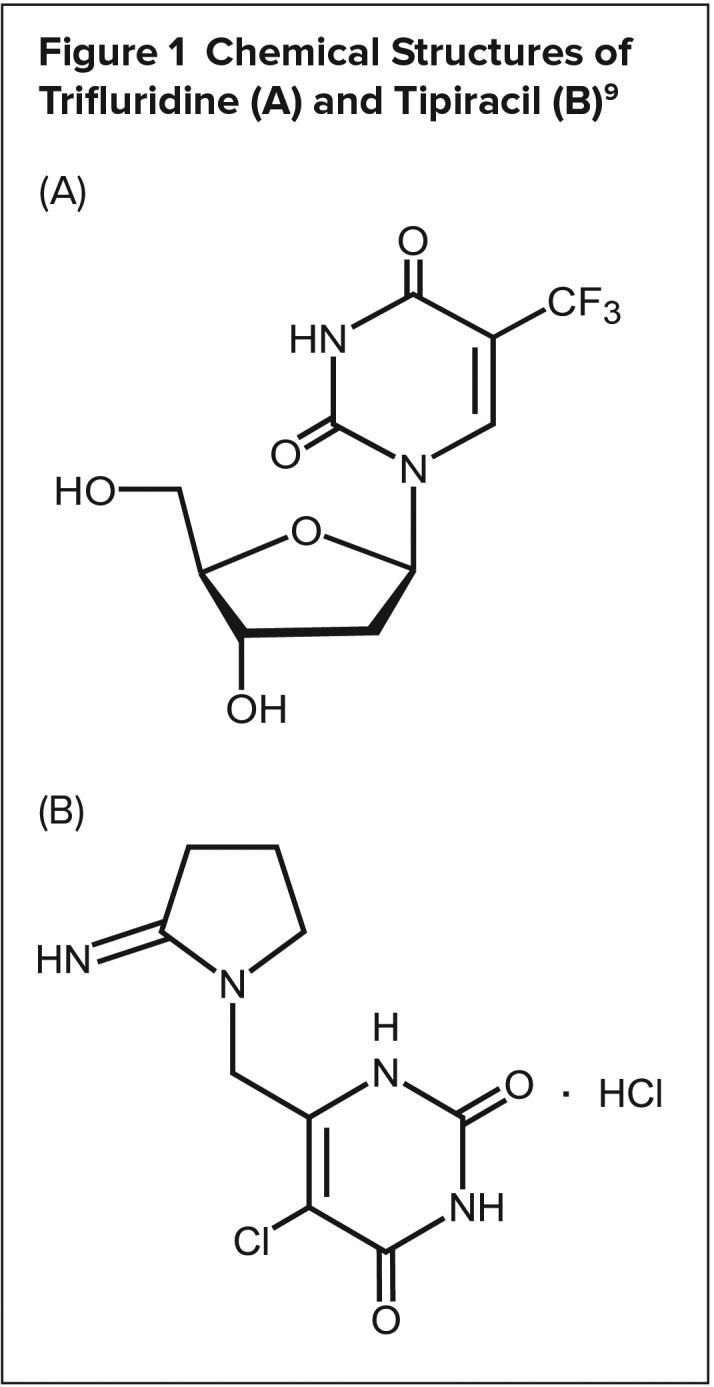
Chemical Structures of Trifluridine (A) and Tipiracil (B)9
PHARMACOKINETICS9
After twice-daily dosing of TFD/TPI, the systemic exposure (area under the concentration curve [AUC]) of TFD increased more than dose-proportionally over the dose range of 15 to 35 mg/m2. After the administration of TFD/TPI 35 mg/m2 twice daily, the mean elimination half-lives of TFD and TPI were 1.4 hours and 2.1 hours, respectively, after a single dose. The mean elimination half-lives at steady state of TFD and TPI were 2.1 hours and 2.4 hours, respectively. The accumulation of TFD was threefold for AUC0–last and twofold for the peak plasma concentration (Cmax) at steady state, whereas no accumulation was observed for TPI. The administration of a single dose of TFD/TPI 35 mg/m2 increased the mean AUC0–last of TFD by 37-fold and the Cmax by 22-fold compared with TFD 35 mg/m2 alone.
After a single oral administration of TFD/TPI 35 mg/m2 in cancer patients, the mean time to Cmax of TFD was approximately two hours. A standardized high-fat, high-calorie meal decreased TFD Cmax, TPI Cmax, and TPI AUC by approximately 40%, but did not change TFD AUC compared with those in a fasting state in cancer patients after the administration of a single dose of TFD/TPI 35 mg/m2.
TFD mainly binds to human serum albumin. The in vitro protein-binding of TFD in human plasma is greater than 96%, independent of the drug concentration and the presence of TPI. The plasma protein-binding of TPI is less than 8%. Neither TFD nor TPI is metabolized by cytochrome P450 enzymes. TFD is mainly eliminated by metabolism via thymidine phosphorylase to form an inactive metabolite, 5-(trifluoromethyl) uracil (FTY). No other major metabolites were detected in plasma or urine.
After a single dose of TFD/TPI 60 mg, the mean 48-hour cumulative urinary excretion was 1.5% for unchanged TFD, 19.2% for FTY, and 29.3% for unchanged TPI.
Renal Impairment
In a clinical study of TFD/TPI, the estimated mean AUC of TFD at steady state was 31% higher in patients with mild renal impairment (creatinine clearance [CrCl], 60 to 89 mL/min) and 43% higher in patients with moderate renal impairment (CrCl, 30 to 59 mL/min) than that in patients with normal renal function (CrCl greater than or equal to 90 mL/ min). The estimated mean AUC of TPI was 34% higher in patients with mild renal impairment and 65% higher in patients with moderate renal impairment than that in patients with normal renal function. The pharmacokinetics of TFD and TPI have not been studied in patients with severe renal impairment (CrCl less than 30 mL/min) or end-stage renal disease.
Hepatic Impairment
In a clinical trial of TFD/TPI, there was no clinically relevant effect of mild hepatic impairment (total bilirubin [TB] less than or equal to the upper limit of normal [ULN] and aspartate aminotransferase [AST] greater than the ULN, or TB less than 1.0 to 1.5 times the ULN and any AST) on the exposure of either TFD or TPI. Patients with moderate (TB greater than 1.5 to 3.0 times the ULN and any AST) or severe (TB greater than three times the ULN and any AST) hepatic impairment were not enrolled in the study. The pharmacokinetic characteristics of TFD and TPI have not been studied in patients with moderate-to-severe hepatic impairment.
CLINICAL TRIALS
Phase 1
Phase 1 studies were conducted to determine the appropriate maximum tolerated dose (MTD) and the dose-limiting toxicity of the TFD/TPI combination. These studies showed that TFD accumulates in the body as demonstrated by AUC observations after multiple doses, leading to increased rates of neutropenia. It was determined that a 14-day pause between doses allowed safe dosing. Other phase 1 studies evaluated the optimal dosing regimen for TFD/TPI. In a study of American and Japanese subjects, TFD/TPI administered twice daily on days 1 to 5 and 8 to 12 every four weeks resulted in an MTD of 70 mg/m2 per day and a disease control rate of 62% (16 of 26 subjects).13
Phase 2
A phase 2, multicenter, double-blind, randomized trial conducted in Japan compared TFD/TPI (35 mg/m2 administered twice daily on days 1 to 5 and 8 to 12 every four weeks) with placebo in 169 patients with metastatic colorectal cancer. All of the patients were older than 20 years of age; had previously received standard chemotherapy treatment with two or more regimens; and were refractory to or intolerant of fluoropyrimidine, irinotecan, and oxaliplatin. The patients received TFD/TPI until tumor progression, unacceptable toxicity, or withdrawal of consent occurred. The study’s primary endpoint was overall survival (OS) in the intention-to-treat population. Secondary endpoints included progression-free survival (PFS); the objective response (OR); the disease control rate (DCR; a complete or partial response plus stable disease more than six weeks after the initiation of study treatment); the duration of response (the time between a patient first achieving a complete or partial response and disease progression); the time to treatment failure; efficacy in patients with or without Kirsten rat sarcoma viral oncogene homolog (KRAS) mutations; and adverse events.14
The patients receiving TFD/TPI showed increased OS, PFS, and DCR compared with the placebo-treated patients. These results are listed in Table 1. Beneficial effects of TFD/TPI were also seen in patients with KRAS mutations. The effect of TFD/TPI on OS was greater in the mutant KRAS population (hazard ratio [HR], 0.44; 95% confidence interval [CI], 0.25–0.80). However, in patients with KRAS wild-type, median OS was 7.2 months (95% CI, 6.1–10.3) in those given TFD/TPI and 7.0 months (95% CI, 3.4–9.4) in those given placebo (P = 0.191). A major limitation of this study was that more than 40% of the patients in both groups received treatment after the trial. Therefore, the patients may not have been truly refractory to other agents.14
Table 1.
Efficacy of Trifluridine/Tipiracil Versus Placebo
| Phase 2 Study14 | Phase 3 Study15 | |
|---|---|---|
| Number of participants | TFD/TPI: n = 112 Placebo: n = 57 |
TFD/TPI: n = 534 Placebo: n = 266 |
| Median OS, months | 9.0 vs. 6.6 HR, 0.56; 95% CI, 0.39–0.81; P = 0.0011 |
7.1 vs. 5.3 HR, 0.68; 95% CI, 0.58–0.81; P < 0.001 |
| Median PFS, months | 2.0 vs. 1.0 HR, 0.41; 95% CI, 0.28–0.59; P < 0.0001 |
2.0 vs. 1.7 HR, 0.48; 95% CI, 0.41–0.57; P < 0.001 |
| Disease control rate, n (%)* | 49 (43) vs. 6 (11) P < 0.001 |
221 (44) vs. 42 (16) P < 0.001 |
| Response rate (%)† | NR | 1.6 vs. 0.4 P = 0.29 |
| Median time to treatment failure, months | 1.9 vs. 1.0 HR, 0.40; 95% CI, 0.28–0.56; P < 0.001 |
NR |
NR = not reported; OS = overall survival; PFS = progression-free survival; TFD/TPI = trifluridine/tipiracil.
A complete or partial response or stable disease more than 6 weeks from the initiation of study treatment.
The proportion of patients whose best response was a complete or partial response.
Phase 3
Mayer and colleagues conducted a pivotal phase 3 study (RECOURSE) to evaluate the efficacy and safety of TFD/ TPI compared with that of placebo in a large international population. The study enrolled 800 patients 18 years of age and older who had received at least two standard chemotherapy treatments, had tumor progression within three months after the last dose, and had received prior treatment with fluoropyrimidine, oxaliplatin, irinotecan, bevacizumab, and cetuximab or pantiumumab (if KRAS wild-type). The study’s primary endpoint was OS, and secondary endpoints included PFS, the response rate (complete or partial response), DCR (complete or partial response or stable disease at least six weeks after randomization), and adverse events.15
The patients’ median age was 63 years; most were white and were from the United States, Europe, and Australia; 79% were randomly assigned to treatment more than 18 months after their diagnosis of metastases; 60% had tried four or more prior regimens; and 51% had a KRAS mutation. The study’s outcomes are listed in Table 1. TFD/TPI achieved improvements in OS, median PFS, and DCR. In addition, the median time to worsening of performance status, as measured with the Eastern Cooperative Oncology Group scale, was 5.7 months for TFD/TPI compared with 4.0 months for placebo (HR, 0.66; 95% CI, 0.56–0.78; P < 0.001). The effects on PFS were the same for KRAS wild-type patients and those with KRAS mutations; however, there was a greater effect on OS in patients with KRAS wild-type disease compared with those with KRAS mutations (HR, 0.58 versus 0.80, respectively). This was the opposite of what had occurred in the phase 2 trial, where a greater effect on OS was observed in mutant KRAS patients.15
SAFETY PROFILE
Adverse Events
Data from the phase 2 and phase 3 trials of TFD/TPI showed that the treatment is fairly well tolerated.14,15 Grade-3 or greater adverse events occurred in 69% of the treatment group and in 52% of the placebo group. The rates of serious adverse events were similar for the two groups: 30% versus 34%. The main dose-limiting toxicity was neutropenia, with 50% of patients experiencing grade-3 or higher involvement. Despite the high rate of neutropenia, only 4% of patients in both studies developed febrile neutropenia. In addition, only 4% of patients discontinued treatment because of toxic effects. Among patients who received at least two cycles of TFD/ TPI, 14% required dose reductions and 53% had a delay of four days or more because of toxicity when beginning the next cycle. The phase 3 trial also showed that there was no difference between the two groups in the development of stomatitis, hand-foot syndrome, or cardiac events.15 However, there was a higher incidence of infection in the TFD/TPI group compared with the placebo group (27% versus 15%, respectively), with the most common infections being nasopharyngitis and urinary tract infections.9 Patients receiving TFD/TPI experienced higher rates of pulmonary embolism compared with placebo-treated patients (2% versus 0%, respectively) and interstitial lung disease (0.2% versus 0%). Adverse events are listed in Table 2.
Table 2.
Safety of Trifluridine/Tipiracil Versus Placebo*
| Phase 2 Study14 | Phase 3 Study15 | |||
|---|---|---|---|---|
| Any Grade (%) | Grade ≥ 3 (%) | Any Grade (%) | Grade ≥ 3 (%) | |
| Serious adverse drug event | 19 vs. 9 | N/A | 30 vs. 34 | N/A |
| Hematological | ||||
| Neutropenia | 72 vs. 2 | 50 vs. 0 | 67 vs. < 1 | 38 vs. 0 |
| Leukopenia | 76 vs. 4 | 28 vs. 0 | 77 vs. 5 | 21 vs. 0 |
| Anemia | 73 vs. 16 | 17 vs. 5 | 77 vs. 33 | 18 vs. 3 |
| Thrombocytopenia | 39 vs. 2 | 4 vs. 0 | 42 vs. 8 | 5 vs. < 1 |
| Nonhematological | ||||
| Fatigue | 58 vs. 42 | 6 vs. 4 | 35 vs. 23 | 4 vs. 6 |
| Diarrhea | 38 vs. 21 | 6 vs. 0 | 32 vs. 12 | 3 vs. < 1 |
| Nausea | 65 vs. 28 | 4 vs. 0 | 48 vs. 24 | 2 vs. 1 |
| Anorexia | 62 vs. 33 | 4 vs. 4 | 39 vs. 29 | 4 vs. 5 |
| Febrile neutropenia | 4 vs. 0 | 4 vs. 0 | 4 vs. 0 | 4 vs. 0 |
| Vomiting | 34 vs. 25 | 4 vs. 0 | 28 vs. 14 | 2 vs. < 1 |
| Abdominal pain | NR | NR | 21 vs. 18 | 2 vs. 4 |
| Fever | NR | NR | 19 vs. 14 | 1 vs. < 1 |
| Alopecia | NR | NR | 7 vs. 1 | NR |
| Other Laboratory Abnormalities | ||||
| Increase in alanine transaminase | NR | NR | 24 vs. 27 | 2 vs. 4 |
| Increase in aspartate aminotransferase | NR | NR | 30 vs. 35 | 4 vs. 6 |
| Increase in total bilirubin | NR | NR | 36 vs. 26 | 9 vs. 12 |
| Increase in alkaline phosphatase level | NR | NR | 39 vs. 45 | 8 vs. 11 |
| Increase in creatinine | NR | NR | 13 vs. 12 | < 1 vs. < 1 |
NR = not reported.
Note: Data presented as percent (%) treatment group versus percent (%) placebo group
Warnings and Precautions
In the phase 2 trial, TFD/TPI caused severe (grade 3 or 4) myelosuppression, including neutropenia, anemia, thrombocytopenia, and febrile neutropenia. In the phase 3 trial, 9% of patients in the TFD/ TPI group received granulocyte colony-stimulating factors. In the event of grade-4 neutropenia, febrile neutropenia, or platelet counts of less than 50,000/mm3, clinicians should hold the current dose of TFD/TPI and resume at a lower dose upon resolution of the adverse event. In addition, based on findings of embryo-fetal toxicity after the administration of TFD/TPI in animal studies, the use of effective contraception during treatment is recommended.9
Use in Specific Populations
Pregnancy and Lactation9
Although no data are available on the use of TFD/TPI in pregnant women, animal studies showed potential risks to the fetus, including decreased fetal weight, embryo-fetal lethality, and structural anomalies at low doses. Because of these findings, pregnant women should be advised about potential fetal risks. In addition, TFD and TPI or their metabolites were observed in the breast milk of nursing rats. It is recommended that women stop breastfeeding during treatment with TFD/TPI and for one day after the last dose.
Given the risk of fetal harm during treatment with TFD/TPI, women of reproductive potential should be counseled on proper contraception during therapy. It is also recommended that men receiving TFD/TPI wear condoms during sexual intercourse for at least three months after their final dose if their partners are of childbearing potential.
Geriatric and Pediatric Use9
In clinical trials, 44% of patients receiving TFD/TPI were 65 years of age or older, and 7% were 75 years of age or older. There was no difference in efficacy between these age groups and younger patients. However, patients 65 years of age and older were at greater risk than younger patients for grade-3 or grade-4 neutropenia (48% versus 30%, respectively), grade-3 anemia (26% versus 12%), and grade-3 or grade-4 thrombocytopenia (9% versus 2%).
The safety and efficacy of TFD/TPI have not been established in pediatric patients.
Hepatic Impairment9
No studies of TFD/TPI have been conducted in patients with hepatic impairment. However, dosage adjustments are not required in patients with mild impairment, defined as total bilirubin levels less than or equal to the ULN and AST levels greater than the ULN, or total bilirubin of 1.0 to 1.5 times the ULN with any AST. Patients with moderate or severe hepatic impairment were not enrolled in clinical studies of TFD/TPI.
Renal Impairment9
The effects of renal impairment on the pharmacokinetics of TFD/TPI have not been determined. In clinical trials, there was a difference of at least 5% in the rates of grade-3 or higher adverse events, serious adverse events, and dose delays and reductions in patients with moderate renal impairment (CrCl, 30 to 59 mL/min) compared with patients with mild renal impairment (CrCl, 60 to 89 mL/min) or normal renal function. While no dosage adjustments of TFD/TPI are currently recommended for patients with renal dysfunction, those with moderate disease may require changes in dose based on toxicity.
Drug–Drug Interactions9
Pharmacokinetic drug–drug interaction studies have not been conducted for TFD/TPI, but it is known that the two components are not metabolized by cytochrome P450 (CYP) enzymes. In vitro, TFD and TPI do not inhibit CYP enzymes and do not induce CYP1A2, CYP2B6, or CYP3A4/5. Other studies have shown that TFD is not a substrate for human uptake and efflux transporters and does not inhibit them.
DOSAGE AND ADMINISTRATION9
The recommended oral dosage of TFD/TPI is 35 mg/m2 (based on the TFD component) twice a day within one hour of finishing the morning and evening meals. The maximum recommended dose is 80 mg. Doses are to be rounded to the nearest 5-mg increment. TFD/TPI is administered in 28-day cycles, with the patient receiving doses on days 1 through 5 and on days 8 through 12 of each cycle. TFD/TPI is supplied as a film-coated tablet that should be stored in its original packaging. The drug should be discarded after 30 days if it is stored outside its original container.
A complete blood count is recommended before starting treatment with TFD/TPI and on day 15 of each cycle. Treatment should not be initiated if a patient’s absolute neutrophil count (ANC) is less than 1,500 cells/mm3, platelets are less than 75,000/mm3, or the patient has active febrile neutropenia or any grade-3 or grade-4 nonhematological reactions that have not resolved to grade 1. TFD/TPI should be withheld if the patient develops an ANC of less than 500 cells/mm3, platelets less than 50,000/mm3, or any grade-3 or grade-4 reactions during a treatment cycle. A dose reduction of 5 mg/m2 is recommended if a patient develops febrile neutropenia, grade-4 neutropenia, or thrombocytopenia resulting in more than a one-week delay for the next cycle, or nonhematologic grade-3 or grade-4 reactions that cannot be controlled by supportive therapy, such as antiemetic or antidiarrheal medications. There can be a maximum of three dose reductions to a minimum dose of 20 mg/m2.
COST
The average wholesale price (AWP) of a single tablet of the 15/6.14-mg formulation of TFD/TPI is $164; for the 20/8.18-mg tablet, the AWP is $219. Multiple package sizes of 20, 40, and 60 tablets are available. For an average-sized patient (5 feet, 6 inches tall; 150 pounds; and a body surface area of 1.81 m2) the standard dosage of TFD/TPI (based on the TFD component) would be 63 mg (rounded up to 65 mg) twice daily for 10 days of a 28-day cycle. This would result in an AWP drug cost of $14,232 for 60 of the 15/6.14-mg tablets and 20 of the 20/8.18-mg tablets.16 Taiho Oncology offers a support program for patients who may have difficulty paying for the therapy.17
P&T COMMITTEE CONSIDERATIONS
Compared with the only other therapy that shares TFD/TPI’s indication— regorafinib10—TFD/TPI may represent not only a more-tolerable approach but also a slightly less-expensive one. Currently, the AWP for a 28-day supply of regorafenib 160 mg is $15,896 compared with approximately $14,200 for TFD/TPI for the same length of treatment.16 In addition, TFD/TPI has more-favorable safety and tolerability profiles compared with regorafenib, considering the latter drug’s association with hand-and-foot skin reactions, diarrhea, mucositis, and potentially fatal hepatotoxicity.10
CONCLUSION
TFD/TPI offers clinicians a new therapeutic option for heavily pretreated patients with metastatic colorectal cancer. The TFD component inhibits DNA synthesis in cancer cells, blocking further cellular proliferation. At the same time, the TPI component inhibits thymidine phosphorylase, which is responsible for the breakdown of TFD, thus boosting TFD levels.9 The recommended dosage is 35 mg/m2 (based on the TFD component) twice a day (within one hour after the morning and evening meals) on days 1 through 5 and days 8 through 12 of each 28-day cycle.9 The AWP of a 28-day supply of tablets is approximately $14,200, which translates to an annual cost of approximately $185,000.16
Footnotes
Disclosure: The authors report no commercial or financial interests in regard to this article.
REFERENCES
- 1.American Cancer Society . Cancer Facts & Figures 2016. Atlanta, Georgia: American Cancer Society; 2016. Available at: www.cancer.org/acs/groups/content/@research/documents/document/acspc-047079.pdf. Accessed March 22, 2016. [Google Scholar]
- 2.National Cancer Institute, Surveillance, Epidemiology, and End Results Program SEER stat fact sheets: colon and rectum cancer. Available at: http://seer.cancer.gov/statfacts/html/colorect.html. Accessed March 24, 2016.
- 3.National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN Guidelines), Colon Cancer, Version 2.2015. Available at: www.tri-kobe.org/nccn/guideline/colorectal/english/colon.pdf. Accessed February 13, 2016.
- 4.Longley DB, Harken DP, Johnston PG. 5-fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003;3(5):330–338. doi: 10.1038/nrc1074. [DOI] [PubMed] [Google Scholar]
- 5.Bijnsdorp IV, Peters GJ, Temmink OH, et al. Differential activation of cell death and autophagy results in an increased cytotoxic potential for trifluorothymidine compared to 5-fluorouracil in colon cancer cells. Int J Cancer. 2010;126(10):2457–2468. doi: 10.1002/ijc.24943. [DOI] [PubMed] [Google Scholar]
- 6.Hotchkiss KA, Ashton AW, Schwartz EL. Thymidine phosphorylase and 2-deoxy-ribose stimulate human endothelial cell migration by specific activation of the integrins alpha 5 beta 1 and alpha V beta 3. J Biol Chem. 2003;278(21):19272–19279. doi: 10.1074/jbc.M212670200. [DOI] [PubMed] [Google Scholar]
- 7.Matsushita S, Nitanda T, Furukawa T, et al. The effect of a thymidine phosphorylase inhibitor on angiogenesis and apoptosis in tumors. Cancer Res. 1999;59(8):1911–1916. [PubMed] [Google Scholar]
- 8.Food and Drug Administration FDA approves new oral medication to treat patients with advanced colorectal cancer. Sep 22, 2015. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm463650.htm. Accessed February 9 2016.
- 9.Lonsurf (trifluridine and tipiracil) prescribing information. Princeton, New Jersey: Taiho Pharmaceutical Co., Ltd.; Sep, 2015. Available at: www.taihooncology.com/us/prescribinginformation.pdf. Accessed March 22, 2016. [Google Scholar]
- 10.Stivarga (regorafenib) prescribing information. Wayne, New Jersey: Bayer HealthCare Pharmaceuticals Inc.; Sep, 2012. Available at: www.accessdata.fda.gov/drugsatfda_docs/label/2012/203085lbl.pdf. Accessed March 24, 2016. [Google Scholar]
- 11.Food and Drug Administration FDA approves new treatment for colorectal cancer. Sep 27, 2012. Available at: www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm321271.htm. Accessed March 24, 2016.
- 12.Peters GJ, Bijnsdorp IV. TAS-102: more than an antimetabolite. Lancet Oncol. 2012;13(12):e518–519. doi: 10.1016/S1470-2045(12)70426-6. [DOI] [PubMed] [Google Scholar]
- 13.Salvatore L, Rosssini D, Moretto R, et al. TAS-102 for the treatment of metastatic colorectal cancer. Expert Rev Anticancer Ther. 2015;15:1283–1292. doi: 10.1586/14737140.2015.1105746. [DOI] [PubMed] [Google Scholar]
- 14.Yoshino T, Mizunuma N, Yamazaki K, et al. TAS-102 monotherapy for pretreated metastatic colorectal cancer: a double-blind, randomised, placebo-controlled phase 2 trial. Lancet Oncol. 2012;13(10):993–1001. doi: 10.1016/S1470-2045(12)70345-5. [DOI] [PubMed] [Google Scholar]
- 15.Mayer RJ, Van Cutsem E, Falcone A, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015;372(20):1909–1919. doi: 10.1056/NEJMoa1414325. [DOI] [PubMed] [Google Scholar]
- 16.Red Book Online. Ann Arbor, Michigan: Truven Health Analytics; Available at: www.micromedexsolutions.com. Accessed April 8, 2016. [Google Scholar]
- 17.Taiho Oncology Taiho Oncology patient support. Sep 29, 2015. Available at: www.taihopatientsupport.com. Accessed April 11, 2016.


