Abstract
Aims: Alcoholics Anonymous (AA) is the most prevalent 12-step mutual-help organization (MHO), yet debate has persisted clinically regarding whether patients whose primary substance is not alcohol should be referred to AA. Narcotics Anonymous (NA) was created as a more specific fit to enhance recovery from drug addiction; however, compared with AA, NA meetings are not as ubiquitous. Little is known about the effects of a mismatch between individuals' primary substance and MHOs, and whether any incongruence might result in a lower likelihood of continuation and benefit. More research would inform clinical recommendations. Method: Young adults (N = 279, M age 20.4, SD 1.6, 27% female; 95% White) in a treatment effectiveness study completed assessments at intake, and 3, 6, and 12 months post-treatment. A matching variable was created for ‘primary drug’ patients (i.e. those reporting cannabis, opiates or stimulants as primary substance; n = 198/279), reflecting the proportion of total 12-step meetings attended that were AA. Hierarchical linear models (HLMs) tested this variable's effects on future 12-step participation and percent days abstinent (PDA). Results: The majority of meetings attended by both alcohol and drug patients was AA. Drug patients attending proportionately more AA than NA meetings (i.e. mismatched) were no different than those who were better matched to NA with respect to future 12-step participation or PDA. Conclusion: Drug patients may be at no greater risk of discontinuation or diminished recovery benefit from participation in AA relative to NA. Findings may boost clinical confidence in making AA referrals for drug patients when NA is less available.
INTRODUCTION
In most developed nations, substance use disorder (SUD) is a highly prevalent health condition that exacts an enormous burden on public health and safety (Bouchery et al., 2011). While many individuals suffering from SUD achieve remission without formal interventions (Sobell et al., 1996, 2000; Cunningham, 1999; Cunningham et al., 2000; Substance Abuse and Mental Health Services Administration, 2013a), those with more severe and complex forms of the illness typically seek assistance from professional treatment. Also, because more severe forms of SUD often have a chronic, relapsing-remitting nature, providing some form of ongoing monitoring and recovery management has shown to be effective and cost-effective (Godley et al., 2007; White, 2008; Kelly and White, 2011; Dennis and Scott, 2012; McCollister et al., 2013). The high cost burden associated with long-term professional recovery management for alcohol and other drug addiction, however, along with increasing incentives for health care agencies to use more cost-efficient resources to help people achieve and sustain SUD remission, has promoted stronger clinical linkage to effective low-cost or freely available community mutual aid resources and has become a recent focus of the UK addiction treatment strategy (Hacker and Walker, 2013; Maust et al., 2013; Public Health England, 2013). In the addiction treatment field, promising results have been found in this regard related to the use of recovery-focused mutual-help organizations (MHOs). Several prospective studies, for example, have shown that clinically facilitating use of 12-step MHOs, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), following treatment, produces higher rates of SUD remission (Kelly, 2003; Moos and Moos, 2004; Kaskutas, 2009; Kelly and Yeterian, 2012) and simultaneous reductions in health care costs (Humphreys and Moos, 1996, 2001, 2007; Mundt et al., 2012).
Of the numerous 12-step MHOs available [e.g. AA, NA, Cocaine Anonymous (CA), Marijuana Anonymous (MA), etc.] designed to assist with recovery from the various types of psychoactive SUDs from which people suffer (e.g. alcohol, cannabis, opiate, stimulant use disorders) AA and NA are by far the largest (Kelly and Yeterian, 2013). Beginning in the 1930s, AA was the first 12-step MHO and focuses specifically on recovery from alcohol dependence (alcoholism). In the USA, AA operates through ∼60,000 weekly groups (Alcoholics Anonymous, 2012). NA, in contrast, emerged later in the 1950s and focuses mostly on recovery from other, largely illicit, SUDs (e.g. opiates, stimulants or cannabis), although NA does address alcohol dependence too (Narcotics Anonymous, 1988).
NA currently has ∼20,000 groups operating weekly in the USA (Narcotics Anonymous, 2010). Although there is substantial overlap in the substance-specific co-morbidities of both organizational memberships (i.e. a large proportion of AA members have other drug problems, and NA members, alcohol problems), in keeping with their names and original raison d'etre, there is a relative emphasis on recovery from specific substances, particularly in AA, regarding alcohol (AA's ‘singleness of purpose’; Alcoholics Anonymous, 2001). This substance-specific focus is intended to promote greater therapeutic benefit via stronger identification resulting in tighter group cohesion and a deeper sense of universality. It also fosters efficient communication of successful recovery strategies that are intimately tied to the distinctive characteristics associated with the use of and recovery from that particular substance (e.g. its pharmacology, withdrawal, and post-acute withdrawal profiles) as well as its sub-cultural context (e.g. legality, cultural stigma, availability) (Alcoholics Anonymous, 1953). Because of the lower availability of NA compared with AA meetings, however, especially in suburban or rural communities, many with primary drug problems other than alcohol, may find it more difficult to access NA meetings, despite them being potentially more relevant and closely matched to their specific addiction histories, experiences and recovery preferences. A question that has lingered, therefore, is whether individuals whose primary drug is not alcohol would attend, become engaged and derive as much benefit from 12-step MHOs if they attended more ubiquitous AA, rather than less available NA, meetings. This question is particularly pertinent to young adults who comprise a substantial proportion of SUD treatment admissions (SAMHSA TEDS 2013) and, compared with older adults, are less likely to report alcohol as their primary substance (Substance Abuse and Mental Health Services Administration, 2013b).
Although many people seeking SUD recovery, as well as referring clinicians, ponder this question, and, in general, we have found in prior work that young adults participate in and benefit from 12-step MHO participation (Kelly et al., 2013), very little is known empirically about the effects of a potential match/mismatch between individuals' primary substance and the specific 12-step MHO they attend. Specifically, it is unclear whether any incongruence might result in more rapid discontinuation and less recovery benefit (perhaps via a lowered sense of universality, cohesion, and identification and reduced exposure to substance-specific recovery skills that many deem so helpful in their 12-step experience; Kelly et al., 2008, 2010a; Labbe et al., 2014). Furthermore, because most prior research has combined AA and NA into a single metric assessing mutual-help participation, little is known descriptively regarding the extent to which patients with different primary SUDs attend and become involved in AA vs. NA following treatment.
To help bridge these knowledge gaps, the current study addresses three specific research questions: (a) Do young adults who report either alcohol, cannabis, opiates, or stimulants, as their primary substance attend 12-step MHOs, and AA and NA specifically, at different rates in the year following residential treatment? (b) Among young adults who report either cannabis, opiates, or stimulants, as their primary substance (‘primary drug patients’), does proportionately greater attendance at AA rather than NA in the first 3 months post-treatment (a theoretical mismatch) result in subsequently lowered rates of attendance and involvement at 6 and 12 month follow-ups? And, (c) Among primary drug patients does proportionately greater attendance at AA during the first 3 months post-discharge result in less subsequent recovery benefit (abstinent days) at 6- and 12-month follow-ups?
If it is found that primary drug patients attending the ostensibly more fitting NA fellowship are more likely to continue to participate and to derive greater benefit, then it would provide support for more targeted and explicit clinical facilitation to NA rather than AA. If, on the other hand, primary drug patients who attend proportionately more AA meetings, because they are more widely available, are found to be at no greater risk of subsequent 12-step discontinuation or diminished recovery benefit, then clinicians could more confidently recommend and facilitate patient linkage to AA if, by chance, NA was unavailable or less available in patients' home areas.
METHODS
Participants
Participants were 279 young adults (18–24 years old) undergoing residential treatment in Minnesota in the USA and enrolled in an observational study of treatment process and outcome. At admission, participants were 20.4 years old on average (SD = 1.6). Most were Caucasian (95.0%) and male (73.4%), while all were single (100%). At admission, 40.6% were employed and 32.5% were students. Most had completed high school: 42.7% had a high school diploma and 39.2% had some college education. Participants in this private treatment sample were more likely to be Caucasian than young adults (18–24 years old) in public sector residential treatment (76%) (Substance Abuse and Mental Health Services Administration, 2009). They were, however, comparable in terms of gender, marital status and employment status, suggesting that results are broadly generalizable to youth treated for substance-related disorders in the USA.
Treatment
Treatment was comprehensive and multi-faceted, based in a 12-step philosophy of recovery. In addition to the 12-step orientation, motivational enhancement and cognitive-behavioral therapeutic approaches, as well as family therapy, were used to facilitate problem recognition, increase treatment engagement and to support recovery. Programming included clinical assessment, individual and group therapy, and a host of specialty groups tailored to meet the needs of individual clients. Integrated mental health care was available, including clinical assessment, psychotherapy and medication management. Participants' average length of stay was 25.7 days (SD = 5.6, ranging = 4–35 days). The majority (83.9%) were discharged with staff approval, indicating a high rate of treatment completion.
Procedure
Participants were enrolled in the study shortly after admission. A total of 607 young adults were admitted to treatment during the recruitment period (10/2006 to 3/2008). All of those aged 21–24 years old were approached for study enrollment, as well as every second individual aged 18–20. This was done to ensure sufficient representation of the older age group, given the predominance of those aged 18–20 at the treatment center. Of those approached (n = 384), 64 declined or withdrew participation. Following enrollment, an additional 17 participants withdrew prior to the baseline assessment and the consent for one participant was misplaced. The final sample of 302 represents 78.6% of those approached for participation. To focus on this study's primary research questions, we excluded individuals who did not report a primary substance of choice (n = 3), reported more than one primary substance (n = 5), or reported a primary substance that was not alcohol, cannabis, opiates or stimulants (n = 15), which resulted in a final sample of 279.
Research staff conducted assessments at baseline, 3, 6 and 12 months post-discharge. Each assessment included an interview portion, completed either in person or by telephone, and self-administered surveys, which were returned by mail. Participants were reimbursed $30 for the baseline assessment and $30, $40 and $50 for the post-treatment assessments at 3, 6 and 12 months, respectively. Assessment completion rates were 81.2, 72.7 and 71.0% at the 3-, 6- and 12-month follow-ups, respectively. At each time point, those who did not complete the assessment were compared with those who were retained in terms of gender, age, race, education, employment status, and baseline psychological symptoms (BSI), dependence severity (LDQ) and percent days of abstinence in the 90 days prior to treatment (α = 0.05). Relative to those with post-secondary education, those with a high school education or less were more likely to be missed at all time points.
The study was conducted in accordance with the Institutional Review Board at Schulmann Associates IRB, an independent review board, and all participants signed informed consent documents.
Measures
Background sociodemographic information, including age, gender, marital status, race and ethnicity, employment status, educational attainment, and student status, was obtained with participants’ full permission, from their medical records.
Structured Clinical Interview for DSM-IV-TR
The Structured Clinical Interview for DSM-IV-TR (SCID) (First et al., 2002) was conducted by trained personnel at baseline to assess SUD diagnoses. To ensure inter-rater reliability and protocol fidelity, supervisory reviews of audio-taped SCID interviews were conducted on all assessments during the first month of data collection and for two randomly chosen interviews each week thereafter.
Leeds Dependence Questionnaire
The Leeds Dependence Questionnaire (LDQ) is a brief, 10-item self-report measure of dependence severity that is not specific to particular substances. Likert Scale responses are summed to provide a total score out of 30, with higher scores indicating greater dependence severity. The measure has shown high internal consistency (α = 0.93) and good construct validity in the present sample (Kelly et al., 2010b), and in other adult and youth samples (Raistrick et al., 1994; Lennings, 1999).
Form-90
The Form-90 (Project MATCH Research Group, 1993; Miller and Del Boca, 1994) is an interview measure capturing substance use in the past 90 days. Modifications were made to subsequent assessments to capture the time period elapsed since previous interview (i.e. averaging 90 days for the 3- and 6-month follow-ups, and 180 days for the 12-month follow-up). Patients' primary substance (aka ‘drug of choice’) and the primary outcome in the current study, percentage of days abstinent (PDA) from all substances except nicotine, were both derived from this instrument. The Form-90 has been tested with adult and adolescent samples and has demonstrated reliability and validity (Tonigan et al., 1997; Slesnick and Tonigan, 2004).
Inventory of Drug Use Consequences—Recent Consequences (InDUC-2R)
The InDUC-2R is a 50-item self-report measure assessing consequences of alcohol and/or drug use. Items are rated in terms of their frequency of occurrence in the past 90 days, from never (0) to daily or almost daily (3) and are summed to provide a total score. The InDUC-2R has demonstrated sensitivity to changes in consequences over a 3-month period (Tonigan and Miller, 2002). Reliability in the current sample was very high (Cronbach's α = 0.95).
Multidimensional Mutual Help Activity Scale
This interview-based index assesses several dimensions of involvement in 12-step MHOs. Responses for each item are provided separately for AA and NA. Items tap frequency of attendance (which was also divided by total days in the follow-up assessment to create percent days attending a meeting), as well as level of active 12-step involvement which was measured by the total sum of 8 dichotomized activities, such as contact with sponsor and other members, step work, reading 12-step literature, and speaking at meetings). As with the Form-90, interviews captured the entire time period elapsed since the previous interview. Analysis of this measure in this same sample of young adults has shown high content validity and reliability (Kelly et al., 2011).
Biological assay
To verify self-reported abstinence from alcohol and other drugs, saliva tests (Cone et al., 2002) were administered on a subsample of subjects that lived within 50 miles of the treatment facility and could attend follow-up interviews in-person. Abstinence was confirmed in 99.6–100% of subjects who self-reported abstinence from all substances during the assessment period prior to each follow-up. Positive tests results were obtained for one subject who reported abstinence prior to the 3-month follow-up and this person was not included in the analysis.
Data analysis plan
We divided the sample into four groups based on patients' reported primary substance: alcohol, cannabis, opiates or stimulants. To compare between-group differences at baseline we used one-way ANOVA's and Chi-square tests. Significant between-group differences were further characterized using post hoc Tukey tests (continuous variables) and contrast statements in logistic regression models (categorical variables). We also compared number of meetings attended for each of AA and NA as a function of primary substance using the Kruskal–Wallis test. To account for multiple comparisons, we adjusted all post hoc tests using a Bonferroni correction. We then examined the effect of primary substance on 12-step attendance and involvement with hierarchical linear models (HLM) using Proc Mixed. To determine whether the trajectories in attendance and involvement differed across time between groups, we added in a group by time interaction term.
To evaluate the relative benefit of 12-step fellowship matching, we first combined the cannabis, opiate and stimulant groups to create a ‘primary drug group’. Next, within this group, we divided the number of AA meetings attended by total 12-step meetings attended, to produce a variable the reflected the proportion of 12-step attendance that was theoretically ‘mismatched’, with higher proportions ostensibly indicating poorer matching of the primary drug group to AA. Using this variable, we constructed HLMs that tested the effect of this matching and the interaction between matching and time on subsequent 12-step attendance and involvement over the 12-month follow-up period among the primary drug patients only.
Lastly, to investigate the effect of fellowship mismatch among the primary drug group on substance use outcomes we used two HLMs which regressed percent days abstinent (PDA) on fellowship mismatch, attendance or involvement, and the interaction between fellowship match and attendance or involvement. In all HLM models, we controlled for predictors of attrition (education) and baseline levels of the dependent variable (e.g. 12-step attendance, 12-step involvement, percent days abstinent), respectively. To adhere to models' statistical assumptions, we transformed PDA using a negative log transformation. Appropriate covariance structures were selected using the likelihood ratio test. All analyses were generated using SAS Version 9.2.
RESULTS
Baseline differences
A comparison of baseline characteristics by primary substance revealed several significant demographic and clinical differences (Table 1). Stimulant patients were significantly younger than alcohol and opiate patients. Cannabis patients were more likely than alcohol or opiate patients to be male. Similarly, opiate patients were more likely to be male than alcohol patients. With respect to clinical characteristics, opiate and stimulant patients presented to treatment with more severe clinical profiles. Specifically, opiate and stimulant patients had lower PDA than alcohol patients, more substance use consequences than cannabis patients, and greater dependence severity than both alcohol and cannabis patients. Stimulant patients also reported more substance use consequences than alcohol patients. As expected, participants were more likely to meet DSM-IV abuse or dependence criteria for their respective primary substance relative to other primary substance groups with one exception. That is, the prevalence of cocaine use disorder did not differ significantly between opiate and stimulant groups; however, it approached significance (P = 0.059) such that a greater proportion of the stimulant group (78.85 vs. 62.50%; Table 1) met relevant criteria. When considering other drug use disorders, alcohol patients were less likely than all other groups to meet criteria for a hallucinogen use disorder and also less likely than opiate and stimulant groups to meet criteria for polysubstance dependence. Similarly, cannabis patients were less likely than stimulant patients to meet criteria for polysubstance dependence. Among patients with primary drug use disorders, 65% (128/198) also met for DSM-IV alcohol abuse or dependence. In addition, all primary drug patients had used alcohol to some degree in the past 3 months prior to treatment entry.
Table 1.
Demographic and pre-treatment characteristics by primary substance (n = 279)
| Alcohol (n = 81) | Cannabis (n = 81) | Opiates (n = 65) | Stimulants (n = 52) | F/χ2 | P | |
|---|---|---|---|---|---|---|
| Demographic | ||||||
| Age | 20.74 ± 1.66a | 20.12 ± 1.50 | 20.66 ± 1.54a | 19.85 ± 1.42b,c | 5.01 | 0.002 |
| Male | 51 (62.96)c,d | 70 (86.42)a,b | 51 (78.46)b | 34 (65.38)d | 14.24 | 0.003 |
| White | 76 (93.83) | 76 (93.83) | 63 (96.92) | 50 (96.15) | 1.12 | 0.773 |
| At least some college | 37 (45.68) | 28 (34.57) | 31 (47.69) | 18 (35.29) | 4.01 | 0.261 |
| Employed | 19 (36.54) | 19 (38.00) | 20 (41.67) | 17 (48.57) | 1.44 | 0.696 |
| Clinical | ||||||
| Percent days abstinent | 35.19 ± 28.42b,c | 24.55 ± 32.14 | 18.15 ± 23.13b | 18.08 ± 23.81b | 6.08 | 0.001 |
| Substance use consequences | 62.41 ± 22.63a | 56.27 ± 25.34a,c | 71.11 ± 22.52d | 76.90 ± 24.32b,d | 9.64 | 0.000 |
| Dependence severity | 16.38 ± 7.61a,c | 14.14 ± 8.29a,c | 21.89 ± 6.68b,d | 21.20 ± 7.79b,d | 16.56 | 0.000 |
| 12-step attendance | 32 (39.51) | 21 (25.93)c | 31 (47.69)a,d | 15 (28.85)c | 9.04 | 0.029 |
| 12-step involvement | 1.53 ± 2.07 | 0.99 ± 1.83 | 1.92 ± 2.31 | 1.40 ± 2.16 | 2.50 | 0.060 |
| Substance use disorders (lifetime) | ||||||
| Alcohol | 80 (98.77)a,c,d | 50 (62.50)a,b | 36 (56.25)a,b | 42 (80.77)b,c,d | 44.09 | 0.000 |
| Cannabis | 43 (53.75)a,d | 74 (92.50)a,b,c | 41 (64.06)d | 41 (78.85)b,d | 33.17 | 0.000 |
| Cocaine | 28 (34.57)a,c | 21 (26.25)a,c | 40 (62.50)b,d | 41 (78.85)b,d | 46.20 | 0.000 |
| Opiate | 8 (9.88)a,c | 11 (13.75)a,c | 57 (89.06)a,b,d | 17 (32.69)b,c,d | 122.87 | 0.000 |
| Anxiolytic | 10 (12.35) | 9 (11.25) | 13 (20.31) | 8 (15.38) | 2.77 | 0.428 |
| Amphetamine | 16 (19.75)a | 12 (15.00)a | 11 (17.19)a | 23 (44.23)b,c,d | 18.11 | 0.000 |
| Hallucinogenic | 3 (3.70)a,c,d | 14 (17.50)b | 13 (20.31)b | 9 (17.31)b | 10.49 | 0.015 |
| Polysubstance | 3 (3.70)a,c | 6 (7.50)a | 10 (15.63)b | 13 (25.00)b,d | 16.41 | 0.001 |
aSignificantly different from stimulant group.
bSignificantly different from alcohol group.
cSignificantly different from opiate group.
dSignificantly different from cannabis group.
Do individuals who report either alcohol, cannabis, opiates, or stimulants, as their primary substance attend 12-step MHOs, and AA and NA specifically, at different rates in the year following residential treatment?
Table 2 describes the mean and median number of meetings attended at each time point by primary substance.
Table 2.
Number of meetings attended at baseline, 3, 6 and 12 months stratified by primary substance
| Fellowship | Average number of meetings attended* |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Alcohol |
Cannabis |
Opiates |
Stimulants |
χ2 | P | |||||
| Mean ± SD | Median | Mean ± SD | Median | Mean ± SD | Median | Mean ± SD | Median | |||
| Any fellowship | ||||||||||
| Baseline | 7.25 ± 17.66 | 0.00 | 5.25 ± 14.71 | 0.00a | 10.95 ± 20.95 | 0.00b | 7.63 ± 19.74 | 0.00 | 8.59 | 0.035 |
| 3 months | 30.66 ± 27.29 | 28.00 | 24.06 ± 20.19 | 21.00 | 29.98 ± 25.24 | 25.00 | 33.44 ± 30.99 | 27.00 | 1.99 | 0.575 |
| 6 months | 31.66 ± 34.80 | 25.50 | 29.66 ± 32.28 | 20.50c | 42.49 ± 34.11 | 39.00 | 53.24 ± 45.58 | 45.50b | 11.30 | 0.010 |
| 12 months | 50.05 ± 50.67 | 31.50 | 46.48 ± 52.24 | 27.50 | 65.63 ± 56.06 | 60.00 | 76.65 ± 86.20 | 58.00 | 4.82 | 0.186 |
| Alcoholics Anonymous | ||||||||||
| Baseline | 6.84 ± 16.62 | 0.00 | 3.64 ± 10.99 | 0.00a | 7.89 ± 16.65 | 0.00b | 5.15 ± 14.78 | 0.00 | 11.48 | 0.009 |
| 3 months | 27.44 ± 24.98 | 23.00 | 18.24 ± 16.18 | 16.00 | 24.46 ± 23.16 | 19.00 | 26.22 ± 27.45 | 20.00 | 3.89 | 0.274 |
| 6 months | 28.53 ± 32.23 | 20.50 | 25.66 ± 28.45 | 18.00 | 32.32 ± 31.80 | 24.00 | 42.12 ± 43.98 | 37.50 | 3.42 | 0.331 |
| 12 months | 46.94 ± 50.05 | 27.50 | 42.00 ± 51.51 | 18.00 | 42.83 ± 45.43 | 28.00 | 61.57 ± 78.49 | 40.00 | 1.30 | 0.728 |
| Narcotics Anonymous | ||||||||||
| Baseline | 0.41 ± 2.07 | 0.00a | 1.60 ± 4.84 | 0.00 | 3.06 ± 9.84 | 0.00d | 2.48 ± 7.77 | 0.00 | 13.80 | 0.003 |
| 3 months | 3.17 ± 5.95 | 0.00 | 5.82 ± 10.67 | 0.50 | 5.53 ± 9.30 | 0.00 | 7.22 ± 11.93 | 3.00 | 4.28 | 0.233 |
| 6 months | 3.13 ± 9.98 | 0.00a,c | 4.00 ± 8.75 | 0.00 | 10.83 ± 20.48 | 0.00d | 11.12 ± 21.71 | 0.00d | 14.90 | 0.002 |
| 12 months | 3.11 ± 12.38 | 0.00a | 4.48 ± 11.39 | 0.00 | 22.80 ± 50.19 | 0.00d | 15.08 ± 36.53 | 0.00 | 15.54 | 0.001 |
aSignificantly different from opiate group.
bSignificantly different from cannabis group.
cSignificantly different from stimulant group.
dSignificantly different from alcohol group.
*Comparisons of number of meetings attended were conducted using the non-parametric Kruskal–Wallis Test.
Attendance at 12-step mutual help organizations
There were between-group differences found at baseline and 6 months post-treatment. At baseline, opiate patients attended more total 12-step meetings than cannabis patients on average. At 6 months, stimulant patients attended more total 12-step meetings than cannabis patients on average. There were no other significant group differences as a function of overall 12-step attendance.
Attendance at AA
There were only differences in average number of AA meetings attended at baseline such that opiate patients reported attending significantly more AA meetings than cannabis patients. There were no other significant group differences.
Attendance at NA
Significant between-group differences in the average number of NA meetings attended were observed at baseline, 6-, and 12-month follow-ups. As expected, opiate patients reported attending significantly more NA meetings than alcohol patients at baseline, 6-month and 12-month follow-ups. Also at 6 months, stimulant patients reported significantly more NA meetings than alcohol patients.
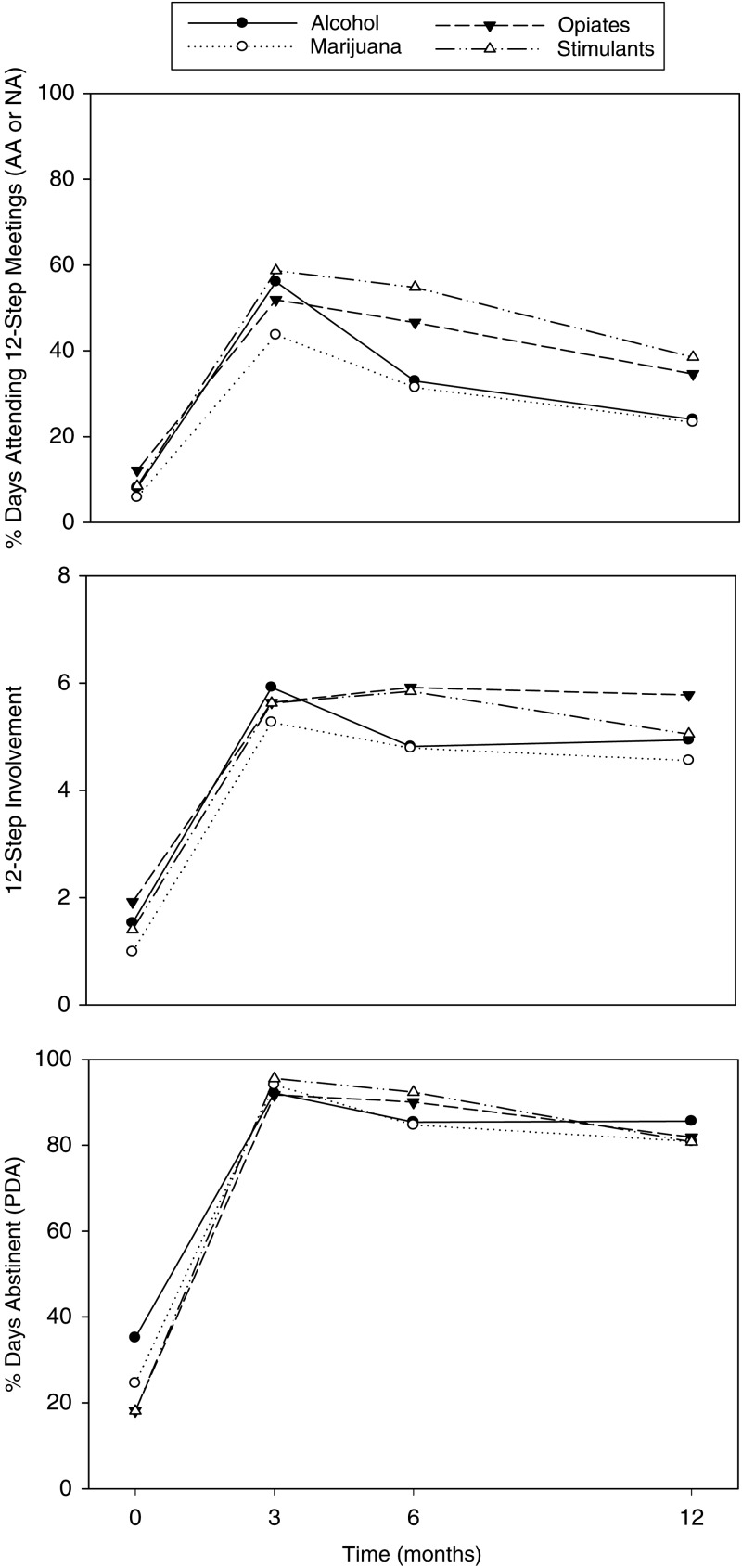
12-step Attendance, involvement and PDA by primary substance
HLMs examining differences between the four primary substance groups and 12-step attendance, involvement, and PDA over time revealed several significant effects. There was a significant main effect for stimulant patients suggesting they had greater percent days attending a 12-step meeting than alcohol patients. There were no significant main effects for either cannabis or opiate groups suggesting their attendance over time did not differ from that of alcohol patients. There were also no significant group by time interactions suggesting that 12-step attendance trajectories were similar between each of the drug groups relative to the alcohol group. Furthermore, separate HLMs also showed that there were no significant effects for any of the drug groups for either 12-step involvement or PDA during the follow-up period, suggesting they were similar to the alcohol group (Fig. 1). Moreover, there were no significant group by time interactions in the 12-step involvement or PDA models, suggesting their trajectories over time for each of the drug groups were also similar to that of the alcohol group. In each of the HLMs, there was an effect of ‘time’, such that 12-step attendance, involvement and PDA decreased significantly over the follow-up period (Table 3 and Fig. 1).
Fig. 1.
Relationship between primary substance and 12-step attendance, involvement, and PDA across time.
Table 3.
Relationship between primary substance and 12-step attendance, involvement, and percent days abstinent over time (3, 6 and 12 months)
| Independent variable | Attendance |
Involvement |
Percent days abstinent |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | F | P | β | SE | F | P | β | SE | F | P | |
| Education | 0.086 | 0.038 | 5.15 | 0.024 | 0.193 | 0.324 | 0.35 | 0.553 | 0.182 | 0.167 | 1.20 | 0.275 |
| Baseline DV | 0.084 | 0.030 | 7.55 | 0.007 | 0.214 | 0.077 | 7.77 | 0.006 | 0.350 | 0.295 | 1.41 | 0.236 |
| Time (months) | −0.025 | 0.003 | 64.83 | 0.000 | −0.083 | 0.024 | 12.42 | 0.001 | −0.076 | 0.012 | 38.47 | 0.000 |
| Cannabis Group | −0.018 | 0.049 | 0.14 | 0.711 | −0.403 | 0.425 | 0.90 | 0.343 | 0.203 | 0.218 | 0.87 | 0.353 |
| Opiate Group | 0.067 | 0.051 | 1.69 | 0.194 | 0.055 | 0.434 | 0.02 | 0.899 | 0.116 | 0.228 | 0.26 | 0.611 |
| Stimulant Group | 0.141 | 0.056 | 6.34 | 0.013 | −0.073 | 0.480 | 0.02 | 0.880 | 0.289 | 0.251 | 1.33 | 0.251 |
There were no significant drug of choice group × time interactions. For each effect of primary substance shown, primary alcohol was the reference group.
Among primary drug patients (i.e. patients reporting either cannabis, opiates or stimulants as their primary substance), does proportionately greater attendance at AA rather than NA (‘fellowship mismatch’) in the first 3 months post-treatment result in subsequently lowered rates of attendance and involvement at 6- and 12-month follow-ups?
As noted previously, the three primary drug groups (cannabis, opiates, stimulants) were combined to form the ‘primary drug’ group. The proportion of meetings attended by the primary drug group that were AA ranged from an average of 69.9% at baseline to 79.4% at 6 months (Fig. 2). Fellowship mismatch among primary drug patients (greater percentage of meetings attended that were AA) was unrelated to subsequent 12-step attendance or involvement over the follow-up period. Furthermore, there was no interaction between time and fellowship mismatch suggesting that primary drug patients' attendance and involvement over time did not depend on whether they attended a greater proportion of AA than NA meetings during the first 3 months post-discharge (Table 4 and Fig. 2).
Fig. 2.
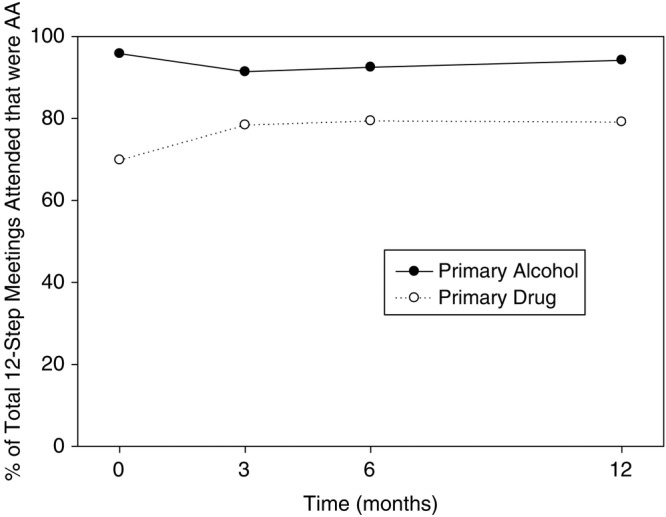
The proportion of 12-step meeting attended by ‘primary alcohol’ and ‘primary drug’ patients that were Alcoholics Anonymous.
Table 4.
Time-lagged effects of fellowship matching at 3 months among participants reporting either cannabis, opiates or stimulants as their reported primary substance (‘primary drug’ group) on attendance and involvement at 6 and 12 months
| Independent variable | Attendance |
Involvement |
||||||
|---|---|---|---|---|---|---|---|---|
| β | SE | F | P | β | SE | F | P | |
| Education | 0.110 | 0.057 | 3.68 | 0.058 | 0.688 | 0.412 | 2.79 | 0.097 |
| Baseline attendance/involvement | 0.069 | 0.044 | 2.43 | 0.122 | 0.136 | 0.092 | 2.19 | 0.141 |
| Time (months) | −0.006 | 0.019 | 0.10 | 0.758 | −0.050 | 0.147 | 0.12 | 0.735 |
| Fellowship mismatch* | 0.280 | 0.234 | 1.43 | 0.234 | 0.749 | 1.565 | 0.23 | 0.633 |
| Time × fellowship mismatch* | −0.023 | 0.022 | 1.04 | 0.310 | −0.058 | 0.176 | 0.11 | 0.742 |
*‘Fellowship mismatch’ indicates the proportion of all 12-step meetings that primary drug patients attended that were AA.
Among primary drug patients does proportionately greater attendance at AA rather than NA (‘fellowship mismatch’) during the first 3 months post-discharge result in less subsequent recovery benefit (i.e. PDA) at 6- and 12-month follow-ups?
Results from the HLM evaluating the effect of fellowship mismatch and the interaction between fellowship mismatch and attendance/involvement during follow-up showed that fellowship mismatch was unrelated to subsequent PDA. Apart from the effect of time, the main effects of attendance and involvement were significant predictors of PDA. Non-significant interactions with fellowship mismatch suggest these 12-step attendance/involvement effects did not differ based on the degree to which primary drug patients attended AA rather than NA, a potentially more complementary fit given their primary substance. Consistent with previous research, the strongest predictors of PDA in this sample were attendance, involvement and time (Table 5).
Table 5.
The effect of fellowship mismatch at 3 months among participants reporting either cannabis, opiates or stimulants as their primary substance (‘primary drug’ group) on percent days abstinent (PDA) at 6 and 12 months controlling for attendance/involvement
| Attendance/involvement only |
Attendance and matching |
Interaction |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | F | P | β | SE | F | P | β | SE | F | P | |
| Attendance | ||||||||||||
| Education | 0.044 | 0.240 | 0.03 | 0.854 | 0.036 | 0.243 | 0.02 | 0.882 | 0.057 | 0.245 | 0.05 | 0.816 |
| Baseline PDA | 0.224 | 0.415 | 0.29 | 0.590 | 0.363 | 0.412 | 0.77 | 0.381 | 0.372 | 0.414 | 0.81 | 0.370 |
| Time (months) | −0.088 | 0.022 | 16.83 | 0.000 | −0.097 | 0.023 | 17.61 | 0.000 | −0.096 | 0.023 | 17.54 | 0.000 |
| Attendance | 1.054 | 0.304 | 12.03 | 0.001 | 0.488 | 0.325 | 2.25 | 0.136 | 1.127 | 1.125 | 1.00 | 0.318 |
| Fellowship mismatcha | 0.388 | 0.454 | 0.73 | 0.393 | 0.757 | 0.765 | 0.98 | 0.324 | ||||
| Attendance × fellowship mismatcha | −0.772 | 1.297 | 0.35 | 0.553 | ||||||||
| Involvement | ||||||||||||
| Education | 0.066 | 0.217 | 0.09 | 0.763 | 0.014 | 0.230 | 0.00 | 0.952 | 0.006 | 0.232 | 0.00 | 0.981 |
| Baseline PDA | 0.374 | 0.381 | 0.96 | 0.328 | 0.418 | 0.392 | 1.14 | 0.289 | 0.422 | 0.394 | 1.15 | 0.287 |
| Time (months) | −0.088 | 0.021 | 16.83 | 0.000 | −0.096 | 0.023 | 17.68 | 0.000 | −0.097 | 0.023 | 17.71 | 0.000 |
| Involvement | 0.284 | 0.045 | 40.57 | 0.000 | 0.247 | 0.063 | 15.28 | 0.000 | 0.209 | 0.182 | 1.31 | 0.255 |
| Fellowship mismatcha | 0.392 | 0.432 | 0.82 | 0.367 | 0.111 | 1.317 | 0.01 | 0.933 | ||||
| Involvement × fellowship mismatcha | 0.049 | 0.216 | 0.05 | 0.822 | ||||||||
a‘Fellowship mismatch’ indicates the proportion of all 12-step meetings that primary drug patients attended that were AA.
DISCUSSION
This study found that the rates of 12-step attendance and involvement in the sample differed somewhat depending on patients’ reported primary substance at intake. In contrast to patients reporting alcohol as their primary substance, those who identified another drug as primary (i.e. either cannabis, opiates or stimulants) attended significantly more NA than AA meetings over the follow-up period. Yet, during the critical early post-treatment phase (1–3 months) primary drug patients attended AA more frequently than NA. While this presented a conceivable early mismatch between their primary substance and AA's alcohol-specific recovery emphasis, the mismatch was not associated with subsequently lower rates of 12-step attendance or involvement nor less derived recovery benefit in terms of abstinence. Since NA is generally less available, especially in smaller communities, findings offer hope for those suffering from a broad range of SUDs as well as for referring programs and clinicians, since primary drug patients may benefit just as much from attending AA if NA meetings are inaccessible in the communities in which they live.
Differences in 12-step participation over the study period
In general, where there were differences detected in 12-step participation at baseline and over the year-long follow-up, opiate and stimulant patients tended to go to more meetings and more NA meetings, specifically, relative to alcohol and cannabis patients. The more frequent attendance in general may reflect these patients' greater addiction severity and more serious clinical profile that was observed at treatment entry. Greater addiction severity has shown to be the most robust predictor of 12-step participation (Kelly, 2003), and although not measured directly in this study, this greater degree of substance-related impairment may have resulted in greater perceived severity of the disorder which is a key mechanism of help-seeking among those with SUD (Finney and Moos, 1995). The more frequent attendance at NA among primary opiate and stimulant patients also may indicate a stronger desire to affiliate with a 12-step fellowship that contains individuals with more similar substance-specific experiences that might increase a sense of belonging and identification, and instill hope for successful recovery (Labbe et al., 2014). With regard to PDA, noteworthy too, was that the different primary substance groups, did not differ significantly. Consequently, it is plausible that aspects of the treatment and 12-step MHO participation experience may have helped partially offset a potentially worse outcome associated with a more severe clinical profile at treatment entry.
The influence of an early post-treatment mismatch between primary drug patients and AA vs. NA on subsequent 12-step participation and abstinence
Of the 12-step meetings attended in the first 3 months post-discharge, nearly all the meetings attended by the primary alcohol patients were AA (96%). A large proportion of the meetings attended by the primary drug patients, however, were also AA (79%). We cannot determine for sure why primary drug patients attended so many AA instead of the presumably more fitting, NA meetings, but one explanation may be that it is because NA meetings were comparatively less available, as noted previously. Consequently, rather than not attend any meetings, these patients may have chosen to attend AA. This apparent mismatch, however, did not appear to lead to disillusionment as it was unrelated to subsequent 12-step participation at either the 6-month or 12-month follow-up nor was it associated with less benefit in terms of PDA at the later follow-ups relative to primary drug patients who were better matched to NA. As we have found previously with this sample, 12-step MHO participation was a strong and independent predictor of better outcomes (Kelly et al., 2013). Consequently, 12-step participation, in general, can aid youth recovery efforts and, despite less supposed similarity between primary drug patients and the explicit AA emphasis on alcohol, participation in the AA fellowship does not appear to result in less benefit nor increase the likelihood of future MHO dropout.
AA groups can vary considerably in their dynamics (Montgomery et al., 1993) and interpersonal climate (Rynes et al., 2013). Anecdotally, AA meetings can vary also in the degree to which they may embrace individuals whose primary substance and experience may be unrelated to alcohol, and some may be particularly welcoming of young members new to sobriety. It is possible that at least some primary drug patients may have selected AA groups that were more welcoming and accommodating of drug-specific differences. It is also true that, similar to the national US treatment population, patients in this sample with primary drug problems also had significant alcohol problems and the majority of patients in each primary substance group met criteria for co-occurring alcohol abuse or dependence. This was particularly true of primary stimulant patients (81%). Also, all patients were using alcohol to varying degrees prior to treatment admission (not shown). Furthermore, while from the inside of these fellowships drug specificity may seem important to group unity (Alcoholics Anonymous, 1953), from a scientific and clinical standpoint the essential features of addiction (e.g. compulsive use, craving, impaired control, continued use despite harmful consequences) are common across all psychoactive substances. Thus, conceivably, although not fitting perfectly with their primary drug preference and related addiction experience, individuals with primarily illicit drug problems would, nevertheless, share common ground with a more alcohol-specific focus given their level of alcohol involvement and prevalence of DSM-IV alcohol abuse or dependence as well as broad shared addiction phenomenology (Alcoholics Anonymous, 1953).
LIMITATIONS
Generalizations from the findings in this study should be considered in light of some important limitations. The sample comes from a 12-step oriented residential treatment program which strongly encouraged 12-step MHO participation following treatment and was based in large part on 12-step philosophy. Consequently, it is unclear whether the relationships observed here would be found among patients treated in treatments with different theoretical orientations. Also, the sample here was comprised of young adults and, given that this is the first study to examine this mismatching phenomenon empirically, we do not know how results found here will compare to older adults or adolescents. However, relative to older adults, young adults are less likely to have alcohol as their primary substance, increasing the significance of this investigation in this population. Sample characteristics, too, should be considered, since the patients in the current sample were mostly white and male. We had considered whether a lack of power might have played a role in non-detection of potentially significant relationships (i.e. a type II error), but given that we had 198 individuals who reported their primary substance as cannabis, opiates or stimulants, and also used a continuous, instead of a dichotomous, variable for fellowship matching (i.e. the proportion of meetings attended that were AA among the primary drug group), thereby further increasing sensitivity to detect an effect, we do not think the lack of statistical significance can be attributed to type II errors.
CONCLUSIONS
A common concern among treatment programs and clinicians is whether patients who report a primary drug other than alcohol should be recommended to attend more common AA meetings when NA or other 12-step MHOs that ostensibly may be a better fit with their drug-specific experiences and recovery preferences, are less available. This is a particularly salient issue for young adults since, compared with older adults, fewer young adults report alcohol as their primary substance (Substance Abuse and Mental Health Services Administration, 2013b). Findings here suggest that, while primary drug patients may attend more NA meetings post-treatment compared with primary alcohol patients in absolute terms, they attend proportionately more AA meetings. The specific fellowship of NA developed to provide a forum to facilitate similarity in experience that could enhance identification and maximize therapeutic benefit through sharing of specific recovery experiences. This in theory should provide greater benefit when primary drug patients attend NA as opposed to AA. We did not find evidence that a greater match between individuals' primary substance and fellowship bears any influence on future 12-step participation or abstinence. Findings suggest, that contrary to expectation, young adults who identify cannabis, opiates or stimulants as their preferred substance may, in general, do as well in AA as NA. This has significance in many communities where NA meetings may be less available or unavailable.
Funding
This research was supported by grant funding from the National Institute of Alcohol Abuse and Alcoholism (R21AA018185-02) and by anonymous donations to the Hazelden Foundation. This work is solely the responsibility of the authors and the funding agencies had no role in the conception or execution of this work nor in the report presented here.
Conflict of interest statement
None declared.
REFERENCES
- Alcoholics Anonymous. Twelve Steps and Twelve Traditions. New York: Alcoholics Anonymous World Services; 1953. [Google Scholar]
- Alcoholics Anonymous. Alcoholics Anonymous: The Story of How Thousands of Men and Women Have Recovered from Alcoholism Alcoholics Anonymous World Services. New York, NY: 2001. [Google Scholar]
- Alcoholics Anonymous. Alcoholics Anonymous 2011 Membership Survey. New York: Alcoholics Anonymous World Services; 2012. [Google Scholar]
- Bouchery E, Harwood HJ, Sacks JJ, et al. Economic costs of excessive alcohol consumption in the U.S., 2006. Am J Prev Med. 2011;41:516–24. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Cone EJ, Presley L, Lehrer M, et al. Oral fluid testing for drugs of abuse: positive prevalence rates by Intercept immunoassay screening and GC-MS-MS confirmation and suggested cutoff concentrations. J Anal Toxicol. 2002;26:541–6. doi: 10.1093/jat/26.8.541. [DOI] [PubMed] [Google Scholar]
- Cunningham JA. Untreated remissions from drug use: the predominant pathway. Addict Behav. 1999;24:267–70. doi: 10.1016/s0306-4603(98)00045-8. [DOI] [PubMed] [Google Scholar]
- Cunningham JA, Lin E, Ross HE, et al. Factors associated with untreated remissions from alcohol abuse or dependence. Addict Behav. 2000;25:317–21. doi: 10.1016/s0306-4603(98)00130-0. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK. Four-year outcomes from the Early Re-Intervention (ERI) experiment using Recovery Management Checkups (RMCs) Drug Alcohol Depend. 2012;121:10–7. doi: 10.1016/j.drugalcdep.2011.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finney JW, Moos RH. Entering treatment for alcohol abuse: a stress and coping model. Addiction. 1995;90:1223–40. doi: 10.1046/j.1360-0443.1995.90912237.x. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Godley M, Godley S, Dennis M, et al. The effect of assertive continuing care on continuing care linkage, adherence and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2007;102:81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- Hacker K, Walker DK. Achieving population health in accountable care organizations. Am J Public Health. 2013;103:1163–7. doi: 10.2105/AJPH.2013.301254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K, Moos RH. Reduced substance-abuse-related health care costs among voluntary participants in Alcoholics Anonymous. Psychiatr Serv. 1996;47:709–13. doi: 10.1176/ps.47.7.709. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Moos R. Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcohol Clin Exp Res. 2001;25:711–6. [PubMed] [Google Scholar]
- Humphreys K, Moos RH. Encouraging posttreatment self-help group involvement to reduce demand for continuing care services: two-year clinical and utilization outcomes. Alcohol Clin Exp Res. 2007;31:64–8. doi: 10.1111/j.1530-0277.2006.00273.x. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA. Alcoholics anonymous effectiveness: faith meets science. J Addict Dis. 2009;28:145–57. doi: 10.1080/10550880902772464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF. Self-help for substance use disorders: history, effectiveness, knowledge gaps & research opportunities. Clin Psychol Rev. 2003;23:639–63. doi: 10.1016/s0272-7358(03)00053-9. [DOI] [PubMed] [Google Scholar]
- Kelly JF, White WL. Addiction Recovery Management. New York: Springer; 2011. [Google Scholar]
- Kelly JF, Yeterian JD. Empirical awakening: the new science on mutual help and implications for cost containment under health care reform. Subst Abus. 2012;33:85–91. doi: 10.1080/08897077.2011.634965. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Yeterian JD. Mutual-Help Groups for Alcohol and Other Substance Use Disorders. In: McCrady BS, Epstein EE, editors. Addictions: A Comprehensive Guidebook. New York: Oxford University Press; 2013. [Google Scholar]
- Kelly JF, Myers MG, Rodolico J. What do adolescents exposed to Alcoholics Anonymous think about 12-step groups? Subst Abus. 2008;29:53–62. doi: 10.1080/08897070802093122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Kahler CW, Humphreys K. Assessing why substance use disorder patients drop out from or refuse to attend 12-step mutual help groups: the ‘REASONS’ questionnaire. Addict Res Theory. 2010a;18:316–25. [Google Scholar]
- Kelly JF, Magill M, Slaymaker V, et al. Psychometric validation of the Leeds Dependence Questionnaire (LDQ) in a young adult clinical sample. Addict Behav. 2010b;35:331–6. doi: 10.1016/j.addbeh.2009.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Urbanoski KA, Hoeppner BB, et al. Facilitating comprehensive assessment of 12-step experiences: a multidimensional measure of mutual-help activity. Alcohol Treat Q. 2011;29:181–203. doi: 10.1080/07347324.2011.586280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout RL, Slaymaker V. Emerging adults’ treatment outcomes in relation to 12-step mutual-help attendance and active involvement. Drug Alcohol Depend. 2013;129:151–7. doi: 10.1016/j.drugalcdep.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labbe AK, Slaymaker V, Kelly JF. Toward Enhancing Twelve-Step Facilitation among young people: a systematic qualitative investigation of Young Adults’ 12-step Experiences. 2014 doi: 10.1080/08897077.2014.950001. Subst Abus. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lennings C. An evaluation of the Leeds Dependence Questionnaire. J Child Adolesc Subst Abuse. 1999;8:73–87. [Google Scholar]
- Maust DT, Oslin DW, Marcus SC. Mental health care in the accountable care organization. Psychiatr Serv. 2013;64:908–10. doi: 10.1176/appi.ps.201200330. [DOI] [PubMed] [Google Scholar]
- McCollister KE, French MT, Freitas DM, et al. Cost-effectiveness analysis of Recovery Management Checkups (RMC) for adults with chronic substance use disorders: evidence from a 4-year randomized trial. Addiction. 2013;108:2166–74. doi: 10.1111/add.12335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. J Stud Alcohol Suppl. 1994;12:112–8. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Montgomery H, Miller W, Tonigan J. Differences among AA groups: implications for research. J Stud Alcohol. 1993;54:502–4. doi: 10.15288/jsa.1993.54.502. [DOI] [PubMed] [Google Scholar]
- Moos RH, Moos BS. Long-term influence of duration and frequency of participation in alcoholics anonymous on individuals with alcohol use disorders. J Consult Clin Psychol. 2004;72:81–90. doi: 10.1037/0022-006X.72.1.81. [DOI] [PubMed] [Google Scholar]
- Mundt MP, Parthasarathy S, Chi FW, et al. 12-Step participation reduces medical use costs among adolescents with a history of alcohol and other drug treatment. Drug Alcohol Depend. 2012;126:124–30. doi: 10.1016/j.drugalcdep.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narcotics Anonymous. Narcotics Anonymous World Services, Incorporated; 1988. Narcotics Anonymous. [Google Scholar]
- Narcotics Anonymous. Narcotics Anonymous 2009 Membership Survey. Van Nuys, CA: Narcotics Anonymous World Services; 2010. [Google Scholar]
- Project MATCH Research Group. Project MATCH (Matching Alcoholism Treatment to Client Heterogeneity): rationale and methods for a multisite clinical trial matching patients to alcoholism treatment. Alcohol Clin Exp Res. 1993;17:1130–45. doi: 10.1111/j.1530-0277.1993.tb05219.x. [DOI] [PubMed] [Google Scholar]
- Public Health England. Mutual Aid Assessment Tool. Alcohol and Drug Recovery. London, UK: Public Health England, PHE; 2013. [Google Scholar]
- Raistrick D, Bradshaw J, Tober G, et al. Development of the Leeds Dependence Questionnaire (LDQ): a questionnaire to measure alcohol and opiate dependence in the context of a treatment evaluation package. Addiction. 1994;89:563–72. doi: 10.1111/j.1360-0443.1994.tb03332.x. [DOI] [PubMed] [Google Scholar]
- Rynes KN, Tonigan S, Rice SL. Interpersonal climate of 12-step groups predicts reductions in alcohol use. Alcohol Treat Q. 2013;31:167–85. doi: 10.1080/07347324.2013.771983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slesnick N, Tonigan JS. Assessment of alcohol and other drug use by runaway youths: a Test-Retest Study of the Form 90. Alcohol Treat Q. 2004;22:21–34. doi: 10.1300/J020v22n02_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Cunningham JA, Sobell MB. Recovery from alcohol problems with and without treatment: prevalence in two population surveys. Am J Public Health. 1996;86:966–72. doi: 10.2105/ajph.86.7.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Ellingstad TP, Sobell MB. Natural recovery from alcohol and drug problems: methodological review of the research with suggestions for future directions. Addiction. 2000;95:749–64. doi: 10.1046/j.1360-0443.2000.95574911.x. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. 2009. Treatment Episode Data Set (TEDS). Highlights 2007. National Admissions to Substance Abuse Treatment Services. DASIS Series: S-45, DHHS Publication No (SMA) 09-4360 http://oas.samhsa.gov/TEDS2k7highlights/toc.cfm. (Accessed 14 December 2010), Rockville, MD.
- Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health. Rockville, MD: SAMHSA; 2013a. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. SAMHSA. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: SAMHSA; 2013b. National Survey of Substance Abuse Treatment Services (N-SSATS): 2012. Data on Substance Abuse Treatment Facilities. BHSIS Series: S-66, HHS Publication No (SMA) 14-4809. [Google Scholar]
- Tonigan JS, Miller WR. The inventory of drug use consequences (InDUC): test-retest stability and sensitivity to detect change. Psychol Addict Behav. 2002;16:165–8. [PubMed] [Google Scholar]
- Tonigan JS, Miller WR, Brown JM. The reliability of Form 90: an instrument for assessing alcohol treatment outcome. J Stud Alcohol. 1997;58:358–64. doi: 10.15288/jsa.1997.58.358. [DOI] [PubMed] [Google Scholar]
- White WL. 2008. Recovery Management and Recovery-Oriented Systems of Care: Scientific Rationale and Promising Practices Northeast Addiction Technology Transfer Center, Great Lakes Addiction Technology Transfer Center, Philadelphia Department of Behavioral Health/Mental Retardation Services.