Abstract
Background and aims
Irritable bowel syndrome (IBS) is one of the most frequent functional gastrointestinal disorders, having its subtypes related to the predominant bowel pattern: IBS with diarrhea (IBS-D), IBS with constipation (IBS-C), mixed IBS (IBS-M) or alternating IBS (IBS-A). Some patients alternate between subtypes (IBS-A). We looked for the prevalence of alternation between subtypes in patients with IBS. We also analyzed changes in pharmacological therapy specifically addressed to IBS.
Methods
We performed a retrospective observational study that included 60 patients diagnosed with IBS according to Rome III criteria. Patients were asked using a detailed structured interview about their stool form changes regarding previous six months. Alternators were defined as patients that changed IBS subtype over time (previous six months).
Results
Out of the 60 patients diagnosed with IBS, 18 patients (30%) were alternators. Of these, 8 patients (44%) changed twice the subtype. Two patients (66.66%) of the IBS-M subgroup shifted between subtypes. Eight patients (44.44%) changed medication over the six months. Four patients (22.2%) of the alternators were on double association of therapy (antispasmodics) addressed to IBS. Four patients (22.22%) discontinued medication.
Conclusions
Patients with IBS often change between subtypes even within six months. Alternators in our pilot study represented 30% of IBS patients. IBS-M seems to be the least stable phenotype. The rarest change is the shift between IBS-C and IBS-D. Alternators also often change their pharmacological treatment (antispasmodics).
Keywords: alternators, irritable bowel syndrome, gastrointestinal diseases, diarrhea, constipation, therapy
Introduction
Irritable bowel syndrome (IBS) is a highly prevalent functional bowel disorder [1–5]. Current diagnosis is established according to Rome III criteria, using a combination of symptoms, of which the altered bowel habit and abdominal discomfort or pain are the key features [1]. Rome III settles also the features for including IBS patients into subtypes [1]. Besides the “classical subtypes”: IBS with constipation (IBS-C), IBS with diarrhea (IBS-D), and IBS-M, there is another subtype of IBS, the alternator subtype (IBS-A), which should be taken into account [1].
The definition of this subtype of IBS is heterogenous. While some authors consider IBS-A to be in fact IBS-M [6], Rome III proposes the terminology of IBS-A for patients that have often a variation of bowel habits over time, underlying that IBS-A is a distinct type, other than IBS-M [1].
Some authors consider that there is no accurate definition of this subtype of IBS [7]. We also believe that there is a need for a proper definition of an alternator, that should take into account the number of shifts between subtypes and also a temporal criteria (time to shift, or/ and time remained in the shifted subtype).
The reported prevalence for alternators varies among studies between 23% to 74% [7,8]. This prevalence is probably not the real prevalence for alternators, since there are studies that considered alternators as IBS-A patients that are in fact IBS-M [3], so the definition of IBS-A has led to confounding prevalence and comparison with some of the studies might be confounding [9], since only Rome III criteria proposes this distinction between IBS-M and IBS-A [1].
Although patients with IBS change their subtypes over time [9], there are few studies addressed to alternators.
Interest for this subgroup of patients has grown, in parallel with the development of new therapies addressed to IBS, most of the therapies being addressed to one of the IBS subtypes (SII–D and SII-C), e.g. Alosetron for IBS-D [10] and Tegaserod for IBS-C [11]. This phenotype due to the instability in time of the symptoms related to bowel transit, might necessitate specific pharmacological treatment.
Although it is considered that pathways that lead to IBS phenotypes are common, there are certain data regarding structural changes in just some of the IBS phenotypes [12], and data to support or to explain shifting of the patients are extremely limited.
Methods
Study Protocol
We performed a retrospective, observational pilot study between February 2015 – August 2015, in which we enrolled 60 consecutive adult patients diagnosed with IBS. Patients included were recruited from a tertiary care centre. Informed consent according to Helsinki Declaration study was obtained from each patient.
For identifying IBS subtypes and changes of their gut transit type as recommended by Rome III criteria, Bristol Stool Form Scale was used (BSFS) [13, 14]. Patients were asked about changes of their type of stool form auto-assessed using a structured questionnaire [7,15]. If their response was an affirmative one, they were questioned about their type of transit at the moment of study inclusion and the type of transit that they presented during previous six months, based on their BSFS. Patients who changed from one type to another were considered as alternators. Eighteen patients fulfilled the criteria for IBS-A (13 females, 5 men, mean age: 49±15.6 years).
Data regarding their pharmacological treatment at the time of inclusion in the study and during previous six months was recorded. The pharmacological treatment analyzed was the one addressed to IBS specifically – antispasmodics.
Patients
Patients included (43 females, 17 men; mean age: 52.2±14 years) in this study were diagnosed according to Rome III criteria [1].
Statistical analysis
Data analyses were performed using descriptive statistics (Microsoft Office Excel 2010 for Windows). Continuous data were expressed as means +/− standard deviation (SD).
Results
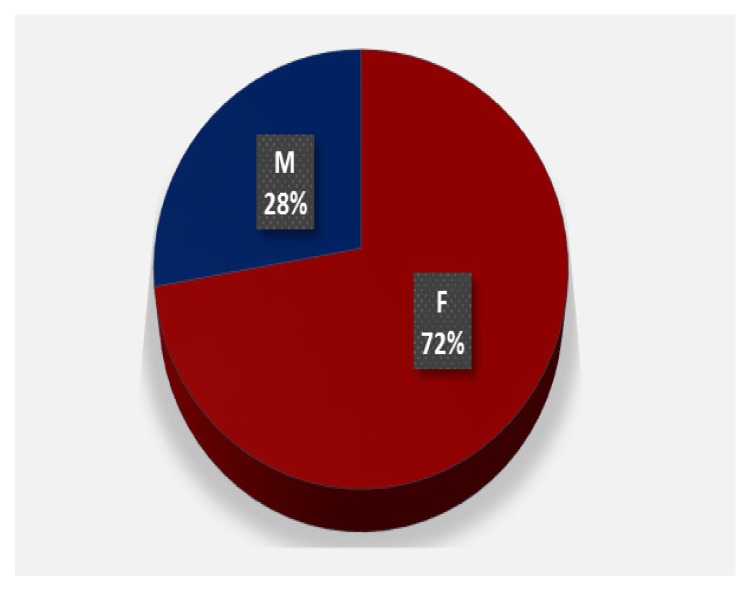
Out of the 60 de patients included in the study, 18 patients (30%) were alternators. Gender distribution with a female to male ratio of 2.6: 1 is represented in figure 1. The 18 patients that were defined as alternators patients at time of inclusion in the study had criteria for the following IBS subtypes: 9 patients IBS-D, 3 patients IBS-M and 6 patients IBS-C (Table I).
Figure 1.
Gender distribution of alternators.
Table I.
Pattern of alternation of IBS-D patients.
| IBS-D (n=9) | |||
|---|---|---|---|
| Alternating | IBS-D* | IBS-M | IBS-C |
| 5 | 2 | 2 | |
IBS-D* - patients that shifted twice in the previous six months.
Out of the 9 IBS-D - 4 patients (44.44%) changed subtype only once, 2 of these (50%) shifted to IBS-M and 2 (50%) to IBS-C (Table II). The other 5 (56.66%) patients with IBS-D had at least two changes between subtypes during last six months. Only 2 (33.33%) of the patients with IBS-C changed subtype.
Table II.
Alternators and pharmacological treatment changes.
| Alternators | |||
|---|---|---|---|
| IBS-D | IBS-M | IBS-C | |
| Type A | 9 | 3 | 6 |
| PT change | 7 | 1 | - |
Type A - subtype of IBS at the moment of inclusion in the study;
PT - pharmacological treatment.
A total number of 8 patients (44.44%) have had at least two changes in stool habit compatible with other IBS subtype.
Out of the 18 alternators, 8 patients (44.44%) changed medication (table II). Four patients (22.2%) of the alternators were on double association (Table III). Four patients (22.22%) discontinued medication.
Table III.
Pharmacological treatment divided into number of drug classes used and the rate of discontinued medication.
| PT | 1 class PT | Association of PT |
|---|---|---|
| PT study inclusion | 14 | 4 |
| Discontinued | 2 | 2 |
PT - pharmacological treatment.
Discussion
IBS-A is one of the IBS phenotypes with a marked temporal instability of symptoms. Although previous opinion or classification used to assign IBS-A to IBS-M, it is now emphasized that there are differences between the two subtypes. It is difficult to classify patients into these subtypes, and literature data points out that according to the type of criteria used they were (or are) classified either as IBS-A or IBS-M [7]. Rome III proposes the separation of the two subtypes, underlining some differences [1]. There are authors that proposed a definition for IBS-A, stating that patients should be included in this subtype only if there is a change from IBS-D to the subtype IBS-C, during one year period, and that the assessment could be performed in a retrospective manner by using questionnaires and asking patients about IBS-D and IBS-C criteria fulfilled in the preceding year [9].
The question how to define an alternator has raised several proposals: one that considers an alternation between diarrhea and constipation as an alternator and another that considers diarrhea or constipation that alternates with a normal bowel habit [9]. These two potential definitions have also some limitations, but we feel that they are closer to defining an alternator, since IBS patients shift between subtypes quite often through the IBS-M subtype [9]. The temporal limits for defining an alternator needs to be established (a year or possibly six months), since there are data regarding a shift to one type to another after three months [9] and other data report even quicker [15,16]. We question if the alternator status should be considered a distinct additional information to be added to the current classification of subtypes, e.g. SII-Da, rather than a subtype.
Since there is not yet an appropriate definition for alternators [6], we also strongly feel there is the need to set precise criteria for defining alternators.
While prevalence for alternators was reported 52.5% by one study [17], others reported that 74% of IBS patients had an alternation of constipation with diarrhea [8].
Our data are similar to another study that assessed prospectively patients and found that IBS-M was the less stable phenotype in the group study formed exclusively by females [9].
There are also financial implications due to changes in pharmacological treatment and also due to care seeking of these patients.
Although there are limitations regarding our study, similar to all retrospective studies in which patients have to recall data that might be incomplete or imprecise [9, 18] we noticed that patients were able to recall data regarding their stool type easily, and they were interested about the changes of stool form and also of pain symptoms over time. We intend to continue and develop the study, in order to try to characterize this subtype of patients.
Further studies in which deep biological characterization are needed in order to better understand the pathways that are involved in alternating from one subtype to other, besides therapy.
Conclusions
Prevalence of alternation between subtypes in our study was 30%. IBS-M seems the phenotype the least stable over time. Shifting between IBS-C and IBS-D is the rarest. Patients with an alternator profile changed also drug therapy specifically addressed (antispasmodics) to IBS over the past six months.
References
- 1.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 2.Ford AC, Vandvik PO. Irritable bowel syndrome. BMJ Clin Evid. 2012;2012:0410. [PMC free article] [PubMed] [Google Scholar]
- 3.Choung RS, Locke GR., 3rd Epidemiology of IBS. Gastroenterol Clin North Am. 2011;40(1):1–10. doi: 10.1016/j.gtc.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 4.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 5.Quigley EM, Abdel-Hamid H, Barbara G, Bhatia SJ, Boeckxstaens G, De Giorgio R, et al. A global perspective on irritable bowel syndrome: a consensus statement of the World Gastroenterology Organisation Summit Task Force on irritable bowel syndrome. J Clin Gastroenterol. 2012;46:356–366. doi: 10.1097/MCG.0b013e318247157c. [DOI] [PubMed] [Google Scholar]
- 6.Mearin F, Balboa A, Badia X, Baró E, Caldwell E, Cucala M, et al. Irritable bowel syndrome subtypes according to bowel habit: revisiting the alternating subtype. Eur J Gastroenterol Hepatol. 2003;15:165–172. doi: 10.1097/00042737-200302000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Choung RS, Locke GR, 3rd, Zinsmeister AR, Melton LJ, 3rd, Talley NJ. Alternating bowel pattern: what do people mean? Aliment Pharmacol Ther. 2006;23:1749–1755. doi: 10.1111/j.1365-2036.2006.02953.x. [DOI] [PubMed] [Google Scholar]
- 8.Hungin AP, Chang L, Locke GR, Dennis EH, Barghout V. Irritable bowel syndrome in the United States: prevalence, symptom patterns and impact. Aliment Pharmacol Ther. 2005;21:1365–1375. doi: 10.1111/j.1365-2036.2005.02463.x. [DOI] [PubMed] [Google Scholar]
- 9.Drossman DA, Morris CB, Hu Y, Toner BB, Diamant N, Leserman J, et al. A prospective assessment of bowel habit in irritable bowel syndrome in women: defining an alternator. Gastroenterology. 2005;128:580–589. doi: 10.1053/j.gastro.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 10.Camilleri M, Northcutt AR, Kong S, Dukes GE, McSorley D, Mangel AW. Efficacy and safety of alosetron in women with irritable bowel syndrome: a randomized, placebo-controlled trial. Lancet. 2000;355:1035–1040. doi: 10.1016/S0140-6736(00)02033-X. [DOI] [PubMed] [Google Scholar]
- 11.Novick J, Miner P, Krause R, Glebas K, Bliesath H, Ligozio G, et al. A randomized, double-blind, placebo-controlled trial of tegaserod in female patients suffering from irritable bowel syndrome with constipation. Aliment Pharmacol Ther. 2002;16:1877–1888. doi: 10.1046/j.1365-2036.2002.01372.x. [DOI] [PubMed] [Google Scholar]
- 12.Camilleri M, Atanasova E, Carlson PJ, Ahmad U, Kim HJ, Viramontes BE, et al. Serotonin-transporter polymorphism pharmacogenetics in diarrhea-predominant irritable bowel syndrome. Gastroenterology. 2002;123:425–432. doi: 10.1053/gast.2002.34780. [DOI] [PubMed] [Google Scholar]
- 13.Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scand J Gastroenterol. 1997;32(9):920–924. doi: 10.3109/00365529709011203. [DOI] [PubMed] [Google Scholar]
- 14.Heaton KW, Ghosh S, Braddon FE. How bad are the symptoms and bowel dysfunction of patients with the irritable bowel syndrome? A prospective, controlled study with emphasis on stool form. Gut. 1991;32:73–79. doi: 10.1136/gut.32.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tillisch K, Labus JS, Naliboff BD, Bolus R, Shetzline M, Mayer EA, et al. Characterization of the alternating bowel habit subtype in patients with irritable bowel syndrome. Am J Gastroenterol. 2005;100:896–904. doi: 10.1111/j.1572-0241.2005.41211.x. [DOI] [PubMed] [Google Scholar]
- 16.Mearin F, Baro E, Roset M, Badia X, Zarate N, Perez I. Clinical patterns over time in irritable bowel syndrome: symptom instability and severity variability. Am J Gastroenterol. 2004;99:113–121. doi: 10.1046/j.1572-0241.2003.04023.x. [DOI] [PubMed] [Google Scholar]
- 17.Abdulmajeed A, Rabab MA, Sliem HA, Hebatallah NE. Pattern of irritable bowel syndrome and its impact on quality of life in primary health care center attendees, Suez governorate, Egypt. Pan Afr Med J. 2011;9:5. doi: 10.4314/pamj.v9i1.71177. Epub 2011 May 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drossman DA, Toner BB, Whitehead WE, Diamant NE, Dalton CB, Duncan S, et al. Cognitive-behavioral therapy versus education and desipramine versus placebo for moderate to severe functional bowel disorders. Gastroenterology. 2003;125:19–31. doi: 10.1016/s0016-5085(03)00669-3. [DOI] [PubMed] [Google Scholar]