Abstract
Background and aims
Nowadays centric relation is defined as a musculoskeletal stable position, with the condyles forward, as far upward as possible, centered transversely and with the articular disc properly interposed. On the other hand, centric occlusion or maximum intercuspidation is a dental determined position. The purpose of this pilot study is to evaluate the direction, frequency and magnitude of the discrepancy between centric occlusion and centric relation in all three axial directions, in a muscular non-deprogrammed population, before the beginning of orthodontic treatment.
Methods
The study group was represented by 40 symptomatic and asymptomatic patients seeking orthodontic treatment in a private dental office in Cluj-Napoca, Romania between 2014 and 2015. All patients had full records and articulator mounted models. All measurements were analyzed three-dimensionally.
Results
85% of the patients had vertical and 87.5% had horizontal CO-CR discrepancy for both condyles. 87.5% of the cases have had a significant condylar displacement in at least one of the three planes.
Conclusions
We should be aware of the dental occlusion determined by the dental contacts and the occlusion dictated by the musculoskeletal stable position of the condyles. The bigger the discrepancy between these two positions at the level of the condyles, the greater the chances to have either a patient who will develop a form of TMD before/during or after the orthodontic or prosthetic treatment, or a patient suffering already, but poorly diagnosed.
Keywords: centric relation, centric dental occlusion, jaw relation record, orthodontics
Introduction
There is a general agreement within the dental profession regarding the ideal position targeted by our patients’ treatment: centric relation [1–3]. Nowadays centric relation is defined as a musculoskeletal stable position, with the condyles forward, as far upward as possible, centered transversely and with the articular disc properly interposed.[1,4–10]
Centric relation (CR) is a musculoskeletal position, anatomically determined, repeatable and reproducible [10]. Treating our patients in this position is one of our biggest challenges, both in orthodontics and prosthetics. This ideal goal will provide long-term stability, improved functionality and esthetics, healthy muscles and joints [10,11].
On the other hand, centric occlusion (CO) or maximum intercuspidation is a dental determined position. Tooth morphology and position are the primary influences determining the mandibular position and movements. The condylar position is strongly determined by the dental contacts and intercuspidation through muscles and ligaments [8–10].
These two reference positions of the mandible do not usually coincide in natural dentition [10,11]. If the dental occlusion is not stabilized in centric relation, the mandible will slide (pathological pro- or laterotrusion with secondary effects like abrasion) every time our teeth touch, from CR to CO, causing a stabilization of the occlusion but also a repositioning of the mandibular condyles in the glenoid fossa. Most frequently this repositioning direction is down and backward, but it can also be anterior and inferior or just inferior. This repositioning forces the mandible and the lower dental arch to assume an anterior position [10].
Historically, the most common way to classify the ideal static state of the dentiton was Angle’s molar relationship. This classification, along with clinical findings, was generally enough for orthodontists to make a diagnosis and decide on a treatment plan. However, once the CR occlusion is analyzed (on articulator mounted models), the discrepancy between CO and CR is present most of the times, and we may find an increased overjet, reduced overbite and Angle’s molar relationship modification - all of these possibly leading to a diagnosis, treatment plan and procedures for treatment changes [2,9,10]. Several methods are given in order to evaluate the discrepancy between CO and CR: direct visual evaluation in the oral cavity, radiological and imaging. Furthermore, there is an easier, simpler and more efficient method, using the MCD (measures condyle displacement) or CPI (condyle position indicator) tool. With this tool we are able to graphically asses in a three-dimensional manner (horizontal, vertical and transversal) the discrepancy between CO and CR- it is simple, repeatable, cheap and easy. The MCD tool is designed based on the same axis as the articulator provided by the manufacturer, which are paired instruments, giving us critical and valuable information about our patients’ seated condylar position - centric relation treatment goal. It is very useful to evaluate the condylar changes that take place during splint therapy as it is an essential indicator of the direction of the condylar movement and the stability of the achieved results [12–24].
The purpose of this pilot study is to evaluate the direction, frequency and magnitude of the discrepancy between CO and CR in all three axial directions, in a muscular non-deprogrammed population, before the beginning of the orthodontic treatment.
Material and methods
The study group was represented by 40 symptomatic and asymptomatic patients seeking orthodontic treatment in a private dental office in Cluj-Napoca, Romania between 2014 and 2015. The screening of signs and symptoms of temporo-mandibular joint disease was done by the analysis of the medical and dental history as well as the clinical examination of the patient. All the patients were examined by the same orthodontist, in order to eliminate the errors given by different examiners. There were 16 male patients and 24 females. The age of the patients was between 9 and 40 years and the average age of the sample was 24.2 years. The age of the female subjects was between 9 and 37 years with an average value of 23.8 years and the age of the male subjects was between 12 and 40 years with an average value of 24.8 years.
The records taken for each patient consisted of:
Written dental and medical history.
Clinical examination.
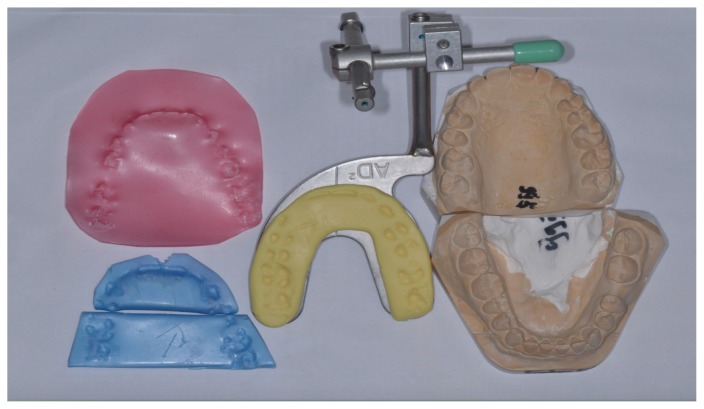
Study cast models (figure 1).
CO bite registrations in pink wax(figure 1).
CR bite registrations in blue Almore wax( centric “ du jour”) (figure 1).
Facebow registration of the terminal estimated hinge axis position( figure 1).
Graphic three-dimensional position of the mandibular condyles.
Photographs.
Orthopantomography and lateral ceph X-rays
Cone Beam CT or MRI scans in certain cases.
Figure 1.
Part of the registrations taken in order to fully diagnose each case: study cast models in class IV plaster, CO and CR wax registrations, facebow bitefork.
The maxillary and mandibular impressions were taken with rim lock metallic trays, after the appropriate size was chosen in order to perfectly fit the patient. All the impressions were taken by the same orthodontist and using the same alginate impression material. Because of the instability of the material, all the impression were poured within 30 minutes. Study models were poured using class IV dye stone. Once the models have cooled down, the laboratory technician has examined the models for bubbles and then were all trimmed to size, without touching the teeth or altering the casts in any other way. The CO registration is always taken first in order not to deprogram the patient’s neuromusculature while instructing him and taking the CR registration.
The CO registration is done using a single sheet of pink wax. The pink wax is trimmed to fit the maxillary arch, then it is warmed in water bath until soft and the patient is asked to close his mouth as he “usually does”. Then, once the mouth is closed, the pink wax registration is cooled with the air syringe, carefully removed and placed in ice cold water.
The CR registration was done using Almore extra hard blue wax, 10x thin. The wax was warmed in 57 degrees water bath, rolled and trimmed - this way we obtained two pieces of wax, an anterior (from canine to canine) and a posterior one (second bicuspid and molars usually). Then, we manipulated the mandible on its arc of closure using the Roth technique. Once we obtained the two blue wax bites, we checked them for any perforations or distortion - if there were none and everything was done correctly, then the two blue wax bites were also placed in ice cold water.
To register and capture the three-dimensional position of the maxilla, its relationship with the temporomandibular joint and the estimated terminal hinge axis position, we used the facebow.
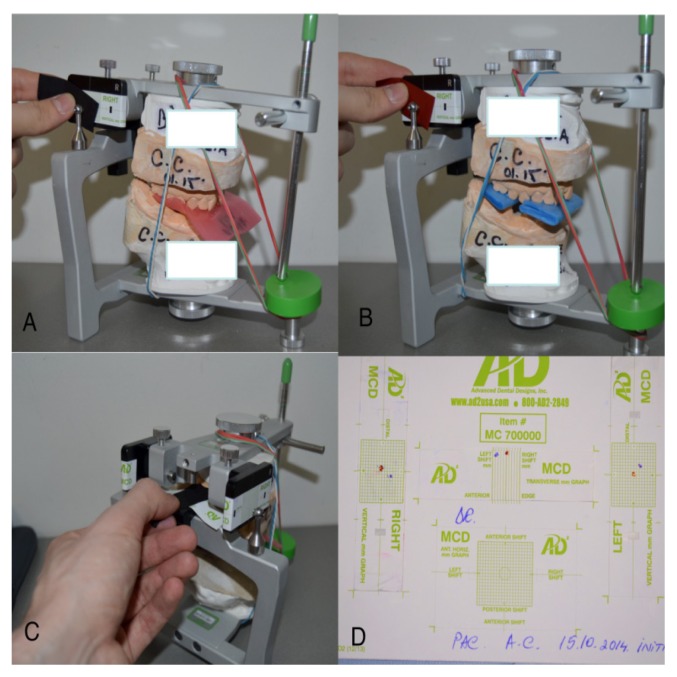
The dental casts were then mounted in a semi adjustable articulator (AD2- Advanced Dental Design, Riverside, CA) (figure 2). The mounted models were transferred into the MCD instrument and with the help of the MCD Patient Graph paper sheet, the three dimensional condylar position change from CR (seated condyles) to CO was recorded. The CR position was recorded by using red articulating paper and the CO by using a blue one. We have had two lateral graphs for the right and left condyle position assessment in the vertical and horizontal planes and a transversal graph for the assessment of the discrepancy between CO and CR in the transversal plane (figure 3).
Figure 2.
AD2 articulator mounted models.
Figure 3.
Condylar position evaluation with the use of MCD: A. CO condylar position in the vertical and horizontal planes; B. CR condylar position in the vertical and horizontal planes; C. Transverse condylar position evaluation in CO; D. MCD paper graph after CO-CR discrepancy registration.
The measurements were done by approximation of 0.1 millimeters (mm) multiples. The horizontal condylar shifts were assigned positive values if they were anterior to the center of the paper graph axis and negative values if they were posterior. The vertical displacement was assigned with positive values if the position of the condyle was inferior and negative values if this position was superior to the center of the paper graph axis. Positive and negative values only indicate the direction of the movement, the magnitude of the displacement was calculated based on the absolute values. For the transverse shift we used only the absolute value of the discrepancy. The statistical analysis was performed using Numbers software (Mac OS X Yosemite v10.10.2) and it studied the frequency, direction as well as the magnitude of the discrepancy of the position of mandibular condyles between these two reference positions, centric occlusion and centric relation. It is a pure descriptive analysis of the discrepancy.
For all clinical and laboratory procedures, each of the manufacturer’s instructions were followed. Also, we used the same articulator and MCD instrument for all patients. All the 120 MCD measurements were analyzed three-dimensionally.
Results
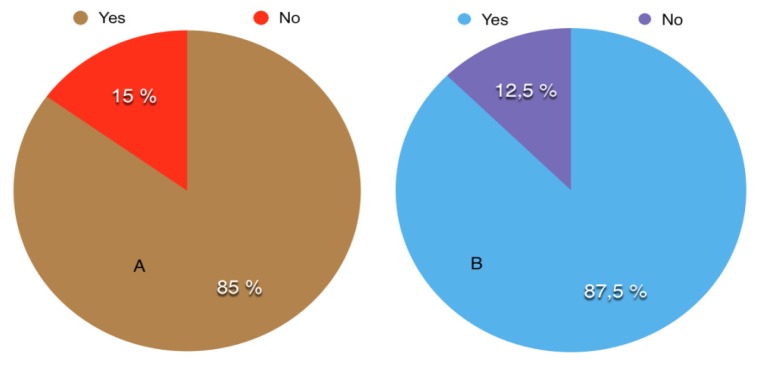
85% of the patients had vertical and 87.5% had horizontal CO-CR discrepancy for both condyles (figure 4).
Figure 4.
The CO-CR discrepancy: A. Vertical discrepancy; B. Horizontal disprepancy.
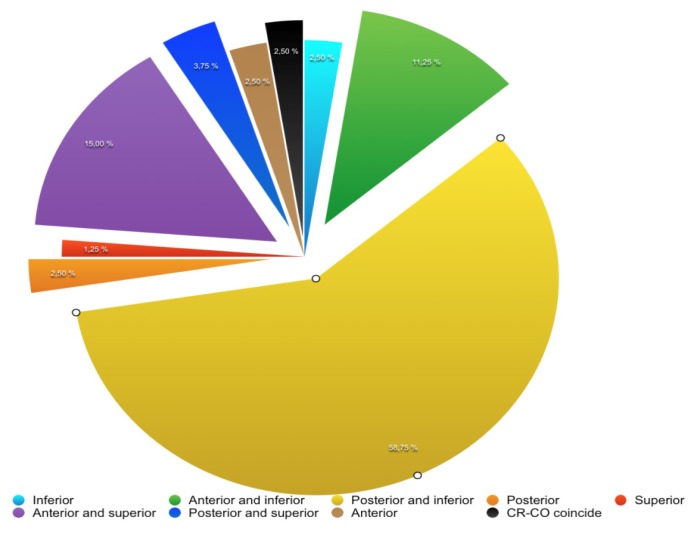
Figure 5 presents the direction of vertical and horizontal condylar displacement. 72.5% of the measurements have shown an inferior position of the mandibular condyle in CO when compared with the CR: 58.75% were posterior and inferior, 11.25 % were anterior and inferior and 2.5% were just inferior.
Figure 5.
Vertical and horizontal condylar displacement between CO-CR.
In the transversal plane, 57.5% of the condylar displacement were to the right, 30% to left and in only 12.5% the two reference positions coincided.
The left condyle had more vertical displacement (52.5%) and less horizontal. The right condyle had 60% vertical displacement and only 40% horizontal. When comparing the movements for both condyles, 42.5% of the measurements had greater vertical discrepancy than horizontal. Only 5% of the condyles had pure horizontal displacement without any vertical shift.
Only 2.5% of the subjects have had the same CO-CR position of the condyles in the horizontal and vertical planes, and for 12.5% of the subjects the two reference positions have coincided in the transversal plane.
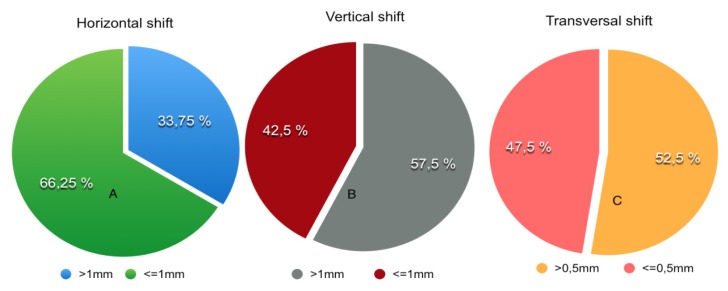
The values of the condylar discrepancy >1mm in the horizontal and vertical plane, and >0.5 mm in the transversal plane are considered clinically significant [15]. According to this, 33.75% of the cases have had a horizontal discrepancy >1 mm, 57.5% of the cases have had a vertical discrepancy >1 mm and 52.5% of the cases have shown a transversal discrepancy >0.5mm (figure 6).
Figure 6.
The distribution of the CO-CR shift: A. Horizontal condylar shift; B. Vertical condylar shift; C. Transversal condylar shift.
87.5% of the cases had a significant condylar displacement in at least one of the three planes.
The vertical and horizontal displacement and the transversal shift of the condyles obtained in our study are shown in Table I.
Table I.
Condylar displacement measurements obtained in our study (absolute values).
| Condylar Displacement: | Condyle | Maximum condyle displacement (mm)* | Mean (mm)** |
|---|---|---|---|
| Vertical | Left | 3.4 | 1.4 |
| Right | 3.3 | 1.25 | |
| Both | 3.4 | 1.3 | |
| Horizontal | Left | 4.2 | 1.1 |
| Right | 2.4 | 0.89 | |
| Both | 4.2 | 0.99 | |
|
| |||
| Transversal shift | To the left | 1.5 | 0.2 |
| To the right | 1.2 | 0.36 | |
| Both sides | 1.35 | 0.28 | |
mm= milimeters;
The minimum value of the condyle displacement was 0 mm in all three directions;
Discussion
Sometimes when analyzing the articulator mounted models and MCD graph, we uncover the real relationship between the jaws. In certain patients this brings clinically significant occlusal modifications such as increased overjet, decreased overbite, midline shifts, cross-bites or Angle’s molar relationship change.
The analysis of the overbite and overjet is very important because sometimes these aspects help the orthodontist decide whether the case is a four bicuspid extraction case, if there’s a need for a vertical control of the posterior area in order to obtain the proper overbite, if the amount of intrusion needed is achievable by orthodontic mechanics, miniscrews or anchor plates, or whether orthognathic surgery should be involved.
The displacement of the condyles from centric occlusion to centric relation in a posterior-inferior (58.75%), anterior-inferior (11.25%) or inferior (2.5%) position we obtained in our study is in concordance with the studies of Wood and Elliot [16] (posterior-inferior-63%, anterior-inferior- 20% and inferior-8%), Crawford [15] (posterior-inferior-70%) and Cordray [10] (posterior-inferior-66.7%, anterior-inferior-25.4% and 5.7% inferior). We obtained a vertical displacement of the condyles that was bigger than the horizontal one: 52.5% for the right condyle, 60% for the left condyle and 42.5% for both. The same results were reported by Hidaka et al. [18], Shildkaraut et al. [13], Wood and Elliot [16], Wood and Korne [22]. Cordray [10] obtained 93.1% vertical displacement for the right condyle, 92.2% for the left one and 88.1% for both. In our study only 5% of the subjects had just horizontal displacements without any vertical one but Cordray [10] obtained 11.5%.
Our study supports Roth’s theory [25] of vertical/horizontal condylar displacement caused by premature dental contacts in the posterior area.
Theoretically, on the paper graphs of the MCD instrument we cannot have the CO position of the condyle superior to CR. In our study CO position was superior in 20% of the condyles, double when compared with Wood and Elliot [16] who observed this situation in 10% of the condyles. This superior position of the condyles in CO may have been caused by an error in CR or hinge axis registration. However, it can also be caused by temporomandibular joint pathology: condylar resorption and remodeling with the loss of vertical height, glenoid fossa remodeling, articular disc displacement or other conditions associated with temporomandibular disorders. Another factor to be taken into consideration is the neuromuscular deprogramming of the patients before CR registration. Karl and Foley [21] have used an anterior jig to obtain muscular deprogramming prior to CR registration and as a result they obtained bigger CO-CR discrepancies when compared to other studies. They proved that even without prior neuromuscular deprogramming, with the two pieces blue wax technique, 18% of the patients had a discrepancy bigger than 2mm in the vertical or horizontal plane and the percentage has grown up to 40% when CR registration was done with prior deprogramming, with an anterior stop. Note that in our study the patients were not neuromusculary deprogrammed.
The mean vertical and horizontal condylar displacement and also the transversal shift we’ve obtained compared with other studies are shown in table II.
Table II.
Comparison between our results and other studies.
| Vertical | Orizontal | Transversal | Number of patients | |
|---|---|---|---|---|
|
|
||||
| Our study | 1.30 mm* | 0.99 mm | 0.28 mm | 40 |
| **Cordray10 | 1.80 mm | 0.86 mm | 0.26 mm | 596 |
| **Karl&Foley21 | 1.76 mm | 1.54 mm | 0.51 mm | 40 |
| Weffort26 (TMD symptoms) | 1.60 mm | 0.64 mm | 0.41 mm | 35 |
| Weffort26 (No TMD symptoms) | 1.26 mm | 0.63 mm | 0.23 mm | 35 |
| Wood22 | 1.20 mm | - | - | 39 |
mm=milimeters;
the patients were neuromuscular deprogrammed previous centric relation registration;
In our study we have considered clinically significant values for the vertical and horizontal discrepancy, superior to 1 mm and superior to 0.5 mm discrepancy in the transversal plane [15]. In literature, the majority of the studies have chosen as clinically significant a minimum value of 2 mm in the vertical and horizontal plane and more than 0.5 mm in the transversal plane [10,13,18]. Therefore, in the vertical plane, values >2mm were obtained by Cordray [10] in 53% of the cases, Shildkraut et al [13] in 52% of the cases and Hidaka et al [18] in 14% of the cases. We have obtained this amount of discrepancy in only 21.25% of the cases. Taking into consideration that our sample was non-deprogrammed, and Karl and Foley [21] have stated that the probability of finding a CO-CR discrepancy >2mm either in the vertical or horizontal plane doubles when the patients are neuromuscular deprogrammed, our percentage is similar to Cordray’s [10] who deprogrammed his patients prior to CR registration. In the horizontal plane we have obtained discrepancies bigger than 2 mm in 7.5% of the measurements, more than Hidaka et al. [18] (2%). Values superior to 1.6 mm were found in 20 % of the measurements, close to Cordray [10] study (19.6%).
In his study Crawford [15] has stated that there is a strong correlation between the CO-CR condylar discrepancy and the presence of signs and symptoms of temporomandibular disorders (TMD). For the patients having a CO-CR discrepancy more than 1 mm, all the clinical parameters were increased. Thus, as the condylar discrepancy augments, the TMD symptoms increase. Padala et al. [27] found in their research that horizontal and vertical condylar discrepancies are significantly greater in symptomatic patients than in the asymptomatic ones. Weffort [26] also claimed that the symptomatic patients have much more important transversal shift than the asymptomatic ones.
The transversal discrepancies greater than 0.5 mm are much more frequently associated with signs and symptoms of TMD. [1]
A clinically significant CO-CR discrepancy was found in 87.5% of the patients, more than what Cordray [10] (57.5%) and Hidaka et al. [18] (38.7%) obtained.
Our results would have been different, if our patients’ sample had been bigger, the patients neuromuscular deprogrammed and also if we had large enough samples for the asymptomatic and symptomatic group in order to correlate the TMD signs and symptoms with the amount of the CO-CR discrepancy.
Error sources in our study could have been:
Hinge axis registration errors
The CR registration technique
CR blue wax bites and CO pink wax distortion when registering the two reference positions and while handling them
MCD graph registration errors
The impression material distortion
Human errors.
The following treatment sequences can be influenced by the presence of a CO-CR discrepancy [9,10,25]:
-
Diagnosis:
- the magnitude of the horizontal, vertical and transversal discrepancy to be corrected
- the mandibular growth direction
- the mandibular autorotation anticipated throughout treatment
- the possible presence of TMD conditions the patients’ susceptibility to TMD
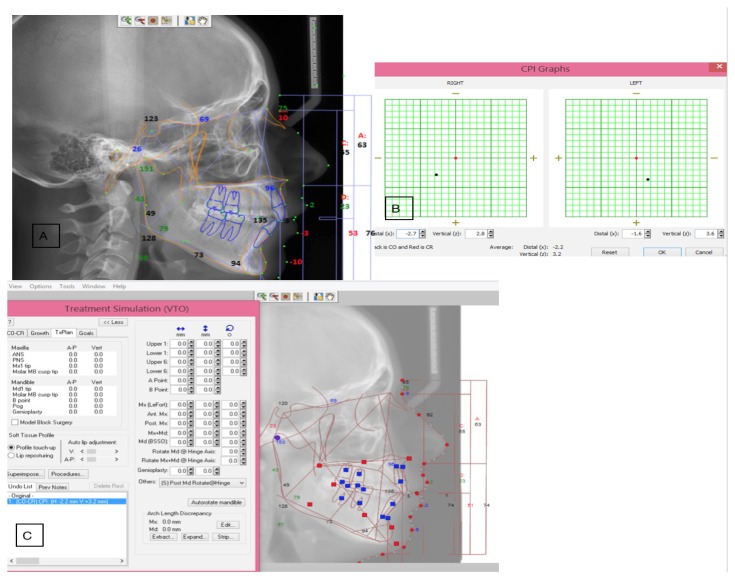
- lateral cephalometric radiograph analysis changes [13] (figure 7)
-
Treatment planning:
- extraction vs. non-extraction treatment
- orthodontic treatment only vs. orthodontic-surgical treatment
Anchorage needs of the case
The treatment mechanics (given especially by the diagnosis and the anchorage needs)
The final occlusal finishing of the case (the position of the dental arches in a three-dimensional approach)
Evaluation of the possible effects of the orthodontic treatment overall
The possible relapse degree of the case.
Figure 7.
Lateral cephalometric radiograph changes when adding the CO-CR discrepancy in Dolphin software; A. Initial analysis; B. CO-CR discrepancy; C. Changes occurring after the CO-CR correction.
In the future we are very much interested in designing a new study that would incorporate larger and homogenous patient samples. Evaluating the CO-CR discrepancy in distinctive facial and growth patterns, before and after splint therapy, before and after different treatment protocols, or even before and after functional therapy in children and adolescents could give us a clearer idea about the effect of our treatment on the temporomandibular joint.
Conclusions
In our study all the patients had at least one plane CO-CR discrepancy. More frequently, this displacement was inferior and posterior when teeth were touching in maximum intercuspation.
Only 2.5% of the subjects have had CO-CR coincidence in the horizontal and vertical plane and 12.5% in the transversal.
The average value of vertical condyle displacement is 1.3 times higher than the horizontal
MCD graph can bring useful information about condyles position and treatment outcome (for orthodontic treatment, orthognathic surgery or maxillary anterior guided orthosis (MAGO) therapy)
MCD graph is an important tool for daily orthodontic diagnosis.
References
- 1.Okeson JP. Management of temporomandibular disorders and occlusion. 6th ed. Mosby Elsevier; St. Louis: 2008. [Google Scholar]
- 2.Girardot RA. Thesis. University of Southern CA; 1972. Functioning tooth relationship in the adult dentition. [Google Scholar]
- 3.Posselt U. Studies in the mobility of the human mandible. Acta Odontol Scand. 1952;10(Suppl):19–27. [Google Scholar]
- 4.Papilian V. Anatomia omului. Volum 1: Aparatul locomotor. Editţia 12. Editura BIC ALL; 2006. [Google Scholar]
- 5.Wilkinson TM. The relationship between the disk and the lateral pterygoid muscle in the human temporomandibular joint. J Prosthet Dent. 1988;60:715–724. doi: 10.1016/0022-3913(88)90406-4. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka TT. TMJ microanatomy: an approach to current controversies. Chula Vista: Calif: Clinical Research Foundation; 1992. [Google Scholar]
- 7.Tanaka TT. Advanced dissection of the temporomandibular joint. Chula Vista: Calif: Clinical Research Foundation; 1989. [Google Scholar]
- 8.Dawson PE. Functional occlusion: From TMJ to Smile Design. Mosby Elsevier; St. Louis: 2007. [Google Scholar]
- 9.Girardot RA Jr, editor. Goal-directed orthodontics. Los Gatos, CA: Roth Williams International Society of Orthodontists; 2013. [Google Scholar]
- 10.Cordray FE. Three-dimensional analysis of models articulated in the seated condylar position from a deprogrammed asymptomatic population: a prospective study. Part 1. Am J Orthod Dentofacial Orthop. 2006;129:619–630. doi: 10.1016/j.ajodo.2004.10.015. [DOI] [PubMed] [Google Scholar]
- 11.Utt TW, Meyers CE, Jr, Wierzba TF, Hondrum SO. A three-dimensional comparison of condylar position changes between centric relation and centric occlusion using the mandibular position indicator. Am J Orthod Dentofac Orthop. 1995;107(3):298–308. doi: 10.1016/s0889-5406(95)70146-x. [DOI] [PubMed] [Google Scholar]
- 12.Slavicek RJ. Clinical and instrumental functional analysis and treatment planning. Part IV: Instrumental analysis of mandibular casts using the mandibular position indicator. J Clin Orthod. 1988;22:566–575. [PubMed] [Google Scholar]
- 13.Shildkraut M, Wood DP, Hunter WS. The CR-CO discrepancy and its effect on cephalometric measurements. Angle Orthod. 1994;64:333–342. doi: 10.1043/0003-3219(1994)064<0333:TCDAIE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Girardot RA. The nature of condylar displacement in patients with temporomandibular pain-dysfunction. Orthod Rev. 1987;1:16–23. [PubMed] [Google Scholar]
- 15.Crawford SD. Condylar axis position, as determined by the occlusion and measured by the CPI instrument, and signs and symptoms of temporomandibular dysfunction. Angle Orthod. 1999;69:103–115. doi: 10.1043/0003-3219(1999)069<0103:CAPADB>2.3.CO;2. discussion 115–6. [DOI] [PubMed] [Google Scholar]
- 16.Wood DP, Elliott RW. Reproducibility of the centric relation bite registration technique. Angle Orthod. 1994;64:211–221. doi: 10.1043/0003-3219(1994)064<0211:ROTCRB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman PJ, Silverman SI, Garfinkel L. Comparison of condylar position in centric relation and in centric occlusion in dentulous subjects. J Prosth Dent. 1973;30:582–588. [PubMed] [Google Scholar]
- 18.Hidaka O, Adachi S, Takada K. The difference in condylar position between centric relation and centric occlusion in pretreatment Japanese orthodontic patients. Angle Orthod. 2002;72:295–301. doi: 10.1043/0003-3219(2002)072<0295:TDICPB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Williamson EH, Evans DL, Barton WA, Williams BH. The effect of bite plane use on terminal hinge axis location. Angle Orthod. 1977;47:25–33. doi: 10.1043/0003-3219(1977)047<0025:TEOBPU>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Williamson EH. Laminagraphic study of mandibular condyle position when recording centric relation. J Prosthet Dent. 1978;39:561–564. doi: 10.1016/s0022-3913(78)80194-2. [DOI] [PubMed] [Google Scholar]
- 21.Karl PJ, Foley TF. The use of a deprogramming appliance to obtain centric relation records. Angle Orthod. 1999;69:117–125. doi: 10.1043/0003-3219(1999)069<0117:TUOADA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Wood DP, Korne PH. Estimated and true hinge axis: a comparison of condylar displacements. Angle Orthod. 1992;62:167–175. doi: 10.1043/0003-3219(1992)062<0167:EATHAA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Hicks ST, Wood DP. Recording condylar movement with two facebow systems. Angle Orthod. 1996;66:293–300. doi: 10.1043/0003-3219(1996)066<0293:RCMWTF>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Rosner D, Goldberg GF. Condylar retruded contact position and intercuspal position and correlation in dentulous patients. Part I: Three dimensional analysis of condylar registrations. J Prosthet Dent. 1986;56:230–239. doi: 10.1016/0022-3913(86)90481-6. [DOI] [PubMed] [Google Scholar]
- 25.Roth RH, Rolfs DA. Functional occlusion for the orthodontist. Part II. J Clin Orthod. 1981;15:100–123. [PubMed] [Google Scholar]
- 26.Weffort SY, de Fantini SM. Condylar displacement between centric relation and maximum intercuspation in symptomatic and asymptomatic individuals. Angle Orthod. 2010;80:835–842. doi: 10.2319/090909-510.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Padala S, Padmanabhan S, Chithranjan AB. Comparative evaluation of condylar position in symptomatic (TMJ dysfunction) and asymptomatic individuals. Indian J Dent Res. 2012;23:122. doi: 10.4103/0970-9290.99060. [DOI] [PubMed] [Google Scholar]