Abstract
Objective: We conducted a preliminary investigation into dimensions of stigma and their relation to disease concealment in a sample of American adults living with multiple sclerosis (MS).
Methods: Fifty-three adults with MS in the United States completed an online survey assessing anticipated, internalized, and isolation stigma, as well as concealment.
Results: Responses to all the scales were relatively low, on average, but above scale minimums (P < .001). Ratings of isolation stigma and concealment were highest. Anticipated stigma strongly predicted concealment.
Conclusions: Many adults living with MS may be concerned that they will be the target of social stigma because of their illness. These concerns are associated with disease concealment. More research is needed to investigate how MS stigma and concealment may be independent contributors to health in patients with MS.
The goal of the present research was to conduct a preliminary investigation into dimensions of stigma and their relation to disease concealment in a sample of American adults living with multiple sclerosis (MS). MS is a chronic, immune-mediated neurologic disorder thought to be triggered when genetically susceptible individuals are exposed to possible environmental agents. The typical age at onset is approximately 30 years. Approximately 85% of people with MS have a relapsing-remitting course, characterized by acute attacks followed by full or partial recovery. As a result, many people with MS may not have overt symptoms for several years after disease onset. However, for most, symptoms eventually become apparent and can be severe and debilitating.1 MS symptoms can include sensory disturbance; visual and cognitive impairment; difficulty with balance; weakness; fatigue; bowel, bladder, and sexual dysfunction; pain; and depression.2
People with chronic illnesses often feel stigmatized by others.3 Social stigma is “a mark that designates the bearer as ‘spoiled’ and therefore as valued less than ‘normal’ people.”4(p3) Greater perception of stigma in people with chronic illness is associated with lower self-esteem,5 lower perception of social support,5 more depression and anxiety,5,6 more social conflict,5 and greater psychological distress.7 These factors can create stress that taxes the immune system8 and undermines positive health behaviors, including physician visits and treatment adherence.3
Unlike in other commonly stigmatized illnesses (eg, HIV infection), the cause of MS is considered to be beyond individual control.9 This should mitigate some of the expected stigma experienced by people with MS.10 Yet, in the small amount of research devoted to the topic, stigma is frequently identified as a concern. Much of this research has yielded insights using qualitative methods.9,11–13 For instance, interviews with 14 people living with MS revealed that strategic concealment and disclosure decisions were common in response to perceived social pressures, particularly in occupational settings.9 Interviews with another 21 people found that confronting an MS diagnosis was a significant life transition associated with uncertainty and concerns of being stereotyped and stigmatized.11 The small amount of research using quantitative measures and including samples of people with MS7,14,15 has tended to use scales that either conflate or omit relevant dimensions of stigma,16 or study quality of life, a related but distinct concept.17,18 Thus, one goal of the present research was to provide preliminary data on MS stigma by relevant stigma dimensions, such as the extent to which individuals anticipate stigma, feel isolated because of stigma, and internalize stigma.
Because MS symptoms may not be visible to others, particularly early in relapsing-remitting MS, people may try to conceal the disease.9 Concealment may prevent discrimination19 but can also be stressful,17 with negative consequences for physical health8 and disease progression.20 Concealment can also undermine opportunities for social support and increase depressive symptoms.21 In an effort to conceal, people may avoid medically related appointments or treatments, which could exacerbate disease progression. Thus, another goal of this research was to quantify MS concealment and to determine the dimensions of stigma that predict concealment behaviors.
Methods
Participants
Data were collected from 53 participants ranging in age from 23 to 71 years (mean = 45.82 years) who were primarily female (79%) and white (83%). Other ethnicities included black/African American (4%), Hispanic/Latino (6%), and mixed white and other ethnicity (7%). The median household income of participants was $75,000 to $90,000, and their median household educational attainment was a college degree, higher than national levels in the United States,22 thus indicating a relatively high socioeconomic status for this sample. Most participants were married (53%) or had a cohabitating domestic partner (6%), with approximately 19% having never been married and 23% being divorced or separated. Most participants (68%) reported living in somewhat to very urban environments. Participants had been diagnosed as having MS for an average of 7 years (mean = 6.99 years), and nearly all (93%) reported having current health insurance.
Procedure
Participants were recruited by electronic announcements with a link to an online survey about “people's experiences with—and thoughts and feelings about—having MS.” This announcement was posted on two websites (the National Multiple Sclerosis Society and This Is MS, an online forum used by patients with MS) and was included in an electronic newsletter distributed by the Consortium of Multiple Sclerosis Centers. Participation was limited to adults with MS who were fluent in English and lived in the United States most of the year. Participants who completed the study were offered $10 that they could receive by mail or donate. All the procedures were approved by the institutional review board of Columbia University (New York, NY).
Measures
Disease Status
Participants provided data on their disease status using the Patient-Determined Disease Steps (PDDS)23 and three MS performance scales (vision, cognitive symptoms, and spasticity symptoms).24 The PDDS measures overall disability on a scale from 0 (normal) to 8 (bedridden) and is well correlated with clinical assessments of disability.24 The three performance scales were summed to form a composite with a possible range of 0 to 14 (α = 0.73).
Stigma
The few quantitative studies that have assessed stigma in people with MS have also included participants with a variety of other illnesses and have used scales designed to measure chronic illness stigma generally.7,15 Although such scales can be important for comparing stigma across conditions, they are necessarily broad in focus and, as noted previously herein, tend to omit relevant dimensions.3 Because of this, we created a measure of stigma for use in the present study based on a combination of stigma measures. A total of 40 items were adapted from preexisting measures based on their psychometric properties and perceived relevance to individuals with MS (a complete list is available from the corresponding author). Items that overlapped considerably between scales or had content specific to a given illness were excluded. Sixteen items came from the Stigma Scale for Chronic Illness,15 seven from the Cataldo Lung Cancer Stigma Scale,25 five from the HIV Stigma Scale,5 four from the Epilepsy Stigma Scale,26 four from an unnamed scale developed by Earnshaw and Quinn,3 two from the Chronic Illness Anticipated Stigma Scale,6 and two from the Internalized Stigma of Mental Illness scale.27
We performed a principal components analysis to analyze the data structure of the stigma items using an oblique rotation strategy (direct oblimin) because earlier studies suggest correlations among stigma subscales.5,15 Although the principal components analysis was largely exploratory, the specific number and content of components were suggested by scales used in earlier research. Scree plot analysis led to specification of a three-component model, accounting for 52% of the variance. Absolute values of component correlations ranged from 0.16 to 0.56. These components formed the basis of three subscales with a total of 36 items, as described later herein (four poor-performing items were dropped). Participants responded to each item on a 5-point scale from 1 (not at all true) to 5 (very true), with higher scores indicating greater stigma.
Anticipated stigma included 20 items (α = 0.94) assessing participants' sense that they and others with MS were or would be targets of stigma (eg, “Because of my MS, I worry about people discriminating against me”). The second component, isolation stigma, included 12 items (α = 0.92) assessing participants' sense of being limited and set apart from others because of their MS (eg, “Because of my MS, I feel left out of things”). Some previous research has included these types of items in a more general enacted stigma subscale,7,15 but because a sense of isolation or separateness from others seems to be a core defining element of MS stigma13 and these items formed a reliable component, the term isolation stigma seemed appropriate. Internalized stigma included four items (α = 0.76) assessing participants' internalized negative feelings about their MS (eg, “I feel I'm not as good as others because I have MS”).
Concealment
Ten items assessed participants' active efforts at concealment (α = 0.91). Six items were adapted from the study by Berger et al.5 (eg, “I am very careful whom I tell that I have MS”), and the others were author generated, beginning with the phrase “In general, I tend to conceal my MS . . .” and followed by “from others,” “at work,” “from family,” or “from friends.” Participants responded to each item using a 5-point scale from 1 (not at all true) to 5 (very true), with higher scores indicating greater concealment.
Demographics and Health Behaviors
Participants reported age at diagnosis, employment and health insurance status, and demographic information. Eighteen participants reported having depression or anxiety; these were combined to form a single dichotomous variable indicating the presence or absence of a mental health condition. Three single-item variables assessed a sample of health behaviors. To assess drinking frequency, participants were asked how often they had had a drink containing alcohol in the past 6 months, with possible responses of 0 (never), 1 (monthly or less), 2 (two to four times a month), 3 (two to three times per week), and 4 (four or more times a week). An item we labeled physician delay asked, “Have you sometimes put off going to the doctor, even when you think maybe you should go?” and an item labeled therapy delay asked, “Have you ever delayed starting medication that your physician recommended?” Both items had response options from 0 (never) to 3 (frequently).
Results
Table 1 presents the characteristics of the sample. Participants were moderately disabled, with a mean PDDS score of 2.83 and an observed range from 0 (normal) to 7 (disability requiring bilateral support). The mean performance scales score was 4.57, with an observed range from 0 to 12. Participants' concerns about stigma and their tendency to conceal their MS were relatively low on average but in all cases were significantly above the scale minimum (P < .001). On a scale from 1 to 5, participants' stigma ratings were highest for the isolation subscale (mean = 2.22) and the concealment scale (mean = 2.07). Scores were somewhat lower on the anticipated stigma (mean = 1.81) and internalized stigma (mean = 1.69) subscales. A set of orthogonal within-subject contrasts revealed higher scores on the isolation subscale and the concealment scale together relative to the average of the other two subscales (F1,52 = 32.62, P < .001, partial η2 = 0.39). There was not a reliable difference between the isolation subscale and the concealment scale (F1,52 = 0.89, P = .35, partial η2 = 0.02) or between the anticipated and internalized stigma subscales (F1,52 = 1.16, P = .29, partial η2 = 0.02).
Table 1.
Descriptive statistics and intercorrelations of study variables (N = 53)
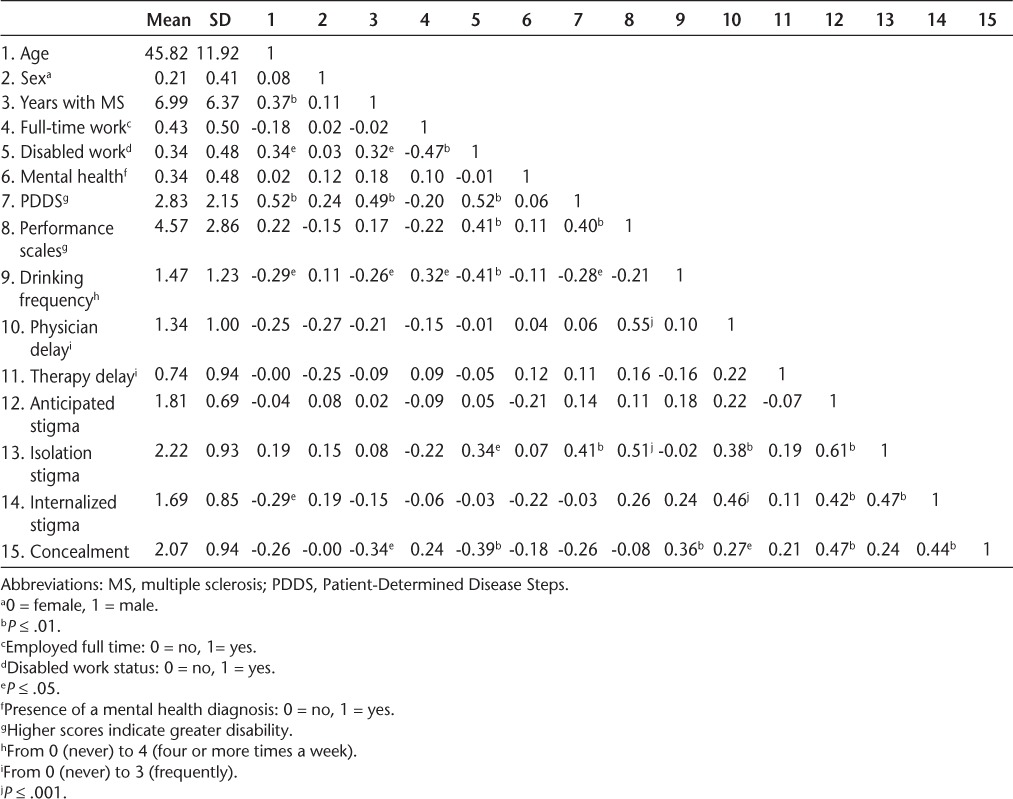
Figure 1 further shows the distribution of responses to the three stigma scales and the concealment scale. The distributions are positively skewed, but most people perceived stigma to at least some degree on all the variables. Just less than 10% of scores were above the scale midpoints for anticipated stigma and internalized stigma, whereas approximately 20% were above the scale midpoint for isolation stigma and concealment.
Figure 1.
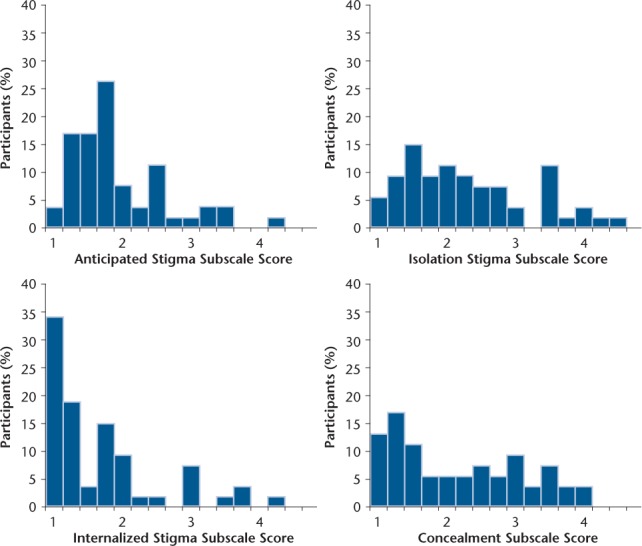
Distribution of stigma and concealment
Higher scores indicate greater stigma or concealment.
Table 1 also presents correlations between study measures. Isolation stigma was associated with disabled work status and greater impairment. Internalized stigma was associated with being younger and delaying needed physician visits. People with higher concealment scores had fewer years with an MS diagnosis and were less likely to report disabled work status, presumably because concealment is less of an option as MS progresses. Concealment was also associated with greater consumption of alcohol and delaying needed physician visits.
To predict factors involved with MS concealment, we specified a hierarchical multiple regression model (Table 2). In the first step, we included sex, participants' disability status with respect to work (no/yes), and the number of years since their MS diagnosis. We included sex as a covariate because of the greater proportion of females than males in the sample. We included the other two variables as covariates because of their significant bivariate associations with concealment. These three variables explained approximately 20% of the variance in concealment (F3,49 = 4.08, P = .01).
Table 2.
Results of primary hierarchical regression models (N = 53)
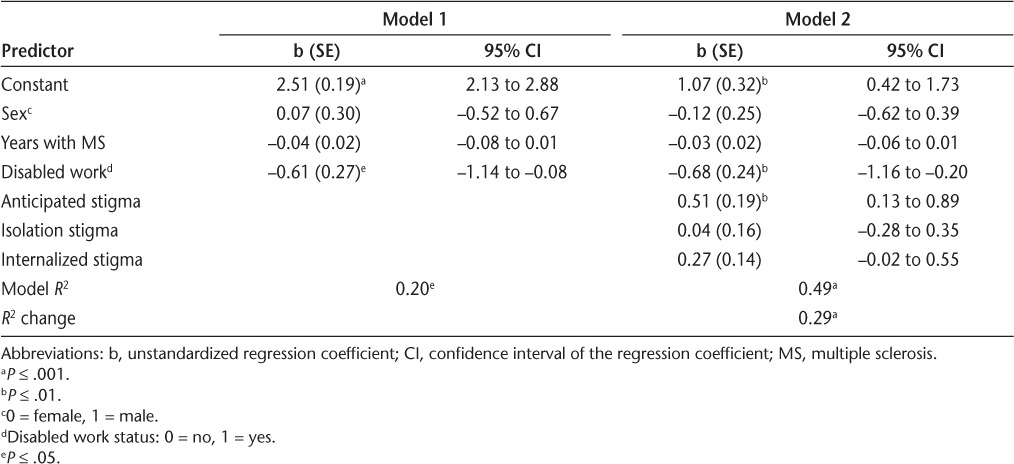
In the next step, we added the three stigma scales to the base model outlined in the previous paragraph, which explained an additional 29% of the variance (F3,46 = 8.62, P < .001) (Table 2). Thus, the complete model (ie, with all six predictors) explained nearly half the variance in concealment (R2 = 0.49). Despite the nonnormal distribution of some predictors, analysis of residuals from the complete model did not reveal any outliers (all studentized deleted residuals < 2.70) or violations of model assumptions.
Of the stigma variables, only anticipated stigma was reliably associated with greater concealment (b = 0.51, t46 = 2.70, P = .01, partial η2 = 0.14, 95% confidence interval [CI], 0.13 to 0.89). Internalized stigma was associated with marginally higher levels of concealment (b = 0.27, t46 = 1.87, P = .07, partial η2 = 0.07, 95% CI, −0.02 to 0.55). However, participants' sense of isolation stigma did not predict concealment (b = 0.04, t46 = 0.23, P = .82, partial η2 = 0.001, 95% CI, −0.28 to 0.35). Because one item on the concealment scale asked about concealment at work and it may not have been clear how to answer this item for participants who were not working, we recalculated the concealment scale without this item and repeated the analyses. No substantive differences emerged.
In addition to stigma, disabled work status was associated with lower concealment (b = −0.68, t46 = −2.84, P = .007, partial η2 = 0.15, 95% CI, −1.16 to −0.20). Among the other covariates, neither sex (b = −0.12, t46 = −0.47, P = .64, partial η2 = 0.01, 95% CI, −0.62 to 0.39) nor years since diagnosis (b = −0.03, t46 = −1.67, P = .10, partial η2 = 0.06, 95% CI, −0.06 to 0.01) emerged as significant predictors of concealment in the complete model. Interactions were nonsignificant between the block of stigma variables and years since diagnosis (R2 change = .01, F3,43 = 0.29, P = .83) and disability status (R2 change = .01, F3,43 = 0.33, P = .80) in predicting concealment, suggesting that the association of stigma with concealment did not depend on how long participants in this sample had MS or whether the illness prevented them from working.
A final set of analyses explored potential health behaviors predicted by concealment. We separately regressed drinking frequency, physician delay, and therapy delay on concealment, including the same set of covariates as mentioned previously herein (ie, sex, work disability status, and years since MS diagnosis). Concealment was associated with delaying needed physician visits (b = 0.31, t48 = 1.98, P = .05, partial η2 = 0.08, 95% CI, −0.01 to 0.62). It was also associated with greater drinking frequency and delaying medical therapy, but these effects did not reach significance (P ≤ .15), most likely because of the limited statistical power available given the sample size.
Discussion
Although perceptions of stigma were relatively low overall, it is notable that most participants reported experiencing at least some stigma, and some experienced a substantial amount. Participants were most likely to feel isolation stigma and anticipated stigma. It was relatively less common for people to internalize negative perceptions about their MS. In fact, the modal response to internalized stigma was the lowest scale response. These results suggest that participants were concerned with negative perceptions and treatment by others, particularly insomuch as this resulted in being socially isolated, but they did not generally internalize negative social perceptions. Thus, at least at the level of personal identity, participants did not feel “less than” because of their MS.
Efforts at concealment were common, with approximately 20% of participants indicating concealment efforts above the scale midpoint. In a multiple regression analysis, concealment was strongly predicted by anticipated stigma such that higher levels of anticipated stigma were associated with greater efforts toward disease concealment. In fact, nearly half the variance in concealment was predicted from the statistical model, with 29% predicted from the stigma scales. In this sample, concealment was not strongly associated with internalized stigma or isolation stigma, suggesting that concealment is primarily motivated by a concern about bias.
The possibility of concealing MS provides individuals with a behavioral coping strategy that may help avoid negative interpersonal interactions or becoming a target of bias and discrimination. However, the continual self-monitoring that concealment requires can be stressful and interfere with health behaviors. For instance, previous research has found that people who conceal may avoid needed doctor visits3 and find treatment adherence more challenging. In the present research, we found significant positive bivariate correlations between concealment and 1) the consumption of alcoholic beverages (suggesting that concealment is stressful) and 2) delaying needed physician visits. We also found a positive but nonsignificant association between concealment and delaying medication therapy. After controlling for sex, disabled work status, and years with MS, only the association between concealment and drinking behavior approached significance. Nevertheless, the associations for the other variables were in the expected direction, suggesting that nonsignificant results may have been due to the limited sample size.
The pattern of associations between concealment and health behaviors found in this sample, coupled with results from previous research, may help explain why approximately 10% of patients with MS have never used disease-modifying therapies and more than a third do not currently use them.28 Because disease-modifying MS medications can limit lesion formation and help prevent brain atrophy,29 it may be important to start such therapies early, before permanent damage develops.30,31 If concealment contributes to delays or interruptions in MS treatment, as preliminarily suggested herein, it could exacerbate long-term disease progression. More research with larger samples is needed to investigate these possibilities and to determine individual differences and environmental factors that predict if or how concealment shifts from a protective coping strategy to one that interferes with health outcomes.
The present research contributes to the literature by considering different dimensions of stigma and their relation to concealment. However, data were collected from a small convenience sample at a single point in time. Thus, results provide a preliminary snapshot of stigma concerns and their relation to concealment but may not be an accurate estimate of stigma and concealment rates in the larger population of people with MS. Studies with larger samples and a longitudinal design will contribute to a better understanding of the prevalence of stigma and concealment in individuals living with MS and clarify the causal relations between concealment and health behaviors. Such research is important for developing effective intervention strategies to help patients cope effectively with MS stigma and potentially increase their use of existing treatments. Possible intervention strategies include psychological approaches that help individuals cope with the stress of MS stigma and manage decisions to conceal or disclose. They can also include educational and procedural approaches directed at clinicians and the general public to help reduce social stigma, promote culturally competent care, and increase social support.32
PracticePoints.
People with chronic illnesses often feel stigmatized, which can have significant effects on health behaviors and disease progression, but the small amount of quantitative research addressing this topic in people with MS has tended to use scales that either conflate or omit relevant dimensions of stigma.
Most participants reported experiencing at least some stigma, and some experienced a substantial amount. Participants were concerned with negative perceptions and treatment by others, particularly insomuch as this resulted in social isolation; efforts at concealment were common.
Culturally competent care of patients with MS may warrant consideration of social stigma and concealment and how these may affect treatment plans and disease progression.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This study was supported by pilot grants from the Consortium of Multiple Sclerosis Centers and the National Multiple Sclerosis Society.
References
- 1.Rejdak K, Jackson S, Giovannoni G. Multiple sclerosis: a practical overview for clinicians. Br Med Bull. 2010;95:79–104. doi: 10.1093/bmb/ldq017. [DOI] [PubMed] [Google Scholar]
- 2.Stüve O, Oksenberg JR. Multiple sclerosis: overview. In: Pagon R, Bird T, Dolan C, editors. GeneReviews [Internet] Seattle, WA: University of Washington; 2011. et al., eds. [Google Scholar]
- 3.Earnshaw VA, Quinn DM. The impact of stigma in healthcare on people living with chronic illnesses. J Health Psychol. 2012;17:157–168. doi: 10.1177/1359105311414952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dovidio JF, Major B, Crocker J. Stigma: introduction and overview. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The Social Psychology of Stigma. New York, NY: Guilford Press; 2000. pp. 1–28. [Google Scholar]
- 5.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 6.Earnshaw VA, Quinn DM, Kalichman SC, Park CL. Development and psychometric evaluation of the Chronic Illness Anticipated Stigma Scale. J Behav Med. 2013;36:270–282. doi: 10.1007/s10865-012-9422-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Molina Y, Choi SW, Cella DF, Rao D. The stigma scale for chronic illnesses 8-item version (SSCI-8): development, validation and use across neurological conditions. Int J Behav Med. 2013;20:450–460. doi: 10.1007/s12529-012-9243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- 9.Grytten N, Måseide P. “What is expressed is not always what is felt”: coping with stigma and the embodiment of perceived illegitimacy of multiple sclerosis. Chronic Illn. 2005;1:231–243. doi: 10.1177/17423953050010030601. [DOI] [PubMed] [Google Scholar]
- 10.Crandall CS. Ideology and lay theories of stigma: the justification of stigmatization. In: Heatherton TF, Kleck RE, Hebl MR, editors. The Social Psychology of Stigma. New York, NY: Guilford Press; 2000. pp. 126–150. [Google Scholar]
- 11.Vickers MH. Illness onset as status passage for people with multiple sclerosis (MS) J Health Hum Serv Adm. 2010;33:193–227. [PubMed] [Google Scholar]
- 12.Joachim G, Acorn S. Stigma of visible and invisible chronic conditions. J Adv Nurs. 2000;32:243–248. doi: 10.1046/j.1365-2648.2000.01466.x. [DOI] [PubMed] [Google Scholar]
- 13.Grytten N, Måseide P. “When I am together with them I feel more ill”: the stigma of multiple sclerosis experienced in social relationships. Chronic Illn. 2006;2:195–208. doi: 10.1177/17423953060020030101. [DOI] [PubMed] [Google Scholar]
- 14.Looper KJ, Kirmayer LJ. Perceived stigma in functional somatic syndromes and comparable medical conditions. J Psychosom Res. 2004;57:373–378. doi: 10.1016/j.jpsychores.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Rao D, Choi S, Victorson D et al. Measuring stigma across neurological conditions: the development of the Stigma Scale for Chronic Illness (SSCI) Qual Life Res. 2009;18:585–595. doi: 10.1007/s11136-009-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13:1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cella DF, Dineen K, Arnason B, Reder A. Validation of the functional assessment of multiple sclerosis quality of life instrument. Neurology. 1996;47:129–139. doi: 10.1212/wnl.47.1.129. [DOI] [PubMed] [Google Scholar]
- 18.Gold SM, Heesen C, Schulz H, Guder U. Disease specific quality of life instruments in multiple sclerosis: validation of the Hamburg Quality of Life Questionnaire in Multiple Sclerosis (HAQUAMS) Mult Scler. 2001;7:119–130. doi: 10.1177/135245850100700208. [DOI] [PubMed] [Google Scholar]
- 19.Gupta ND, Jürges H. Do workers underreport morbidity? the accuracy of self-reports of chronic conditions. Soc Sci Med. 2012;75:1589–1594. doi: 10.1016/j.socscimed.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 20.Cole SW, Kemeny ME, Taylor SE, Visscher BR. Accelerated course of human immunodeficiency virus infection in gay men who conceal their homosexual identity. Psychosom Med. 1996;58:219–231. doi: 10.1097/00006842-199605000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Sedlovskaya A, Purdie-Vaughns V, Eibach RP, LaFrance M, Romero-Canyas R, Camp N. Internalizing the closet: concealment heightens the cognitive distinction between public and private selves. J Pers Soc Psychol. 2013;104:695–715. doi: 10.1037/a0031179. [DOI] [PubMed] [Google Scholar]
- 22.US Census Bureau. Statistical Abstract of the United States: 2012. 131st ed. Washington, DC: US Census Bureau; 2012. [Google Scholar]
- 23.Hohol MJ, Orav EJ, Weiner HL. Disease steps in multiple sclerosis: a longitudinal study comparing disease steps and EDSS to evaluate disease progression. Mult Scler. 1999;5:349–354. doi: 10.1177/135245859900500508. [DOI] [PubMed] [Google Scholar]
- 24.Marrie RA, Goldman M. Validity of performance scales for disability assessment in multiple sclerosis. Mult Scler. 2007;13:1176–1182. doi: 10.1177/1352458507078388. [DOI] [PubMed] [Google Scholar]
- 25.Cataldo JK, Slaughter R, Jahan TM, Pongquan VL, Hwang WJ. Measuring stigma in people with lung cancer: psychometric testing of the Cataldo Lung Cancer Stigma Scale. Oncol Nurs Forum. 2011;38:E46–E54. doi: 10.1188/11.ONF.E46-E54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DiIorio C, Osborne Shafer P, Letz R, Henry T, Schomer DL, Yeager K. The association of stigma with self-management and perceptions of health care among adults with epilepsy. Epilepsy Behav. 2003;4:259–267. doi: 10.1016/s1525-5050(03)00103-3. [DOI] [PubMed] [Google Scholar]
- 27.Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003;121:31–49. doi: 10.1016/j.psychres.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Buchanan RJ, Zuniga MA, Carrillo-Zuniga G et al. Comparisons of Latinos, African Americans, and Caucasians with multiple sclerosis. Ethn Dis. 2010;20:451–457. [PubMed] [Google Scholar]
- 29.Calabrese M, Bernardi V, Atzori M et al. Effect of disease-modifying drugs on cortical lesions and atrophy in relapsing-remitting multiple sclerosis. Mult Scler. 2012;18:418–424. doi: 10.1177/1352458510394702. [DOI] [PubMed] [Google Scholar]
- 30.Goodin DS, Bates D. Treatment of early multiple sclerosis: the value of treatment initiation after a first clinical episode. Mult Scler. 2009;15:1175–1182. doi: 10.1177/1352458509107007. [DOI] [PubMed] [Google Scholar]
- 31.Kappos L, Freedman MS, Polman CH et al. Effect of early versus delayed interferon beta-1b treatment on disability after a first clinical event suggestive of multiple sclerosis: a 3-year follow-up analysis of the BENEFIT study. Lancet. 2007;370:389–397. doi: 10.1016/S0140-6736(07)61194-5. [DOI] [PubMed] [Google Scholar]
- 32.Cook JE, Purdie-Vaughns V, Meyer IH, Busch JTA. Intervening within and across levels: a multilevel approach to stigma and public health. Soc Sci Med. 2014;103:101–109. doi: 10.1016/j.socscimed.2013.09.023. [DOI] [PubMed] [Google Scholar]


