Abstract
This article examines how nations split decision-making about health services between federal and sub-federal levels, creating variation between states or provinces. When is this variation ethically acceptable? We identify three sources of ethical acceptability—procedural fairness, value pluralism, and substantive fairness—and examine these sources with respect to a case study: the fact that only 30 out of 51 US states or territories passed mandates requiring private insurers to offer extensive coverage of autism behavioral therapies, creating variation for privately insured children living in different US states. Is this variation ethically acceptable? To address this question, we need to analyze whether mandates go to more or less needy states and whether the mandates reflect value pluralism between states regarding government’s role in health care. Using time-series logistic regressions and data from National Survey of Children with Special Health Care Needs, Individual with Disabilities Education Act, legislature political composition, and American Board of Pediatrics workforce data, we find that the states in which mandates are passed are less needy than states in which mandates have not been passed, what we call a cumulative advantage outcome that increases between-state disparities rather than a compensatory outcome that decreases between-state disparities. Concluding, we discuss the implications of our analysis for broader discussions of variation in health services provision.
Keywords: autism, distributive justice, ethics, health policy, private insurance mandates
Introduction
The cost of services for a child or adolescent with an autism spectrum disorder (ASD) is considerable, with estimates ranging from a mean of approximately US$6000 per child (Leslie and Martin, 2007) to as high as US$35,000 per child for children in the first 5 years of life (Ganz, 2007). These costs raise questions about the role the government should play in either financing these services themselves or requiring private entities to finance these services. This article focuses on one particular issue at the intersection of government decision-making and autism policy: ethical issues that arise when decision-making over health policy is split between federal and sub-federal levels, with the split creating variation in autism health services between states or provinces in a given nation.
The issue has arisen in contexts that split health-care policymaking between federal and sub-federal levels such as Canada, Australia, and, this article’s focus, the United States. In Canada, although the Canada Health Act of 1984 establishes federal-level principles such as universality and comprehensiveness, provinces are responsible for enacting and funding policies that comply with these principles (Allin, 2008). The country therefore faces significant debates about which treatments fall under this federal guarantee and which do not (Allin, 2008). The debate became salient with respect to autism when in a 2004 case, Auton v. British Columbia, the Canadian Supreme Court ruled that persons with autism had no federally guaranteed right to intensive behavioral interventions for their condition (Auton v. British Columbia, 2004). The devolvement of decision-making to the provincial level thus creates variation in autism coverage and ethical questions about whether this variation is acceptable.
Similarly, despite Australia’s universal coverage scheme, individual states have some leeway regarding which interventions to cover, with some commentators arguing that split decision-making is “perhaps its [Australia’s] largest source of [healthcare] inefficiencies and inequities” (Peacock and Segal, 1999: 21). For autism, Australian states differ in which treatments they fund versus expect persons to pay for out-of-pocket (Roberts, 2003), the number of years for which they guarantee funding for intensive behavioral treatments (Roberts, 2003), and whether or not they have passed special, autism-specific legislation that guarantees more generous funding (Roth, 2013).
Therefore, although this article focuses on one case study where these issues are salient—the passage of US state–level mandates for private insurance coverage of intensive behavioral treatments—we believe the analysis is generalizable to any context in which (1) decision-making over health policy is split between a centralized federal level and a de-centralized state/provincial/territorial level, and (2) even if the nation has universal, federally guaranteed health coverage, sub-federal entities have some decision-making power over which interventions fall under the guarantee versus which do not.
Of course, different federations will have different amounts of variation in health policies. Countries with more robust federally guaranteed health coverage may only have variation in citizens’ access to “marginal” services such as pharmaceuticals, dental coverage, or interventions with contested evidence. Countries with less robust federally guaranteed health coverage, such as the United States, may have wide amounts of variation between states in both which citizens access any care and what care those citizens access. Therefore, ethical issues created by variation between states/provinces within a nation will be present across many contexts but more or less acute depending on the robustness of federally guaranteed health-care coverage.
The question that variation in health policies between sub-federal entities creates is: when is it ethically acceptable for a government to enact policy at a de-centralized state level rather than a centralized federal level? Drawing upon Greer and Jacobson (2010), we argue that there are three ways in which policy enacted at the sub-federal level could be ethically acceptable. First, if the policy reflects procedural fairness—does the policy reflect state responsiveness to the preferences of citizens in a way that a centralized, federal entity may not? Second, if the policy reflects value pluralism—does the policy stem from the values of citizens in different states about the government’s proper role in the regulation of health services? Third, if the policy results in substantive fairness—does the policy address the needs of vulnerable populations more quickly or more robustly than a federal entity? These principles are salient anytime policy enacted at the sub-federal level means that persons with a similar condition living in different states have unequal access to a beneficial intervention.
Having outlined these principles, we now turn to our concrete case study: US state–level mandates that require private insurers in the state to cover potentially costly autism behavioral therapies. Over the past decade, US state legislatures have passed insurance mandates to help alleviate some of costs of intensive autism services for families schools, and public insurance programs such as Medicaid. Autism insurance legislation often explicitly requires coverage of Applied Behavior Analysis (ABA), a group of therapies that focus on improving children’s language, social, and academic skills and that clinicians recommend should be started before the age of 5 years and should be implemented at the intensity of 20 h or more per week (Vismara and Rogers, 2010).
These intensive behavioral interventions targeted by the mandates can cost between US$10,000 and US$100,000 per year (Bouder et al., 2009; Zane et al., 2008). As a result, private insurers have been reluctant to cover ABA and other expensive behavioral treatments, with some insurers arguing that these forms of treatment are experimental, not “medically necessary,” or learning services that should be financed under the rubric of special education rather than medical services that should be financed by health insurance (Bussey v. Corning Life Serv., Inc., 2000; Dicker and Bennett, 2011; Stuart, 2012; Wang et al., 2013). Meanwhile, US states and school districts are reluctant to provide financing for ABA and other behavioral therapies, and courts have not required districts to provide ABA as part of the child’s individualized education plan (IEP) as long as the school covers an alternative program that gives the child some meaningful benefit (Lt. T.B. v. Warwick School Committee, 2004; Zirkel, 2011). Furthermore, although the goals of special education interventions—to improve the child’s educational functioning—may overlap with the goals of certain rehabilitative or habilitative “medical” treatments, these goals may not fully overlap, and splitting care between medical and educational settings can lead to problematic fragmentation in care delivery. As a result, coverage for expensive autism services before the passage of mandates seems to be largely borne by government-funded Medicaid programs (Wang et al., 2013), leading commentators to underscore the importance of mandates forcing private insurers into more generous reimbursement of autism services (Wang et al., 2013), especially as state Medicaid programs experience increasing budget constraints (Stein et al., 2012).
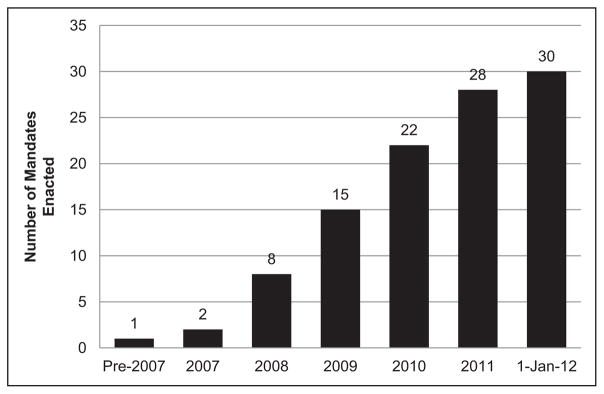
Responding to these problems, a number of US states, gaining momentum in 2007, enacted autism insurance reform legislation, a legislative goal that has been the focus of Autism Speaks, a well-financed autism advocacy group founded in February 2005 (Autism Speaks, 2013; Singh et al., 2009). Before 2005, only one state—Indiana—had passed legislation mandating private insurance coverage for autism services, but from 2005 to January 2012, 29 additional states passed autism insurance reform laws (see Figures 1 and 2) (National Conference of State Legislatures (NCSL), 2012). The clearest causal factor for the passage of the autism state insurance mandates is the formation of the patient advocacy group, Autism Speaks. However, Autism Speaks and its sister organization, Autism Votes, which focuses on state and federal legislative activities, have chapters in every state, yet only 59% of states and territories (30 out of 51) have passed legislative mandates as of the January 2012 cutoff of our analysis. What explains the differential passage of these mandates? And more importantly, since privately insured children living in a state where an insurance mandate is passed will likely have access to a wider breadth and greater depth of services than privately insured children in states without such a mandate, is the between-state variation the mandates create ethically acceptable? The mandates may force private insurers to cover a larger breadth of services that include behavioral treatments and/or to cover these services more generously, correcting inequity between children able to qualify for Medicaid-based autism services and those relying on private insurance. But assuming that ABA provides some meaningful benefit to children with autism, the mandates may create new equity issues between children in states with a mandate and children in states without a mandate.
Figure 1.
Cumulative number of mandates enacted by year.
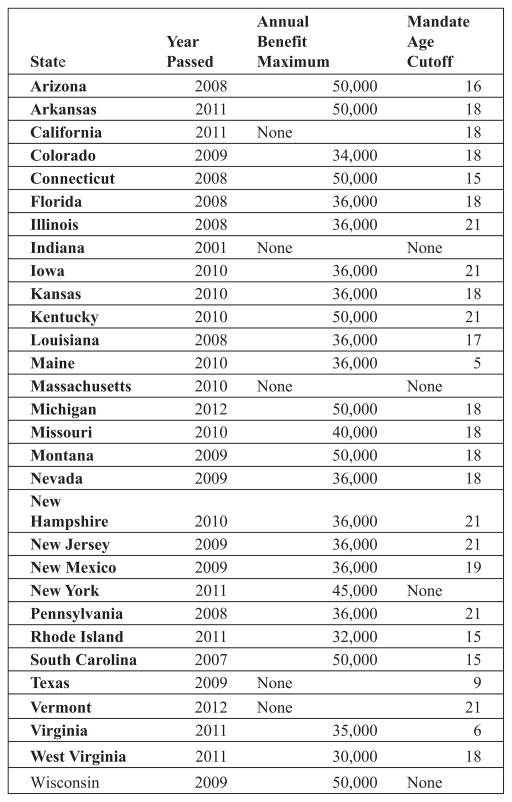
Figure 2.
State-level variation in mandates.
To examine the ethical acceptability of autism insurance mandates and the variation between states the mandates create, we examine the mandate’s passage with attention to the three sources of ethical acceptability for state variation discussed above: do the mandates reflect procedural responsiveness, stem from value pluralism between citizens in different states, and address the needs of vulnerable populations? To answer these questions, we must examine why some states pass mandates and others do not. Do the mandates reflect value pluralism about the proper role of government in health services? Do the states that pass mandates have more vulnerable autism populations? These questions remain unanswered by existing research, which has investigated the impact of autism insurance mandates on insurance premiums (Bouder et al., 2009) and the effect of the mandates on utilization of Medicaid services for autism (Stein et al., 2012), but has not investigated factors that contribute to the passage of a mandate or the comparative “neediness” of the states in which mandates are passed.
This article addresses this gap in the literature, examining why some US states have passed autism insurance mandates and asking whether these reasons for a mandate’s passage make the variation the mandates create ethically acceptable. While our data are from the US context, we have argued that our analysis offers insight into broader debates in any system in which sub-federal entities have some decision-making over coverage of health interventions.
Methods
Data
Data are derived from different sources that span across the years 2005–2012, years in which many of the mandates were passed and for which publicly available data exist. As we discuss more fully in the “Discussion” section, our variables are intended to map on to three aspects of the mandates’ acceptability: (1) procedural fairness (the dependent variable if a mandate was passed at all), (2) value pluralism (the political composition of a state’s legislature), and (3) substantive fairness (the prevalence of autism in a state, the density of pediatricians, and a state’s median income).
Examining these variables, first, estimations of the prevalence of autism within each state are from the National Survey of Children with Special Health Care Needs (NS-CSHCN) (CDC/National Center for Health Statistics, 2013). The survey uses a random digit dialing sampling method, where telephone numbers are randomly called to identify households with one or more children under the age of 18 years. In each household, one child is randomly selected to be the subject of the interview. Approximately 750 interviews are conducted per state, and the results are weighted to represent the population of non-institutionalized children aged 0–17 years nationally and in the state. Our model uses data from the 2005–2006 and 2009–2010 surveys, examining parental responses by state to the following question: “To the best of your knowledge, does your child currently have Autism or Autism Spectrum Disorder, that is ASD (Ages 0–17)” (2005–2006) and “For each condition [autism or autism spectrum disorders], please tell me if a doctor or other provider ever told you that your child had the condition, even if (he/she) does not have the condition now (Ages 2–17)” (2009–2010).
Estimates of the number of children receiving special education services for autism are derived from the Individual with Disabilities Education Act (IDEA) child count data, which provides yearly counts of special education services for 2005 through 2010 separated by the type of disability diagnosis (Data Accountability Center, 2011). For children with multiple diagnoses, the data classify the child according to his or her primary diagnosis. IDEA child counts for the primary diagnosis of autism are often used as a proxy for the prevalence of autism (e.g. Kao et al., 2010). However, these IDEA counts will likely underestimate the prevalence of autism: one surveillance study of autism in a given area suggests that over 91% of children aged 6–10 years in that area received special education services, but only 48% of those children have autism as their primary special education classification (Newschaffer et al., 2005). Yet because there are no data suggesting that some states’ IDEA counts may underestimate the prevalence of autism more than other states’ IDEA counts, the data can still serve as a useful proxy measure for comparing between-state differences in autism prevalence.
Estimates of the density of general pediatricians in a given state from 2005 to 2012 were derived from American Board of Pediatrics (ABP) workforce data. The ABP tracks the board-certified pediatrician workforce through multiple methods, including a tracking system for pediatric residents and a questionnaire given to persons who take the general pediatrics certifying examination (Nichols, 2013). Yearly data were obtained from the ABP master file and are given as the number of general pediatricians per 10,000 children, with estimates of the child population derived from US census data of persons under the age of 18 years. Data on autism service utilization suggest that pediatricians are the type of health-care provider seen by the highest proportion of children with autism (as compared to psychiatrists, for example) (Croen et al., 2006), so the availability of general pediatricians in a given state is one indication of the state’s robustness of autism health infrastructure.
The state’s political affiliation was derived from NCSL data (NCSL, 2013). To estimate political affiliation, we created a composite variable for each state that took into account the governor’s political affiliation, the state senate majority affiliation, and state house majority affiliation. Each political area was given a score of either 0 = Democrat, 1 = Independent, or 2 = Republican. The composite variable ranged from 0 (most liberal, all affiliations were Democrat) to 6 (most conservative, all affiliations were Republican). Then, for ease of interpretation, we separated states into Democrat-leaning legislatures (0–2 points) versus Republican-leaning legislatures (4–6 points).
Another important state-level variable is the percent of private insurance plans in the state that are exempt from state mandates. The Employee Retirement Income Security Act (ERISA) of 1973 exempts self-insured plans from state insurance benefits legislation (United States Department of Labor, 2013), and up to half of privately employed employees in a state may be exempt from mandates (Buchmueller et al., 2007). Data on the percent of exempt private plans are provided by the 2010 version of the Medical Expenditure Panel Survey (MEPS) (Agency for Healthcare Research and Quality, 2013). The total number of other insurance mandates a state has also may be a predictive variable for the presence or absence of an autism insurance mandate in a given state; these data are derived from the Council for Affordable Health Insurance (CAHI), which performs a yearly survey of state-level insurance mandates (Bunce and Wieske, 2010). A state’s median income was measured using data from the US Census Bureau (2012).
For the model using IDEA counts as a proxy for autism prevalence, since each state is granted the power under IDEA to define its own specific criteria under the general federal disability criteria of “autism,” we coded variations in the state’s special education criteria for autism based on MacFarlane and Kanaya’s (2009) analysis of state autism special education criteria. A total of 20 states explicitly included two ASDs—Asperger’s syndrome and Pervasive Developmental Disorder, Not Otherwise Specified (PDD-NOS)—in their autism special education criteria and 31 states do not explicitly include these disorders in their criteria. States including ASDs were labeled as having “generous” special education criteria.
Finally, the presence or absence of a state mandate for autism coverage is coded using data from state legislative statutes (for a list, see NCSL, 2013) (Figure 2).
Analyses
Our dataset is composed of longitudinal data, where characteristics such as the prevalence of autism and the density of pediatricians both vary across states and vary across time. Since each state in our sample is observed across multiple years, there are likely unobserved characteristics of a state that influence the passage of a mandate. Therefore, we use a time-series model to control for time effects and state-specific effects (STATA’s xtlogit model). The model estimates the following equation where the dependent variable is the likelihood of a mandate’s passage in a given state (i) in a given year (t). The independent predictor variables include a state’s prevalence of autism (measured either using NS-CSHCN autism prevalence rates or IDEA autism prevalence rates), density of pediatricians, median income, percent of private insurance plans exempt from mandates under ERISA, total number of insurance mandates, political affiliation, and, for the model that uses IDEA prevalence criteria, the generosity of special education criteria in the state. The model has the advantage over a standard logit model of not only analyzing how differences between states predict a state’s passage or non-passage of a mandate, but also analyzing how changes over time affect the likelihood of a state passing a mandate. It also takes into account when a mandate is passed during 2005–2012 in addition to if a mandate is passed during that time period:
Our analysis uses STATA version 13.0 (2013).
Results
Table 1 shows descriptive information for each of the variables included in the models. This table illustrates increases in the prevalence of autism between the beginning of the measurement period (2005) and the end of the measurement period (2012) in both the NS-CSHCN autism prevalence data and the IDEA autism counts, as well as increases in the ratio of general pediatricians per child. States are split between Democrat- and Republican-leaning legislatures (41.18% vs 58.82%, respectively) and having generous special education criteria for the autism category and non-generous criteria (39.22% vs 60.78%, respectively).
Table 1.
Means and SDs for variables in models.
| Variable | Mean (SD) |
|---|---|
| NS-CSHCN autism prevalence | |
| 2005–2006 | 5.19 (1.54) |
| 2009–2010 | 7.76 (2.17) |
| Change from 2005 to 2009 | +2.58 (1.69) |
| IDEA autism prevalence | |
| 2005–2010 | 3.44 (1.25) |
| Change from 2005 to 2010 | +0.47 (0.77) |
| General pediatricians per 10,000 children | |
| 2005–2012 | 6.83 (2.87) |
| Change from 2005 to 2012 | +1.37 (1.00) |
| State median income | 50,738.22 (7558) |
| Percent of private insurance plans exempt from mandates under ERISA | 36.38 (5.76) |
| Total state mandates | 44.35 (13.62) |
| Variable | Percent of states |
|---|---|
| State legislature political affiliation | |
| 0–2 (Democrat) | 41.18 |
| 3 (Independent) | 0 |
| 4–6 (Republican) | 58.82 |
| Special education generosity | |
| Not generous | 60.78 |
| 39.22 | |
SD: standard deviation; NS-CSHCN: National Survey of Children with Special Health Care Needs; IDEA: Individual with Disabilities Education Act; ERISA: Employee Retirement Income Security Act.
Table 2 shows the results of two sets of logit models: first, a logit model that uses NS-CSHCN autism prevalence data; second, a logit model that uses IDEA autism child counts. The first model shows three significant predictor variables. First, the prevalence of autism is associated with significant increases in the likelihood of a mandate’s passage (p < 0.001). Holding the other variables constant, we see that a one-unit increase in autism prevalence results in an 11-fold increase in the likelihood of a mandate’s passage. Second, the density of pediatricians also significantly increased the likelihood of a mandate’s passage (p < 0.001); a one-unit increase in the number of pediatricians per 10,000 children results in a fourfold increase in the likelihood of a mandate’s passage. In contrast, an increase in a state’s median income is associated with a decrease in the likelihood of a mandate’s passage (p < 0.01).
Table 2.
Logistic regression models for the likelihood of a mandate’s passage.
| Predictor | NS-CSHCN prevalence data
|
IDEA prevalence data
|
||||
|---|---|---|---|---|---|---|
| B | SE B | Odds ratio | B | SE B | Odds ratio | |
| Autism prevalence | 2.41*** | 0.56 | 11.13*** | 2.51*** | 0.60 | 12.43*** |
| Pediatrician density | 1.53*** | 0.34 | 4.63*** | 1.96*** | 0.37 | 7.12*** |
| Median income | −0.0004** | 0.0002 | 0.99** | −0.0004** | 0.0002 | 0.99** |
| Number of state mandates | 0.09 | 0.07 | 1.09 | 0.04 | 0.07 | 1.04 |
| Percent of plans exempt from mandates under ERISA | 30.34 | 18.42 | 0 | 23.02 | 19.49 | 0 |
| Republican political affiliationa | 1.35 | 2.19 | 3.87 | 4.95* | 2.22 | 141.04* |
| Generosity of special education criteriaa | – | – | – | −1.71 | 1.95 | 0.18 |
| Constant | −24.18 | 13.07 | −18.00 | 13.57 | ||
| χ2 | 27.99*** | 44.04*** | ||||
| df | 6 | 7 | ||||
SE: standard error; df: degree of freedom; NS-CSHCN: National Survey of Children with Special Health Care Needs; IDEA: Individual with Disabilities Education Act; ERISA: Employee Retirement Income Security Act.
Reference categories are Democrat (state political affiliation) and not generous (generosity of special education criteria).
p < 0.05;
p < 0.01;
p < 0.001.
The second model offers a more complete picture of state and time characteristics associated with a mandate’s passage, since the IDEA offers prevalence data for more years than the NS-CSHCN. The model shows similar results to the first model, with the same three significant predictor variables: higher autism prevalence and higher pediatrician density associated with a significant increase in the likelihood of a mandate’s passage (p < 0.001), while a higher median income is significantly associated with a decrease in the likelihood of a mandate’s passage (p < 0.01). In addition, the model using IDEA data suggests that a Republican legislature is associated with a significantly increased likelihood of a mandate’s passage (p < 0.05), an unexpected finding we discuss in greater detail below.
Discussion
At the article’s outset, we suggested three ways in which a state mandate for autism insurance coverage and the between-state variation it creates may be ethically acceptable: if the mandates reflect (1) procedural fairness: state responsiveness to citizen demands to pass a mandate; (2) value pluralism: between-state variation in values about the role of government in health care; and (3) substantive fairness: the mandates addressing the needs of vulnerable populations (Greer and Jacobson, 2010). We argue that the mandates reflect procedural fairness—since they stemmed from political organizing efforts by Autism Votes, the mandates certainly reflect a state responding to the concerns that some of its citizens have about private insurance coverage of autism services. Having argued that the mandates fulfill the procedural fairness criteria for ethical acceptability, we now analyze the other two criteria—value pluralism and substantive fairness—more closely.
Value pluralism and autism insurance mandates
First, we can investigate whether the mandates reflect legitimate differences in the values that citizens in different states hold about government’s role in health care. US citizens who identify as Republican (the party in the United States generally associated with fiscal conservatism) are significantly less likely to approve of increased government regulation of the health-care sector and are significantly less likely to agree that the government should guarantee citizens access to health care (Konisky and Richardson, 2013). If these general attitudes about the government’s role in health care apply to specific attitudes about the government’s role in autism, we might predict that states in our sample scoring as more Republican/conservative might have citizens who are more reluctant to regulate private health insurers through the imposition of a government mandate that guarantees reimbursement of specific autism services. However, the model using NS-CSHCN data found no significant differences between Republican- and Democrat-led legislatures in the likelihood of a mandate’s passage. The model using IDEA data found a higher likelihood of Republican-led legislatures passing a mandate than Democrat-led legislatures (p < 0.05). This predictor variable, though statistically significant, displayed a much weaker association with the likelihood of a mandate’s passage than two other predictor variables: the prevalence of autism in a state and the density of pediatricians, and unlike the two other variables, were not consistent across models. Therefore, the passage of autism state mandates seems to only weakly reflect value pluralism about the role of government in health care.
Substantive fairness and autism insurance mandates
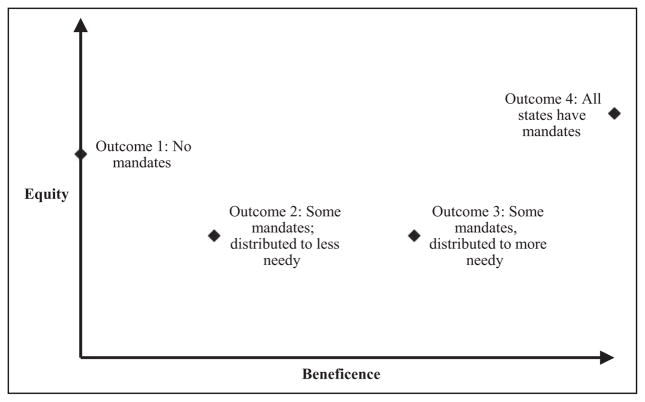
Arguably more important than the mandate’s promotion of procedural fairness or reflection of value pluralism is the third criterion for assessing the mandates’ ethical acceptability: their substantive fairness. We argue that substantive fairness can be broken down into two dimensions: do the mandates minimize the extent to which the services a person receives depend on the state in which he lives (the equity component of substantive fairness), while maximizing the number of persons with autism helped by the mandate’s provision (beneficence component of substantive fairness)? Furthermore, it seems that we ought to prioritize beneficence over equity—that is, it is better for the mandates to exist and help some children with autism than for the mandates to not exist and help no children with autism.
We can use each of these components of substantive fairness to plot four outcomes of the mandates’ existence and distribution (Figure 3), which we rank below:
Figure 3.
Autism state coverage policy matrix.
No US states have private insurance mandates.
Some US states have private insurance mandates and these mandates are distributed to states with an autism population that needs the mandates less (“less needy” states, with mandates having a cumulative advantage effect).
Some US states have private insurance mandates and these mandates are distributed to states with an autism population that needs the mandates more (“more needy” states, with mandates having a compensatory effect).
All US states have private insurance mandates.
Clearly, the mandates neither reflect outcome 1 nor outcome 4, since some states have passed mandates while others have not. Therefore, we can either characterize the mandates as outcome 2—less needy states pass mandates—or as outcome 3—more needy states pass mandates. Which of these represents a more accurate characterization of the US states that pass private insurance mandates compared to the states that do not?
We argue that we can define the neediness of a US state for an autism insurance mandate with reference to three of the predictor variables from our models: the state’s autism prevalence, the state’s density of pediatricians, and the state’s median income. Examining which of these variables predict a mandate’s passage, we can investigate whether the mandates go to less needy states and have what we call a cumulative advantage effect, where they help states with stronger existing autism infrastructure further improve that infrastructure by bringing more funding to autism treatment. Or, the mandates may go to more needy states and have a compensatory effect, where they help states with weaker existing autism infrastructure compensate for that weakness and improve services through increased funding availability. Now, we turn to our predictor variables.
First is autism prevalence—what is the relationship between the prevalence of autism in a state and its degree of neediness for an autism mandate? One intuitive answer is that the higher a state’s autism prevalence, the more the state needs a mandate. Yet this intuitive answer fails to distinguish between a state’s actual prevalence of autism—the number of children who suffer from autism’s deficits and impairments—and the state’s identified prevalence of autism, also referred to as a state’s administrative or measured prevalence. Unless state-specific environmental factors play a large role in autism’s etiology, the actual prevalence of autism should not vary widely between states. Yet the identified prevalence of autism does vary substantially between states. While our dataset only included state-level demographic variables, research examining individual factors contributing to higher identified prevalence of autism points to higher parental socioeconomic status (Durkin et al., 2010), higher levels of parental education (Kogan et al., 2009), and white, non-Hispanic race (Kogan et al., 2009). Community-level factors that predict a higher identified prevalence of autism include producing more revenue as a school district (Palmer et al., 2005), the strength of the autism health infrastructure via pediatricians and school districts (Eyal et al., 2010: 44–45; Mandell and Palmer, 2005), and greater economic resources in the community (measured by median property values), especially during early, rapid increases in the prevalence of less severe forms of autism (King and Bearman, 2011). Combining these data on individual- and community-level contributors to identified prevalence rates, we contend that states with a higher identified prevalence of autism are less needy than states with a lower identified prevalence of autism, since the former group of states has been shown to have better child health systems in place to detect the presence of autism.
With this definition of neediness in mind, we note that each of the prevalence measures in our models assesses the identified prevalence of autism: NS-CSHCN data ask parents about an existing clinical diagnosis of autism and IDEA data count children receiving autism special education services. Our models find that states with a higher identified prevalence of autism are significantly more likely to pass a mandate (p < 0.001 in each model). Therefore, less needy states—as measured by a higher identified prevalence of autism—are more likely to pass mandates.
The second measure of a state’s neediness—the ratio of general pediatricians per 10,000 children—supports this interpretation. Just as states with a higher identified prevalence of autism are significantly more likely to pass a mandate, states with a higher density of pediatricians are significantly more likely to pass a mandate (p < 0.001 in each model). States’ identified prevalence of autism and pediatrician density are somewhat but not highly correlated (R2 < 0.5), showing some relationship between the two variables but not indicating a high risk of collinearity problems that would affect the interpretation of our regression results. The fact that a model incorporating both the identified prevalence of autism and the pediatrician density found each to significantly increase the likelihood of a mandate’s passage lends support to the idea that less needy states are more likely to pass mandates.
The third predictor variable associated with a state’s neediness—its median income—somewhat complicates this portrait of less needy states displaying a higher likelihood of passing a mandate. In each of our models, lower median income was associated with an increased likelihood of passing a mandate (p < 0.01). Does this finding suggest that states that pass mandates, although they have a higher identified prevalence of autism and a higher density of pediatricians, are actually more needy than states that do not pass mandates? The answer depends on how much weight one places on each component of neediness. Assuming each of the three components has equal weight, we see that the effect of median income is less significant (p < 0.01) than the effects of prevalence and pediatrician density (p < 0.001). Put another way, the relationship between median income and the likelihood of passing a mandate, though statistically significant, requires large differences in median incomes to substantially change the probabilities of a mandate’s passage. For instance, states with a median income in the bottom 25% of states (US$45,000) had a 67% chance of passing a mandate, while states with a median income in the top 25% of states (US$55,000) had a 55% chance of passing a mandate. The difference, though statistically significant, is less than differences in the contribution of prevalence to the passage. For instance, states in the bottom 25% of autism prevalence for 2005 (4.2/100 children) had a 52% chance of passing a mandate by 2012, while states in the top 25% of autism prevalence in 2005 (6.6/100 children) had a 71% chance. These differences highlight that states more needy on two measures—autism prevalence and pediatrician density—are more likely to pass an insurance mandate.
These findings highlight a potential process of substantive unfairness at work. Children living in states with a lower identified prevalence of autism and lower pediatrician density, two characteristics that other studies have linked to certain markers of disadvantage and poor health infrastructure, are less likely to have a state mandate that could provide more robust private insurance financing to spark the development of needed services. Our models incorporating year-specific data suggest that these state characteristics precede the passage of a mandate, but a mandate is likely to continue a given state’s trend of establishing stronger autism services than states that lack a mandate. Indeed, a troubling cycle might occur. First, some states may establish better autism-related health services that result in a higher identified prevalence of autism (Mandell and Palmer, 2005). Second, some parents may move to these states in search of better services, further increasing the well-resourced state’s identified prevalence of autism and decreasing the less-resourced state’s identified prevalence. There are no empirical data of which we are aware on the topic of parental relocation to a different state in search of better autism services, so this link is speculative at this point in time. Third, higher identified prevalence states, according to our models, are more likely to pass a private insurance mandate that likely further widens service disparities between states. This raises issues of substantive fairness between children living in the two types of states, especially those whose parents have less mobility to seek out better autism services. The mandates, rather than compensating for poor service development in some states, seem to widen between-state service disparities.
In sum, our results suggest that the current US mandates resemble outcome 2—less needy states passing mandates—which is less ethically preferable than outcome 3 or outcome 4. However, our ethical analysis argues that outcome 2—some mandates, with those mandates unfairly distributed—is preferable to outcome 1—no state mandates—suggesting that while the existence of the private insurance mandates is not ethically ideal, it is better than no mandated private coverage at all. Combined with the fact that the mandates reflect procedural fairness in a state’s responsiveness to its citizens needs, the mandates are ethically acceptable.
Moving from the US context to other federal entities, our article highlights the need to connect normative reasoning about when variation created by sub-federal policy is ethically permissible with empirical examinations of whom a policy helps and whether those recipients are better or worse off than recipients whose state or province fails to pass a policy. For example, Canada has rejected establishing a national formulary for pharmaceuticals, and researchers have devoted considerable attention to variation between provinces in publicly funded pharmaceutical coverage (e.g. Demers et al., 2008; Pomey et al., 2010). What remains less explored is how the variation may reflect tradeoffs between a province’s responsiveness to citizens, value pluralism about the role of taxpayer-funded coverage of pharmaceuticals, and the level of substantive unfairness the variation creates. Focusing on substantive fairness, commentators could explore the relationship between a province’s generosity of pharmaceutical benefits and the percentage of citizens in that province who already receive robust pharmaceutical coverage through an employer-sponsored plan. Do the provinces that guarantee more generous pharmaceutical benefit schemes for working-age citizens have a lower percentage of citizens receiving employer-sponsored coverage (with the public coverage thus compensating for disadvantage)? Or do generous pharmaceutical benefit schemes go to provinces that are better off in terms of having a higher percentage of citizens with employer-sponsored pharmaceutical coverage, with public coverage creating cumulative advantage for that province? Answering these questions through connecting normative and empirical analyses is important.
Limitations
Our study has several limitations. The most significant limitation is that our data examined aggregate, state-level characteristics associated with the presence of a mandate rather than individual- and community-level factors that likely influence passage of a mandate. Other research aptly documents the link between these individual- and community-level factors and the identified prevalence of autism (e.g. Durkin et al., 2010; King and Bearman, 2011). Future researchers with access to individual- and community-level data could help connect our findings about a state’s identified prevalence of autism increasing the likelihood of a mandate’s passage to analyses of the role of individual- and community-level features and autism-directed political action, especially in predicting which states are earlier versus later adopters of legislation.
Second, we relied on NS-CSHCN and IDEA data for measures of autism’s identified prevalence within a state. Each has limitations as a source of prevalence data. The NS-CSHCN relies on parental self-report of autism diagnoses, though the more recent iteration specifies that the diagnosis should come from a health-care provider, a method that may be less accurate than directly picking up autism “cases” from medical records. Meanwhile, although IDEA data are directly derived from special education records, they miss children diagnosed with autism but who have a different “primary” diagnosis for educational disability coding as well as children educated outside the public school system. Recent autism surveillance networks, such as the Centers for Disease Control and Prevention’s Autism and Developmental Disabilities Monitoring (ADDM) Network, have attempted to incorporate more integrated, record-based surveillance and community screening to overcome these limitations. Yet for now, the NS-CSHCN and IDEA are the only two publicly available sources of which we are aware that provide prevalence data for all 51 states and territories.
Third, in deriving our pediatrician densities from the ABP master file, we may miss up to 17% of clinicians who present themselves as pediatricians but who are not board certified (Freed et al., 2007). However, since commentators promote board certification and recertification as a means of quality improvement (Huang et al., 2013), the density of board-certified pediatricians in a given state is one measure of the robustness of its health infrastructure. Fourth, although our models tracked the likelihood of a mandate’s passage across years and across states, for our special education generosity variable, we used the state special education criteria for autism from 2009. We believe this is not a significant limitation for two reasons: (1) the special education generosity variable ended up not being a significant predictor of a mandate’s passage and (2) these criteria are unlikely to change substantially over time.
Moving from limitations faced by our empirical analysis to issues we did not address in our normative analysis, fifth, our ethical analysis focused on fairness between children with autism living in different states and did not address questions of substantive fairness between children with autism and children with other developmental disorders who may be impacted if a mandate detracts from private insurer generosity toward their condition. Sixth, we assumed for the purposes of this article that in line with evidence reviews, ABA provides some benefit to at least some subset of children with autism who receive the therapy. Therefore, we considered it unfair if a child living in state A received ABA, while a similar child living in state B did not. However, what matters the most morally are not inequalities in health services a child receives but preventable inequalities in health outcomes. As a result, future research should examine how the variation in access to ABA affects health outcomes for children with autism.
Implications
In this article, we explored the ethical acceptability of variation between sub-federal entities in autism services, asking when this variation is more or less ethically acceptable. Using the case study of US private insurance mandates for autism services, we linked three sources of ethical acceptability for variation to characteristics of a state. We found that the mandates reflect procedural fairness of state responsiveness to citizen concerns and a small degree of value pluralism about government’s role in health care, but that the mandates likely create substantive unfairness between children with autism living in more needy, no-mandate states and children with autism living in less needy, mandate states. As we put it, the mandates as they stand create cumulative advantage for some states rather than compensate for a state’s weak autism health infrastructure by spurring service development. However, because the mandates represent an outcome preferable from the standpoint of beneficence toward children with autism than no mandates at all, if one prioritizes beneficence over equity, then this uneven distribution of mandates is ethically preferable to no mandates at all.
Ethical issues surrounding variation in health services will require continued attention as the United States and other federations make coverage decisions amidst national priorities to constrain health-care cost growth. More broadly, this article gestures at the need to combine empirical analyses of health policies with normative analyses of whether those policies widen or reduce existing inequalities. For instance, as the United States goes forward with implementation of the Patient Protection and Affordable Care Act (ACA), which grants states the power to define the specific substance of federally outlined Essential Health Benefits (Cassidy, 2012), only 23 out of 50 US states have explicitly included coverage of autism behavioral treatments when filling out the substance of Essential Health Benefits (Center for Medicare and Medicaid Services, 2013). Investigating the sources of this variation is a topic for further research. Our framework for analyzing the ethical acceptability of different sources of variation in health services provides a starting point for these further analyses of normative issues within health policy.
Acknowledgments
The authors would like to thank Dr Linda Althouse and Cathy Koenig, MS from the American Board of Pediatrics for generous access to their yearly pediatrician workforce data. The authors would also like to thank Dr Bob Wesley for statistical advice.
Funding
This work was supported by the Intramural Research Program of the NIH Clinical Center.
Footnotes
Declaration of conflicting interests
The Authors declare that there are no conflicting interests.
The opinions expressed here are the views of the authors. They do not represent any position or policy of the US National Institutes of Health, the Public Health Service, or the Department of Health and Human Services.
References
- Agency for Healthcare Research and Quality. [accessed 15 May 2013];Medical expenditure panel survey. 2013 Available at: http://meps.ahrq.gov/mepsweb/
- Allin S. Does equity in healthcare use vary across Canadian provinces? Healthcare Policy. 2008;3(4):83–99. [PMC free article] [PubMed] [Google Scholar]
- Autism Speaks. [accessed 15 March 2013];About us: Autism Speaks history. 2013 Available at: http://www.autismspeaks.org/about-us.
- Auton v. British Columbia (2004) 3 S.C.R. 657, 2004 SCC 78. Available at: http://www.canlii.org/en/ca/scc/doc/2004/2004scc78/2004scc78.html
- Bouder JN, Spielman S, Mandell DS. Brief report: quantifying the impact of autism coverage on private insurance premiums. Journal of Autism and Developmental Disorders. 2009;39(6):953–957. doi: 10.1007/s10803-009-0701-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmueller TC, Cooper PF, Jacobson M, et al. Parity for whom? Exemptions and the extent of state mental health parity legislation. Health Affairs. 2007;26(4):w483–w487. doi: 10.1377/hlthaff.26.4.w483. [DOI] [PubMed] [Google Scholar]
- Bunce VC, Wieske JG. Report, Council for Affordable Health Insurance. Alexandria, VA: 2010. Oct, Health insurance mandates in the states. [Google Scholar]
- Bussey v. Corning Life Serv., Inc. (2000) No. 97CV8875, 2000 U.S. Dist. (N.D. Ill. 2000).
- Cassidy A. Health policy brief. Essential health benefits. Health Affairs. 2012 Apr; Available at: http://healthaffairs.org/healthpolicybriefs/brief_pdfs/healthpolicybrief_68.pdf.
- CDC/National Center for Health Statistics. [accessed 20 May 2012];National survey of children with special health care needs. 2013 Available at: http://www.cdc.gov/nchs/slaits/cshcn.htm.
- Center for Medicare and Medicaid Services. [accessed 15 June 2013];Additional information on proposed state Essential Health Benefits benchmark plans. 2013 Available at: http://www.cms.gov/cciio/resources/data-resources/ehb.html#reviewbenchmarks.
- Croen LA, Najjar DV, Ray GT, et al. A comparison of health care utilization and costs of children with and without autism spectrum disorders in a large group-model health plan. Pediatrics. 2006;118(4):e1023–e1211. doi: 10.1542/peds.2006-0127. [DOI] [PubMed] [Google Scholar]
- Data Accountability Center. [accessed 15 May 2012];Individuals with Disabilities Education Act (IDEA) data. 2011 Available at: http://catalog.data.gov/dataset?q=IDEA+Child+Count&sort=score+desc%2C+name+asc&ext_location=&ext_bbox=&ext_prev_extent=-139.21874999999997%2C8.754794702435618%2C-61.87499999999999%2C61.77312286453146.
- Demers V, Melo M, Jackevicius C, et al. Comparison of provincial prescription drug plans and the impact on patients’ annual drug expenditures. Canadian Medical Association Journal. 2008;178:405–409. doi: 10.1503/cmaj.070587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dicker S, Bennett E. Engulfed by the spectrum: the impact of autism spectrum disorders on law and policy. Valparaiso University Law Review. 2011;45(2):415–455. [Google Scholar]
- Durkin MS, Maenner MJ, Meaney FJ, et al. Socioeconomic inequality in the prevalence of autism spectrum disorder: evidence from a U.S. cross-sectional study. PLoS One. 2010;5(7):e11551. doi: 10.1371/journal.pone.0011551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyal G, Hart B, Onculer E, et al. The Autism Matrix. Cambridge: Polity Press; 2010. [Google Scholar]
- Freed GL, Uren RL, Hudson EJ, et al. Who claims to be a pediatrician? Journal of Pediatrics. 2007;150(6):644–658. doi: 10.1016/j.jpeds.2006.12.053. [DOI] [PubMed] [Google Scholar]
- Ganz ML. The lifetime distribution of the incremental societal costs of autism. Archives of Pediatrics & Adolescent Medicine. 2007;161(4):343–349. doi: 10.1001/archpedi.161.4.343. [DOI] [PubMed] [Google Scholar]
- Greer SL, Jacobson PD. Health care reform and federalism. Journal of Health Politics, Policy and Law. 2010;35(2):203–226. doi: 10.1215/03616878-2009-050. [DOI] [PubMed] [Google Scholar]
- Huang JS, Chun S, Sandhu A, et al. Quality improvement in childhood obesity management through the maintenance of certification process. The Journal of Pediatrics. 2013;163(5):1313–1316. e1. doi: 10.1016/j.jpeds.2013.05.011. [DOI] [PubMed] [Google Scholar]
- Kao HT, Buka SL, Kelsey KT, et al. The correlation between the rates of cancer and autism: an exploratory ecological investigation. PLoS One. 2010;5:e9372. doi: 10.1371/journal.pone.0009372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MD, Bearman PS. Socioeconomic status and the increased prevalence of autism in California. American Sociological Review. 2011;76(2):320–346. doi: 10.1177/0003122411399389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kogan MD, Blumberg SJ, Schieve LA, et al. Prevalence of parent-reported diagnosis of autism spectrum disorder among children in the US. Pediatrics. 2009;124(5):1395–1403. doi: 10.1542/peds.2009-1522. [DOI] [PubMed] [Google Scholar]
- Konisky DM, Richardson L. Personal and collective evaluations of the 2010 health care reform. [accessed 23 May 2013];Journal of Health Politics, Policy, and Law. 2013 doi: 10.1215/03616878-2334665. Available at: http://myweb.uiowa.edu/bhlai/workshop/richardson.pdf. [DOI] [PubMed]
- Leslie DL, Martin A. Health care expenditures associated with autism spectrum disorders. Archives of Pediatric & Adolescent Medicine. 2007;161(4):350–355. doi: 10.1001/archpedi.161.4.350. [DOI] [PubMed] [Google Scholar]
- Lt. T.B. v. Warwick School Committee (2004) 361 F.3d 80 (1st Circuit).
- MacFarlane JR, Kanaya T. What does it mean to be autistic? Inter-state variation in special education criteria for autism services. Journal of Child and Family Studies. 2009;18(6):662–669. [Google Scholar]
- Mandell DS, Palmer R. Differences among states in the identification of autistic spectrum disorders. Archives of Pediatrics & Adolescent Medicine. 2005;159(3):266–269. doi: 10.1001/archpedi.159.3.266. [DOI] [PubMed] [Google Scholar]
- National Conference of State Legislatures (NCSL) [accessed 10 May 2013];Insurance coverage for autism. 2012 Available at: http://www.ncsl.org/issues-research/health/autism-and-insurance-coverage-state-laws.aspx.
- National Conference of State Legislatures. [accessed 18 March 2014];Insurance Coverage for Autism. 2012 Available at: http://www.ncsl.org/research/health/autism-and-insurance-coverage-state-laws.aspx.
- Newschaffer CJ, Falb MD, Gurney JH. National autism prevalence trends from united states special education data. Pediatrics. 2005;115(3):e277–e282. doi: 10.1542/peds.2004-1958. [DOI] [PubMed] [Google Scholar]
- Nichols DG. [accessed 20 September 2013];The American Board of Pediatrics 2012–2013 workforce data. 2013 Available at: https://www.abp.org/abpweb-site/stats/wrkfrc/menu1.htm.
- Palmer RF, Blanchard S, Jean CR, et al. School district resources and identification of children with autistic disorder. American Journal of Public Health. 2005;95(1):125–130. doi: 10.2105/AJPH.2003.023077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock S, Segal L. Working paper 98. Centre for Health Program Evaluation; 1999. [accessed 16 February 2014]. Equity and the funding of Australian health services: prospects for weighted capitation. Available at: http://www.buseco.monash.edu.au/centres/che/pubs/wp98.pdf. [Google Scholar]
- Pomey MP, Morgan S, Church J, et al. Do provincial drug benefit initiatives create an effective policy lab? The evidence from Canada. Journal of Health Politics, Policy, and Law. 2010;35(5):705–742. doi: 10.1215/03616878-2010-025. [DOI] [PubMed] [Google Scholar]
- Roberts JM. A Review of the Research to Identify the Most Effective Models of Best Practice in the Management of Children with Autism Spectrum Disorders. Sydney, NSW, Australia: Centre for Developmental Disability Studies; 2003. [Google Scholar]
- Roth L. Autism spectrum disorder. Australian Policy Online. 2013 Available at: http://apo.org.au/research/autism-spectrum-disorder.
- Singh J, Illes J, Lazzeroni L, et al. Trends in US autism research funding. Journal of Autism and Developmental Disorders. 2009;39(5):788–795. doi: 10.1007/s10803-008-0685-0. [DOI] [PubMed] [Google Scholar]
- Stein BD, Sorbero MJ, Goswami U, et al. Impact of a private health insurance mandate on public sector autism service use in Pennsylvania. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(8):771–779. doi: 10.1016/j.jaac.2012.06.006. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata statistical software: release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- Stuart M. Autism insurance reform: a comparison of state initiatives. Indiana Health Law Review. 2012;8(2):498–537. [Google Scholar]
- U.S. Census Bureau. [accessed 20 May 2012];State median income. 2012 Available at: http://www.census.gov/hhes/www/income/data/statemedian/
- United States Department of Labor. Self-insured health benefit plans. 2013 Available at: http://www.dol.gov/ebsa/pdf/ACASelfFundedHealthPlansReport033113.pdf.
- Vismara LA, Rogers SJ. Behavioral treatments in autism spectrum disorder: what do we know? Annual Review of Psychology. 2010;6:447–468. doi: 10.1146/annurev.clinpsy.121208.131151. [DOI] [PubMed] [Google Scholar]
- Wang L, Mandell DS, Lawer L, et al. Healthcare service use and costs for autism spectrum disorder: a comparison between Medicaid and private insurance. Journal of Autism and Developmental Disorders. 2013;43(5):1057–1064. doi: 10.1007/s10803-012-1649-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zane T, Davis C, Rosswurm M. The cost of fad treatments in autism. Journal of Early and Intensive Behavior Intervention. 2008;5(2):44–51. [Google Scholar]
- Zirkel PA. Autism litigation under the IDEA: a new meaning of “disproportionality”? Journal of Special Education Leadership. 2011;24(2):92–103. [Google Scholar]