Abstract
Purpose
To determine the extent to which the 24-2 visual field (VF) misses macular damage confirmed with both 10-2 VF and optical coherence tomography (OCT) tests and to evaluate the patterns of damage missed.
Methods
One hundred forty-one eyes of 141 glaucoma patients or suspects underwent 24-2 VF (mean deviation [MD] better than −6 dB), 10-2 VF, and OCT testing. Retinal nerve fiber layer (RNFL) and retinal ganglion cell plus inner plexiform (RGC+) probability plots were combined with 10-2 VF probability plots. Eyes were classified as “abnormal macula” if abnormal regions on both the 10-2 VF and OCT plots agreed. The number of abnormal eyes missed (i.e., false negatives) was determined for the following 24-2 VF metrics: MD; pattern standard deviation (PSD); glaucoma hemifield test (GHT); cluster criteria (CC); and abnormal points within ± 10°. Eyes that were missed on one or more of the 24-2 metrics were classified by damage type based upon circumpapillary RNFL thickness plots.
Results
Fifty-nine (41.8%) eyes were classified as “abnormal macula,” and comprised the reference standard. Of the 59, 31 (52.5%) were missed by one or more of the 24-2 metrics. The individual 24-2 metrics missed between 7 (CC) and 20 (MD) eyes. The eyes missed had widespread macular damage, as well as both shallow and deep local defects.
Conclusions
Eyes with macular glaucomatous damage may be classified as normal based on the 24-2 VF alone.
Translational Relevance
To detect macular damage with perimetry, the 10-2 VF test (or a modified 24-2 VF test) is essential.
Keywords: glaucoma, perimetry, macula, optical coherence tomography
The macular region (i.e., ±8° from fixation) covers less than 2% of the retinal area, but contains over 30% of the retinal ganglion cells (RGCs).1 Glaucomatous damage to the macula (central ±8°) is relatively common, involves defects that are deep and local as well as those that are shallow and widespread, and can occur early in the disease process.2–11 Because central vision is necessary for tasks such as reading, recognizing faces, and driving,12 early detection of macular damage is vital to clinical practice. The visual field (VF) pattern most widely used to detect glaucomatous damage, the 24-2 test pattern, does not adequately test the macular region, as the 6° grid of the 24-2 pattern has only four points within ± 8°. When these four 24-2 central points are displaced to take into account the anatomical position of the RGCs, they fall outside of the region of the macula most affected by glaucoma.7,8
It is therefore not surprising that the 24-2 VF misses glaucomatous damage of the macula that a test pattern with a 2° grid (i.e., the 10-2 pattern) detects.5–10,13,14 For example, Langerhorst et al.5 found that the 10° (2° grid) VF showed a greater number, and more severe, glaucomatous macular defects than a 30° (6° grid). Similarly, Traynis et al.9 found that 22.7% of the eyes classified as normal on the 24-2 VF were abnormal on the 10-2 (2° grid) VF. Further, in analyzing progression of macular defects, Park et al.13 found that 70.8% of the eyes with progression detected by the 10-2 VF were missed by the 24-2 VF. These studies used various methods of interpreting the 24-2 VF. However, they did not address the ability of the 24-2 to detect macular damage with the typical metrics used by the clinician.
Here we ask: Can the clinician detect eyes with macular damage using the standard metrics of the 24-2 VF, such as mean deviation (MD), pattern standard deviation (PSD), and glaucoma hemifield test (GHT)? In addition, unlike previous work that implicitly assumed the 10-2 VF is the gold standard for defining macular damage, we defined an abnormal macular region based upon both 10-2 VF and optical coherence tomography (OCT) macular RGC and/or RNFL damage.8 In particular, an eye was classified as having macular damage only if the 10-2 VF and OCT RGC and/or probability plots showed abnormalities in the same region of the macula.
Thus, we tested the hypothesis that clinicians using standard 24-2 metrics may miss eyes with confirmed macular damage. In addition, we evaluated the patterns of macular damage that were missed.
Methods
The study was approved by the Columbia University and New York Eye and Ear Infirmary of Mount Sinai Institutional Review Board and adheres to the tenets set forth in the Declaration of Helsinki and the Health Insurance Portability and Accountability Act (HIPAA). Written informed consent was obtained from all subjects.
One hundred forty-one eyes of 141 patients previously studied15 met the following criteria: (1) abnormal or suspicious discs on fundus photography; (2) best-corrected visual acuity of 20/40 or better; (3) MD better than −6.0 dB on the 24-2 VF; (4) open angles on gonioscopy; (5) cataracts no worse than NO02, NC02, C2, and P2 on the Lens Opacities Classification System III (LOCS);16 (6) refractive error within ± 6.0 D; and (7) no other disorders that could affect vision, such as neuro-ophthalmic or retinal disease, or corneal opacity. To help assure other conditions such as macular holes, age-related macular degeneration, dystrophies, and macular edema were not present, all eyes had horizontal and vertical OCT macular lines scans. In addition, all eyes had 6 × 6 mm frequency-domain (fd) OCT cube scans of the macula and disc (3D-OCT2000, Topcon, Inc., Tokyo, Japan) and reliable 24-2 and 10-2 VFs (fixation losses 33% or better, false-positives and false-negatives (FNs) 20% or better) obtained with Humphrey SITA-standard automated perimetry.
Abnormal Macula Eyes
Fifty-nine of these 141 eyes were categorized as “abnormal macula” as part of a previous study.15 These 59 patients (38 females/21 males) were 61.1 ± 11.8 years of age and had a mean refractive error of −1.20 ± 2.58 D (range −6.0 to 2.75). Their 24-2 and 10-2 VFs had a MD of −2.97 ± 1.69 and −3.21 ± 2.24 dB, respectively.
For the macula to be judged abnormal in that study, the probability plots of the 10-2 VF and the OCT macular scan (RGC+ and/or RNFL thickness) had to be abnormal. Further, the regions of abnormality had to show topographical agreement. To make these judgments, three experienced graders viewed RGC+ and RNFL probability plots with 10-2 VF points superimposed.15 These combined probability plots were part of a single-page report.17,18
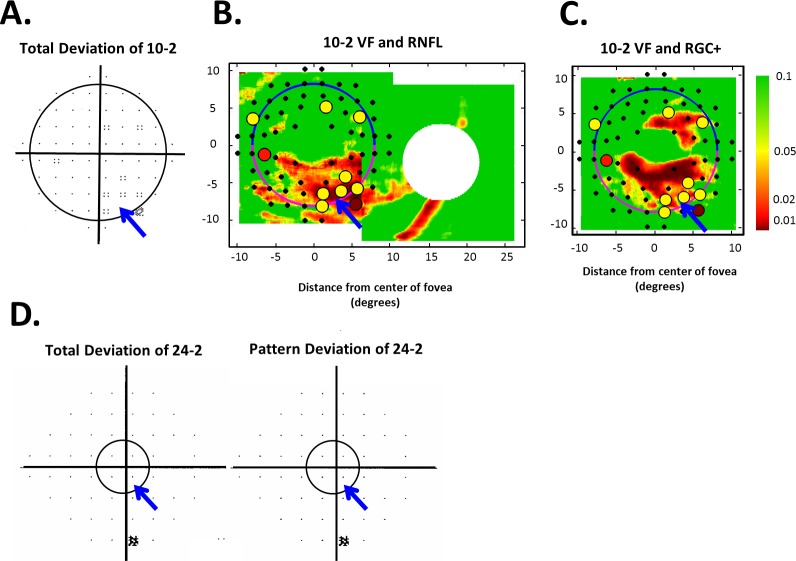
Figures 1B, 1C show these combined plots for one of the abnormal macula eyes. The circles indicate the 10-2 VF points after morphing to take into consideration the location of the RGCs.6 Both sets of data are shown in field view, and the same probability scale is used for the RNFL (panel B) and RGC+ (panel C) thickness (background color) and 10-2 total deviation (TD; circles) values. In Figure 1 (blue arrows), there is topographical agreement between the abnormal 10-2 VF (A) locations and the abnormal RNFL (B) and RGC+ (C) regions. Thus, this eye was classified as “abnormal macula.”
Figure 1.
(A) The 10-2 VF TD plot. (B, C) The 10-2 TD (color circles and black points) combined with macular RNFL (B) and RGC+ (C) probability plots (background) are shown in field view with the macular region encircled. The scale to the right refers to the TD, RFNL, and RGC+ probabilities. (D) The 24-2 TD and PD plots with the macular region encircled (±8°).
Based upon these plots, three experienced graders classified each eye as “macular normal,” “abnormal macula,” or “mismatch” (i.e., the 10-2 VF and OCT probability plots did not agree) in the previous study.15 Only the 59 eyes classified as abnormal macula were analyzed in the current study.
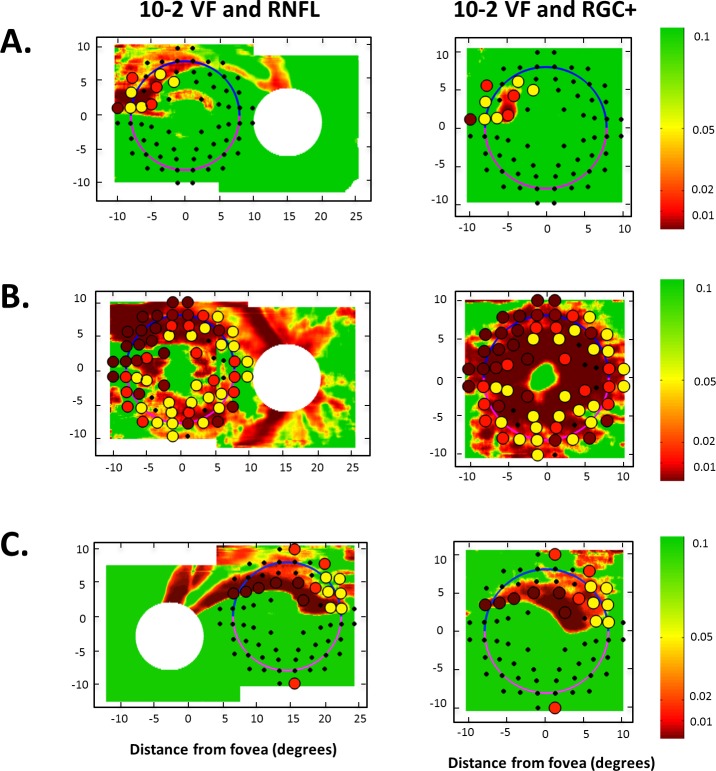
Because the criteria used for abnormal 10-2 VF, and agreement between 10-2 VF and OCT probability plots, were subjective in our earlier study, we performed a post hoc analysis of the 59 eyes. For 56 of the 59 eyes, the 10-2 VF had five or more contiguous points at a probability of 5% or less. For the other three, the points followed an arcuate pattern, but were not strictly contiguous. Concerning the agreement between the regions of abnormality seen on 10-2 and OCT probability plots, 58 of the 59 eyes had four or more 10-2 VF points within the abnormal region of one or both of the OCT probability plots. In the case of the 59th eye, the defects fell close but did not overlap, undoubtedly due to intersubject variability in RGC displacement. This analysis supports the assertion in the earlier study that we can be “reasonably confident” that these eyes had macular damage. While Figures 1 and 2A show examples with relatively subtle damage, most of the eyes had more obvious damage in one or both of the hemispheres. Figures 2B, 2C illustrate the more typical findings.
Figure 2.
(A, B, C) The 10-2 VF TD combined with the macular and disc RNFL thickness probability plots (left panels) and the macular RGC+ thickness probability plot (right panels), from three examples of abnormal macula eyes.2 The scale to the right refers to the TD, RFNL, and RGC+ probabilities.
24-2 Metrics
For each of 59 abnormal macula eyes, the following metrics were used to define the 24-2 as abnormal: MD: P ≤ 5%; PSD: P ≤ 5%; GHT: outside normal limits (ONLs); cluster criteria (CC): three neighboring points at 5%, 5%, and 1% or 5%, 2%, and 2% probability or worse within a hemifield on TD or pattern deviation (PD) plots, with only one point allowed on the edge of the 24-2; macular points (MPs) within ± 10°: one point at 1% or two at 2% within a hemifield on TD or PD.
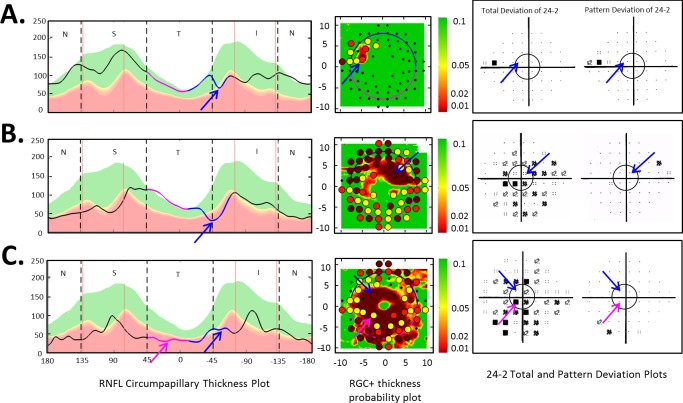
For each of the FNs, circumpapillary retinal nerve fiber layer (cpRNFL) thickness plots (left column in Fig. 3) were used to categorize the pattern of macular damage. The cpRNFL thickness plot (left panel) is oriented such that the temporal quadrant of the disc is centered (NSTIN orientation), with the pink line representing the thickness of nerve fibers traveling from the superior macula and the blue line representing the thickness of nerve fibers traveling from the inferior macula.17 Local damage was defined as a defect that spanned less than half of the macular region, whereas widespread was defined as a defect or series of defects collectively spanning 50% or more of the macular region. The three categories of macular damage were: shallow local damage (an RNFL defect within the 5% confidence interval [CI]), deep local damage (an RNFL defect within the 1% CI), and widespread damage (an RNFL defect throughout the macular region).
Figure 3.
Examples of patterns of macular damage: shallow local damage (A), deep local damage (B), and widespread damage (C) of the macula. In each row, the left panel is the cpRNFL thickness plot (in NSTIN view), the central panel is the combined 10-2 TD (colored circles) and macular RGC+ (background color) probability plots (in field view), and the right panel is the total and PD probability plots of the 24-2 VF. On the cpRNFL plot, the pink line represents the RNFL thickness associated with the superior macula, and the blue line represents the RNFL thickness associated with the inferior macula. The arrows indicate corresponding locations.
Results
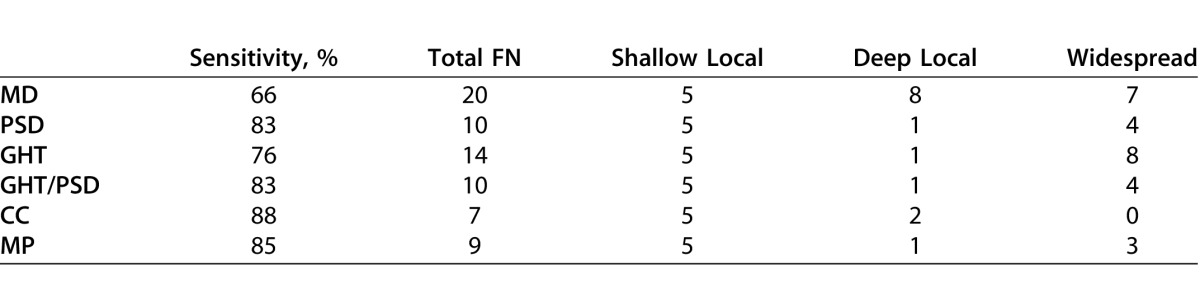
Of the 59 abnormal macula eyes, based upon 10-2 VF and OCT macular scans, 31 (52.5%) were missed (FNs) by one or more 24-2 VF metrics. The individual 24-2 VF metrics missed (FN) between 7 (CC) and 20 (MD) eyes and sensitivity varied from 66% (MD) to 88% (CC; see Table 1, columns 2 and 3).
Table 1.
Metric Sensitivity, Total Number of FNs, and Number of FNs Categorized by Pattern of Macular Damage
Three eyes were missed (FNs) on all 24-2 VF metrics. Figure 1D shows the 24-2 VFs for one of these eyes. Although this VF was normal on all the 24-2 VF metrics, there was clearly macular damage in this eye as indicated by the agreement between the abnormal regions seen on the 10-2 (circles) and OCT (background color) probability plots in Figures 1B, 1C. Note that the circles in all figures have a radius of 8° and encompass the macular region.
Of the 31 eyes that were missed by one or more metrics, 7 (22.5%) were classified as having shallow local damage, 10 (32.3%) as having deep local damage, and 14 (45.2%) as having widespread damage. Figure 3 illustrates examples of each. Figure 3A (same eye as Fig. 2A) is an example of shallow local damage missed on 7 of 31 FNs. Notice that the macular defects are apparent on the cpRNFL thickness plot (left panel) and the combined 10-2 TD and OCT probability plots (middle panel) and in Figure 2A, but not on the 24-2 TD or PD (right panel). (The arrows indicate corresponding locations.) In Figure 3C, the cpRNFL plot and the combined probability plots show deep local damage missed on 10 of 32 FNs. The pattern of deep local damage is not seen on the 24-2 TD or PD plots. In Figure 3C, widespread glaucomatous damage confirmed with OCT and 10-2 VFs does not appear on the PD plot and is missed by 14 of 31 FNs.
Discussion
The purpose of this study was to determine the extent to which 24-2 metrics, commonly used in clinical practice, miss macular damage and, to evaluate the patterns of damage most frequently missed by these metrics. The most sensitive 24-2 VF metric, CC, missed 7 (12%) of the eyes with confirmed macular damage, and the least sensitive 24-2 VF metric, MD, missed 20 (34%). Thus, these common metrics miss macular damage documented on both OCT macular scans and 10-2 VFs. The patterns of damage missed included shallow and deep local damage, as well as widespread damage. Interestingly, the CC metric, designed to detect local damage, was the most sensitive for detecting widespread macular damage.
To compensate for the inability of the MD, PSD, GHT, and CC 24-2 metrics to detect macular damage, some clinicians examine the TD values of a few central points. We attempted to mimic this strategy with our MPs metric. However, this metric still missed 9 (15%) of the 59 abnormal macula eyes.
Additionally, many clinicians judge glaucomatous damage based upon the PD plot rather than the TD plot. In particular, when the 24-2 TD plot shows generalized depressed sensitivity and the PD plot is normal, they conclude that there is no significant damage to the macula and surrounding area. However, these eyes can sometimes have widespread macular damage.10 This is evident in Figures 3B and 3C, where the cpRNFL thickness plot and combined 10-2 and OCT macular probability plots show macular damage that is not evident on the 24-2 PD plots.
While previous work argued that tests with a 6° grid missed damage detected by the 10-2 grid,5,9 it was not possible to get accurate measures of sensitivity as there was no “gold standard” for macular damage. To minimize this problem, we created a reference standard based upon both 10-2 VF and OCT tests. In particular, the macular was considered abnormal only if the 10-2 TD and the RGC+ and/or RNFL probability plot showed abnormal regions that topographically agreed. While theoretically our approach can result in an eye falsely classified as abnormal, false-positives should be rare given that the VF and OCT results should have largely independent sources of error and our criteria of an abnormal 10-2 were relatively conservative (see Methods).
Even with this relatively strict definition of an abnormal macula, the individual 24-2 metrics missed 12% or more of these eyes. In order to improve the sensitivity of the 24-2, it is possible to combine the information provided by the various metrics as clinicians frequently do in practice, but this will only increase the number of eyes falsely identified as having macular damage. In any case, combining the most common metrics (GHT and PSD) did not improve sensitivity compared to PSD alone. To put this in perspective, this common set of criteria missed 10 (17%) of the eyes classified as abnormal macula.
Given the prevalence of early macular damage, patients should not be screened with only the 24-2 VF. Although our 141 patients were a mix of suspects and patients with mild glaucoma (i.e., MD better than −6.0 dB), over 40% of them had macular damage as defined by our 10-2 and OCT analysis. This estimate is conservative as it does not include the eyes with macular damage that were classified as abnormal on only the 10-2 VF or the OCT macular scans.
What are the alternatives? We are not suggesting replacing the 24-2 VF with a 10-2 VF. In a population of patients similar to ours, Traynis et al.9 found that the percentage of eyes classified as normal on the 10-2 VF, but abnormal on the 24-2 VF, was approximately the same as the percentage normal on the 24-2 VF, but abnormal on the 10-2 VF. We believe the preferred solution is to use a modified 24-2 pattern.19,20 For example, adding 16 of the points from the 10-2 pattern to the 24-2 pattern will identify most of the eyes with macular damage with the same number of test points in the 10-2 pattern.20 However, we realize this will not be feasible until manufacturers make it easy to compare the results of this modified 24-2 to previous 24-2 tests, as well as to normative values. Until an improved 24-2 VF is available commercially, we favor the current practice followed by some clinicians of alternating 24-2 and 10-2 VFs on successive visits, although this does have the disadvantage of decreasing the number of tests available for progression analysis. In any case, 10-2 VF results should be combined with OCT macular RGC+ probability plots.15
Limitations and Caveats
To be clear, we asked whether eyes with macular damage might be misclassified as normal if only a 24-2 VF was available. It is important to note that some of the eyes with macular damage were correctly classified as abnormal by a 24-2 metric because they had damage outside the macula, as well as inside. That is, it was the damage outside the macula that was correctly detected. Had we asked whether the clinician could determine if macular damage were present based upon the 24-2 VF, then only the central four points of the 24-2 VF points (i.e., those within the macula) would have been relevant and many more eyes would have been missed.
It is also important to note that these eyes had relatively mild glaucoma, at least as assessed by the 24-2 VF. If we had included eyes with 24-2 VF MD worse than −6 dB, the percentage of misses would have been lower.
Conclusions and Clinical Implications
Individually, the 24-2 VF metrics missed between 12% and 34% of the 59 eyes with confirmed macular damage. Eyes with macular glaucomatous damage may be classified as normal based on the 24-2 VF alone. To detect macular damage reliably with perimetry, either the 10-2 VF test or a modified 24-2 VF test19,20 is essential.
Acknowledgments
The authors thank Daiyan Xin, who was involved in the recruiting and testing of the patients in this study.
Supported by the National Institutes of Health Grant R01-EY-02115 (DCH).
Disclosure: L.M. Grillo, None; D.L. Wang, None; R. Ramachandran, None; A.C. Ehrlich, None; C.G. de Moraes, None; R. Ritch, None; D.C. Hood, Topcon Medical Systems, Inc. (F, C)
References
- 1. Curcio CA,, Allen KA. Topography of ganglion cells in human retina. J Comp Neurol. 1990. ;300:5 – 25. [DOI] [PubMed]
- 2. Anctil JL,, Anderson DR. Early foveal involvement and generalized depression of the visual field in glaucoma. Arch Ophthalmol. 1984; 102: 363–370. [DOI] [PubMed] [Google Scholar]
- 3. Stamper RL. The effect of glaucoma on central visual function. Trans Am Ophthalmol Soc. 1984; 82: 792–826. [PMC free article] [PubMed] [Google Scholar]
- 4. Pickett JE,, Terry SA,, O'Connor PS,, O'Hara M. Early loss of central visual acuity in glaucoma. Ophthalmology. 1985; 92: 891–896. [DOI] [PubMed] [Google Scholar]
- 5. Langerhorst CT,, Carenini LL,, Bakker D,, De Bie-Raakman MAC. Measurements for description of very early glaucomatous field defects. In: Wall M,, Heiji A, eds Perimetry Update 1996/1997. New York, NY: Kugler Publications; 1997: 67–73.
- 6. Schiefer U,, Papageorgiou E,, Sample PA,, et al. Spatial pattern of glaucomatous visual field loss obtained with regionally condensed stimulus arrangements. Invest Ophthalmol Vis Sci. 2010; 51: 5685 –568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hood DC,, Raza AS,, de Moraes CG,, et al. Initial arcuate defects within the central 10 degrees in glaucoma. Invest Ophthalmol Vis Sci. 2011; 52: 940–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hood DC,, Raza AS,, deMoraes CG,, Liebmann JM,, Ritch R. Glaucomatous damage of the macula. Prog Retin Eye Res. 2013; 32: 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Traynis I,, De Moraes CG,, Raza AS,, Liebmann JM,, Ritch R,, Hood DC. Prevalence and nature of early glaucomatous defects in the central 10 degrees of the visual field. JAMA Ophthalmology. 2014; 132: 291–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hood DC,, Slobodnick A,, Raza AS,, de Moraes CG,, Teng CC,, Ritch R. Early glaucoma involves both deep local, and shallow widespread, retinal nerve fiber damage of the macular region. Invest Ophthalmol Vis Sci. 2014; 55: 632–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Araie M. Pattern of visual field defects in normal-tension and high-tension glaucoma. Curr Opin Ophthalmol. 1995; 6: 36–45. [DOI] [PubMed] [Google Scholar]
- 12. Nelson P,, Aspinall P,, Papasouliotis O,, et al. Quality of life in glaucoma and its relationship with visual function. J Glaucoma. 2003; 12: 139–150. [DOI] [PubMed] [Google Scholar]
- 13. Park SC,, Kung Y,, Su D,, et al. Parafoveal scotoma progression in glaucoma: humphrey 10-2 versus 24-2 visual field analysis. Ophthalmology. 2013; 120: 1546–1550. [DOI] [PubMed] [Google Scholar]
- 14. Hangai M,, Ikeda HO,, Akagi T,, Yoshimura N. Paracentral scotoma in glaucoma detected by 10-2 but not by 24-2 perimetry. Jpn J Ophthalmol. 2014; 58: 188–196. [DOI] [PubMed] [Google Scholar]
- 15. Wang D,, Raza A,, de Moraes CG,, et al. Central glaucomatous damage of the macula can be overlooked by conventional OCT retinal nerve fiber layer thickness analyses. Trans Vis Sci Technol. 2015; 4: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chylack LT,, Jr,, Wolfe JK,, Singer DM,, et al. The Lens Opacities Classification System III. The longitudinal study of cataract study group. Arch Ophthalmol. 1993; 111: 831 –836. [DOI] [PubMed] [Google Scholar]
- 17. Hood DC,, Raza AS. On improving the use of OCT imaging for detecting glaucomatous damage. Br J Ophthalmol. 2014; 98 (suppl 2): ii1–ii9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hood DC,, Raza AS,, De Moraes CG,, et al. Evaluation of a one-page report to aid in detecting glaucomatous damage. Trans Vis Sci Technol. 2014; 3: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ehrlich AC,, Raza AS,, Ritch R,, Hood DC. Modifying the conventional visual field test pattern to improve the detection of early glaucomatous defects in the central 10°. Transl Vis Sci Technol. 2014; 3: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hood DC,, Nguyen M,, Ehrlich AC,, et al. A test of a model of glaucomatous damage of the macula with high-density perimetry: implications for the locations of visual field test points. Transl Vis Sci Technol. 2014; 3: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]