Abstract
In this article, we review the current evidence for the cellular and molecular mechanisms of AKI, focusing on epithelial cell pathobiology and related cell-cell interactions, using ischemic AKI as a model. Highlighted are the clinical relevance of cellular and molecular targets that have been investigated in experimental models of ischemic AKI and how such models might be improved to optimize translation into successful clinical trials. In particular, development of more context-specific animal models with greater relevance to human AKI is urgently needed. Comorbidities that could alter patient susceptibility to AKI, such as underlying diabetes, aging, obesity, cancer, and CKD, should also be considered in developing these models. Finally, harmonization between academia and industry for more clinically relevant preclinical testing of potential therapeutic targets and better translational clinical trial design is also needed to achieve the goal of developing effective interventions for AKI.
Keywords: acute renal failure, kidney, pathophysiology of renal disease and progression
Cellular and molecular mechanisms of AKI have been extensively investigated in a variety of experimental models, through which a number of candidate therapies for AKI have been identified. This article reviews the current evidence by dissecting the cellular and molecular mechanisms of AKI, focusing on epithelial cell pathobiology and related cell-cell interactions, and using the example of ischemic AKI to describe our approach. Specifically, we reviewed the cellular and molecular epithelial cell targets that have been investigated in experimental models of ischemic AKI, and considered the clinical relevance of these models in human AKI and how such models might be improved to optimize translation into successful clinical trials. We have structured our review to answer two key questions:
(A) What are the cellular and molecular targets that are important in the pathogenesis of AKI? (B) What are the animal models in which these targets have been tested?
(A) What are the clinical correlates of these animal models in human AKI? (B) How can we improve the translation of these models to achieve effective diagnosis and therapy of AKI?
What Are the Cellular and Molecular Targets that Are Important in the Pathogenesis of AKI?
Cell Membrane
The plasma membrane is a primary site of damage in AKI. With necrotic cell injury, compromise of cell membrane integrity results in extrusion of intracellular contents, and with apoptosis there is translocation of phospholipids from the inner to the outer membrane leaflet, followed by membrane blebbing. In addition, there are four potential mechanisms by which the plasma membrane can play an important role in AKI that could be fruitful subjects for further research: by alterations in (1) membrane composition, (2) membrane-associated proteins, and (3) membrane-associated enzymatic activity, and by (4) signaling by membrane-associated components. Examples for each of these potential roles for the plasma membrane in AKI include the following: (1) the composition of cholesterol-rich microdomains is altered after AKI, and lipid microdomains are important both for preventing cell injury and developing subsequent cytoresistance to further insult1,2; (2) there is increased expression of FAS ligand,3 altered caveolin-1 expression,4,5 and decreased Na transporters after AKI6; (3) decreased membrane-associated alkaline phosphatase7 and altered expression of the zinc-dependent metalloproteinase meprin A are associated with AKI8; and (4) a potential role has been suggested for microvesicles/exosomes in protection and recovery from AKI.9,10
Recent studies have highlighted the importance of regulated necrosis or necroptosis, a receptor-interacting protein kinase-dependent necrotic cell death in AKI. Key proteins involved in the signaling pathway of necroptosis—such as necrostatin-1, receptor-interacting protein kinase 3, and mixed lineage kinase domain-like protein, that regulate a molecular switch to induce plasma membrane rupture—could be potential targets in AKI (reviewed in11). Pyroptosis, another form of programmed cell death, was thought to occur predominantly in macrophages, but features of pyroptosis have also been described in other cell types including tubular epithelial cells. Pyroptosis differs from apoptosis. (1) Caspase-1 and -11 are associated with pyroptosis, and (2) during pyroptosis, damage-associated molecular pattern molecules and proinflammatory cytokines are released that mediate cell damage. An iron-dependent form of nonapoptotic cell death, ferroptosis, has been recently described (reviewed in11). Small molecules that block ferroptosis demonstrate significant cytoprotection both in vitro and in vivo in animal models12 and may be targets for therapeutic intervention in AKI.
Nucleus
Major components of the nucleus including DNA and chromatin, transcription factors, and epigenetic regulators of gene expression are among the key targets in AKI. Cell cycle regulatory proteins are also important in the pathogenesis of AKI and are discussed below (see Cell Cycle). Among transcription factors, Nrf2, the AP-1 family, NF-κB, hypoxia-inducible factors, Sp1, and several others have been implicated in the pathogenesis of AKI via regulation of numerous genes. Many of these have also been potential therapeutic targets for AKI. However, given the mostly ubiquitous tissue distribution of transcription factors, specific targeting to particular cell types in the kidney—although feasible in animal models—will be a challenge to translate to human studies. Recent studies have highlighted the importance of epigenetic modifications, including microRNAs,13,14 as determinants for the outcome of AKI and the AKI-to-CKD transition. Oxidants and endonucleases such as deoxyribonuclease I and endonuclease G (both highly expressed in the kidney) can have effects on nuclear constituents causing DNA damage15 and are also potential targets in acute tubular injury.
Cytoskeleton
Alterations in the cytoskeleton, particularly for actin, have been described in the pathogenesis of AKI.16 These changes occur very rapidly, correlate with the severity and duration of experimental AKI, and are important for the structural and functional integrity of renal proximal tubule cells, endothelial cells, and vascular smooth muscle cells during AKI. Alterations in the actin cytoskeleton regulate changes in cell polarity, cell-cell interactions, and cell-matrix interactions, and, as a result, influence the GFR and tubular function. The role of growth factors, mesenchymal stem cells, and other key mediators of tissue regeneration in the context of AKI is reviewed by Humphreys et al. in a related Journal of the American Society of Nephrology article.17
Endoplasmic Reticulum
The endoplasmic reticulum (ER) is an interconnected network of membrane-enclosed tubes within the cytoplasm and is continuous with the outer membrane of the nucleus. ER stress due to accumulation of unfolded proteins has been shown to occur in both animal models and human AKI. Recent studies have highlighted the importance of sex differences in susceptibility to ER stress,18 wherein male mice are more susceptible to ER stress–induced AKI compared with female mice, a finding that could be relevant in the development of therapeutic interventions to mitigate ER stress. Identification of the molecular mechanisms involved in ER stress, such as the PERK-ATF4-CHOP pathway (PERK, protein kinase RNA-like ER kinase; ATF4, activating transcription factor 4; CHOP, CCAAT/enhancer-binding protein homologous protein; reviewed in19), also represent potentially new therapeutic targets in AKI.
Mitochondria
The chemical work of reclaiming >100 l/d from the glomerular filtrate is performed by the tubular epithelium of the healthy kidney. In order to move sodium and other solutes against strong electrochemical gradients, epithelial cells of the nephron—in particular, proximal tubular cells—are rich in mitochondria. Per milligram of tissue, only the heart exceeds the kidney in mitochondrial content.20 Not unexpectedly, mitochondrial pathology is a shared feature across diverse forms of human AKI, ranging from renal ischemia to sepsis and nephrotoxic injury.21–24 Ultrastructural features of mitochondrial injury include swelling with rarefaction of the cristae and mitochondrial fragmentation. With few exceptions, the spectrum of experimental rodent models of AKI demonstrates widespread mitochondrial injury,25–27 and the onset of mitochondrial pathology typically precedes detectable loss of renal function.
In response to hypoxia, increases in cytosolic calcium concentration, changes in NAD/NADH ratios, reduced mitochondrial membrane voltage, oxidative stress, and other noxious stimuli, mitochondria serve as a critical mediator of cell death not only by reducing ATP generation, but also by at least two distinct mechanisms28—involving reactive oxygen species (ROS) and mitochondrial permeability transition (MPT). First, injured mitochondria become a robust source of excess ROS. Whereas efforts to target ROS in post-ischemic AKI with generic antioxidants have been unsuccessful, promising preclinical results have been attained with mitochondrially targeted antioxidants—compounds that achieve mitochondrial accumulation of antioxidant activity either by a chemical modification (e.g., MitoQ) or by tethering to a targeting peptide (e.g., SS-31).29,30
Opening of the MPT pore is a key event. The MPT is composed of several proteins and its opening permits the passage of small molecules and water between the mitochondrial matrix and the cytoplasm. MPT pore opening releases mitochondrial calcium, which in turn can activate MPT in neighboring organelles, and proapoptotic mediators including cytochrome c. MPT pore opening also results in osmotic swelling of the mitochondrial matrix that can swell and even rupture mitochondria. Cyclosporin is commonly applied to inhibit the MPT in cellular and animal models, and is even being tested for the attenuation of the cardiac ischemia-reperfusion injury.31 Application in post-ischemic renal injury may require the development of MPT inhibitors with less renal vasoconstriction.
Within a given cell, the abundance of mitochondria is maintained by a balance between generative (biogenesis) and destructive/recycling (mitophagy) processes. Moreover, the population of extant mitochondria can undergo fusion and fission, dynamic processes whose net balance influences the efficiency of ATP generation and the vulnerability to apoptotic stimuli. Mitochondrial biogenesis is orchestrated by a family of transcriptional coactivators whose canonical member is PGC1α (peroxisome proliferator activated receptor gamma coactivator 1 alpha). PGC1α is expressed in the most metabolically active organs; within the kidney, the pattern of PGC1α expression superimposes the pattern of mitochondrial abundance, with cortical epithelial cells exhibiting the highest expression. During experimental sepsis, the expression of PGC1α falls proportionally to the degree of functional impairment, and recovery is associated with restored PGC1α expression. Importantly, mice with global or proximal tubule–specific PGC1α deletion display no basal renal phenotype, but develop more sustained renal injury after endotoxemia compared with littermate controls.26 The pattern of reduced renal PGC1α expression during injury followed by a rebound to normal has also been reported in ischemia-reperfusion injury.33 Collectively, these results suggest that mitochondrial biogenesis may be an important step in recovery from AKI.
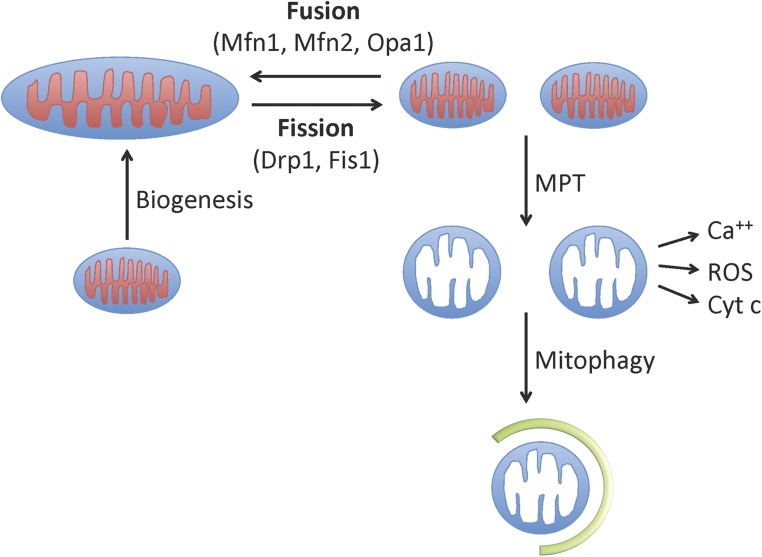
Mitochondrial dynamics are profoundly altered in ischemic and nephrotoxic injury (Figure 1). In either situation, Brooks et al. showed that mitochondrial fragmentation arose before overt renal tubular injury or cell death.25 They demonstrated that AKI is associated with an excess of mitochondrial fission compared with fusion. Dynamin-related protein 1 (DRP1) initiates the process of mitochondrial cleavage. Pharmacologic inhibition of DRP1 ameliorated experimental AKI and improved mitochondrial morphology. The damage wrought by mitochondrial fragmentation may relate to excess production of ROS, increased susceptibility to stimuli that initiate the insertion of the proapoptotic protein Bax, or other processes.34,35 Finally, mitophagy enables the clearance of damaged mitochondria and is intimately linked to the dynamics of fission and fusion. During fission, if a daughter mitochondrion loses membrane potential, it may not fuse and may instead undergo clearance via mitophagy.36 Dynamics therefore couples with mitophagy to maintain the quality of mitochondria in the healthy cell. Because AKI appears to be a state of excess fission, a greater burden is placed on mitophagy to clear fragmented mitochondria. Consistent with this concept, Ishihara et al. have reported the involvement of autophagy molecules sestrin-2 and BNIP-3 in the acutely injured kidney.37
Figure 1.
Involvement of mitochondria in ischemic AKI: Healthy mitochondria generate the ATP necessary for cellular health and, in the renal tubule, the energy needed for the movement of solute and water against gradients. Ischemia-reperfusion injury leads to rapid fragmentation of mitochondrial networks through a dynamic process termed fission regulated by proteins such as dynamin-related protein 1 (Drp1) and mitochondrial fission 1 protein (Fis1). The mitochondrial fusion machinery includes mitofusin 1 (Mfn1), Mfn2 and optic atrophy 1. Fragmented mitochondria appear to be a less efficient source of ATP and can undergo the MPT. MPT results in mitochondrial swelling from the influx of water, and it promotes cell death through the release of calcium (Ca++), cytochrome c (Cyt c), and other proapoptotic proteins. Damaged mitochondria can be cleared and recycled through mitophagy, the first step of which is envelopment of the injured mitochondrion by a double-membrane structure termed the autophagosome (shown in green). Finally, in surviving cells, mitochondrial biogenesis results in an expansion of mitochondrial mass through regulated gene expression of structural and enzymatic components of mitochondria. Reprinted from www.adqi.net, with permission.
Mitochondrial fusion is mediated by proteins including mitofusin 1, mitofusin 2 (Mfn2), and optic atrophy 1. Recent studies have demonstrated that deletion of Mfn2 selectively in renal epithelial cells leads to mitochondrial fragmentation and apoptosis after ATP depletion in vitro.38 However, in contrast to these effects observed in vitro, selective deletion of Mfn2 from renal proximal tubules increased survival and improved renal function after ischemia-induced AKI in vivo.39 Although further studies are needed, therapies that inhibit fission, favor fusion, or enhance mitophagy may be beneficial in one or more phases of AKI.
Receptors
Studies in experimental animal models have implicated cell-surface receptors in both initiation and/or propagation of epithelial injury in response to AKI and as important mediators of subsequent epithelial repair. Examples of receptors involved in AKI-mediated injury include the FAS receptor and TGFβ receptor.40,41 Examples of receptors involved in epithelial cytoprotection and repair include the EGF receptor,42 HGF receptor (c-Met),43 sphingosine-1-phosphate receptor,44 and netrin-1 receptor.45 Many questions relating to the role of receptors in AKI remain unanswered, including the sources of the putative ligands, mechanisms of receptor activation, and signaling pathways involved in protection from injury or involved with epithelial repair. The important role of receptors involved in innate immunity (like TLRs) is discussed in a related Journal of the American Society of Nephrology review by Rabb et al.46
Cell Cycle
Under normal physiologic conditions, cell proliferation in kidneys is limited to a small percentage of cells, indicating that most cells are quiescent at the G0 phase of the cell cycle at any given point in time. In AKI, there is notable cell proliferation, especially in the damaged renal tubules.47 The mechanism of cell cycle reactivation is currently unclear, but it may involve the release of contact inhibition. When an injured renal tubular cell is dying or is sloughed into the tubular lumen, neighboring cells may stretch to cover the denuded area, become de-differentiated, and activate the cell cycle. This process appears to be driven by various cyclins and cyclin-dependent kinases (CDKs).48 After proliferation or cell division, the newly generated cells can redifferentiate into polarized, functional tubular cells for kidney repair.48
Interestingly, inhibitory cell cycle regulators are also induced during AKI. For example, p21 is induced in ischemic and cisplatin-induced AKI.49,50 Also referred to as CDK-interacting protein 1 (CIP1), p21 binds to and antagonizes cyclin-CDK complexes, resulting in G1 phase cell cycle arrest. Depending on the conditions, p21 is induced in AKI by both p53-dependent and p53-independent mechanisms.50,51 It is noteworthy that, in addition to cell cycle inhibition, p21 may also be an important cytoprotective factor in AKI.52 Another major cell cycle inhibitor that is rapidly induced in AKI is p53.53,54 In cisplatin AKI, p53 is induced via the DNA damage response mediated by ATR/Chk2.55,56 However, in ischemic AKI, the ATM-mediated DNA damage response may be responsible.47 p53 may activate the transcription and expression of p21 to arrest the cell cycle. There may be a threshold effect of cell cycle inhibition, because other studies have shown that p53 can trigger tubular cell death in AKI.57,58
Although the kidneys are known to have a remarkable reparative capacity, when injury is extensive or prolonged the repair in AKI may not be complete, leading to a maladaptive response that contributes to the late development of fibrosis and decline of renal function.59,60 The cellular and molecular basis of this maladaptive response remains elusive, but it may involve transient cell cycle activation followed by cell cycle arrest. As a result, a small population of tubular cells may become arrested at the G2/M phase and acquire a senescence-like phenotype. Notably, these cells appear to be highly secretory and produce cytokines that promote fibrosis.48 Recent studies have validated the use of urinary levels of insulin like growth factor binding protein-7 and tissue inhibitor of metalloproteinase-2, both inducers of G1 cell cycle arrest, as important biomarkers in human AKI.61
Lysosomes
Lysosomal disruption results in the release of various degradative enzymes including cathepsins, which may lead to a specific form of cell death called lysosomal cell death. It is unclear if lysosomal cell death plays a critical role in AKI. However, lysosomes are important for the completion of autophagy, a cellular process recently implicated in AKI.62 Autophagy is an intracellular process that delivers cytoplasmic constituents to the lysosome for degradation and recycling. In ischemic, nephrotoxic, and septic AKI models, autophagy is rapidly induced in proximal tubular cells.62 Tubular autophagy is also detected in transplanted human kidneys.63 Although autophagy-mediated tubular injury in AKI eluded earlier studies,63,64 recent studies have demonstrated compelling evidence for a renoprotective role of autophagy, and timing of autophagy may be important in determining its beneficial or deleterious effect. Pharmacologic inhibitors of autophagy, such as chloroquine, sensitize animals to AKI.65 Moreover, deletion of autophagy genes, including Atg5 and Atg7, blocks autophagy induction in AKI and enhances kidney injury.66–68
It remains unclear as to how autophagy is activated in AKI. p53 inhibitors can partially suppress cisplatin-induced autophagy in renal tubular cells,67 suggesting a role of p53 in triggering autophagy. In ischemic AKI, oxidative stress has been implicated in autophagy induction. Apparently, the signaling pathways leading to autophagy activation may differ in different AKI models. In addition, autophagy has been implicated in tubular atrophy,69,70 a pathologic phenotype in post-AKI tubules that may contribute critically to renal fibrosis.71 It is also important to elucidate whether and how autophagy contributes to kidney repair after AKI, including fibrosis.
Peroxisomes
Peroxisomes are small single-membrane organelles that are rich in enzymes such as catalase. They are highly dynamic and metabolically active and are required for regenerating tubular epithelial cells. Peroxisomes decrease in animal models of AKI and peroxisome proliferator-activated receptor-alpha ligands are able to increase labeling of peroxisomes in AKI. The role of peroxisomes in AKI is further substantiated by findings that overexpression of Sirt1, an NAD-dependent protein deacetylase that regulates intracellular metabolism and attenuates ROS-induced cell death, mediates these protective effects through maintaining peroxisomal number and function.72
What Are the Animal Models in which these Targets Have Been Tested?
Animal models of AKI serve at least three scientific purposes: (1) to gain insight into pathogenic mechanisms of the human correlate; (2) to identify and test new markers and treatments; and (3) to understand fundamental aspects of the connections among cellular, tissue, and organ-level injury. The first two cases compel investigators to seek animal models that optimally mimic the human disease situation. Although numerous reasons have been proposed for failure to translate promising preclinical results into effective AKI therapies, more rigorous development of next-generation context-specific AKI models may help mitigate at least one commonly cited factor. We focus here on mouse models because these are the most commonly studied animals. However, with the growing adoption of genome-editing technologies to study genotype-phenotype relations in previously inaccessible model organisms,73 it is anticipated that mechanistic studies of AKI will be more feasible in higher-order species.
Human AKI is widely recognized to be multifactorial. The most common risk factors include advanced age, CKD, diabetes, volume depletion, and exposure to potentially nephrotoxic drugs. Too few attempts have been made to model these risk factors in mice, but the results are noteworthy. In 1988, Heyman et al. reported the induction of contrast nephropathy in rats—notoriously difficult to achieve in rodents—by employing a combinatorial approach.74 Heyman’s group subjected adult Wistar-derived rats to uninephrectomy to reduce renal mass, then a low-sodium diet for 7 days and exposure to the cyclo-oxygenase inhibitor indomethacin 1 hour before sodium iothalamate injection. The rats suffered a rapid doubling of serum creatinine and exhibited histologic features consistent with human contrast nephropathy. More recently, Star’s group has studied septic AKI in mice by introducing several different factors: advanced age, pre-existing chronic renal impairment, administration of fluids and antibiotics, and even multiple starting times for candidate therapies relative to induction of sepsis.75,76 In one recent study, Leelahavanichkul et al. found that neutralization of vascular endothelial growth factor effectively treated sepsis, but was ineffective in the setting of sepsis with 5/6 nephrectomy.77 More recent work has demonstrated the hypersensitivity of diabetic models to ischemic AKI that involves hyperglycemia, p53, and mitochondrial damage.78
With promising initial results, we propose a more systematic effort to develop and characterize “multihit” models of renal injury. For example, studying the features of renal ischemia-reperfusion injury in an obese/diabetic model (e.g., ob/ob mice) may lead to a deeper understanding of the pathogenesis of AKI among patients with type 2 diabetes who sustain shock. More broadly, mechanistic AKI research should leverage the increasing precision of genetic engineering to study how the kidney responds to combinations of stimuli that vary both in time and intensity.
We have identified a number of cellular and molecular targets in epithelial cells that are relevant to the pathogenesis of AKI. Any target that is identified needs to be validated in more than one animal model. These would include models not only of ischemia-reperfusion injury, but also of sepsis, nephrotoxin exposure, and others. Development of more context-specific models with greater relevance to human AKI is urgently needed (Figure 2, Table 1). These should tend to replicate the initial insults in clinical settings, but also consider comorbidities that would alter patient susceptibility, such as underlying diabetes, aging, obesity, cancer, and CKD. For example, renoprotective agents for cisplatin-induced AKI are best tested in tumor-bearing animal models.79 After target validation in context-specific animal models, early-phase clinical trials should seek to identify appropriate predictive biomarkers to guide selection, timing, and monitoring of therapy in human clinical trials. Some of the specific targets in preclinical studies along with the timing for the intervention are shown in Table 2. Development of an AKI animal models consortium for evaluating and testing of better context-specific models would be an important next step.
Figure 2.
Validating targets from simple to context-specific experimental models of AKI and subsequently in human AKI. Several therapeutic targets (red circles) may be identified by initial studies in simple experimental models of AKI. These should then be tested in more context-specific experimental models of AKI. Some therapeutic targets, albeit a smaller number, may be directly validated in context-specific animal models (yellow, blue, and light green circles). On the basis of studies in animal models (simple or context-specific), a limited number of therapeutic targets may be available for testing in human AKI. It is important to relate the findings seen with a given therapeutic target in human studies back to the experimental model system to gain better understanding of underlying mechanism(s). Reprinted from www.adqi.net, with permission.
Table 1.
Components of context-specific experimental AKI models
| Model | Susceptibilities | Exposure | Modifiers | Interventional Variables |
|---|---|---|---|---|
| Ischemia-reperfusion | Age | Aortic cross-clamp: | Fluids temperature | Timing: pre-, early post-, late postinsult |
| Genetic | Complete versus partial | Dose | ||
| CKD | Duration | |||
| Cardiopulmonary bypass | Age | Duration | Pump prime | Timing: pre-, early post-, late postinsult |
| Genetic | Mannitol | Dose | ||
| CKD | Loop diuretics | |||
| Temperature | ||||
| Transfusion | ||||
| Sepsis | Age | LPS (type, route, dose) | Fluid resuscitation: | Timing: pre-, early post-, late postinsult |
| Genetic | Cecal ligation and puncture | Route (iv, ip) | Dose | |
| CKD | Pneumonia | Volume | ||
| Type (crystalloids, colloids) | ||||
| Antibiotic therapy | ||||
| Contrast-induced AKI | Age | Radiocontrast type: | Fluid resuscitation: | Timing: pre-, early post-, late postinsult |
| Genetic | Ionic versus nonionic | Volume | Dose | |
| CKD | Osmolality | Type (crystalloid choice: saline, bicarbonate) | ||
| DM | Contrast volume | Timing (pre-, during, postcontrast) | ||
| Proteinuria | Contrast route: | |||
| Obesity | iv versus ia | |||
| Volume depletion |
Table 2.
Examples of specific targets and timing of therapies in experimental models of AKI
| Targets, Agents, Models | Timing of Therapy | ||
|---|---|---|---|
| Preinsult | Early postinsult (<6 hours) | Late postinsult (>6 hours) | |
| Cell membrane | |||
| S1P agonists | |||
| Mouse IRI86–88 | +++ | ||
| Rat IRI89 | +++ | ||
| Thromboxane receptor antagonists | + | ||
| Mouse (LPS)90 | ++ | ||
| Rat IRI91 | + | ||
| Omega-3 derivatives—resolvins, protectin D1 | |||
| Mouse IRI (PD1, 17-OH-DHA)92 | ++ | ++ | |
| Endoplasmic reticulum | |||
| EPO rat cisplatin93 | ? | ||
| EET analogues rat cisplatin94 | +++ | ||
| Mitochondria | |||
| Mitochondria protectant: | |||
| Cyclosporin A (inhibit MPT): rat IRI | ++++ | ||
| Minocycline (increase Bcl2): rat IRI95 | +++ (24 hours before) | ||
| mdivi-1 (prevent fission): mouse IR and cisplatin25 | +++ | ||
| Nucleophosmin/Bax blocking peptide: mouse IRI96 | +++ | ||
| Mitochondrial biogenesis stimulators | |||
| Rat IRI (SRT1720)97 | + | ||
| Mouse folate (sildenafil)98 | +++ | ||
| Mitochondrially targeted antioxidants | |||
| Rat IRI (SS-31)30 | +++ | ||
| Mouse cisplatin (MitoQ, Mito-CP)34 | +++ | ||
| Receptors | |||
| Angiopoietin-1 and Tie2 agonists | |||
| Mouse IRI (COMP-Ang1)99 | +++ | ||
| Mouse CLP (vasculotide)100 | ++ | ||
| HMGB1 antagonists | + | ||
| Mouse 5/6Nx + CLP (Ab)77 | +++ | ||
| Mouse IRI (ethyl pyruvate)101 | +++ | ||
| Mouse IRI (Ab)102 | +++ | ||
| Mouse IRI (rHMGB1 preconditioning)103 | |||
| Alpha-7 nicotinic acetylcholine receptor agonists | |||
| Mouse IRI (nicotine)104 | +++ | ||
| Mouse IRI (ultrasound)105 | +++ | ||
| Rat IRI (nicotine)106 | +++ | ||
| Rat IRI (GTS-21)106 | ++ | ||
| Mouse LPS (nicotine)107 | + | ||
| Mouse LPS (GTS-21)107 | ++ | ||
| SDF-1-CXCR4 agonists | |||
| Mouse CLP (endothelial progenitor cells)108 | +++ | ||
| Endothelin receptor antagonists | |||
| Dog IRI109 | ++ | +++ | ++ |
| Rat IRI110–112 | |||
| IGF-1 | |||
| Rat IRI113,114 | +++ | ||
| Human IRI115 | + | ||
Scoring of protective effect: ++++, complete (≥80%) protection; +++, substantial (50%–79%) protection; ++, partial (30%–49%) protection; +, minor (10%–29%) protection; -: negligible (<10%) protection.
What Are the Clinical Correlates of these Animal Models in Human AKI?
Numerous candidate agents have shown therapeutic activity in preclinical experimental models of AKI, but none of these has been confirmed in a successful phase III clinical trial. Accordingly, although a number of development programs and early-phase clinical trials of promising agents are in progress, there is no approved drug for the prevention or therapy of AKI.80 The vast majority of successful preclinical experiments to date have been prophylactic, with exposure to the protective agent before an ischemic, septic, or nephrotoxic insult.81 Fewer experimental models also include early postinsult exposures, which in some cases are successful. However, a major weakness of current preclinical experimental AKI models is that they do not routinely incorporate a more delayed secondary prevention/therapeutic component, with late addition of therapy when AKI is already developing. Ideally, such a model should find protective activity of therapy beyond 6 hours postinsult; realistically, of course, because clinical AKI is not routinely identified until 1 or more days postinsult(s), activity at even later time points would be more likely to be translated successfully. Although there are some clinical settings in which a predictable insult makes a purely prophylactic approach possible—e.g., contrast-induced AKI, or AKI induced by cardiac or aortic surgery—this is the minority of severe AKI in clinical practice. In contrast, most cases of severe, clinically significant AKI in modern practice are not predictable and are often caused by the interaction of multiple insults (ischemic, nephrotoxic, inflammatory) against a background of multiple comorbidities. Taken together with the other limitations in preclinical models of human AKI (complexities of age, preinsult CKD, other comorbidities, practice variability in concurrent supportive care, etc.), it is not surprising that although preclinical models remain useful to identify mechanisms of kidney damage, successful translation to clinical therapeutics has failed to date. It is clear that we must thoughtfully re-evaluate our approach to drug target and candidate development for the indication of AKI prevention and/or therapy, focusing on improved clinical relevance of preclinical experiments, to improve the odds of successful translation.
Furthermore, after target validation in context-specific animal models, as discussed above, preclinical models and early-phase clinical trials should be used to identify appropriate predictive biomarkers to guide selection, timing, and monitoring of therapy in pivotal phase III human clinical trials. This initiative should build on current efforts to use biomarkers of kidney damage to provide correlative evidence of efficacy (along with markers of renal function) in proof-of-concept phase II trials, and to use such biomarkers to trigger early postinsult enrollment in future clinical trials (not successfully achieved to date).82,83 Ideally, such predictive biomarkers should be validated to become companion diagnostics that can effectively personalize AKI therapy in clinical practice, matching susceptible patients with AKI with the correct mechanistically targeted therapy at the right time to target the precise phase of evolution of injury. As part of drug development, there should also be an iterative process from bedside back to bench to utilize results (both positive and negative) to help inform and develop more appropriate context-specific AKI models (Figure 2).
How Can We Improve the Translation of these Models to Achieve the Effective Diagnosis and Therapy of AKI?
Harmonization between academia and industry, for more clinically relevant preclinical testing of potential therapeutic targets and better translational clinical-trial design, is urgently needed to achieve the goal of developing AKI therapies. This is an entirely unmet need that must be approached more thoughtfully by all stakeholders in the field, and certain deficiencies are clearly remediable. Specifically, preclinical models can be significantly improved to enhance their clinical relevance, and clinical trials can become more thoughtfully translational. Preclinical models incorporating delayed administration of candidate AKI interventions should be prioritized. Although more sophisticated context-specific models are also a priority, it is vital not to neglect the simple imperative to include significantly delayed administration (secondary prevention) of candidate AKI therapies in comprehensive dose-response and time-action studies. Furthermore, both preclinical and clinical studies of AKI should be designed to incorporate the acquisition of biologic samples (including blood, urine, and, where possible, tissue) and imaging to discover and validate biomarkers that are predictive of drug response and toxicity to guide the initiation, monitoring, and titration of novel AKI therapies. Clinical trials in AKI should similarly have a comprehensive translational research program (informed by preclinical discoveries) to optimize the understanding of positive and negative studies with appropriate phase II and phase III end points,84,85 and to facilitate ancillary studies with biologic samples and/or imaging that may lead to the development of companion diagnostics. Although it is recognized that such efforts add significantly to the complexity and expense of drug discovery and translation to clinical use, it must be recognized that such tools have been crucial to the successful development of targeted therapies in other challenging fields—e.g., cancer, HIV, etc.—and our failures to date in AKI add urgency to any call for a more sophisticated approach.
Consensus Statements
Broaden the scope of preclinical models—We have identified a number of cellular and molecular targets in epithelial cells that are relevant to the pathogenesis of AKI. Any target that is identified needs to be validated in more than one animal model. These would include models beyond ischemia-reperfusion injury, such as sepsis, nephrotoxins, and others (especially cardiopulmonary bypass).
Develop more context-specific models with relevance to human AKI for testing of targets—These should replicate the initial insults in clinical settings, but also consider comorbidities that would alter patient susceptibility, such as underlying diabetes, aging, obesity, and CKD.
Integrate a focus on predictive and mechanistically informative biomarkers in early-phase clinical trials—After target validation in context-specific animal models, early-phase clinical trials should seek to identify appropriate predictive biomarkers to guide selection, timing, and monitoring of therapy in human clinical trials.
Modify preclinical approaches on the basis of clinical results—These should be an iterative process from bedside back to bench to utilize both positive and negative results to inform and develop more appropriate context-specific models.
Expand the preclinical therapeutic focus to secondary prevention and therapy of established AKI—The vast majority of agents that have been effective in preclinical studies of AKI have only been used prophylactically, and only a subset have been tested in clinical studies.
Map the evolution and extent of context-specific renal injury—To trigger appropriately timed and mechanistically targeted therapy appropriate to the phase of AKI evolution.
Create an experimental hub—Development of an AKI preclinical models consortium for evaluating and testing of better context-specific models.
Build collaborations among stakeholders—Harmonization between academia and industry for preclinical testing and better trial development for potential therapeutic targets.
Emphasize multifunctional clinical trials—Clinical trials in AKI should have a comprehensive research effort to optimize understanding of positive and negative clinical studies and allow for ancillary studies with biologic samples and/or imaging.
Account for CKD in studies of AKI—Furthermore, these clinical studies have used patients with underlying CKD to maximize the risk for developing AKI; this leads to a selection of subpopulations of patients with greater risk for AKI and a possibly more complex underlying mechanism of AKI, which may not have been evaluated in the preclinical model.
Methods
The 13th Acute Dialysis Quality Initiative meeting (April 11–13, 2014, Charlottesville, Virginia) on “Therapeutic Targets of Human Acute Kidney Injury: Harmonizing Human and Animal AKI, 2014” assembled experts in the area, including nephrologists, intensivists, pediatricians, emergency physicians, and physiologists (a list of participants is available in Supplemental Appendix 1), and performed a modified Delphi analysis of the existing literature. The Delphi method is a structured and standardized process for collecting, summarizing, and disseminating knowledge from a group of experts focused on a specific problem or task. Further information is available at www.adqi.net.
Before the meeting, the working subgroup “Cellular and Molecular Mechanisms” developed a list of preliminary questions and objectives with particular focus on identifying the cellular and molecular targets in the pathogenesis of AKI. It was recognized that the work was a continuation of the work of other groups, in particular the work of the subgroup “Inflammation.”
The group performed a literature search using the MEDLINE database (via the PubMED interface) using the following search terms: “cellular,” “molecular,” “pathways,” “pathogenesis,” and “acute kidney injury.” The group searched bibliographies of relevant review articles or editorials and personal records of participating members for any additional potentially relevant studies. After review of the literature, the group summarized the existing evidence. In case of lack of evidence on specific key areas, the working subgroup formulated consensus statements and questions for future research.
Disclosures
The following report no conflicts of interest: A.A., Z.D., R.H., P.M., S.P., M.R., and C.R.
J.K. has received consulting fees from Abbott Laboratories (Alameda, CA), Aethlon, Alere, Alung, AM Pharma, Astute Medical, Atox Bio, Baxter, Cytosorbents, venBio, Gambro, Grifols, Roche, Spectral Diagnostics, Sangart, and Siemens. J.K. has also received research grants from Alere, Astute Medical, Atox Bio, Bard, Baxter, Cytosorbents, Gambro, Grifols, Kaneka, and Spectral Diagnostics, and has licensed technologies through the University of Pittsburgh to Astute Medical, Cytosorbents, and Spectral Diagnostics.
Supplementary Material
Acknowledgments
This work was supported in part by US National Institutes of Health (NIH) grants R01-DK059600 and P30-DK079337 (to A.A.); NIH grants R01-DK058831 and R01-DK087843 and a Veterans Administration Merit Review Award (to Z.D.); a Veterans Administration Merit Award and NIH grants R01-DK38226 and R01-DK51265 (to R.C.H.); and a grant from the American Diabetes Association and NIH R01-DK0950972, R01-HL093234, and R01-HL125275 (to S.M.P.).
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2015070740/-/DCSupplemental.
References
- 1.Zager RA: Plasma membrane cholesterol: a critical determinant of cellular energetics and tubular resistance to attack. Kidney Int 58: 193–205, 2000 [DOI] [PubMed] [Google Scholar]
- 2.Zager RA, Kalhorn TF: Changes in free and esterified cholesterol: hallmarks of acute renal tubular injury and acquired cytoresistance. Am J Pathol 157: 1007–1016, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lorz C, Ortiz A, Justo P, González-Cuadrado S, Duque N, Gómez-Guerrero C, Egido J: Proapoptotic Fas ligand is expressed by normal kidney tubular epithelium and injured glomeruli. J Am Soc Nephrol 11: 1266–1277, 2000 [DOI] [PubMed] [Google Scholar]
- 4.Mahmoudi M, Willgoss D, Cuttle L, Yang T, Pat B, Winterford C, Endre Z, Johnson DW, Gobé GC: In vivo and in vitro models demonstrate a role for caveolin-1 in the pathogenesis of ischaemic acute renal failure. J Pathol 200: 396–405, 2003 [DOI] [PubMed] [Google Scholar]
- 5.Fujigaki Y, Sakakima M, Sun Y, Goto T, Ohashi N, Fukasawa H, Tsuji T, Yamamoto T, Hishida A: Immunohistochemical study on caveolin-1alpha in regenerating process of tubular cells in gentamicin-induced acute tubular injury in rats. Virchows Arch 450: 671–681, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Kwon TH, Frøkiaer J, Han JS, Knepper MA, Nielsen S: Decreased abundance of major Na(+) transporters in kidneys of rats with ischemia-induced acute renal failure. Am J Physiol Renal Physiol 278: F925–F939, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Peters E, van Elsas A, Heemskerk S, Jonk L, van der Hoeven J, Arend J, Masereeuw R, Pickkers P: Alkaline phosphatase as a treatment of sepsis-associated acute kidney injury. J Pharmacol Exp Ther 344: 2–7, 2013 [DOI] [PubMed] [Google Scholar]
- 8.Kaushal GP, Haun RS, Herzog C, Shah SV: Meprin A metalloproteinase and its role in acute kidney injury. Am J Physiol Renal Physiol 304: F1150–F1158, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cantaluppi V, Gatti S, Medica D, Figliolini F, Bruno S, Deregibus MC, Sordi A, Biancone L, Tetta C, Camussi G: Microvesicles derived from endothelial progenitor cells protect the kidney from ischemia-reperfusion injury by microRNA-dependent reprogramming of resident renal cells. Kidney Int 82: 412–427, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Bruno S, Grange C, Collino F, Deregibus MC, Cantaluppi V, Biancone L, Tetta C, Camussi G: Microvesicles derived from mesenchymal stem cells enhance survival in a lethal model of acute kidney injury. PLoS One 7: e33115, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Linkermann A, Chen G, Dong G, Kunzendorf U, Krautwald S, Dong Z: Regulated cell death in AKI. J Am Soc Nephrol 25: 2689–2701, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Friedmann Angeli JP, Schneider M, Proneth B, Tyurina YY, Tyurin VA, Hammond VJ, Herbach N, Aichler M, Walch A, Eggenhofer E, Basavarajappa D, Rådmark O, Kobayashi S, Seibt T, Beck H, Neff F, Esposito I, Wanke R, Förster H, Yefremova O, Heinrichmeyer M, Bornkamm GW, Geissler EK, Thomas SB, Stockwell BR, O’Donnell VB, Kagan VE, Schick JA, Conrad M: Inactivation of the ferroptosis regulator Gpx4 triggers acute renal failure in mice. Nat Cell Biol 16: 1180–1191, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhatt K, Wei Q, Pabla N, Dong G, Mi QS, Liang M, Mei C, Dong Z: MicroRNA-687 Induced by Hypoxia-Inducible Factor-1 Targets Phosphatase and Tensin Homolog in Renal Ischemia-Reperfusion Injury. J Am Soc Nephrol 26: 1588–1596, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei Q, Bhatt K, He HZ, Mi QS, Haase VH, Dong Z: Targeted deletion of Dicer from proximal tubules protects against renal ischemia-reperfusion injury. J Am Soc Nephrol 21: 756–761, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhdanov DD, Fahmi T, Wang X, Apostolov EO, Sokolov NN, Javadov S, Basnakian AG: Regulation of Apoptotic Endonucleases by EndoG. DNA Cell Biol 34: 316–326, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Molitoris BA: Actin cytoskeleton in ischemic acute renal failure. Kidney Int 66: 871–883, 2004 [DOI] [PubMed] [Google Scholar]
- 17.Humphreys BD, Cantaluppi V, Portilla D, Singbartl K, Yang L, Rosner MH, Kellum JA, Ronco C, and Acute Dialysis Quality Initiative XIII Work Group: Targeting Endogenous Repair Pathways after AKI. J Am Soc Nephrol 27: XXX–XXX, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hodeify R, Megyesi J, Tarcsafalvi A, Mustafa HI, Hti Lar Seng NS, Price PM: Gender differences control the susceptibility to ER stress-induced acute kidney injury. Am J Physiol Renal Physiol 304: F875–F882, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taniguchi M, Yoshida H: Endoplasmic reticulum stress in kidney function and disease. Curr Opin Nephrol Hypertens 24: 345–350, 2015 [DOI] [PubMed] [Google Scholar]
- 20.Pagliarini DJ, Calvo SE, Chang B, Sheth SA, Vafai SB, Ong SE, Walford GA, Sugiana C, Boneh A, Chen WK, Hill DE, Vidal M, Evans JG, Thorburn DR, Carr SA, Mootha VK: A mitochondrial protein compendium elucidates complex I disease biology. Cell 134: 112–123, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trump BF, Valigorsky JM, Jones RT, Mergner WJ, Garcia JH, Cowley RA: The application of electron microscopy and cellular biochemistry to the autopsy. Observations on cellular changes in human shock. Hum Pathol 6: 499–516, 1975 [DOI] [PubMed] [Google Scholar]
- 22.Takasu O, Gaut JP, Watanabe E, To K, Fagley RE, Sato B, Jarman S, Efimov IR, Janks DL, Srivastava A, Bhayani SB, Drewry A, Swanson PE, Hotchkiss RS: Mechanisms of cardiac and renal dysfunction in patients dying of sepsis. Am J Respir Crit Care Med 187: 509–517, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perazella MA: Tenofovir-induced kidney disease: an acquired renal tubular mitochondriopathy. Kidney Int 78: 1060–1063, 2010 [DOI] [PubMed] [Google Scholar]
- 24.Parekh DJ, Weinberg JM, Ercole B, Torkko KC, Hilton W, Bennett M, Devarajan P, Venkatachalam MA: Tolerance of the human kidney to isolated controlled ischemia. J Am Soc Nephrol 24: 506–517, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brooks C, Wei Q, Cho SG, Dong Z: Regulation of mitochondrial dynamics in acute kidney injury in cell culture and rodent models. J Clin Invest 119: 1275–1285, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tran M, Tam D, Bardia A, Bhasin M, Rowe GC, Kher A, Zsengeller ZK, Akhavan-Sharif MR, Khankin EV, Saintgeniez M, David S, Burstein D, Karumanchi SA, Stillman IE, Arany Z, Parikh SM: PGC-1α promotes recovery after acute kidney injury during systemic inflammation in mice. J Clin Invest 121: 4003–4014, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zsengellér ZK, Ellezian L, Brown D, Horváth B, Mukhopadhyay P, Kalyanaraman B, Parikh SM, Karumanchi SA, Stillman IE, Pacher P: Cisplatin nephrotoxicity involves mitochondrial injury with impaired tubular mitochondrial enzyme activity. J Histochem Cytochem 60: 521–529, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zamzami N, Kroemer G: The mitochondrion in apoptosis: how Pandora’s box opens. Nat Rev Mol Cell Biol 2: 67–71, 2001 [DOI] [PubMed] [Google Scholar]
- 29.Dare AJ, Bolton EA, Pettigrew GJ, Bradley JA, Saeb-Parsy K, Murphy MP: Protection against renal ischemia-reperfusion injury in vivo by the mitochondria targeted antioxidant MitoQ. Redox Biol 5: 163–168, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Szeto HH, Liu S, Soong Y, Wu D, Darrah SF, Cheng FY, Zhao Z, Ganger M, Tow CY, Seshan SV: Mitochondria-targeted peptide accelerates ATP recovery and reduces ischemic kidney injury. J Am Soc Nephrol 22: 1041–1052, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mewton, N, Cung, TT, Morel, O, Cayla, G, Bonnefoy-Cudraz, E, Rioufol, G, Angoulvant, D, Guerin, P, Elbaz, M, Delarche, N, Coste, P, Vanzetto, G, Metge, M, Aupetit, JF, Jouve, B, Motreff, P, Tron, C, Labeque, JN, Steg, PG, Cottin, Y, Range, G, Clerc, J, Coussement, P, Prunier, F, Moulin, F, Roth, O, Belle, L, Dubois, P, Barragan, P, Gilard, M, Piot, C, Colin, P, Morice, MC, Monassier, JP, Ider, O, Dubois-Rande, JL, Unterseeh, T, Lebreton, H, Beard, T, Blanchard, D, Grollier, G, Malquarti, V, Staat, P, Sudre, A, Hansson, MJ, Elmer, E, Boussaha, I, Jossan, C, Torner, A, Claeys, M, Garcia-Dorado, D, Ovize, M, and CIRCUS Study Investigators: Rationale and design of the Cyclosporine to ImpRove Clinical oUtcome in ST-elevation myocardial infarction patients (the CIRCUS trial). Am Heart J 169(6): 758–766.e6, 2015 [DOI] [PubMed]
- 32.Puigserver P, Wu Z, Park CW, Graves R, Wright M, Spiegelman BM: A cold-inducible coactivator of nuclear receptors linked to adaptive thermogenesis. Cell 92: 829–839, 1998 [DOI] [PubMed] [Google Scholar]
- 33.Funk JA, Schnellmann RG: Persistent disruption of mitochondrial homeostasis after acute kidney injury. Am J Physiol Renal Physiol 302: F853–F864, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mukhopadhyay P, Horváth B, Zsengellér Z, Zielonka J, Tanchian G, Holovac E, Kechrid M, Patel V, Stillman IE, Parikh SM, Joseph J, Kalyanaraman B, Pacher P: Mitochondrial-targeted antioxidants represent a promising approach for prevention of cisplatin-induced nephropathy. Free Radic Biol Med 52: 497–506, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brooks C, Cho SG, Wang CY, Yang T, Dong Z: Fragmented mitochondria are sensitized to Bax insertion and activation during apoptosis. Am J Physiol Cell Physiol 300: C447–C455, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Youle RJ, van der Bliek AM: Mitochondrial fission, fusion, and stress. Science 337: 1062–1065, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ishihara M, Urushido M, Hamada K, Matsumoto T, Shimamura Y, Ogata K, Inoue K, Taniguchi Y, Horino T, Fujieda M, Fujimoto S, Terada Y: Sestrin-2 and BNIP3 regulate autophagy and mitophagy in renal tubular cells in acute kidney injury. Am J Physiol Renal Physiol 305: F495–F509, 2013 [DOI] [PubMed] [Google Scholar]
- 38.Gall JM, Wang Z, Liesa M, Molina A, Havasi A, Schwartz JH, Shirihai O, Borkan SC, Bonegio RG: Role of mitofusin 2 in the renal stress response. PLoS One 7: e31074, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gall JM, Wang Z, Bonegio RG, Havasi A, Liesa M, Vemula P, Borkan SC: Conditional knockout of proximal tubule mitofusin 2 accelerates recovery and improves survival after renal ischemia. J Am Soc Nephrol 26: 1092–1102, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gewin L, Vadivelu S, Neelisetty S, Srichai MB, Paueksakon P, Pozzi A, Harris RC, Zent R: Deleting the TGF-β receptor attenuates acute proximal tubule injury. J Am Soc Nephrol 23: 2001–2011, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gentle ME, Shi S, Daehn I, Zhang T, Qi H, Yu L, D’Agati VD, Schlondorff DO, Bottinger EP: Epithelial cell TGFβ signaling induces acute tubular injury and interstitial inflammation. J Am Soc Nephrol 24: 787–799, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen J, Chen JK, Harris RC: Deletion of the epidermal growth factor receptor in renal proximal tubule epithelial cells delays recovery from acute kidney injury. Kidney Int 82: 45–52, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou D, Tan RJ, Lin L, Zhou L, Liu Y: Activation of hepatocyte growth factor receptor, c-met, in renal tubules is required for renoprotection after acute kidney injury. Kidney Int 84: 509–520, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Okusa MD, Lynch KR: Targeting sphingosine 1 phosphate receptor type 1 receptors in acute kidney injury. Drug Discov Today Dis Mech 4: 55–59, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ranganathan P, Jayakumar C, Navankasattusas S, Li DY, Kim IM, Ramesh G: UNC5B receptor deletion exacerbates tissue injury in response to AKI. J Am Soc Nephrol 25: 239–249, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rabb H, Griffin MD, McKay DB, Swaminathan S, Pickkers P, Rosner MH, Kellum JA, Ronco C, and Acute Dialysis Quality Initiative Consensus XIII Work Group: Inflammation in AKI: Current Understanding, Key Questions, and Knowledge Gaps. J Am Soc Nephrol 27: XXX–XXX, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang L, Besschetnova TY, Brooks CR, Shah JV, Bonventre JV: Epithelial cell cycle arrest in G2/M mediates kidney fibrosis after injury. Nat Med 16: 535–543, 1p, 143, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bonventre JV, Yang L: Cellular pathophysiology of ischemic acute kidney injury. J Clin Invest 121: 4210–4221, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Megyesi J, Safirstein RL, Price PM: Induction of p21WAF1/CIP1/SDI1 in kidney tubule cells affects the course of cisplatin-induced acute renal failure. J Clin Invest 101: 777–782, 1998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Megyesi J, Udvarhelyi N, Safirstein RL, Price PM: The p53-independent activation of transcription of p21 WAF1/CIP1/SDI1 after acute renal failure. Am J Physiol 271: F1211–F1216, 1996 [DOI] [PubMed] [Google Scholar]
- 51.Zhang D, Liu Y, Wei Q, Huo Y, Liu K, Liu F, Dong Z: Tubular p53 regulates multiple genes to mediate acute kidney injury. J Am Soc Nephrol 25: 2278–2289, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Price PM, Safirstein RL, Megyesi J: Protection of renal cells from cisplatin toxicity by cell cycle inhibitors. Am J Physiol Renal Physiol 286: F378–F384, 2004 [DOI] [PubMed] [Google Scholar]
- 53.Jiang M, Yi X, Hsu S, Wang CY, Dong Z: Role of p53 in cisplatin-induced tubular cell apoptosis: dependence on p53 transcriptional activity. Am J Physiol Renal Physiol 287: F1140–F1147, 2004 [DOI] [PubMed] [Google Scholar]
- 54.Kelly KJ, Plotkin Z, Vulgamott SL, Dagher PC: P53 mediates the apoptotic response to GTP depletion after renal ischemia-reperfusion: protective role of a p53 inhibitor. J Am Soc Nephrol 14: 128–138, 2003 [DOI] [PubMed] [Google Scholar]
- 55.Pabla N, Huang S, Mi QS, Daniel R, Dong Z: ATR-Chk2 signaling in p53 activation and DNA damage response during cisplatin-induced apoptosis. J Biol Chem 283: 6572–6583, 2008 [DOI] [PubMed] [Google Scholar]
- 56.Pabla N, Ma Z, McIlhatton MA, Fishel R, Dong Z: hMSH2 recruits ATR to DNA damage sites for activation during DNA damage-induced apoptosis. J Biol Chem 286: 10411–10418, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang D, Liu Y, Wei Q, Huo Y, Liu K, Liu F, Dong Z: Tubular p53 regulates multiple genes to mediate AKI. J Am Soc Nephrol 25: 2278–2289, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jiang M, Dong Z: Regulation and pathological role of p53 in cisplatin nephrotoxicity. J Pharmacol Exp Ther 327: 300–307, 2008 [DOI] [PubMed] [Google Scholar]
- 59.Chawla LS, Kimmel PL: Acute kidney injury and chronic kidney disease: an integrated clinical syndrome. Kidney Int 82: 516–524, 2012 [DOI] [PubMed] [Google Scholar]
- 60.Venkatachalam MA, Griffin KA, Lan R, Geng H, Saikumar P, Bidani AK: Acute kidney injury: a springboard for progression in chronic kidney disease. Am J Physiol Renal Physiol 298: F1078–F1094, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kashani K, Al-Khafaji A, Ardiles T, Artigas A, Bagshaw SM, Bell M, Bihorac A, Birkhahn R, Cely CM, Chawla LS, Davison DL, Feldkamp T, Forni LG, Gong MN, Gunnerson KJ, Haase M, Hackett J, Honore PM, Hoste EA, Joannes-Boyau O, Joannidis M, Kim P, Koyner JL, Laskowitz DT, Lissauer ME, Marx G, McCullough PA, Mullaney S, Ostermann M, Rimmelé T, Shapiro NI, Shaw AD, Shi J, Sprague AM, Vincent JL, Vinsonneau C, Wagner L, Walker MG, Wilkerson RG, Zacharowski K, Kellum JA: Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care 17(1): R25, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Livingston MJ, Dong Z: Autophagy in acute kidney injury. Semin Nephrol 34: 17–26, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Suzuki C, Isaka Y, Takabatake Y, Tanaka H, Koike M, Shibata M, Uchiyama Y, Takahara S, Imai E: Participation of autophagy in renal ischemia/reperfusion injury. Biochem Biophys Res Commun 368: 100–106, 2008 [DOI] [PubMed] [Google Scholar]
- 64.Chien CT, Shyue SK, Lai MK: Bcl-xL augmentation potentially reduces ischemia/reperfusion induced proximal and distal tubular apoptosis and autophagy. Transplantation 84: 1183–1190, 2007 [DOI] [PubMed] [Google Scholar]
- 65.Jiang M, Liu K, Luo J, Dong Z: Autophagy is a renoprotective mechanism during in vitro hypoxia and in vivo ischemia-reperfusion injury. Am J Pathol 176: 1181–1192, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bolisetty S, Traylor AM, Kim J, Joseph R, Ricart K, Landar A, Agarwal A: Heme oxygenase-1 inhibits renal tubular macroautophagy in acute kidney injury. J Am Soc Nephrol 21: 1702–1712, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Periyasamy-Thandavan S, Jiang M, Wei Q, Smith R, Yin XM, Dong Z: Autophagy is cytoprotective during cisplatin injury of renal proximal tubular cells. Kidney Int 74: 631–640, 2008 [DOI] [PubMed] [Google Scholar]
- 68.Jiang M, Wei Q, Dong G, Komatsu M, Su Y, Dong Z: Autophagy in proximal tubules protects against acute kidney injury. Kidney Int 82: 1271–1283, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li L, Zepeda-Orozco D, Black R, Lin F: Autophagy is a component of epithelial cell fate in obstructive uropathy. Am J Pathol 176: 1767–1778, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Koesters R, Kaissling B, Lehir M, Picard N, Theilig F, Gebhardt R, Glick AB, Hähnel B, Hosser H, Gröne HJ, Kriz W: Tubular overexpression of transforming growth factor-beta1 induces autophagy and fibrosis but not mesenchymal transition of renal epithelial cells. Am J Pathol 177: 632–643, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lan R, Geng H, Polichnowski AJ, Singha PK, Saikumar P, McEwen DG, Griffin KA, Koesters R, Weinberg JM, Bidani AK, Kriz W, Venkatachalam MA: PTEN loss defines a TGF-β-induced tubule phenotype of failed differentiation and JNK signaling during renal fibrosis. Am J Physiol Renal Physiol 302: F1210–F1223, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hasegawa K, Wakino S, Yoshioka K, Tatematsu S, Hara Y, Minakuchi H, Sueyasu K, Washida N, Tokuyama H, Tzukerman M, Skorecki K, Hayashi K, Itoh H: Kidney-specific overexpression of Sirt1 protects against acute kidney injury by retaining peroxisome function. J Biol Chem 285: 13045–13056, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sander JD, Joung JK: CRISPR-Cas systems for editing, regulating and targeting genomes. Nat Biotechnol 32: 347–355, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Heyman SN, Brezis M, Reubinoff CA, Greenfeld Z, Lechene C, Epstein FH, Rosen S: Acute renal failure with selective medullary injury in the rat. J Clin Invest 82: 401–412, 1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Miyaji T, Hu X, Yuen PS, Muramatsu Y, Iyer S, Hewitt SM, Star RA: Ethyl pyruvate decreases sepsis-induced acute renal failure and multiple organ damage in aged mice. Kidney Int 64: 1620–1631, 2003 [DOI] [PubMed] [Google Scholar]
- 76.Doi K, Leelahavanichkul A, Yuen PS, Star RA: Animal models of sepsis and sepsis-induced kidney injury. J Clin Invest 119: 2868–2878, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Leelahavanichkul A, Huang Y, Hu X, Zhou H, Tsuji T, Chen R, Kopp JB, Schnermann J, Yuen PS, Star RA: Chronic kidney disease worsens sepsis and sepsis-induced acute kidney injury by releasing High Mobility Group Box Protein-1. Kidney Int 80: 1198–1211, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Peng J, Li X, Zhang D, Chen JK, Su Y, Smith SB, Dong Z: Hyperglycemia, p53, and mitochondrial pathway of apoptosis are involved in the susceptibility of diabetic models to ischemic acute kidney injury. Kidney Int 87: 137–150, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pabla N, Dong G, Jiang M, Huang S, Kumar MV, Messing RO, Dong Z: Inhibition of PKCδ reduces cisplatin-induced nephrotoxicity without blocking chemotherapeutic efficacy in mouse models of cancer. J Clin Invest 121: 2709–2722, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Faubel S, Chawla LS, Chertow GM, Goldstein SL, Jaber BL, Liu KD; Acute Kidney Injury Advisory Group of the American Society of Nephrology : Ongoing clinical trials in AKI. Clin J Am Soc Nephrol 7: 861–873, 2012 [DOI] [PubMed] [Google Scholar]
- 81.Palevsky PM, Molitoris BA, Okusa MD, Levin A, Waikar SS, Wald R, Chertow GM, Murray PT, Parikh CR, Shaw AD, Go AS, Faubel SG, Kellum JA, Chinchilli VM, Liu KD, Cheung AK, Weisbord SD, Chawla LS, Kaufman JS, Devarajan P, Toto RM, Hsu CY, Greene T, Mehta RL, Stokes JB, Thompson AM, Thompson BT, Westenfelder CS, Tumlin JA, Warnock DG, Shah SV, Xie Y, Duggan EG, Kimmel PL, Star RA: Design of clinical trials in acute kidney injury: report from an NIDDK workshop on trial methodology. Clin J Am Soc Nephrol 7: 844–850, 2012 [DOI] [PubMed] [Google Scholar]
- 82.Murray PT: Acute kidney injury biomarkers and endpoints for clinical trials. Contrib Nephrol 171: 208–212, 2011 [DOI] [PubMed] [Google Scholar]
- 83.Murray PT, Mehta RL, Shaw A, Ronco C, Endre Z, Kellum JA, Chawla LS, Cruz D, Ince C, Okusa MD; ADQI 10 workgroup : Potential use of biomarkers in acute kidney injury: report and summary of recommendations from the 10th Acute Dialysis Quality Initiative consensus conference. Kidney Int 85: 513–521, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Murray PT, Le Gall JR, Dos Reis Miranda D, Pinsky MR, Tetta C: Physiologic endpoints (efficacy) for acute renal failure studies. Curr Opin Crit Care 8: 519–525, 2002 [DOI] [PubMed] [Google Scholar]
- 85.Palevsky PM, Metnitz PG, Piccinni P, Vinsonneau C: Selection of endpoints for clinical trials of acute renal failure in critically ill patients. Curr Opin Crit Care 8: 515–518, 2002 [DOI] [PubMed] [Google Scholar]
- 86.Bajwa A, Jo SK, Ye H, Huang L, Dondeti KR, Rosin DL, Haase VH, Macdonald TL, Lynch KR, Okusa MD: Activation of sphingosine-1-phosphate 1 receptor in the proximal tubule protects against ischemia-reperfusion injury. J Am Soc Nephrol 21: 955–965, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lien YH, Yong KC, Cho C, Igarashi S, Lai LW: S1P(1)-selective agonist, SEW2871, ameliorates ischemic acute renal failure. Kidney Int 69: 1601–1608, 2006 [DOI] [PubMed] [Google Scholar]
- 88.Park SW, Kim JY, Ham A, Brown KM, Kim M, D’Agati VD, Lee HT: A1 adenosine receptor allosteric enhancer PD-81723 protects against renal ischemia-reperfusion injury. Am J Physiol Renal Physiol 303: F721–F732, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Delbridge MS, Shrestha BM, Raftery AT, El Nahas AM, Haylor JL: Reduction of ischemia-reperfusion injury in the rat kidney by FTY720, a synthetic derivative of sphingosine. Transplantation 84: 187–195, 2007 [DOI] [PubMed] [Google Scholar]
- 90.Boffa JJ, Just A, Coffman TM, Arendshorst WJ: Thromboxane receptor mediates renal vasoconstriction and contributes to acute renal failure in endotoxemic mice. J Am Soc Nephrol 15: 2358–2365, 2004 [DOI] [PubMed] [Google Scholar]
- 91.Kramer HJ, Mohaupt MG, Pinoli F, Bäcker A, Meyer-Lehnert H, Schlebusch H: Effects of thromboxane A2 receptor blockade on oliguric ischemic acute renal failure in conscious rats. J Am Soc Nephrol 4: 50–57, 1993 [DOI] [PubMed] [Google Scholar]
- 92.Duffield JS, Hong S, Vaidya VS, Lu Y, Fredman G, Serhan CN, Bonventre JV: Resolvin D series and protectin D1 mitigate acute kidney injury. J Immunol 177: 5902–5911, 2006 [DOI] [PubMed] [Google Scholar]
- 93.Kong D, Zhuo L, Gao C, Shi S, Wang N, Huang Z, Li W, Hao L: Erythropoietin protects against cisplatin-induced nephrotoxicity by attenuating endoplasmic reticulum stress-induced apoptosis. J Nephrol 26: 219–227, 2013 [DOI] [PubMed] [Google Scholar]
- 94.Khan MA, Liu J, Kumar G, Skapek SX, Falck JR, Imig JD: Novel orally active epoxyeicosatrienoic acid (eet) analogs attenuate cisplatin nephrotoxicity. FASEB J 27: 2946–2956, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Wang J, Wei Q, Wang CY, Hill WD, Hess DC, Dong Z: Minocycline up-regulates bcl-2 and protects against cell death in mitochondria. J Biol Chem 279: 19948–19954, 2004 [DOI] [PubMed] [Google Scholar]
- 96.Wang Z, Gall JM, Bonegio R, Havasi A, Illanes K, Schwartz JH, Borkan SC: Nucleophosmin, a critical bax cofactor in ischemia-induced cell death. Mol Cell Biol 33: 1916–1924, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Funk JA, Schnellmann RG: Accelerated recovery of renal mitochondrial and tubule homeostasis with SIRT1/PGC-1α activation following ischemia-reperfusion injury. Toxicol Appl Pharmacol 273: 345–354, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Whitaker RM, Wills LP, Stallons LJ, Schnellmann RG: cGMP-selective phosphodiesterase inhibitors stimulate mitochondrial biogenesis and promote recovery from acute kidney injury. J Pharmacol Exp Ther 347: 626–634, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jung YJ, Kim DH, Lee AS, Lee S, Kang KP, Lee SY, Jang KY, Sung MJ, Park SK, Kim W: Peritubular capillary preservation with COMP-angiopoietin-1 decreases ischemia-reperfusion-induced acute kidney injury. Am J Physiol Renal Physiol 297: F952–F960, 2009 [DOI] [PubMed] [Google Scholar]
- 100.Kumpers P, Gueler F, David S, Slyke PV, Dumont DJ, Park JK, Bockmeyer CL, Parikh SM, Pavenstadt H, Haller H, Shushakova N: The synthetic tie2 agonist peptide vasculotide protects against vascular leakage and reduces mortality in murine abdominal sepsis. Crit Care 15: R261, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Rabadi MM, Ghaly T, Goligorksy MS, Ratliff BB: HMGB1 in renal ischemic injury. Am J Physiol Renal Physiol 303: F873–F885, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Li J, Gong Q, Zhong S, Wang L, Guo H, Xiang Y, Ichim TE, Wang CY, Chen S, Gong F, Chen G: Neutralization of the extracellular HMGB1 released by ischaemic damaged renal cells protects against renal ischaemia-reperfusion injury. Nephrol Dial Transplant 26: 469–478, 2011 [DOI] [PubMed] [Google Scholar]
- 103.Wu H, Steenstra R, de Boer EC, Zhao CY, Ma J, van der Stelt JM, Chadban SJ: Preconditioning with recombinant high-mobility group box 1 protein protects the kidney against ischemia-reperfusion injury in mice. Kidney Int 85: 824–832, 2014 [DOI] [PubMed] [Google Scholar]
- 104.Sadis C, Teske G, Stokman G, Kubjak C, Claessen N, Moore F, Loi P, Diallo B, Barvais L, Goldman M, Florquin S, Le Moine A: Nicotine protects kidney from renal ischemia/reperfusion injury through the cholinergic anti-inflammatory pathway. PLoS One 2: e469, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gigliotti JC, Huang L, Ye H, Bajwa A, Chattrabhuti K, Lee S, Klibanov AL, Kalantari K, Rosin DL, Okusa MD: Ultrasound prevents renal ischemia-reperfusion injury by stimulating the splenic cholinergic anti-inflammatory pathway. J Am Soc Nephrol 24: 1451–1460, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yeboah MM, Xue X, Duan B, Ochani M, Tracey KJ, Susin M, Metz CN: Cholinergic agonists attenuate renal ischemia-reperfusion injury in rats. Kidney Int 74: 62–69, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chatterjee PK, Yeboah MM, Dowling O, Xue X, Powell SR, Al-Abed Y, Metz CN: Nicotinic acetylcholine receptor agonists attenuate septic acute kidney injury in mice by suppressing inflammation and proteasome activity. PLoS One 7: e35361, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Fan H, Goodwin AJ, Chang E, Zingarelli B, Borg K, Guan S, Halushka PV, Cook JA: Endothelial progenitor cells and a stromal cell-derived factor-1α analogue synergistically improve survival in sepsis. Am J Respir Crit Care Med 189: 1509–1519, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Roux S, Qiu C, Sprecher U, Osterwalder R, Clozel JP: Protective effects of endothelin receptor antagonists in dogs with aortic cross-clamping. J Cardiovasc Pharmacol 34: 199–205, 1999 [DOI] [PubMed] [Google Scholar]
- 110.Gellai M, Jugus M, Fletcher T, DeWolf R, Nambi P: Reversal of postischemic acute renal failure with a selective endothelin A receptor antagonist in the rat. J Clin Invest 93: 900–906, 1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Knoll T, Schult S, Birck R, Braun C, Michel MS, Bross S, Juenemann KP, Kirchengast M, Rohmeiss P: Therapeutic administration of an endothelin-A receptor antagonist after acute ischemic renal failure dose-dependently improves recovery of renal function. J Cardiovasc Pharmacol 37: 483–488, 2001 [DOI] [PubMed] [Google Scholar]
- 112.Wilhelm SM, Stowe NT, Robinson AV, Schulak JA: The use of the endothelin receptor antagonist, tezosentan, before or after renal ischemia protects renal function. Transplantation 71: 211–216, 2001 [DOI] [PubMed] [Google Scholar]
- 113.Ding H, Kopple JD, Cohen A, Hirschberg R: Recombinant human insulin-like growth factor-I accelerates recovery and reduces catabolism in rats with ischemic acute renal failure. J Clin Invest 91: 2281–2287, 1993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Miller SB, Martin DR, Kissane J, Hammerman MR: Insulin-like growth factor I accelerates recovery from ischemic acute tubular necrosis in the rat. Proc Natl Acad Sci U S A 89: 11876–11880, 1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Franklin SC, Moulton M, Sicard GA, Hammerman MR, Miller SB: Insulin-like growth factor I preserves renal function postoperatively. Am J Physiol 272: F257–F259, 1997 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.