Abstract
Purpose
To determine risk factors for glaucoma in a population-based study in the United States.
Methods
Participants age 40 and older from the National Health and Nutrition Examination Survey underwent questionnaires, physical examination, laboratory tests, and vision tests including fundus imaging. Glaucoma was determined based on expert grading of fundus photographs. Regression modeling of glaucoma risk factors was performed.
Results
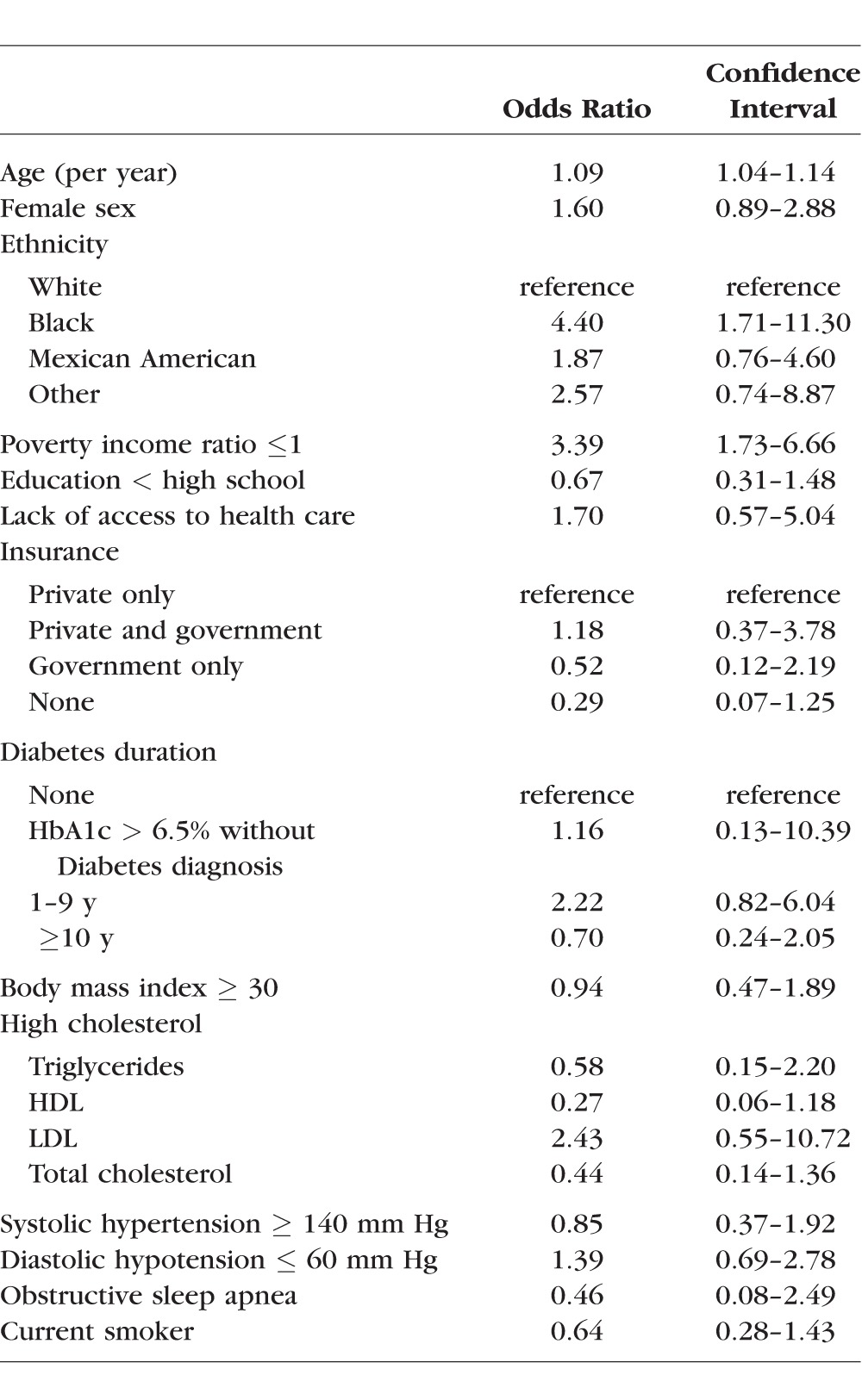
Participants with glaucoma (172) were older (mean age 68.1 [95% confidence interval (CI) 65.6–70.7] vs. 56.4 years [95% CI 55.6–57.2, P < 0.001]), likely to have less than high school education (25.1% vs. 18.1%, P = 0.05), to have diabetes (23.1% vs. 10.8%, P < 0.001), to have central obesity (72.5% vs. 60.7%, P = 0.01), to have systolic hypertension (30.3% vs. 20.1%, P = 0.01), to have diastolic hypotension (30.3% vs. 13.9%, P < 0.001), and to be nonsmokers (91.0% vs. 79.3%, P = 0.002). Sex, poverty, access to health care, fasting glucose, insulin dependence, body mass index, cholesterol levels, diastolic hypertension, systolic hypotension, obstructive sleep apnea, and marijuana were not associated with glaucoma. Multivariable modeling showed associations between glaucoma and older age (odds ratio [OR] 1.09 per year, 95% CI 1.04–1.14), black race (OR 4.40, 95% CI 1.71–11.30), and poverty (OR 3.39, 95% CI 1.73–6.66). Diabetes was no longer associated with glaucoma after adjustment for triglyceride levels. Sex, education, insurance status, body mass index, blood pressure, obstructive sleep apnea, and smoking were not associated with glaucoma.
Conclusions
People who are older, of black race, and with lower income levels have a higher prevalence of glaucoma. A novel association between diabetes, triglyceride levels, and glaucoma is also identified.
Keywords: glaucoma, glaucoma risk factors, NHANES
Ocular hypertension is an established risk factor for glaucoma, and treatments for glaucoma are primarily aimed at lowering intraocular pressure.1–4 Other risk factors for glaucoma prevalence include age, first-degree relatives with glaucoma, African American race, thinner central corneal thickness, observed features of the optic nerve, pseudoexfoliation, pigment dispersion, and myopia.5,6 Glaucoma has been also associated with both systemic hypertension7,8 and hypotension.8,9 Diabetes, hypothyroidism, obstructive sleep apnea, smoking tobacco cigarettes, and marijuana use have also been reported as risk factors for glaucoma, but evidence remains inconclusive.1,10–16 Although the literature on potential risk factors for glaucoma is extensive, most studies have been limited by the use of highly selected, nonrepresentative populations.
This study analyzes data from the National Health and Nutrition Examination Survey (NHANES) from 2005 to 2008, a representative sample of the US population. This phase of the NHANES included fundus imaging, questionnaires, physical examination, and laboratory data that can be used to identify risk factors for the presence of glaucoma in the US population.
Methods
The NHANES 2005–2008 protocol was reviewed and approved by the National Center for Health Statistics research ethics review board. Expert grading of disc photos was reviewed and approved by the Johns Hopkins University School of Medicine Institutional Review Board. Written informed consent was obtained from all participants. The study adhered to the tenets of the Declaration of Helsinki.
Study Population
The National Health and Nutrition Examination Survey is a representative cross-sectional survey of the civilian noninstitutionalized US population conducted by the National Center for Health Statistics of the Centers for Disease Control and Prevention, with ongoing surveys performed in 2-year cycles since 1999. Participants in NHANES complete a household interview and are invited for an extensive examination in a mobile examination center (MEC), including a physical examination, specialized measurements, and laboratory tests. We used data from the 2005 to 2008 cycles, when additional eye and vision testing including fundus imaging was performed in participants ≥ 40 years of age (n = 6797). We excluded 1051 participants with missing or ungradable fundus photographs. A detailed comparison of the characteristics of the participants who were included and excluded is available elsewhere (Gupta et al.17). The final sample included 5746 participants (2883 men and 2863 women).
Data Collection
Data on demographic characteristics, lifestyle habits, history of disease, medication use, diabetes, obstructive sleep apnea, smoking, marijuana use, socioeconomic status, insurance status, and access to health care were collected by standard questionnaires at the household interview.
Educational attainment was defined as less than high school if the participant reported having less than 12 years of schooling or equivalent. Poverty was defined as a poverty-to-income ratio (PIR) ≤ 1, where PIR is a ratio of family income to the poverty threshold. Access to health care and health insurance coverage at the time of survey were assessed via the questions “Is there a place you usually go when you are sick or need advice about your health”? and “Are you covered by health insurance or some other kind of health care plan”? We categorized health insurance as private only, government only, a combination of private and government, or no health insurance.
Self-reported diabetes was assessed by asking participants whether they had been informed by a doctor that they had diabetes, and at what age they received the diagnosis. This was then used to calculate the duration of diabetes since diagnosis. Participants also reported whether they required insulin for diabetes. Similarly, obstructive sleep apnea, smoking, and marijuana use were assessed by questionnaire. People who formerly smoked but had quit were defined as nonsmokers. A drug use questionnaire was administered to those less than 69 years of age. Marijuana use was defined as using marijuana at least 5 days per month, the median reported use determined during sensitivity testing.18,19
Anthropometry, blood pressure measurement, and collection of blood samples were performed at the MEC using standardized methods.18,19 Obesity was defined as a body mass index (BMI) greater than or equal to 30 kg/m2, and central obesity was defined as a waist circumference greater than 102 cm in men or 88 cm in women. Hypertension was defined as having a systolic pressure of 140 mm Hg or greater and a diastolic pressure of 90 mm Hg or greater. Hypotension was defined as having a systolic pressure of less than 90 mm Hg or a diastolic pressure of less than 60 mm Hg. We evaluated current blood pressure, as opposed to historic blood pressure; thus, a person who was previously hypertensive but is receiving medication could potentially be categorized as normotensive or hypotensive.
Participants were instructed to fast prior to measurements for glucose, triglyceride, and low-density lipoprotein (LDL) levels.18,19 Other laboratory testing included hemoglobin A1c (HbA1c), total cholesterol, and high-density lipoprotein (HDL).20 Tests that required fasting were performed for a subset of participants: Where appropriate, this was accounted for by weighting to account for sampling of half the study population.21,22 Hemoglobin A1c > 6.5%, fasting glucose > 125 mg/dL, total cholesterol greater than or equal to 240 mg/dL, HDL less than 40 mg/dL in men or 50 mg/dL in women, LDL ≥ 160 mg/dL, and triglycerides ≥ 200 mg/dL were evaluated as potential risk factors for glaucoma.
Grading of Optic Disc Photographs
Photographs of the optic nerve were obtained using a nonmydriatic fundus camera (CR6-45NM; Canon USA, Melville, NY, USA). Initial grading of cup-to-disc ratio (CDR) was performed at the University of Wisconsin Fundus Photograph Reading Center.23 All people with a CDR ≥ 0.6 in at least one eye per the reading center were regraded by three glaucoma specialists (DSF, MVB, PR) at the Wilmer Eye Institute. In addition, 180 participants with CDR < 0.6 in both eyes on initial grading were randomly selected for review by the glaucoma specialists. Of these 180 with CDR < 0.6, 3 cases (1.7%) were designated as glaucoma by expert graders. These were not included in statistical analysis, but were taken into consideration when interpreting results. At the Wilmer Eye Institute, the images were evaluated by using a tablet-based review system (TruthMarker; IDx, LLC, Iowa City, IA, USA) and graded to determine image quality, vertical CDR, notching of the neuroretinal rim, excavation of the optic cup, optic disc hemorrhage, tilting of the disc, and disc size. The three glaucoma specialists graded each image to determine likelihood of glaucoma (No, Possible, Probable, Definite, Unable), and the results were adjudicated where necessary (Gupta et al.17). A participant was designated as having glaucoma if the consensus expert grading in either eye was “Probable” or “Definite.” For this analysis, we assumed that participants with CDR < 0.6 in both eyes did not have glaucoma (this value is close to the optimal cutoff point for defining glaucomatous optic neuropathy in population-based glaucoma risk factor analysis).24 As a consequence, all glaucoma cases in the analysis were derived from participants who had at least one eye with CDR ≥ 0.6 on initial grading.
Statistical Analysis
We analyzed NHANES data to assess potential risk factors for prevalent glaucoma based on optic disc photos. Regression analysis was first performed with individual variables to identify factors that were significantly associated with glaucoma (P ≤ 0.05). These variables, together with basic demographic variables, were then included in a multivariable regression model to identify factors that remained independently associated with glaucoma. Stepwise logistic regression analysis was performed to identify factors that were independently associated with glaucoma. A P value ≤ 0.05 was used to define statistical significance for this study.
All data were analyzed using SAS (version 9.2; SAS Institute, Cary, NC, USA). Because of the multistage probability sampling design of the NHANES, weights computed by National Center for Health Statistics were used to obtain valid estimates of population prevalence and standard errors. In other words, NHANES oversamples small subgroups, such as ethnic minorities, then accounts for this through weighting to model the actual US census population. The weights are based on the probability of a person's being selected and are adjusted for likelihood of nonresponse.20 Appropriate weights were also applied to the fasting lab values included in the multivariable models.20 These results were confirmed using nonfasting weights, and there were no significant differences.
Results
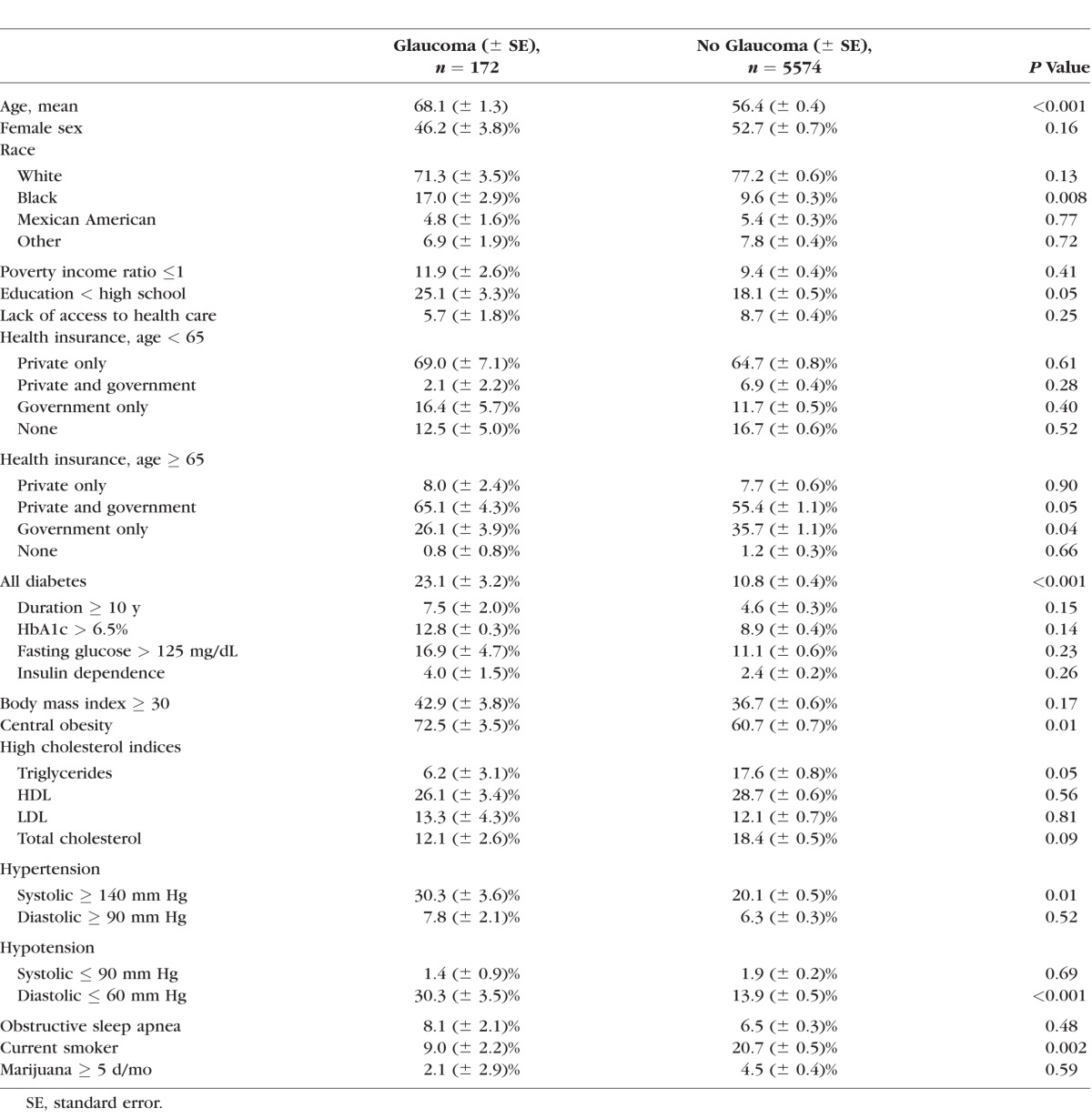
Among 6797 participants, 5764 had adequate-quality disc photos graded by the reading center. Of these, 1073 eyes from 548 participants with cup-to-disc ratio of 0.6 or larger were regraded by glaucoma experts, who identified 172 glaucoma cases. Participants with glaucoma were significantly older (mean age 68.1 vs. 56.4, P < 0.001) and more likely to be African American (17.0% vs. 9.6%, P = 0.008). They were also significantly more likely to have education less than high school (25.1% vs. 18.1%, P = 0.049), to have diabetes (23.1% vs. 10.8%, P < 0.001), to have central obesity (72.5% vs. 60.7%, P = 0.01), to have systolic hypertension ≥ 140 mm Hg (30.3% vs. 20.1%, P = 0.01), and to have diastolic hypotension ≤ 60 mm Hg (30.3% vs. 13.9%, P < 0.001). They were less likely to be current smokers (9.0% vs. 20.7%, P = 0.002) (Table 1). Among those 65 years and older, those with glaucoma were more likely to have a combination of private and government-sponsored insurance, and less likely to have government insurance only; there were no significant differences among other types of insurance, and there were no significant differences in insurance type among those younger than 65 years old. Sex, poverty, lack of access to health care, fasting glucose, insulin dependence, BMI ≥ 30, lipid levels, diastolic hypertension, systolic hypotension, obstructive sleep apnea, and marijuana use were not significantly associated with the prevalence of glaucoma.
Table 1.
Characteristics of Those With and Without Glaucoma Based on Expert-Graded Disc Photos
Single-variable analysis confirmed that older age was significantly associated with glaucoma (odds ratio [OR] 1.08, 95% confidence interval [CI] 1.06–1.10 per year). Regression analyses including demographic variables, controlled for age, showed that black race was significantly associated with glaucoma (OR 2.59, 95% CI 1.44–4.64). Regression analyses of variables related to general health were controlled for age, sex, and race and showed that diabetes (OR 1.77, 95% CI 1.03–3.04) and BMI ≥ 30 (OR 1.63, 95% CI 1.10–2.41) were significantly associated with glaucoma. Diabetes of 1 to 9 years duration (OR 2.42, 95% CI 1.23–4.75) was significantly associated with glaucoma, whereas diabetes of greater than or equal to 10 years duration was not significantly associated with glaucoma. Furthermore, triglyceride levels ≥ 200 mg/dL were inversely associated with the prevalence of glaucoma, and this was statistically significant. The associations with education less than high school, insurance status, central obesity, systolic hypertension, diastolic hypotension, and smoking status were not statistically significant when these variables were adjusted for age (Tables 2, 3, 4).
Table 2.
Single-Variable Regression of Age as a Risk Factor for Glaucoma
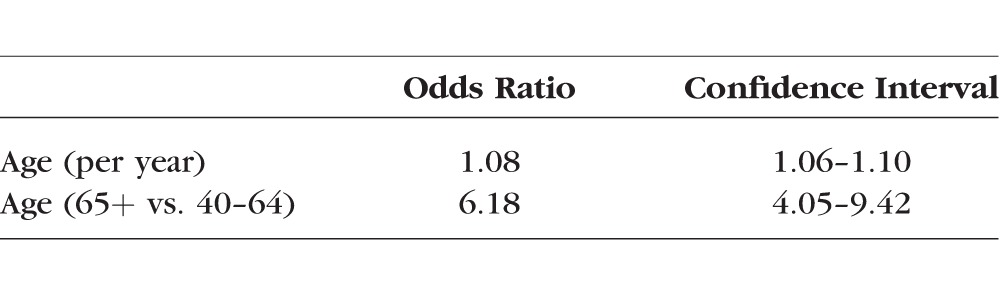
Table 3.
Univariable Logistic Regression of Demographic Risk Factors for Glaucoma, Controlling for Age
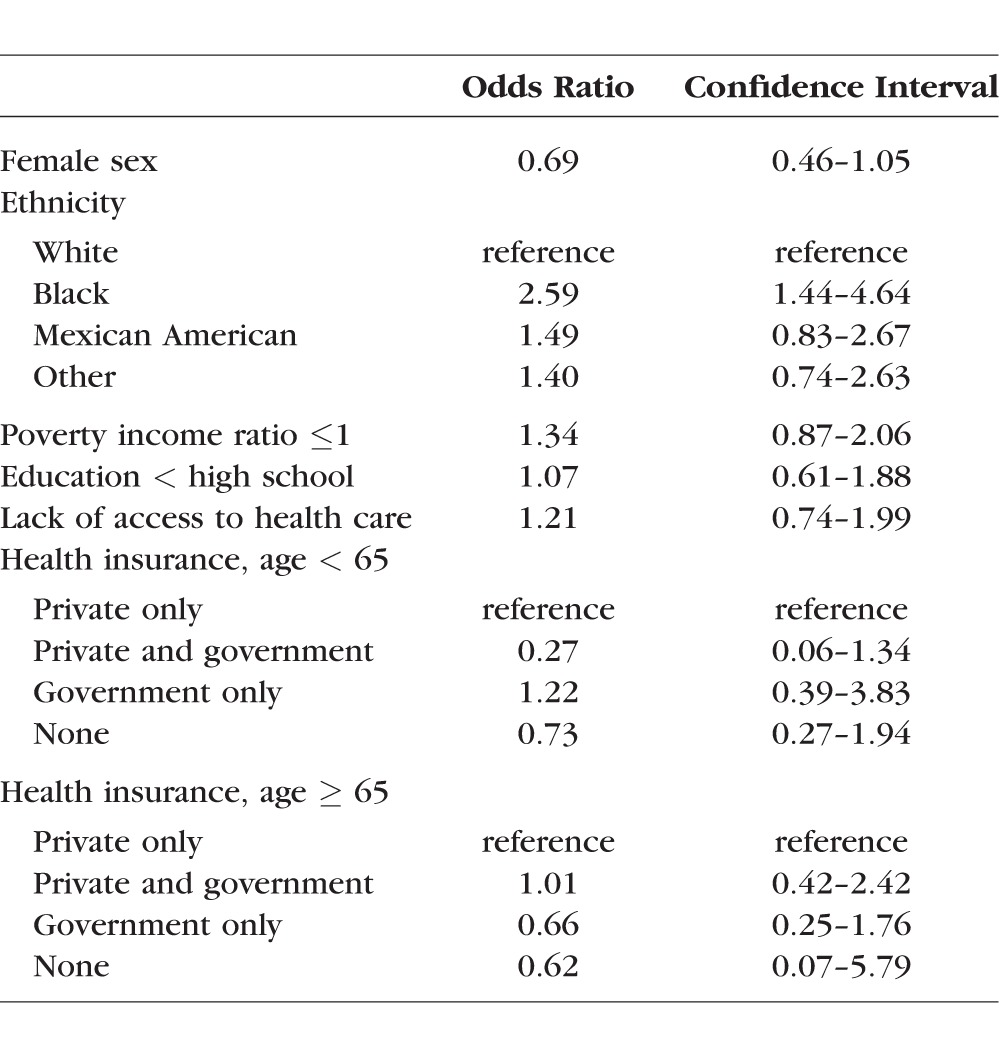
Table 4.
Multivariable Logistic Regression of Health-Related Risk Factors and Glaucoma, Controlling for Age, Sex, and Ethnicity
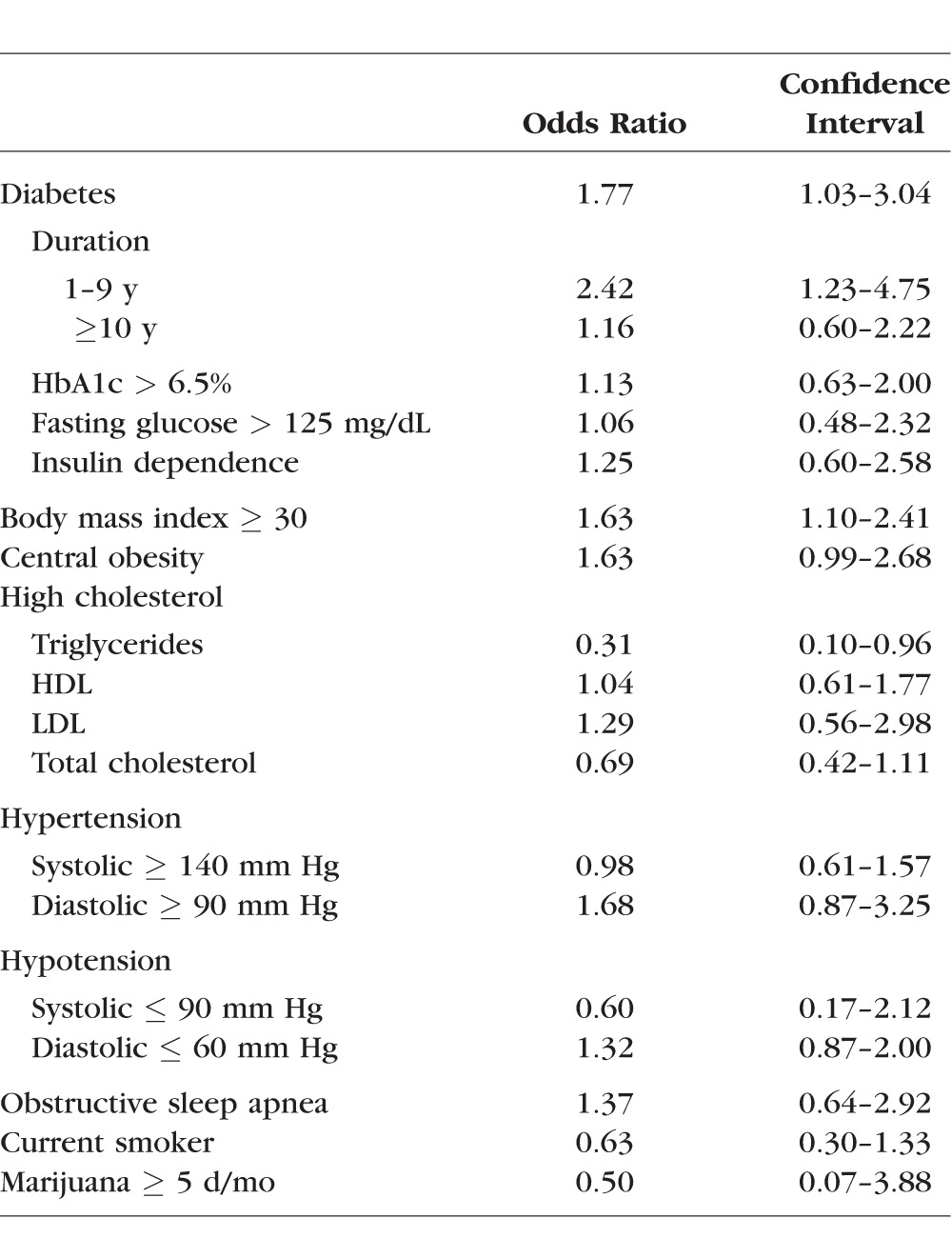
Multivariable regression modeling was performed with all risk factors described above. Age (OR 1.09, 95% CI 1.04–1.14) and black race (OR 4.40, 95% CI 1.71–11.3) remained significantly associated with glaucoma. In addition, poverty appeared as a risk factor (OR 3.39, 95% CI 1.73–6.66). Diabetes was not significantly associated with glaucoma once all confounders, including triglyceride levels, were included in the model. Of note, diabetes was significant only if triglyceride levels were excluded from the multivariable regression model, but diabetes was not significant if triglyceride levels were included in the model. Sex, education less than high school, insurance status, and BMI ≥ 30 were not statistically related to glaucoma prevalence in the multivariable model (Table 5).
Table 5.
Multivariable Logistic Regression of Risk Factors for Glaucoma
Discussion
Using optic nerve appearance on fundus photographs, we found that older age (OR 1.09 per year), black race (OR 4.89 compared to whites), and poverty (OR 3.14) were significantly associated with glaucoma. Interestingly, diabetes appeared to be significantly associated with glaucoma if considered alone, and even after controlling for demographic factors. However, if triglyceride levels were included in multivariable regression modeling, then the association with diabetes was no longer statistically significant.
Older age and black race, both of which are nonmodifiable, have been identified as strong risk factors in multiple studies,5 and our findings confirm these results. A recent meta-analysis found that diabetes, diabetes duration, and fasting glucose levels were all associated with increased risk of glaucoma.15 Potential mechanisms proposed for this increased risk include hyperglycemia leading to trabecular meshwork dysfunction, osmotic gradient changes related to autonomic dysregulation, or microvascular insult to the retina or optic nerve.25–28 Interestingly, single-variable analysis suggests that duration of diabetes is associated with different risk of glaucoma compared to those without diabetes. This may be due to survivor effect—that is, people who have diabetes for a longer duration may have had comorbidities that limited the quality of their fundus photos and prevented grading; furthermore, the effect disappears after triglycerides are added to the model. To our knowledge, no previous reports have noted an inverse association of triglyceride levels with the prevalence of glaucoma. This confounding role of triglyceride levels may explain the conflicting evidence for the association between diabetes and glaucoma.5,29,30 Alternatively, this effect may be related to use of systemic medications in people with metabolic disturbances. If systemic medications could alter glaucoma risk, this could have implications for glaucoma prevention and treatment. Further studies are needed to elucidate the role of lipid levels on glaucoma risk.
In the present study, glaucoma experts graded the optic disc photographs of NHANES participants to identify those with likely glaucoma. The majority of previously reported risk factors were not statistically related to glaucoma prevalence in this study. One possible explanation is that prior studies may have been affected by selective sampling or reporting that is less likely in the NHANES. Furthermore, risk factors previously thought to be independent may actually be markers of general poor health or older age. The lack of association may also be due to insufficient power in the current study, or to misclassification of those with and without glaucoma. One potential source of misclassification is the assumption of no glaucoma in the group with cup-to-disc ratios < 0.6. FDT was considered in making the diagnosis of glaucoma; however, work by others in our group has shown poor sensitivity and specificity.31 Furthermore, 25% of those studied did not successfully complete frequency-doubling technology (FDT); thus, FDT was not used to diagnose glaucoma in this study. Using self-report may also lead to misclassification of those with diabetes, although this is likely mitigated by inclusion of those with elevated fasting blood glucose or HbA1c. It is possible that certain variables, especially vascular risk factors, may be significant in only specific subtypes of glaucoma, such as so-called normal-tension glaucoma, which cannot be diagnosed without assessment of intraocular pressure and thus could not be separately analyzed in the current study.
Strengths of our study include its representative population-based sampling and standardized methodology. We studied a large database of optic disc photos graded by glaucoma experts to find associations with glaucoma. Our study is limited by its reliance on optic disc photos to identify people with glaucoma. Images were nonstereoscopic; however, they were high quality and multiple features of the optic nerve were considered, including not only vertical CDR, but also notching of the neuroretinal rim, excavation of the optic cup, optic disc hemorrhage, tilting of the disc, and disc size. Furthermore, three experts separately graded the images and resolved any discrepancies with adjudication. Given that characteristic optic disc changes are the defining feature of glaucomatous nerve damage, we believe that the majority of optic nerves with glaucoma were identified in the current study.
Our findings showed that people who are older, are of black race, and have lower income levels were at higher risk of glaucoma. We also identified a novel association between triglyceride levels and glaucoma that may help us understand inconsistent previous findings relating diabetes to increased glaucoma risk. This has implications for public health programs and may help to guide the direction of future research.
Acknowledgments
Research at the Wilmer Eye Institute is supported by National Institutes of Health Grant EY01766 and by a grant from Research to Prevent Blindness. The funding agencies had no role in the design or conduct of this research.
Disclosure: F. Ko, None; M.V. Boland, None; P. Gupta, None; S.K. Gadkaree, None; S. Vitale, None; E. Guallar, None; D. Zhao, None; D.S. Friedman, Allergan (C), Nidek (C), ForSight (C), Zeiss (C), Alcon (R)
References
- 1. Coleman AL,, Miglior S. Risk factors for glaucoma onset and progression. Surv Ophthalmol. 2008; 53 (suppl 1): S3–S10. [DOI] [PubMed] [Google Scholar]
- 2. Leske MC,, Heijl A,, Hyman L,, Bengtsson B,, Komaroff E. Factors for progression and glaucoma treatment: the Early Manifest Glaucoma Trial. Curr Opin Ophthalmol. 2004; 15: 102–106. [DOI] [PubMed] [Google Scholar]
- 3. Kass MA,, Heuer DK,, Higginbotham EJ,, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002; 120: 701–713, discussion 829–830. [DOI] [PubMed] [Google Scholar]
- 4. The effectiveness of intraocular pressure reduction in the treatment of normal-tension glaucoma. Collaborative Normal-Tension Glaucoma Study Group. Am J Ophthalmol. 1998; 126: 498–505. [DOI] [PubMed] [Google Scholar]
- 5. Boland MV,, Quigley HA. Risk factors and open-angle glaucoma: classification and application. J Glaucoma. 2007; 16: 406–418. [DOI] [PubMed] [Google Scholar]
- 6. Marcus MW,, de Vries MM, Junoy Montolio FG, Jansonius NM. Myopia as a risk factor for open-angle glaucoma: a systematic review and meta-analysis. Ophthalmology. 2011; 118: 1989–1994, e2. [DOI] [PubMed] [Google Scholar]
- 7. Xu L,, Wang H,, Wang Y,, Jonas JB. Intraocular pressure correlated with arterial blood pressure: the Beijing Eye Study. Am J Ophthalmol. 2007; 144: 461–462. [DOI] [PubMed] [Google Scholar]
- 8. Zhao D,, Cho J,, Kim MH,, Guallar E. The association of blood pressure and primary open-angle glaucoma: a meta-analysis. Am J Ophthalmol. 2014; 158: 615–627, e9. [DOI] [PubMed] [Google Scholar]
- 9. Charlson ME,, de Moraes CG,, Link A,, et al. Nocturnal systemic hypotension increases the risk of glaucoma progression. Ophthalmology. 2014; 121: 2004–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pasquale LR,, Kang JH,, Manson JE,, Willett WC,, Rosner BA,, Hankinson SE. Prospective study of type 2 diabetes mellitus and risk of primary open-angle glaucoma in women. Ophthalmology. 2006; 113: 1081–1086. [DOI] [PubMed] [Google Scholar]
- 11. Girkin CA,, McGwin G,, Jr,, McNeal SF,, Lee PP,, Owsley C. Hypothyroidism and the development of open-angle glaucoma in a male population. Ophthalmology. 2004; 111: 1649–1652. [DOI] [PubMed] [Google Scholar]
- 12. Wang D,, Huang Y,, Huang C,, et al. Association analysis of cigarette smoking with onset of primary open-angle glaucoma and glaucoma-related biometric parameters. BMC Ophthalmol. 2012; 12: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bonovas S,, Filioussi K,, Tsantes A,, Peponis V. Epidemiological association between cigarette smoking and primary open-angle glaucoma: a meta-analysis. Public Health. 2004; 118: 256–261. [DOI] [PubMed] [Google Scholar]
- 14. Lin CC,, Hu CC,, Ho JD,, Chiu HW,, Lin HC. Obstructive sleep apnea and increased risk of glaucoma: a population-based matched-cohort study. Ophthalmology. 2013; 120: 1559–1564. [DOI] [PubMed] [Google Scholar]
- 15. Zhao D,, Cho J,, Kim MH,, Friedman DS,, Guallar E. Diabetes fasting glucose, and the risk of glaucoma: a meta-analysis. Ophthalmology. 2015; 122: 72–78. [DOI] [PubMed] [Google Scholar]
- 16. Jampel H. American glaucoma society position statement: marijuana and the treatment of glaucoma. J Glaucoma. 2010; 19: 75–76. [DOI] [PubMed] [Google Scholar]
- 17. Gupta P,, Zhao D,, Gullar E,, Ko F,, Boland MV,, Friedman DS. Prevalence of glaucoma in the United States: the 2005-2008 National Health and Nutrition Examination Survey. Ophthalmol Vis Sci. In press. [DOI] [PMC free article] [PubMed]
- 18. Centers for Disease Control and Prevention. 2005-2006 National Health and Nutrition Examination Survey (NHANES): Survey Operations Manuals. http://www.cdc.gov/nchs/nhanes/nhanes2005-2006/manuals05_06.htm. Accessed December 31, 2014.
- 19. Centers for Disease Control and Prevention. 2007-2008 National Health and Nutrition Examination Survey (NHANES): Survey Operations Manuals. http://www.cdc.gov/nchs/nhanes/nhanes2007-2008/manuals07_08.htm. Accessed September 2, 2014.
- 20. Johnson CL,, Paulose-Ram R,, Ogden CL,, et al. National Health and Nutrition Examination Survey: Analytic Guidelines, 1999–2010. http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/nhanes_analytic_guidelines_dec_2005.pdf. Accessed September 2, 2014. [PubMed]
- 21. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: 2005-2006 Laboratory Manual List. http://wwwn.cdc.gov/nchs/nhanes/search/variablelist.aspx?Component=Laboratory&CycleBeginYear=2005. Accessed December 31, 2014.
- 22. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: 2007-2008 Laboratory Manual List. http://wwwn.cdc.gov/nchs/nhanes/search/variablelist.aspx?Component=Laboratory&CycleBeginYear=2007. Accessed December 31, 2014.
- 23. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey: Vision Procedures Manual. http://www.cdc.gov/nchs/data/nhanes/nhanes_05_06/VI.pdf. Accessed December 31, 2014.
- 24. Ramdas WD,, Rizopoulos D,, Wolfs RC,, et al. Defining glaucomatous optic neuropathy from a continuous measure of optic nerve damage - the optimal cut-off point for risk-factor analysis in population-based epidemiology. Ophthalmic Epidemiol. 2011; 18: 211–216. [DOI] [PubMed] [Google Scholar]
- 25. Oh SW,, Lee S,, Park C,, Kim DJ. Elevated intraocular pressure is associated with insulin resistance and metabolic syndrome. Diabetes Metab Res Rev. 2005; 21: 434–440. [DOI] [PubMed] [Google Scholar]
- 26. Sato T,, Roy S. Effect of high glucose on fibronectin expression and cell proliferation in trabecular meshwork cells. Invest Ophthalmol Vis Sci. 2002; 43: 170–175. [PubMed] [Google Scholar]
- 27. Chopra V,, Varma R,, Francis BA,, et al. Type 2 diabetes mellitus and the risk of open-angle glaucoma: the Los Angeles Latino Eye Study. Ophthalmology. 2008; 115: 227–232, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Feke GT,, Bex PJ,, Taylor CP,, et al. Effect of brimonidine on retinal vascular autoregulation and short-term visual function in normal tension glaucoma. Am J Ophthalmol. 2014; 158: 105–112, e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tielsch JM,, Katz J,, Quigley HA,, Javitt JC,, Sommer A. Diabetes intraocular pressure, and primary open-angle glaucoma in the Baltimore Eye Survey. Ophthalmology. 1995; 102: 48–53. [DOI] [PubMed] [Google Scholar]
- 30. Quigley HA. Can diabetes be good for glaucoma? Why can't we believe our own eyes (or data)? Arch Ophthalmol. 2009; 127: 227–229. [DOI] [PubMed] [Google Scholar]
- 31. Boland MV,, Gupta P,, Ko F,, Zhao D,, Guallar E,, Friedman DS. Evaluation of frequency-doubling technology perimetry as a means of screening for glaucoma and other eye diseases using the National Health and Nutrition Examination Survey. JAMA Ophthalmol. 2016; 134: 57–62. [DOI] [PubMed] [Google Scholar]


