Abstract
Objective
Platelets modulate hemostasis and immune responses via interactions with immune cells, through secretion of immune-modulators and cell-cell interactions. The P2Y12 receptor mediates ADP-induced aggregation and secretion in platelets.
Approach
using a mouse model of intra-abdominal sepsis and acute lung injury, we investigated the role of the P2Y12 receptor in neutrophil migration and lung inflammation in P2Y12 null mice and in mice pre-treated with the P2Y12 antagonist clopidogrel.
Results
our data show a decrease in circulating white blood cells and a decrease in platelet activation and platelet-leukocyte interactions in treated mice compared to untreated. Additionally, lung injury and platelet sequestration were diminished in clopidogrel-treated mice compared to their untreated septic littermates. Similar results were observed in P2Y12 null mice: platelet activation and platelet-leukocyte aggregates were decreased in septic P2Y12 null mice compared to wild-type. P2Y12 null mice were refractory to lung injury compared to wild-type. Lastly, to evaluate P2Y12 independent effects of clopidogrel, we pre-treated P2Y12 null mice. Interestingly, the number of circulating neutrophils was reduced in treated septic P2Y12 null mice, suggesting neutrophils as a target for clopidogrel pleiotropic effects. No difference was observed in P2Y1 null mice during sepsis, indicating that the P2Y12 receptor is responsible for the effects.
Conclusions
P2Y12 null mice are refractory to sepsis-induced lung injury, suggesting a key role for activated platelets and the P2Y12 receptor during sepsis.
Keywords: sepsis, platelets, P2Y12 receptor
Introduction
Platelets regulate thrombus formation and hemostasis and play important roles during inflammation. Upon activation, platelets activate immune cells through cell-cell interactions and by secreting inflammatory mediators and second mediators, such as ADP, that recruit other platelets 1. ADP-induced aggregation is mediated by two members of the P2Y receptor family: P2Y1 and P2Y12 2. Both are G protein-coupled receptors that are expressed on platelet membranes 3. P2Y1 is coupled to Gq protein, whose activation causes platelet shape changes and a weak, transient aggregation 4. P2Y12 is coupled to Gi protein, whose activation leads to platelet aggregation and potentiation of granule release, indicating a role for the P2Y12 receptor in platelet secretion 5. Signaling events downstream of the P2Y12 receptor also potentiate agonist-induced dense granule release, pro-coagulant activity, and thrombus formation 6.
Platelets activate leukocytes through cell-cell interactions involving adhesion molecules such as P-selectin, a glycoprotein that, upon cell activation, is rapidly translocated from cytoplasmic α-granules to the cell surface 7. P2Y12 activation is required for α-granule release and subsequent expression of P-selectin on activated platelets 7. P-selectin binds P-selectin glycoprotein ligand 1 (PSGL-1) on leukocytes, which activates leukocytes and promotes their infiltration into inflamed tissue 8.
Platelet-leukocyte interactions are important in the pathogenesis of sepsis 9, and leukocyte-platelet aggregates and P-selectin secretion are altered in septic patients 10. In a model of sepsis induced by cecal ligation and puncture (CLP), neutrophil infiltration in the lungs was reduced following platelet depletion 11, suggesting that platelets play a role in neutrophil activation during inflammation. Similar observations were made in other inflammation models, such as pancreatitis and ischemia reperfusion 12, 13. In a rat model of LPS-induced inflammation, induction of pro-inflammatory cytokines (IL-6 and TNF-α), lung damage, and liver damage were attenuated upon treatment with clopidogrel, a drug that antagonizes the P2Y12 receptor 14. Both P2Y12 receptor antagonism and platelet depletion reduced inflammation during sepsis, suggesting a role for platelets in regulating the inflammatory response in sepsis.
P2Y12 receptor gene variants correlate with pulmonary inflammation and asthma 15. Also, P2Y12 receptor deficiency and platelet depletion abrogate dust mite-induced airway inflammation 16, suggesting a role for the P2Y12 receptor in pulmonary inflammation. The mechanisms that trigger neutrophil infiltration are poorly understood but may result from the development of a pro-inflammatory phenotype in the lung. These observations suggest a regulatory role for the P2Y12 receptor and activated platelets in regulating neutrophil influx into the lung.
In support of this hypothesis, studies by Rahman et al demonstrated a lung protective effect in septic animals treated with the P2Y12 antagonist, ticagrelor suggesting a regulatory role for P2Y12 receptor signaling in sepsis 17. However, several studies indicate that ticagrelor may have pleiotropic effects in addition to its anti-platelet properties 18. To establish a role for P2Y12 signaling in sepsis and sepsis-induced acute lung injury, we examined the effects of receptor deficiency (P2Y12 null mice) and P2Y12 antagonism (clopidogrel) in the CLP model of sepsis. We further pre-treated P2Y12 null mice with clopidogrel to investigate P2Y12 independent effects. Lastly, we studied P2Y1 null mice in the same sepsis model to determine whether these effects were due to P2Y12 deficiency or to altered responses to ADP. Our findings show that inflammation was decreased in P2Y12 null mice but not in P2Y1 null mice. Interestingly, P2Y12 deficiency and receptor antagonism in this model of sepsis provided similar results, suggesting that modulation of the P2Y12 receptor offers a new therapeutic option for sepsis.
Materials and methods
Materials and Methods are available in the online-only Data Supplement.
Results
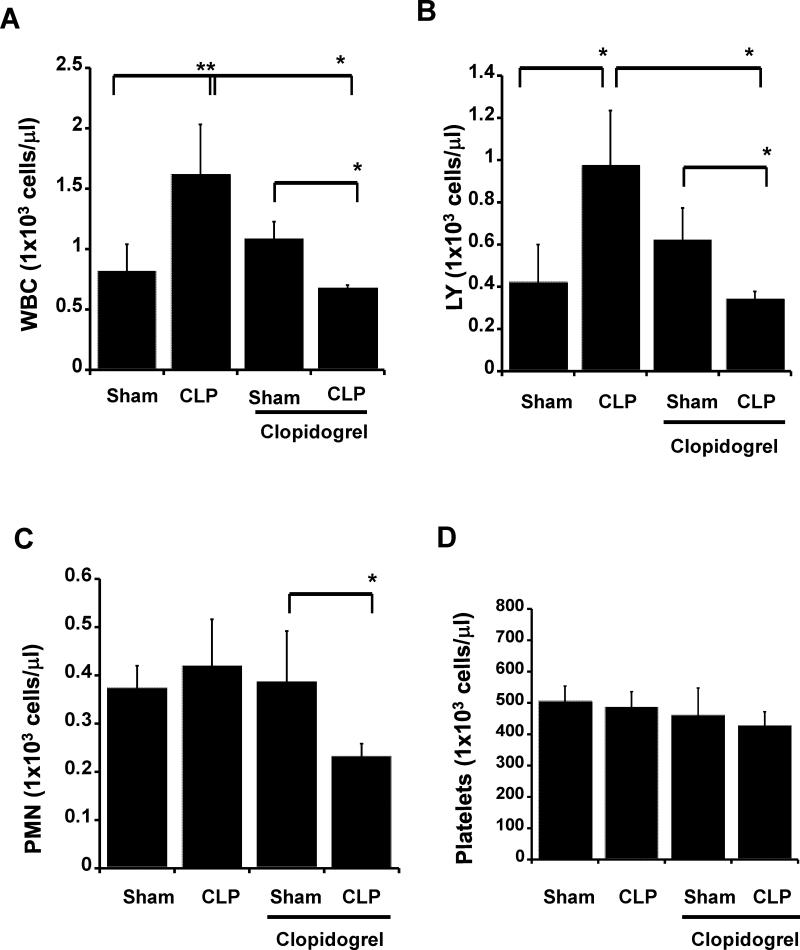
Circulating white blood cells (WBCs) did not increase following clopidogrel treatments in septic mice
To study P2Y12 receptor antagonism in sepsis, mice were treated with the P2Y12 receptor antagonist clopidogrel (loading dose: 30 mg/kg; maintenance dose: 10 mg/kg) prior to surgery in a model of sepsis and lung injury. Both sham and CLP mice were treated. First, we analyzed the number of circulating WBCs in blood samples (Fig. 1) from treated and untreated mice. In septic mice, the WBC count was significantly increased compared with the sham control, but WBCs were not elevated in clopidogrel-treated CLP mice (Fig. 1A; **p < 0.01; sham versus CLP, *p < 0.05 clopidogrel-treated CLP versus untreated CLP). Interestingly, the WBC count in the treated CLP animals was lower than in the sham control (*p < 0.05). When we analyzed the cells more specifically, we noticed that lymphocytes were increased following sepsis, whereas no difference was noted in neutrophils. However, following clopidogrel treatment, both cells were significantly reduced (Fig. 1B and C; *p < 0.05; clopidogrel-treated CLP versus clopidogrel untreated CLP and treated sham versus treated CLP). No difference was reported in the platelet count among all groups (Figure 1D).
Figure 1. Circulating white blood cells did not increase in sepsis following clopidogrel treatments.
Blood samples were collected by cardiac puncture in 3.8% sodium citrate (10:1) and hematology studies were performed. Graphs show counts of (A) white blood cells (WBC), (B) lymphocytes (LY), (C) neutrophils (PMN), and (D) platelets in clopidogrel-treated or untreated mice. Both sham and CLP samples were analyzed for treated and untreated mice. Values are expressed as 1×103 cells/μL, mean ± S.E.M., (n = 8; *p<0.05 WT sham versus CLP mice; **p<0.01 treated CLP versus untreated CLP).
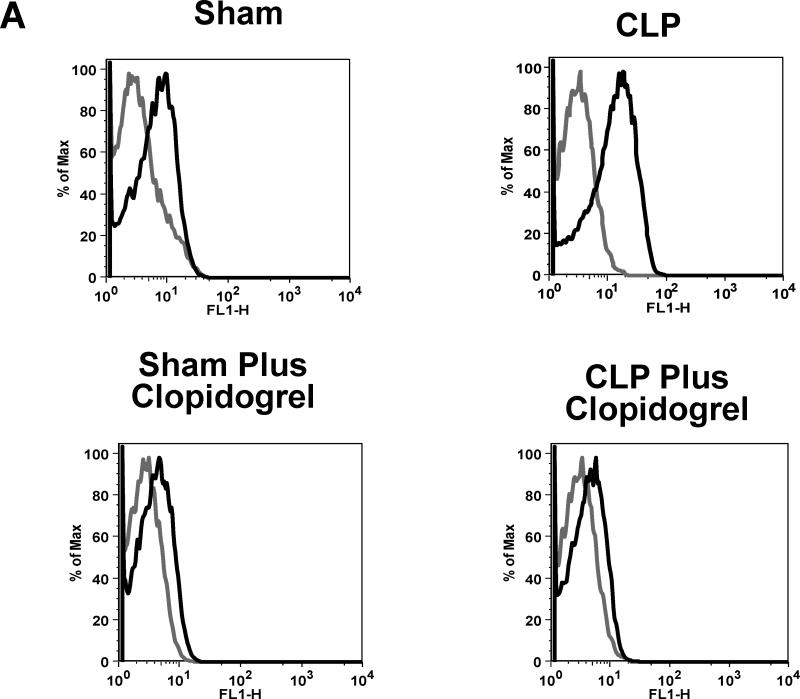
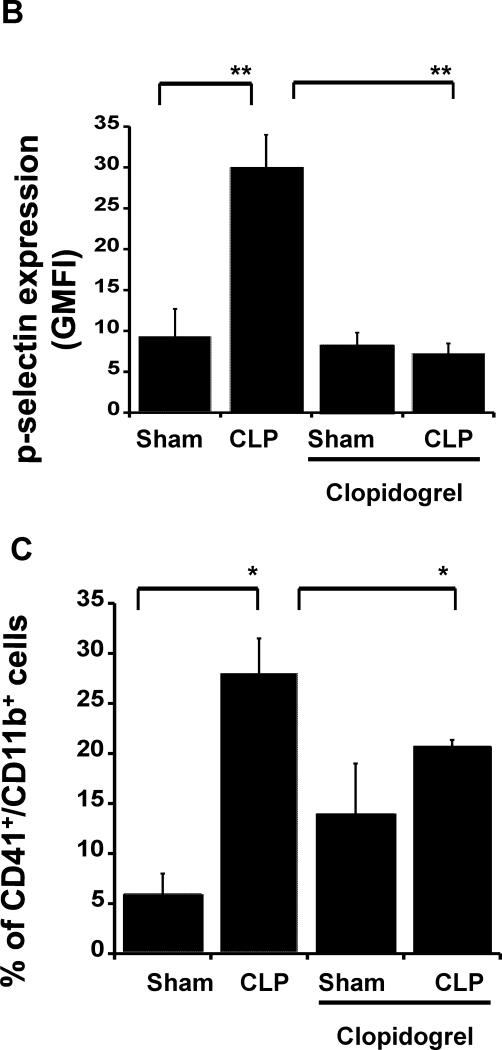
Clopidogrel treatment prevents septic-induced P-selectin increase and platelet-leukocyte aggregate formation
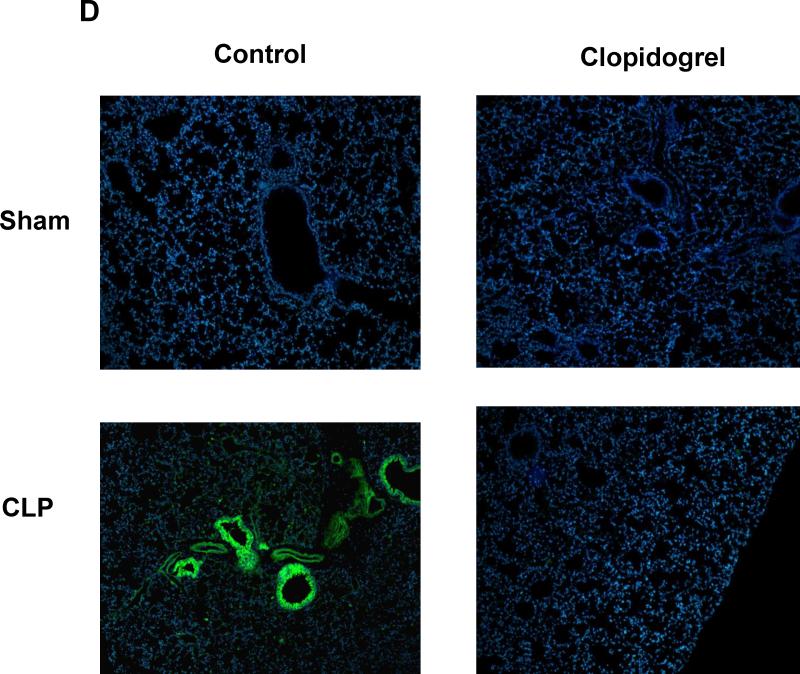
To determine whether clopidogrel exposure alters platelet activation during sepsis, we investigated P-selectin expression on platelet membranes following CLP in treated and untreated mice using flow cytometry (Fig. 2 A and B). P-selectin expression was increased after CLP (Fig. 2A and B; **p < 0.01; CLP versus sham), but no elevation was noted in mice pretreated with clopidogrel compared to the treated sham control (Fig 2A and B **p < 0.01; untreated CLP versus treated CLP). Next we investigated the effect of clopidogrel treatment on leukocyte-platelet aggregate formation (Fig. 2C and D). Aggregate formation was elevated in samples from CLP mice compared to sham mice (Fig. 2C and D; *p < 0.05 CLP versus sham). However, in clopidogrel-treated mice, aggregate formation was significantly reduced compared to untreated mice (Fig. 2C; *p < 0.05 CLP versus treated CLP). Then we investigated platelet sequestration in the lungs of septic mice. Lung samples were stained with the platelet marker CD41. Representative images are shown in Figure 2D, indicating that an increase in CD41 was observed in wild-type mice after CLP surgery (Fig. 2D, left panels, n = 4), but it was not noted in clopidogrel-treated mice (Fig. 2D, right panels).
Figure 2. P-selectin expression and leukocyte-platelet aggregates were not elevated in clopidogrel treated mice during sepsis.
(A) and (B) Blood samples were collected by cardiac puncture in 3.8% sodium citrate (10:1), and P-selectin expression on platelet surface was analyzed through flow cytometry. Representative flow cytometry histograms are shown for CLP and sham controls in WT and KO animals. Isotype control is shown in gray and P-selectin stained samples in black. (C) Blood samples were labelled with antibodies against CD61 (platelet marker) and CD11b (leukocyte marker). Activated leukocytes were gated based on CD11b expression and cell shape, and data were analyzed as a percentage of aggregates expressing both CD41 and CD11b. Values are expressed as percentage of CD41+/CD11b+ cells, mean ± SEM (*p < 0.05; WT sham versus WT CLP and KO CLP versus WT, n = 6). (D) Representative images of CD41 staining (CD41: green; Nucleus: blue; 20x) for CLP and sham samples for both treated and untreated mice. Images are representative of 4 different experiments.
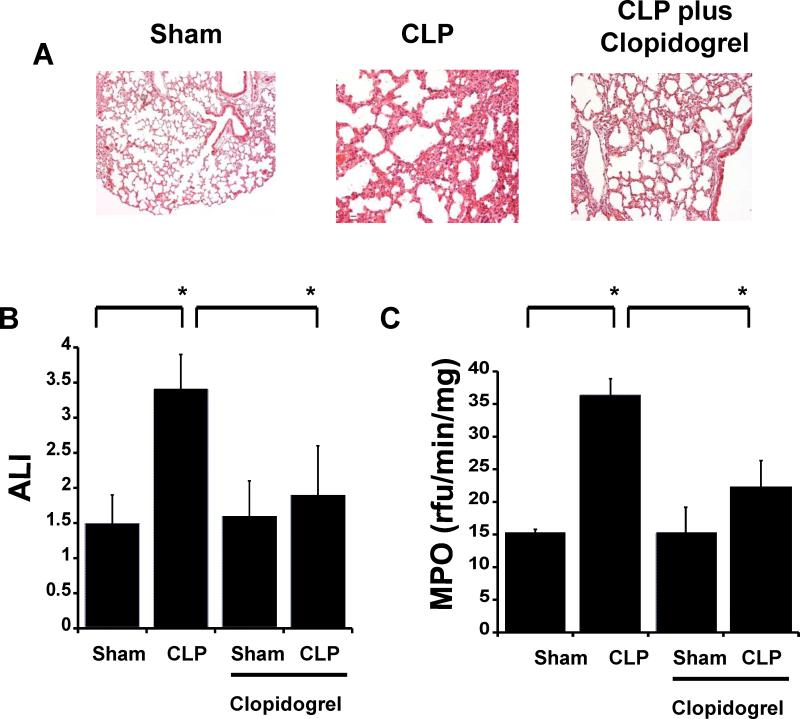
Clopidogrel treated mice are refractory to sepsis-induced lung injury
We analyzed whether clopidogrel treatment alters sepsis-induced acute lung injury. Following CLP, mouse lung architecture was disrupted, signs of edema were apparent, and increased cell infiltration was notable (Fig. 3A). However, inflammation levels were diminished in clopidogrel-treated mice compared to untreated CLP mice (Fig. 3A *p < 0.05; CLP versus treated CLP). Similarly, histology scores (Fig. 3B) were not increased in the CLP group pre-treated with clopidogrel compared to the treated sham (Fig. 3B). These data suggest a protective role for clopidogrel during lung inflammation. To determine neutrophil infiltration in the lungs, we investigated MPO activity. We observed a significant increase in MPO levels in septic mice compared to the sham group (Fig. 3C *p < 0.05; CLP versus sham), whereas MPO decreased in septic mice pre-treated with clopidogrel compared to untreated CLP mice (Fig 3C; *p < 0.05; CLP versus treated CLP).
Figure 3. Sepsis-induced lung injury is ameliorated in clopidogrel-treated mice.
(A) Photomicrographs of hematoxylin- and eosin-stained tissue sections were obtained after CLP surgery. Representative images of lung tissue specimens are shown for sham and CLP in clopidogrel-treated and untreated mice (Magnification 20 and 40x; n = 5). (B) Acute lung injury (ALI) scores were assessed in treated and untreated animals. (C) MPO analysis was performed in lung samples of sham and CLP mice. Values are expressed as rfu/min/mg, mean ± SEM (*p < 0.05; CLP versus sham, n = 7).
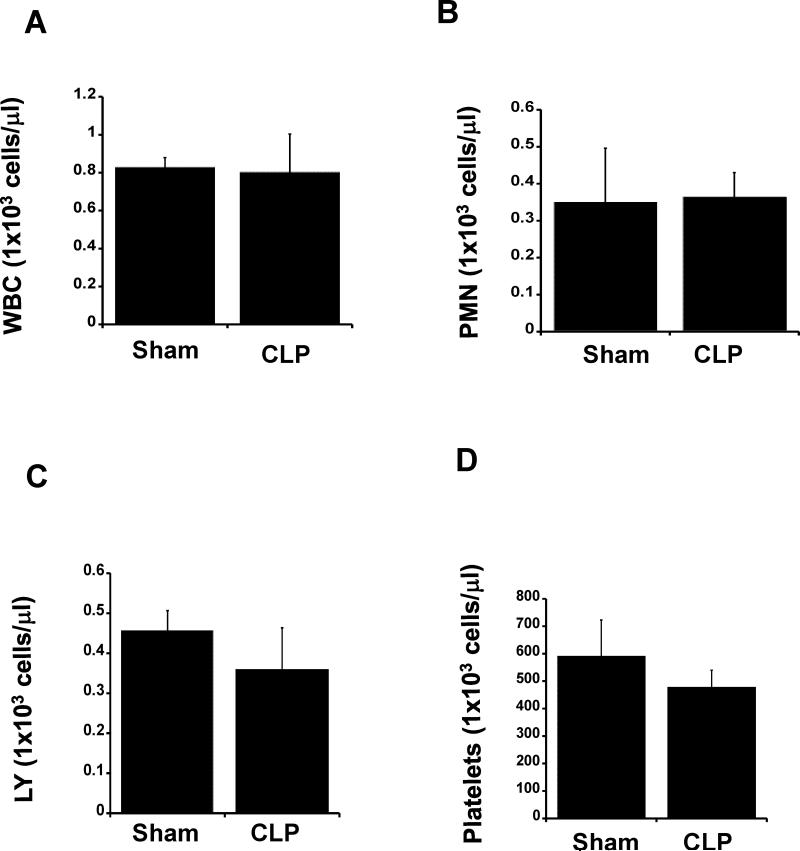
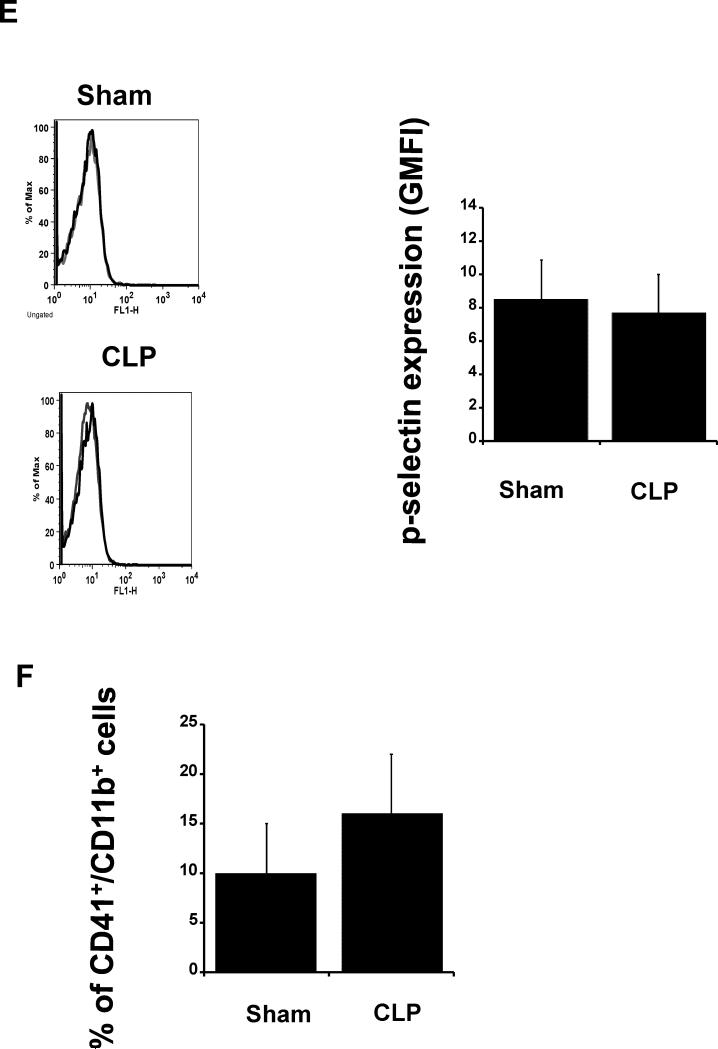
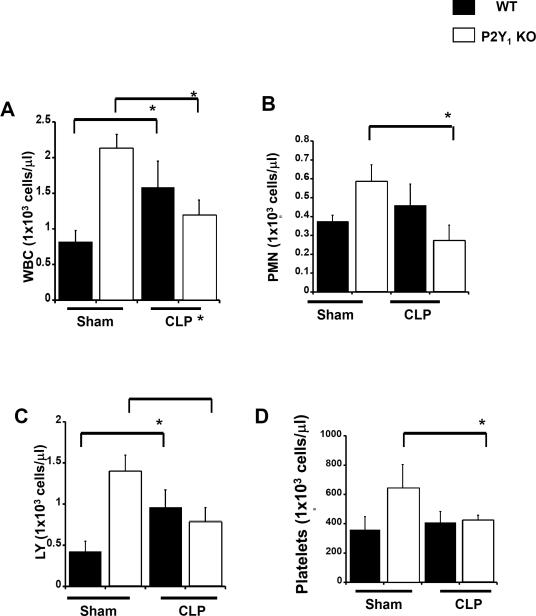
Sepsis-induced increase in circulating white blood cells was not noted in P2Y12 null mice
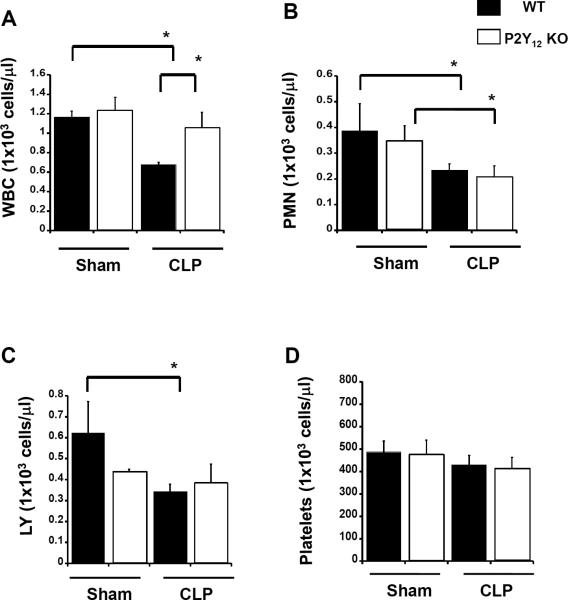
To compare receptor antagonism with receptor deficiency, we analyzed P2Y12 null mice in the same model of sepsis-induced inflammation. First we investigated the number of WBCs in blood samples of P2Y12 null mice 24 hours after either CLP or sham surgery (Fig. 4). No increase in circulating WBCs in septic mice was noted compared to the sham control (Fig. 4A). Specifically, no differences in neutrophils (Fig.4B) and lymphocytes (Fig. 4C) were observed in null mice in either the CLP or sham groups. Interestingly, platelet count was similar in all groups (Figure 1D).
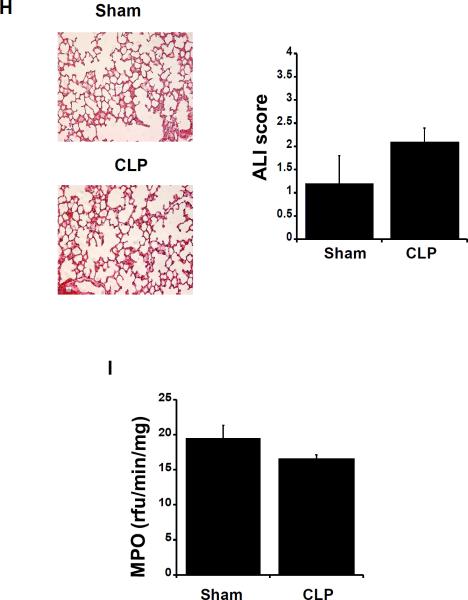
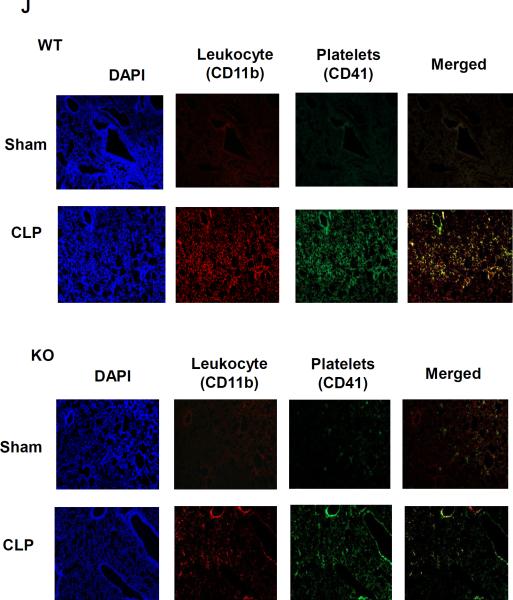
Figure 4. Circulating white blood cells counts, platelet activation, and platelet-leukocyte aggregate formation are not increased in P2Y12 null mice.
Blood samples were collected by cardiac puncture in 3.8% sodium citrate (10:1), and hematology studies performed. Graphs show counts of (A) white blood cells (WBC), (B) neutrophils (PMN), (C) lymphocytes (LY), and (D) platelets in WT P2Y12 KO mice. Both sham and CLP samples were analyzed. Values are expressed as 1×103 cells/μL, mean ± S.E.M., (n = 8; **p<0.01 WT CLP versus KO CLP mice). (E) Blood samples were collected by cardiac puncture in 3.8% sodium citrate (10:1), and p-selectin expression on platelet surface was analyzed through flow cytometry. Representative flow cytometry histograms are shown for CLP and sham control mice. Isotype control is shown in gray and P-selectin stained samples in black. (F) The percentage of aggregates is reported for all groups. Blood samples were labelled with antibodies against CD61 (platelet marker) and CD11b (leukocyte marker). Activated leukocytes were gated based on CD11b expression, and cell shape and data were analyzed as a percentage of aggregates expressing both CD41 and CD11b. Values are expressed as percentage of CD41+/CD11b+ cells, mean ± SEM (*p < 0.05; WT sham versus WT CLP and KO CLP versus WT, n = 6). (G) Plasma samples obtained from each animal were utilized for detection levels of TNF-α, Il-10, IL-6 and MIP-1b in WT (black) and KO (white) mice. Both Sham and CLP samples were analyzed for wild type and KO animals. Values are expressed as pg/ml, mean ± S.E.M. (*p < 0.05; **p < 0.01; KO CLP model versus WT CLP, n=5). (H) Photomicrographs of hematoxylin- and eosin-stained tissue sections obtained after CLP surgery. Representative images of lung tissue specimens are shown for sham and CLP samples (Magnification 20 and 40x; n = 5). Acute lung injury (ALI) score, was assessed in KO mice. (I) MPO analysis was performed in lung samples of sham and CLP mice. Values are expressed as rfu/min/mg, mean ± SEM (n = 5). (J) Representative images of CD41 and CD11b staining (CD41: green; CD11b: red; Nucleus: blue; 20x) for CLP and sham samples for both WT and KO mice. Images are representative of 3 different experiments.
Platelet activation and platelet-leukocyte interaction is not elevated in P2Y12 null mice
We investigated whether P2Y12 deficiency influences platelet activation during sepsis-induced inflammation. P-selectin expression was not increased after CLP in both CLP and sham mice (Fig. 4E). Leukocyte-platelet aggregate formation was not elevated in samples from CLP P2Y12 null mice compared to sham P2Y12 null mice (Fig. 4F).
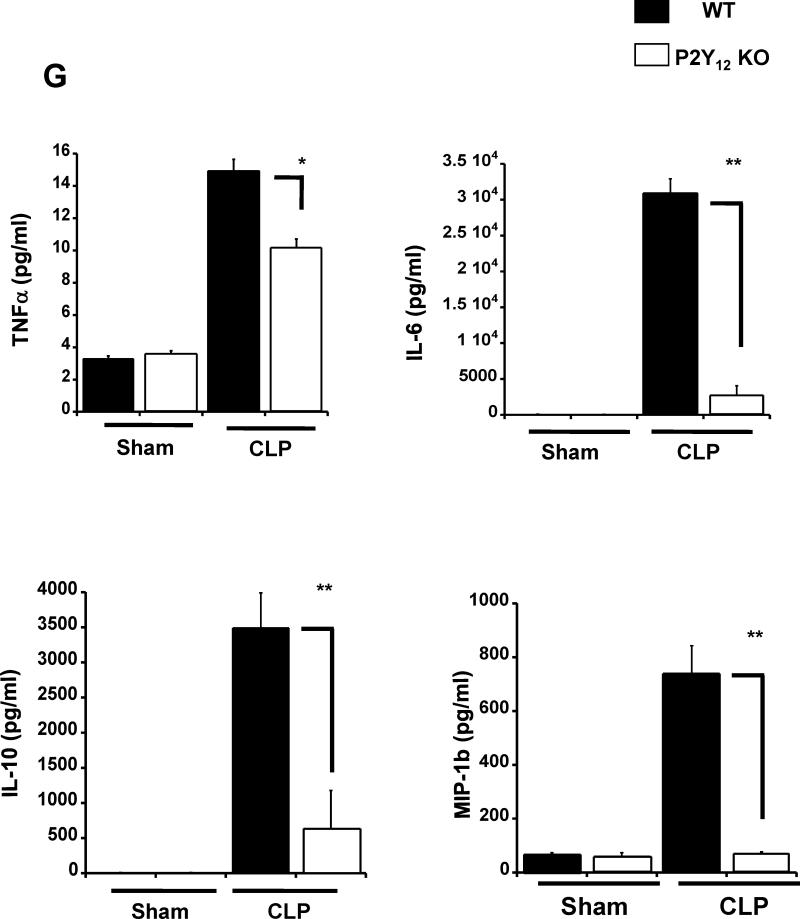
Sepsis-induced increases in plasma cytokines are diminished in P2Y12 KO mice
Next we investigated the role of P2Y12 in regulating sepsis-induced elevations in plasma levels of cytokines (TNF-α, IL-10, IL-6 and MIP-1β) (Fig. 4G). As expected, the plasma concentration of each cytokine was elevated during sepsis in both WT and P2Y12 null mice animals as compared to sham control. However, the sepsis-induced increase was significantly lower in P2Y12 null mice as compared to WT mice, for all the cytokines analyzed (**p < 0.01 KO CLP model versus WT CLP). These data suggest a decreased level of inflammation in the absence of P2Y12 receptor-mediated signaling.
Lung injury is decreased in septic P2Y12 null mice
In P2Y12 null mice 24 hours following CLP, no lung damage was observed as compared to the sham control (Figure 4H). Similarly, histology scores of ALI were not elevated. Furthermore, neutrophil infiltration (MPO levels) was not increased in P2Y12 null mice following CLP (Fig. 4I). These data suggest that the P2Y12 receptor plays a key role in pulmonary inflammation and inflammatory cell recruitment. To analyze how P2Y12 receptor influences platelets/leukocytes interaction in the lung, we stained lung tissue for CD41 (platelet marker) and CD11b (leukocyte marker) (Figure 4J). As expected, in WT animals Sham mice, the lungs did not show cell infiltration, while in septic WT mice both platelets and leukocytes infiltration were observed (Figure 4J, top panels). Co-localization was observed suggesting leukocyte-platelet aggregation in the lungs as well as in the periphery during sepsis. In contrast, P2Y12 null animals had decreased levels of platelets and neutrophils interaction in the lungs, suggesting a decrease in aggregation (Figure 4J, bottom panels).
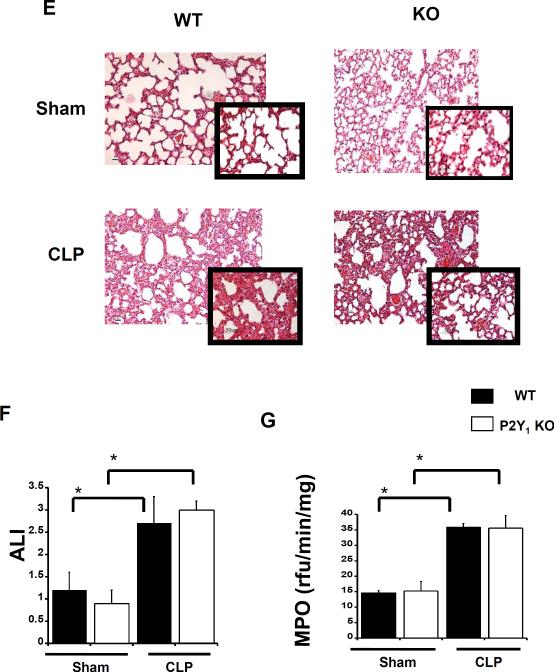
Clopidogrel pre-treatment decreased circulating neutrophils in P2Y12 null mice during sepsis
To determine whether clopidogrel has P2Y12 independent effects, we treated P2Y12 null mice with clopidogrel prior to surgery in the same model of sepsis (Fig. 5). Both sham and CLP mice were treated orally with clopidogrel (loading dose: 30 mg/kg; maintenance dose: 10 mg/kg). The decrease in WBC observed in treated WT CLP mice compared with treated Sham was not noted in treated P2Y12 null mice compared to treated sham P2Y12 null mice (Fig. 5A *p < 0.05;treated WT CLP versus treated WT Sham and treated CLP WT versus treated CLP P2Y12 null mice). On the contrary, neutrophils were significantly lower in septic treated mice compared to the treated sham control for both WT and P2Y12 null mice (Fig 5B, p < 0.05; treated WT sham versus treated WT CLP and treated P2Y12 null mice Sham versus treated CLP P2Y12 null mice). Lymphocyte count was not altered in treated P2Y12 null mice compared with their respectively treated Sham control (Fig. 5C). The data show that clopidogrel has P2Y12 independent effects during sepsis and suggest that circulating neutrophils may be the target cells.
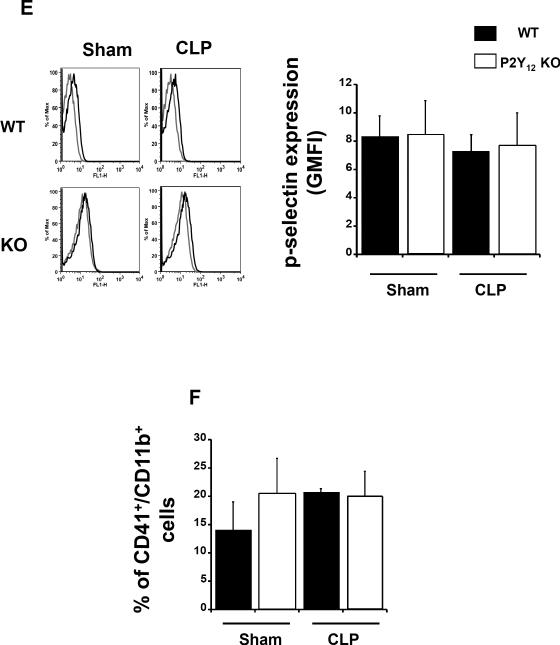
Figure 5. Clopidogrel treatment alter circulating neutrophil in septic P2Y12 null mice.
Blood samples were collected by cardiac puncture in 3.8% sodium citrate (10:1), and hematology studies performed. Graphs show counts of (A) white blood cells (WBC), (B) neutrophils (PMN), (C) lymphocytes (LY), and (D) platelets in clopidogrel-treated WT (black) and P2Y12 null mice (white). Both sham and CLP samples were analyzed. Values are expressed as 1×103 cells/μL, mean ± S.E.M., (n = 8; *p<0.05 WT CLP versus KO CLP mice and *p<0.05 treated-CLP WT versus treated-CLP P2Y12 null mice). (E) Blood samples were collected by cardiac puncture in 3.8% sodium citrate (10:1), and p-selectin expression on platelet surface was analyzed through flow cytometry. Representative flow cytometry histograms are shown for CLP and sham control mice in WT (black) and P2Y12 null (white) mice. Isotype control is shown in gray and P-selectin stained samples in black. (F) The percentage of aggregates is reported for CLP and sham control mice in WT (black) and P2Y12 null (white) mice. Blood samples were labelled with antibodies against CD61 (platelet marker) and CD11b (leukocyte marker). Activated leukocytes were gated based on CD11b expression, and cell shape and data were analyzed as a percentage of aggregates expressing both CD41 and CD11b. Values are expressed as percentage of CD41+/CD11b+ cells, mean ± SEM (n = 6). (G) Photomicrographs of hematoxylin- and eosin-stained tissue sections obtained after CLP surgery. Representative images of lung tissue specimens are shown for sham and CLP samples (Magnification 20, n = 5) in CLP and sham control mice in WT (black) and P2Y12 null (white) mice. (H) Acute lung injury (ALI) score, was assessed in Sham and CLP clopidogrel-treated WT (black) and P2Y12 null (white) mice. (I) MPO analysis was performed in lung samples of sham and CLP mice for Sham and CLP clopidogrel-treated WT (black) and P2Y12 null (white) mice. Values are expressed as rfu/min/mg, mean ± SEM (n = 5).
Clopidogrel treatment did not alter platelet activation and platelet-leukocyte aggregate formation in in P2Y12 null mice during sepsis
We investigated whether clopidogrel treatment can influence platelet activation in P2Y12 null mice during sepsis. Both sham and CLP groups were treated with clopidogrel. Data were compared with clopidogrel-treated WT sham and CLP. P-selectin expression was not increased after CLP in both treated CLP and sham mice for WT and P2Y12 null mice (Fig. 5E). Leukocyte-platelet aggregate formation was not elevated in samples from treated CLP P2Y12 null mice compared to treated sham P2Y12 null mice (Fig. 5F). The data are similar to what observed in clopidogrel-treated sham and CLP WT. Then we investigated platelet sequestration in the lungs of septic mice. No CD41 staining was observed in treated P2Y12 null mice after CLP surgery as well as in the treated sham control (data not shown). The data suggest that P2Y12 independent effects of clopidogrel do not involve platelets.
Clopidogrel treated P2Y12 null mice are still refractory to acute lung injury
We investigated acute lung injury in P2Y12 null mice during sepsis following clopidogrel treatments. In treated P2Y12 null mice 24 hours following CLP, no lung damage was observed as compared to the sham control (Fig. 5G). Similarly, histology scores of ALI were not elevated in the treated P2Y12 null CLP group compared to the treated P2Y12 null sham group (Fig. 5H). These data are similar to what observed in clopidogrel-treated sham and CLP WT. To confirm leukocyte infiltration, we investigated MPO activity in lung tissue samples (Fig. 5I). MPO levels was not increased in treated P2Y12 null mice following CLP. These data suggest that clopidogrel has no P2Y12 independent effects on lung tissue.
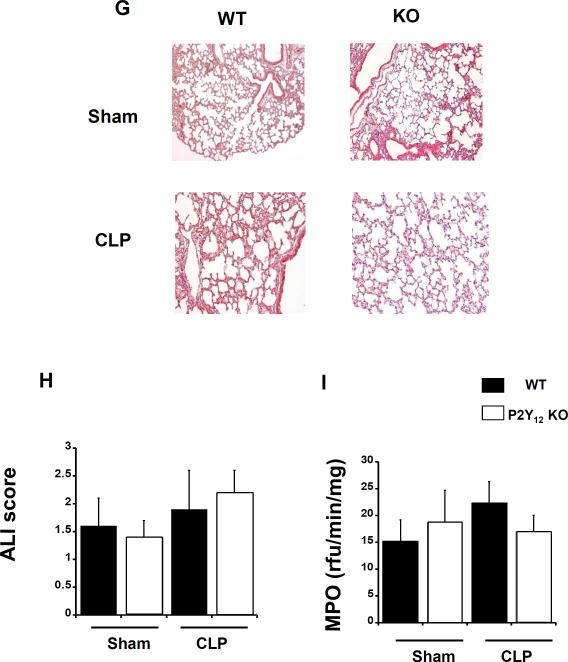
P2Y1 deficiency does not influence sepsis-induced inflammation levels
The same model of sepsis was investigated in P2Y1 null mice to investigate whether the data collected in P2Y12 null mice were due to changes in cell responses to ADP or specifically to P2Y12. First we analyzed circulating WBCs in blood samples (Figure 6). No significant difference in WBC number was observed in P2Y1 null mice compared to wild type (Fig. 6A), with similar results for neutrophils (Fig. 6B) and lymphocytes (Fig. 6C). Platelet counts were similar among groups (Fig. 6D). Interestingly, the cell count in the sham group was significantly higher than the CLP and wild-type sham groups (Figure 6; p < 0.05; KO sham versus KO CLP).
Figure 6. Inflammation-induced elevation in circulating white blood cell, platelet counts, and lung injury are not altered in P2Y1 null mice.
Blood samples were collected by cardiac puncture in 3.8% sodium citrate (10:1), and hematology studies were performed. Graphs show counts of (A) white blood cells (WBC), (B) neutrophils (PMN), (C) lymphocytes (LY), and (D) platelets in WT (black) and P2Y12 KO (white) mice. Both sham and CLP samples were analyzed for wild-type and KO mice. Values are expressed as 1×103 cells/μL, mean ± S.E.M. (E) Photomicrographs of hematoxylin- and eosin-stained tissue sections obtained after CLP surgery. Representative images of lung tissue specimens were obtained for sham and CLP in wild-type and KO mice (Magnification 20 and 40x; n = 5). (G) Acute lung injury (ALI) score, based on alveolar capillary congestion, hemorrhage, infiltration, or aggregation of neutrophils in the airspace or the vessel wall and thickness of the alveolar wall, was assessed in wild-type (black bars) and KO (white bars). (F) MPO analysis was performed in lung samples of sham and CLP in wild-type (black) and KO (white) mice. Values are expressed as rfu/min/mg, mean ± SEM (*p < 0.05; KO CLP model versus WT, n = 5).
We investigated lung injury in P2Y1 null mice and wild-type mice following CLP. No significant differences in lung injury were observed (Fig. 6E and F). In both groups there was significant inflammatory cell infiltration, edema, and disruption of tissue architecture. No differences in MPO activity were observed (Figure 6F). The data suggest that the P2Y1 receptor does not contribute to sepsis-induced lung injury in this animal model.
Discussion
Platelets play a role in hemostasis and are increasingly recognized for their ability to modulate immune responses1. The P2Y12 receptor plays a central role in various platelet functions, including secretion. P2Y12 receptor antagonists prevent platelet aggregation and secretion 19, 20 and alter the inflammatory state in LPS-induced inflammation, myocardial infarction, and rheumatoid arthritis 13, 21, 22, suggesting that P2Y12 modulation can influence inflammation by mechanisms which have yet to be fully elucidated. Pretreatment with the P2Y12 antagonist ticagrelor was shown to be lung protective and decrease circulating levels of leukocyte-leukocyte aggregates during sepsis17. The results presented here provide essential new information about the role of P2Y12 signaling in sepsis. We investigated for the first time this model of sepsis in P2Y12 null mice and WT mice treated with another P2Y12 antagonist, clopidogrel. Interestingly, clopidogrel has shown to exhibit pleiotropic effects 23 as well as ticagrelor that can inhibit equilibrative nucleoside transporter 1 18 Hence it is important to study sepsis in the P2Y12 null mouse model to compare receptor deficiency and antagonism and clarify the mechanism of these anti-platelet drugs. Further, we examined the effect of clopidogrel treatment on P2Y12 mice to identify P2Y12 independent effects. Our studies demonstrate that clopidogrel-treated mice are more refractory to inflammation and lung injury compared with untreated animals, which is similar to what we observed in P2Y12 null mice, suggesting that the P2Y12 receptor plays a central role during sepsis. Our studies demonstrate that P2Y12 deficiency and receptor antagonism in this model of sepsis provided similar results, suggesting that the P2Y12 signaling has an important role in the inflammation and tissue injury associated with sepsis. Platelets are important for the development of sepsis through an unknown mechanism 22, 24, 25. Recent studies have shown that interactions between platelets and leukocytes, in particular neutrophils 26, play a role during sepsis that can be relevant for the outcome of the disease 27. Lung injury and neutrophil infiltration, for example, were decreased during anti-platelet therapy 17 or platelet depletion 11. Similar results were noted in a model of myocardial infarction 13, where platelet depletion lessened the inflammation levels in the heart. Our results are in line with these previous findings 11, 13, suggesting that platelets are important mediators during inflammation. As previously reported, P2Y12 receptor plays a role in regulating platelet secretion during ADP-induced aggregation and when platelets are activated by other agonists 2, 6. Indeed, activated platelets not only secrete second messengers that recruit other platelets, but they also secrete inflammatory mediators such as IFN-γ, TGF-β and RANTES 1, 28. Hence, antagonizing the P2Y12 receptor can directly influence the inflammatory process by altering platelet secretion of inflammation mediators. There are other pathways in platelet that are activated during inflammation and lead to increased secretion, such as the TLR-4 cascade 29 Platelet-leukocyte interactions are regulated through secretion of inflammatory mediators and through cell-cell interactions mediated by adhesion molecules. Upon P2Y12 mediated activation, platelets express P-selectin on the cell surface. P-selectin binds PSGL-1 on leukocytes, activating the leukocytes and promoting their infiltration into the inflamed tissue 8. Furthermore, adhesion of dendritic cells to injured carotid arteries in mice is mediated by platelets, specifically by interaction with PSGL-1 on dendritic cells 30. Our data show for the first time that during sepsis the expression of P-selectin was reduced in P2Y12 null mice compared to their wild-type counterparts. As a result, platelet and leukocyte aggregate formation was also reduced. The data suggest that a decrease in membrane P-selectin expression may be the mechanism through which platelets contribute to decreased leukocyte activation during inflammation. Because P-selectin expression is P2Y12-dependent, receptor antagonism may modulate platelet-leukocyte interactions. A decrease in the septic-induced co- aggregate formation was also observed in the septic lung of P2Y12 null mice, suggesting that platelet-leukocyte interaction was also modulated within organs as well as systemically. The decrease in inflammation levels is most likely due to changes in platelet activation instead of variation in cell number, as the numbers of circulating platelets were similar among the treatment groups. Interestingly, P-selectin secretion in plasma samples of septic patients was increased compared to healthy controls 9, indicating that P-selectin regulation may play a role in sepsis. A decrease in platelet activation was also noted in clopidogrel-treated mice, and again there was no change in platelet number. The alignment between receptor deficiency and blockage emphasizes that modulating P2Y12 may be a new therapeutic option for sepsis, although the P2Y12 independent effects need to be fully characterized.
Circulating lymphocyte levels during sepsis were elevated in wild-type mice but not in P2Y12 null mice, which is similar to what was observed in clopidogrel-treated mice. Lymphocyte abnormalities have been reported in septic patients, and they were related with the pathophysiology of the disease 31. P2Y12 receptor antagonism influenced circulating lymphocyte numbers over platelets and neutrophils. Previous studies indicate that expression of the P2Y12 receptor is not exclusive to platelets 32, 33. For example, P2Y12 receptor mRNA was detected in lymphocytes and dendritic cells 34, 35, and the decreased inflammation levels and lymphocyte numbers might have resulted from the P2Y12 receptor antagonist affecting the immune system directly instead of through platelets. Considering that sepsis increases lymphocyte apoptosis, it would be interesting to investigate whether P2Y12 receptor deficient lymphocytes are less sensitive to apoptosis. However, although lymphocytes have shown to express P2Y12 mRNA 34, 35, it has not been established that they express a functional P2Y12 receptor. In contrast, platelets are known to express a functional P2Y12 receptor that is crucial for platelet functions and biology. Hence following our study and these previous observations we can conclude that platelet P2Y12 play a determinant role during inflammation.
In an earlier study, we demonstrated that prasugrel metabolites inhibit neutrophil functions in vitro, even though neutrophils do not express the P2Y12 receptor 36. The data suggest a P2Y12 independent effect for this class of drugs. Interestingly, we found for the first time that circulating neutrophils in septic P2Y12 null mice treated with clopidogrel were decreased compared to untreated septic P2Y12 null mice. Hence, clopidogrel may have P2Y12 independent effects during sepsis, and neutrophils are the most likely target. Indeed, the P2Y12 independent effects observed in vitro 36 may explain the altered neutrophil functions observed in vivo.
Our group investigated a murine model of systemic inflammation in which mice were treated with repeated doses of LPS for 4 days23. We found that inflammation was more severe in P2Y12 null mice compared with their wild-type counterparts. In this model of inflammation, however, we observed that P2Y12 null mice are protected against sepsis. The discrepancy may be due to a different phase of inflammation (4 days versus 24 hours) or to a different disease. Interestingly, these different results have been previously observed during a model of rheumatoid arthritis. Specifically, in a peptidoglycan polysaccharide-induced arthritis model following clopidogrel treatment, the disease was exacerbated 21, 37, whereas serum transfer arthritis was more severe in wild-type compared to P2Y12 null mice 38. Indeed, inhibiting platelet activation has different outcomes depending on the phase of inflammation and on the disease model. More investigations are needed to better understand how to safely administer this class of drugs during inflammation.
ADP plays an important role in hemostasis. When released by activated platelets, ADP acts as an aggregating agent and potentiates platelet responses to other agonists. ADP-induced aggregation is mediated by both the P2Y1 and P2Y12 receptors 39. Previous studies have shown that the P2Y1 receptor on endothelial cell surfaces modulates leukocyte recruitment, suggesting a role for P2Y1 during vascular inflammation 40. However, the role of the P2Y1 receptor during sepsis has not been previously investigated. Hence, we wondered whether our observations were due to P2Y12 receptor deficiency or to an altered platelet response to ADP. To address this question, we analyzed P2Y1 null mice in the same model of sepsis. We noted that the P2Y1 receptor did not influence the inflammation levels in the CLP model. Overall, our data suggest that P2Y12 receptor deficiency is responsible for the effects previously observed.
In conclusion, our data show that P2Y12 null mice are protected against sepsis-induced lung injury, which is similar to what we observed following P2Y12 antagonism with clopidogrel. Platelet activation and segregation in the lungs were diminished, suggesting that platelets play a role in inflammation both directly and through immune cell interactions and that their functions can be modulated through the P2Y12 receptor. This effect is specifically due to the P2Y12 receptor and not to an altered response to ADP. Taken together, the data indicate that during sepsis activated platelets play a central role that is dependent on P2Y12 receptor activation.
Supplementary Material
Significance.
Sepsis and sepsis-induced lung injury are one of the leading causes of death in the ICU. Sepsis is characterized by a systemic inflammatory response leading to excessive neutrophil infiltration of the lungs producing tissue damage. There is growing evidence that platelets are involved in neutrophil recruitment and play a key role in neutrophil-mediated organ damage. Hence targeting platelets could offer new therapeutic option for this disease.
Our data show that P2Y12 null mice are refractory to sepsis-induced lung injury, which is similar to what we observed following P2Y12 antagonism with clopidogrel. This effect is specifically due to the P2Y12 receptor, as receptor deficiency and antagonism provided similar results. Hence, targeting the P2Y12 receptor may offer a unique therapeutic strategy for the control of neutrophil migration and activation in sepsis-induced lung injury.
Acknowledgments
Sources of funding
This work was supported by the Research grants HL93231 and HL118593 (S.P.K.), HL111552 (L.E.K.) and HL103197 (M.C.R.) from the National Institutes of Health.
Abbreviations
- ALI
acute lung injury
- CLP
cecal ligation and double puncture
- H&E
hematoxylin and eosin
- PSGL-1
P-selectin glycoprotein ligand 1
- MPO
Myeloperoxidase
- WBC
white blood cells
Footnotes
Conflict of interest disclosures
None
References
- 1.Semple JW, Freedman J. Platelets and innate immunity. Cell Mol Life Sci. 2010;67:499–511. doi: 10.1007/s00018-009-0205-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kunapuli SP, Ding Z, Dorsam RT, Kim S, Murugappan S, Quinton TM. ADP receptors--targets for developing antithrombotic agents. Curr Pharm Des. 2003;9:2303–2316. doi: 10.2174/1381612033453947. [DOI] [PubMed] [Google Scholar]
- 3.Jin J, Kunapuli SP. Coactivation of two different G protein-coupled receptors is essential for ADP-induced platelet aggregation. Proc Natl Acad Sci U S A. 1998;95:8070–8074. doi: 10.1073/pnas.95.14.8070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin J, Daniel JL, Kunapuli SP. Molecular basis for ADP-induced platelet activation. II. The P2Y1 receptor mediates ADP-induced intracellular calcium mobilization and shape change in platelets. J Biol Chem. 1998;273:2030–2034. doi: 10.1074/jbc.273.4.2030. [DOI] [PubMed] [Google Scholar]
- 5.Kahner BN, Shankar H, Murugappan S, Prasad GL, Kunapuli SP. Nucleotide receptor signaling in platelets. J Thromb Haemost. 2006;4:2317–2326. doi: 10.1111/j.1538-7836.2006.02192.x. [DOI] [PubMed] [Google Scholar]
- 6.Kim S, Kunapuli SP. P2Y12 receptor in platelet activation. Platelets. 2011;22:54–58. doi: 10.3109/09537104.2010.497231. [DOI] [PubMed] [Google Scholar]
- 7.Quinton TM, Murugappan S, Kim S, Jin J, Kunapuli SP. Different G protein-coupled signaling pathways are involved in alpha granule release from human platelets. J Thromb Haemost. 2004;2:978–984. doi: 10.1111/j.1538-7836.2004.00741.x. [DOI] [PubMed] [Google Scholar]
- 8.Faraday N, Scharpf RB, Dodd-o JM, Martinez EA, Rosenfeld BA, Dorman T. Leukocytes can enhance platelet-mediated aggregation and thromboxane release via interaction of P-selectin glycoprotein ligand 1 with P-selectin. Anesthesiology. 2001;94:145–151. doi: 10.1097/00000542-200101000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Russwurm S, Vickers J, Meier-Hellmann A, Spangenberg P, Bredle D, Reinhart K, Losche W. Platelet and leukocyte activation correlate with the severity of septic organ dysfunction. Shock. 2002;17:263–268. doi: 10.1097/00024382-200204000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Yaguchi A, Lobo FL, Vincent JL, Pradier O. Platelet function in sepsis. J Thromb Haemost. 2004;2:2096–2102. doi: 10.1111/j.1538-7836.2004.01009.x. [DOI] [PubMed] [Google Scholar]
- 11.Asaduzzaman M, Lavasani S, Rahman M, Zhang S, Braun OO, Jeppsson B, Thorlacius H. Platelets support pulmonary recruitment of neutrophils in abdominal sepsis. Crit Care Med. 2009;37:1389–1396. doi: 10.1097/CCM.0b013e31819ceb71. [DOI] [PubMed] [Google Scholar]
- 12.Hackert T, Sperber R, Hartwig W, Fritz S, Schneider L, Gebhard MM, Werner J. P-selectin inhibition reduces severity of acute experimental pancreatitis. Pancreatology. 2009;9:369–374. doi: 10.1159/000212098. [DOI] [PubMed] [Google Scholar]
- 13.Liu Y, Gao XM, Fang L, Jennings NL, Su Y, Q X, Samson AL, Kiriazis H, Wang XF, Shan L, Sturgeon SA, Medcalf RL, Jackson SP, Dart AM, Du XJ. Novel role of platelets in mediating inflammatory responses and ventricular rupture or remodeling following myocardial infarction. Arterioscler Thromb Vasc Biol. 2011;31:834–841. doi: 10.1161/ATVBAHA.110.220467. [DOI] [PubMed] [Google Scholar]
- 14.Harada K, Matsumoto Y, Umemura K. Adenosine diphosphate receptor P2Y12-mediated migration of host smooth muscle-like cells and leukocytes in the development of transplant arteriosclerosis. Transplantation. 2011;92:148–154. doi: 10.1097/TP.0b013e318221d407. [DOI] [PubMed] [Google Scholar]
- 15.Bunyavanich S, Boyce JA, Raby BA, Weiss ST. Gene-by-environment effect of house dust mite on purinergic receptor P2Y12 (P2RY12) and lung function in children with asthma. Clin Exp Allergy. 2012;42:229–237. doi: 10.1111/j.1365-2222.2011.03874.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paruchuri S, Tashimo H, Feng C, Maekawa A, Xing W, Jiang Y, Kanaoka Y, Conley P, Boyce JA. Leukotriene E4-induced pulmonary inflammation is mediated by the P2Y12 receptor. J Exp Med. 2009;206:2543–2555. doi: 10.1084/jem.20091240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rahman M, Gustafsson D, Wang Y, Thorlacius H, Braun OO. Ticagrelor reduces neutrophil recruitment and lung damage in abdominal sepsis. Platelets. 2014;25:257–263. doi: 10.3109/09537104.2013.809520. [DOI] [PubMed] [Google Scholar]
- 18.Alsharif KF, Thomas MR, Judge HM, Khan H, Prince LR, Sabroe I, Ridger VC, Storey RF. Ticagrelor potentiates adenosine-induced stimulation of neutrophil chemotaxis and phagocytosis. Vascul Pharmacol. 2015;71:201–207. doi: 10.1016/j.vph.2015.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gachet C. ADP receptors of platelets and their inhibition. Thromb Haemost. 2001;86:222–232. [PubMed] [Google Scholar]
- 20.Kunapuli SP, Dorsam RT, Kim S, Quinton TM. Platelet purinergic receptors. Curr Opin Pharmacol. 2003;3:175–180. doi: 10.1016/s1471-4892(03)00007-9. [DOI] [PubMed] [Google Scholar]
- 21.Garcia AE, Mada SR, Rico MC, Dela Cadena RA, Kunapuli SP. Clopidogrel, a P2Y12 receptor antagonist, potentiates the inflammatory response in a rat model of peptidoglycan polysaccharide-induced arthritis. PLoS One. 2011;6:e26035. doi: 10.1371/journal.pone.0026035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hagiwara S, Iwasaka H, Hasegawa A, Oyama M, Imatomi R, Uchida T, Noguchi T. Adenosine diphosphate receptor antagonist clopidogrel sulfate attenuates LPS-induced systemic inflammation in a rat model. Shock. 2011;35:289–292. doi: 10.1097/SHK.0b013e3181f48987. [DOI] [PubMed] [Google Scholar]
- 23.Liverani E, Rico MC, Yaratha L, Tsygankov AY, Kilpatrick LE, Kunapuli SP. LPS-induced systemic inflammation is more severe in P2Y12 null mice. J Leukoc Biol. 2013;95:313–323. doi: 10.1189/jlb.1012518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liverani E, Rico MC, Yaratha L, Tsygankov AY, Kilpatrick LE, Kunapuli SP. LPS-induced systemic inflammation is more severe in P2Y12 null mice. J Leukoc Biol. 2013 doi: 10.1189/jlb.1012518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiang B, Zhang G, Guo L, Li XA, Morris AJ, Daugherty A, Whiteheart SW, Smyth SS, Li Z. Platelets protect from septic shock by inhibiting macrophage-dependent inflammation via the cyclooxygenase 1 signalling pathway. Nat Commun. 2013;4:2657. doi: 10.1038/ncomms3657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clark SR, Ma AC, Tavener SA, McDonald B, Goodarzi Z, Kelly MM, Patel KD, Chakrabarti S, McAvoy E, Sinclair GD, Keys EM, Allen-Vercoe E, Devinney R, Doig CJ, Green FH, Kubes P. Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in septic blood. Nat Med. 2007;13:463–469. doi: 10.1038/nm1565. [DOI] [PubMed] [Google Scholar]
- 27.McCafferty DM, Kubes P, Wallace JL. Inhibition of platelet-activating factor-induced leukocyte adhesion in vivo by a leumedin. Eur J Pharmacol. 1993;232:169–172. doi: 10.1016/0014-2999(93)90770-i. [DOI] [PubMed] [Google Scholar]
- 28.Semple JW, Italiano JE, Jr., Freedman J. Platelets and the immune continuum. Nat Rev Immunol. 2011;11:264–274. doi: 10.1038/nri2956. [DOI] [PubMed] [Google Scholar]
- 29.Zhang G, Han J, Welch EJ, Ye RD, Voyno-Yasenetskaya TA, Malik AB, Du X, Li Z. Lipopolysaccharide stimulates platelet secretion and potentiates platelet aggregation via TLR4/MyD88 and the cGMP-dependent protein kinase pathway. J Immunol. 2009;182:7997–8004. doi: 10.4049/jimmunol.0802884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Langer HF, Daub K, Braun G, Schonberger T, May AE, Schaller M, Stein GM, Stellos K, Bueltmann A, Siegel-Axel D, Wendel HP, Aebert H, Roecken M, Seizer P, Santoso S, Wesselborg S, Brossart P, Gawaz M. Platelets recruit human dendritic cells via Mac-1/JAM-C interaction and modulate dendritic cell function in vitro. Arterioscler Thromb Vasc Biol. 2007;27:1463–1470. doi: 10.1161/ATVBAHA.107.141515. [DOI] [PubMed] [Google Scholar]
- 31.de Pablo R, Monserrat J, Prieto A, Alvarez-Mon M. Role of circulating lymphocytes in patients with sepsis. Biomed Res Int. 2014;2014:671087. doi: 10.1155/2014/671087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sasaki Y, Hoshi M, Akazawa C, Nakamura Y, Tsuzuki H, Inoue K, Kohsaka S. Selective expression of Gi/o-coupled ATP receptor P2Y12 in microglia in rat brain. Glia. 2003;44:242–250. doi: 10.1002/glia.10293. [DOI] [PubMed] [Google Scholar]
- 33.Wang L, Ostberg O, Wihlborg AK, Brogren H, Jern S, Erlinge D. Quantification of ADP and ATP receptor expression in human platelets. J Thromb Haemost. 2003;1:330–336. doi: 10.1046/j.1538-7836.2003.00070.x. [DOI] [PubMed] [Google Scholar]
- 34.Diehl P, Olivier C, Halscheid C, Helbing T, Bode C, Moser M. Clopidogrel affects leukocyte dependent platelet aggregation by P2Y12 expressing leukocytes. Basic Res Cardiol. 2010;105:379–387. doi: 10.1007/s00395-009-0073-8. [DOI] [PubMed] [Google Scholar]
- 35.Wang L, Jacobsen SE, Bengtsson A, Erlinge D. P2 receptor mRNA expression profiles in human lymphocytes, monocytes and CD34+ stem and progenitor cells. BMC Immunol. 2004;5:16. doi: 10.1186/1471-2172-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liverani E, Rico MC, Garcia AE, Kilpatrick LE, Kunapuli SP. Prasugrel metabolites inhibit neutrophil functions. J Pharmacol Exp Ther. 2013;344:231–243. doi: 10.1124/jpet.112.195883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boilard E, Nigrovic PA, Larabee K, Watts GF, Coblyn JS, Weinblatt ME, Massarotti EM, Remold-O'Donnell E, Farndale RW, Ware J, Lee DM. Platelets amplify inflammation in arthritis via collagen-dependent microparticle production. Science. 2010;327:580–583. doi: 10.1126/science.1181928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Su X, Floyd DH, Hughes A, Xiang J, Schneider JG, Uluckan O, Heller E, Deng H, Zou W, Craft CS, Wu K, Hirbe AC, Grabowska D, Eagleton MC, Townsley S, Collins L, Piwnica-Worms D, Steinberg TH, Novack DV, Conley PB, Hurchla MA, Rogers M, Weilbaecher KN. The ADP receptor P2RY12 regulates osteoclast function and pathologic bone remodeling. J Clin Invest. 2012;122:3579–3592. doi: 10.1172/JCI38576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Murugappa S, Kunapuli SP. The role of ADP receptors in platelet function. Front Biosci. 2006;11:1977–1986. doi: 10.2741/1939. [DOI] [PubMed] [Google Scholar]
- 40.Zerr M, Hechler B, Freund M, Magnenat S, Lanois I, Cazenave JP, Leon C, Gachet C. Major contribution of the P2Y(1)receptor in purinergic regulation of TNFalpha-induced vascular inflammation. Circulation. 2011;123:2404–2413. doi: 10.1161/CIRCULATIONAHA.110.002139. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.