1. Introduction
A 20-year trend documents an increase in youth routinely skipping breakfast [1]. Breakfast skipping increases with age from 20% among children age 9–13 to 36% among adolescents age 13–18 [2]. Minority youth are sometimes but not always reported to have higher rates of skipping breakfast compared with their white peers [3], [4], [5] and girls are more likely to skip breakfast than boys, especially to lose weight [3], [6], [7].
Observational studies indicate breakfast eaters have healthier diets [8], [9], make better food choices, and are less likely to eat high fat snacks [10], [11]. Establishing healthy weight promoting behaviors during adolescence, such as eating breakfast is especially important as the average American gains 30 pounds between 18 and 35 years of age [12]. Cross-sectional [13] and observational [14] studies provide evidence of an increase in body mass index (BMI) among breakfast skippers.
Eating breakfast and particularly the school provided breakfast is also associated with an improvement in cognition and academic outcomes among adolescents. This benefit may be more realized by undernourished and urban, minority youth, suggesting a promising strategy for closing the achievement gap [15], [16], [17].
Students in rural schools are more likely to attend small schools, live in poverty, be food insecure, be eligible for free or reduced priced school meals, and come to school unprepared to learn compared to students from urban or suburban areas [18]. A 2015 meta-analysis found that rural youth have 26% greater odds of obesity, compared to urban children [19]. Very little research has been done on how to improve the school food environment in small town and rural schools even though these environments are lagging behind urban and suburban schools [20]. The few studies on rural schools have focused on younger students [21], the school lunch program [22], or competitive food options [23]. The purpose of this clinical trial is to evaluate the effectiveness of a school-based intervention designed to increase participation in the National School Breakfast Program (SBP) among rural high school students by improving physical access to the program, changing social norms, and engaging in promotional activities.
2. Methods
2.1. Theoretical model that guided intervention development
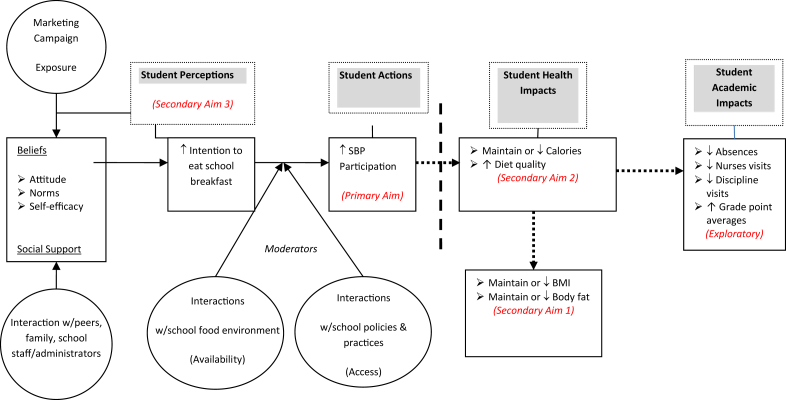
Experts believe that improving school food environment policies and practices may be an effective way to improve youth dietary patterns and address childhood obesity [24], [25], [26]. Very little formal research is reported in the literature about creating and evaluating supportive school breakfast environments. Environment and policy-level interventions that address complex behaviors like dietary patterns need to draw from multiple perspectives to guide intervention development and evaluation. The breakFAST study conceptual model in Fig. 1 draws from the Social Ecologic Model (SEM) [27]and Theory of Planned Behavior (TPB) [28]. The SEM describes the interplay between individual, social and environmental factors. The TPB posits that individual and normative beliefs influence intentions and are mediated by the amount of control of behavior within an environment. TPB allows the development of a framework for identifying key behavioral and normative beliefs affecting intentions that drive behavior [29]. Research has repeatedly shown that social-environmental factors (norms, role models, social support, food environments) are powerful predictors of adolescent behavior [30], [31], [32].
Fig. 1.
Conceptual model.
2.2. Brief intervention description
The design of the breakFAST study intervention was informed by the research and best practice literature, the researchers' own experience conducting school interventions [33], [34], and a pilot study [35], [36]. The intervention aimed to improve student SBP participation by ameliorating the following environmental factors in the high school setting that potentially moderate student intention to eat school breakfast:1) increasing availability and easy access to the SBP through school-wide policy changes 2) addressing normative and attitudinal beliefs through a school-wide SBP marketing campaign 3) providing opportunities for positive interactions that encourage eating school breakfast with social support and role modeling from peers and teachers.
Increased SBP availability and accessibility was to be accomplished by implementing a grab and go style cart or breakfast line located outside the cafeteria in a high traffic hallway, atrium or commons area. New grab and go SBPs were to be developed individually at each intervention school to meet unique needs of each school.
School-wide marketing campaigns were developed by a community partner, Community BluePrint, a marketing and design firm experienced in public health campaigns in educational settings and targeted at youth. Community BluePrint worked with a group of students to design the marketing campaign at each intervention school. A student lead campaign may provide a more relevant and attractive message to the student body than one developed by others.
Positive interactions and social support were to be created by developing school policies, if not already in place, to allow students to eat breakfast in the hallway. Schools were also encouraged to allow eating breakfast in some classrooms when appropriate. Additionally, teachers and school staff were asked to encourage the breakfast program.
As informed by best practices [37], [38], [39], the development of a School Breakfast Expansion Team (SBET) was encouraged at each intervention school. These teams were to consist of a variety of contributors including, but not limited to the principal, food service director, nurse, students, wellness coordinator, and teachers. Team members were expected to meet at least five times. Three times in the year before implementing the SBP changes, and two times after the new program was initiated. The first 3 meetings were to cover the topics of, 1) assessment of the current SBP and goal setting; 2) creating an action plan and 3) discussing communication strategies. The 2 meetings in the year during the new SBP were designed to cover the topics, 4) monitoring your new program and 5) evaluating progress and success.
A key component to the intervention was the partnership with University of Minnesota, Extension. University Extension organizations were developed through federal, state and county funding to “extend” research, knowledge and expertise to the public. Extension's education and research staff live and work across the state, creating a local approach to translating evidence based practices to communities across the state. Extension Coordinators, trained in school wellness programing, served as the intervention facilitators and were assigned to schools in their geographical area. Extension Coordinators were to provide support to schools in intervention development and implementation, communicated progress, successes, and also to assist in the logistics (e.g., reserve measurement rooms) for data collection. Study staff were to meet bi-weekly with the Extension team to troubleshoot issues with interventions as well as discuss upcoming research activities and provide training on protocols.
2.3. Study design overview
A convenience sample of 16 rural high schools agreed to study participation and were randomized to treatment or delayed treatment groups in equal allocation. The delayed treatment group served as a non-interventional control for the first year of follow-up for the primary comparison with the treatment group at the end of the first year of follow-up, but implemented a modified form of the intervention in the second year of follow-up. The primary reason for this approach was to provide comparison schools with an equitable incentive and benefit to participating in the research study. Comparison schools received the same monetary incentive as intervention schools, as well as research study staff support in implementing the delayed intervention. The main difference was the marketing package offered to intervention schools, but not to comparison schools. Investigators were also interested to see results of the implementation of the intervention without a professional marketing package, to investigate a slightly more “real-world” approach to the intervention. Additionally, because of budget and staff limitations, the study was conducted across 2 waves of eight schools where each wave was implemented in successive school (calendar) years. Thus, in year one, four schools implemented the intervention, in year two eight schools (four intervention, four delayed intervention) implemented the intervention and in year three four delayed intervention schools implemented the intervention. Throughout, the schools in the delayed intervention group will be described as the ‘control condition’ during the first year of follow-up, and the ‘delayed intervention condition’ in the second year of follow-up.
The process of randomization of schools to treatment assignment was blocked so that 4 schools were assigned to intervention and 4 to control in each wave. As of the start of wave 1, only 13 schools had been recruited (see 4. Limitations), so a simple random subsample of 8 was assigned to wave 1. Within this subsample of 8, schools were randomly assigned to treatment or control by selection of a random permutation of the 8 labels (4 intervention, 4 control). For wave 2, three additional schools had been recruited prior to the randomization for wave 2, for a total of 8 schools. The wave 2 schools were then randomized similarly to wave 1. Importantly, all wave 2 schools were recruited prior to randomization to treatment or control for wave 2.
Study schools received $5000 each to use toward implementing their interventions. Delayed intervention schools did not receive these funds until after they had completed their control phase. Schools were allowed to use funds for equipment purchases, construction or technology needs (e.g., hardwiring areas where carts were located), additional staff time needed for implementation, promotion and anything else identified by the school and used for the intervention only. As a requirement of receiving this funding, schools were expected to install a new grab and go breakfast cart outside of the cafeteria, and change or update policy to allow eating in the hallways. During the first year of follow-up for each wave, four fidelity observations of both the intervention and delayed intervention groups were conducted to evaluate adherence to the requirement of either making these necessary changes to the SBP (intervention) or not making any changes to regular breakfast service (control).
The primary outcome for the randomized comparison was change in mean school breakfast participation from baseline (academic year prior to implementation of intervention) to school year follow-up 1 (academic year during which the intervention was being implemented).
For secondary outcomes (change in knowledge, attitudes, and beliefs; body mass index; and nutritional quality of the diet), a cohort of students identified as “breakfast skippers” were randomly selected to participate in survey, objectively measured height, weight, and percent body fat, and 24-h dietary recalls. The survey and dietary measures were collected at baseline and 1 school year follow-up (time point 1). The anthropometric measures were collected at baseline, 1 school year follow up (time point 1) and 2 school years follow-up (time point 2).
2.4. School recruitment
To recruit the study schools an open invitation was posted on the Minnesota School Nutritional Association (MNSA) website and listserv. The MSNA is used by many Minnesota food service directors as a resource to locate funding and support for school food programs. Several informational webinars were conducted for interested school personnel (mainly the principal and food service director). The webinar recordings are available on the study website: z.umn.edu/projectbreakfast. Schools were generally evaluated for study inclusion based upon being located outside of the 7-county Twin Cities metropolitan area; not having a grab and go reimbursable school breakfast option; and low SBP (under 20%) participation. Sufficient student enrollment (e.g., over 500) size) and student minority enrollment (at 10%) were also considered.
At each participating school the Principal (Superintendent at one school) and Food Service Director both signed a detailed Memorandum of Understanding (MOU), developed by University of Minnesota study staff and approved by the University of Minnesota Office of the General Council. The MOU outlined the expectations of the study schools to provide support for data collection and to carry out the intervention, or control followed by delayed intervention condition as assigned. The MOU also outlined the expectations of the University of Minnesota study staff to provide support to the intervention, grant dollars to study schools for intervention development, and safe and respectful data collection practices. The MOU was signed during in-person meetings at each study school.
2.5. Student recruitment and enrollment
2.5.1. Initial classroom screening for the cohort of “breakfast skippers”
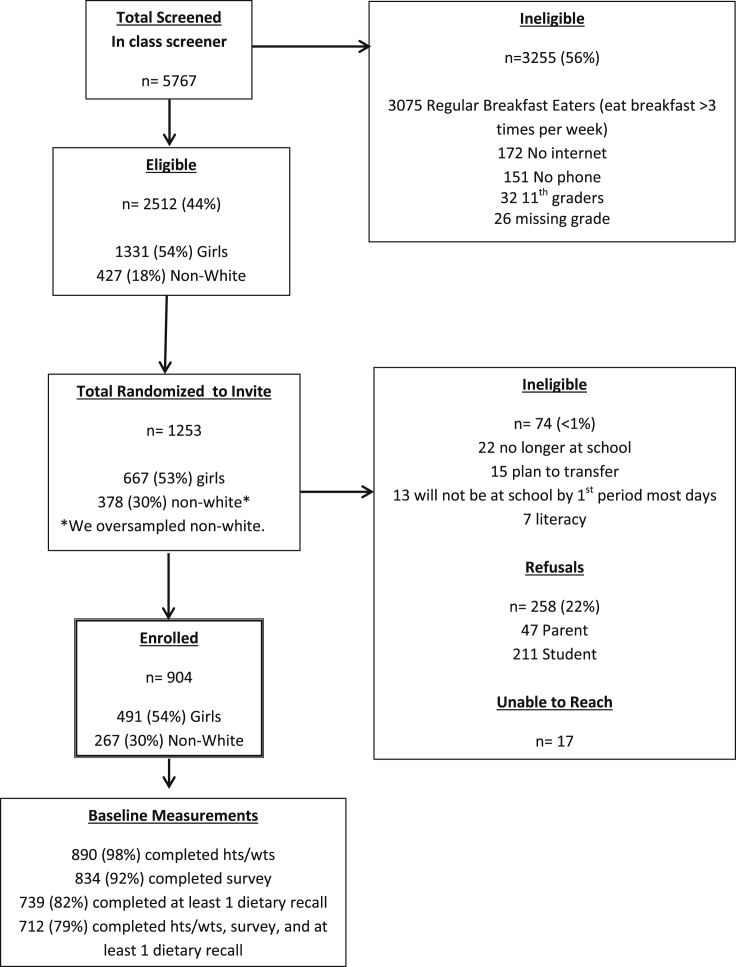
The initial identification of “breakfast skippers” (eat breakfast ≤3 days in a school week) was important in assessing influence of the intervention on most at risk students. All 9th and 10th grade students attending study schools and who were present on the day of screening were invited to complete an initial 7-item screening paper/pencil questionnaire to assess the frequency of eating breakfast during a normal school week (Monday through Friday). Forty-four percent of screened students were eligible to be randomly selected for invitation into the BreakFAST study because they were in 9th or 10th grade, had access to a phone and internet at home, at school or at the library, and ate breakfast 3 or fewer days per school week (44%, n = 2512). Primary reasons for initial student ineligibility were due to already eating breakfast from any source at least 4 days in a usual school week (53%, n = 3075), no access to the internet (0.03%, n = 172) or phone (0.03%, n = 151). See Fig. 2 for CONSORT flow diagram.
Fig. 2.
CONSORT flow diagram.
2.5.2. Identification of “breakfast skipper” cohort and parent consent
Among the eligible sample, 50% (1253) were randomly selected and invited to participate in the breakFAST study, with a target sample size of 800 (50 per school). To meet a minority enrollment goal of 30%, we oversampled for nonwhite/minority students at each study school. A passive parental consent process was used, with a signed letter from the school principal and the study principal investigator (PI) mailed to the parent(s) or guardian(s) of the invited students describing the study. The mailing also included a consent page, an example of survey items, and instructions on how to withdraw consent for participation of their student. Parents were given 10 days to withdraw consent by contacting the school or project manager by phone, email, or mail with all contact information provided.
2.5.3. Invite to student to determine enrollment eligibility for the “breakfast skipper” cohort
After the 10 day waiting period, contact information (address and phone number) was requested from the schools for all initially eligible and consented students. Students were then mailed a letter inviting them to be screened for a second time to determine eligibility to participate in the study. Multiple modalities (e.g., internet, phone, at school) were necessary to maximize recruitment rates. Students were eligible based on affirmative survey responses to not planning to transfer schools, planning to be present in the mornings the next school year, not being pregnant (if female) and ability to understand written and spoken English at least “sort of well”. Eligible students were provided a study packet that described the study including, a hard copy consent page, a unique username, password and directions for completing an online baseline survey assessing breakfast attitudes and perceived barriers, and a Food Amounts Booklet for completing the dietary recalls.
A final ‘stop and check’ step was added to enrollment procedures asking students to think about the time requested to complete the study measures (completing height and weight at school, a 10-minute online survey and three 20-minute 24-hour dietary recalls collected over the phone), and decide if they are sure they want to participate and can complete all study measures. Accordingly, refusal rates went up after implementation of this important final step. This process was continued for the duration of enrollment.
Only 17 students were unable to be reached during the recruitment phase. Study staff enrolled 533 (59%) students through telephone recruitment. The remaining 371 students were either enrolled online or in-person at the school. A total of 47 (<1%) parents and 211 (17%) students declined participation. Participating students received a maximum of $75 incentive for each data collection point. Gift card amounts were accumulative and based upon incentives earned through completing the study measures. The University of Minnesota Institutional Review Board approved the recruitment and enrollment process.
2.6. Protocol – recruitment and enrollment
Extensive protocols were developed for the school and student recruitment and enrollment process for Project breakFAST. The following protocols (e.g., forms, quality control procedures) related to recruitment and enrollments are available on the study website: z.umn.edu/projectbreakfast.
-
•
Memorandum of Understanding (MOU)
-
•
Letters to parents and students
-
•
Student phone call scripts
-
•
Student enrollment tracking forms
2.7. Measures
Study assessments were conducted at baseline (school year prior to intervention period), during intervention school year (follow up 1), and school year one year after the intervention school year (follow-up 2). Measures come from two primary sources: school provided administrative data and student subsample provided data.
2.7.1. Primary outcome and measures
The breakFAST study primary outcome (participation in school breakfast program) was measured by collecting school-level data (N = 7792 at baseline) provided by the school for three school years. First, at baseline (all incoming 9th and 10th grade students) prior to the intervention school year; school year follow-up 1 (all 10th and 11th grade students) and at school year follow-up 2 (all 11th and 12th grade students). The primary hypothesis is that during the intervention school year; school-wide SBP participation will be higher in the intervention schools versus comparison group.
Each school received an excel file of variables and definitions requested. For each student, demographic information (e.g., race, ethnicity, grade level); grade point average (GPA) (term/semester GPAs and cumulative GPAs); attendance (days in attendance during school year); disciplinary action (number of events and description during school year) free and reduced priced meal eligibility status; and school breakfast participation (number of days during the school year) were requested. Administrative data were de-identified, which does not allow for measuring within-student changes across academic years except in the cohort of self-reported breakfast skippers, where consent was obtained for collection of an identifier.
2.7.2. Secondary aims and outcome measures
Three secondary aims were investigated using objectively measured height, weight and percent body fat, three dietary recalls and survey data from the student subsample (n = 904). Evaluations were completed at baseline (at time of enrollment) and time point 1 (approximately 1 year after enrollment). Only height, weight, and percent body fat will be collected from the cohort during time point 2 (approximately 2 years after enrollment).
Secondary Aim 1
High school students in the intervention condition will decrease their rate of weight gain relative to height gain as measured by change in body mass index and percent body fat compared to students in the control condition from baseline to the end of the first year of follow-up.
2.7.2.1. Body mass index (BMI)
Student BMI, adjusted for age and gender was calculated according to the formula: weight in kilograms/((height in meters)*(height in meters)). BMI is the recommended method of assessing overweight and obesity among children and adults [40]. Height and weight were to be measured for all consented/assented students at baseline, time point 1 and time point 2. At each measurement time-point, trained staff took height and weight measures in a private setting in the school with students dressed in light clothing, shoes removed and pockets emptied. Weight was measured in duplicate on a portable digital scale, Tanita Model BF350A Body Composition Analyzer/Scale, and recorded to the nearest 0.1 kg for both trials. If the two measures differed by more than 0.2 kg, a third measure was obtained. The mean of the two, or closest two of three, values was used for analysis. The scale was calibrated with a 5-kg weight at the beginning of each testing day. Height was measured in duplicate, using a portable Schorr stadiometer (Schorr Production, Olney, MD) and recorded to the nearest 1 mm for both waves. If the two measures differed by more than 5 mm, a third measure was obtained. The mean of two, or closest two of three, values was used for analysis. Percent Body Fat. The Tanita uses a foot-to-foot approach that has been shown to be highly reliable (r = 0.98) and provides valid estimates of percent body fat in children [41], [42]. Staff entered the student sex and height in centimeters along with a weight reading. Percent body fat was measured twice and the mean of the replicates was used in analyses.
Secondary Aim 2
High school students in the intervention condition will maintain or decrease their energy intake while improving dietary intakes of low fat dairy, whole grains and fruit compared to the control students at the end of the first year of follow-up.
2.7.2.2. Energy intake
To assess energy intake 2 weekday and 1 weekend 24-h telephone recalls were to be collected from each student participant at baseline and time point 1. The dietary recalls were collected via telephone using Nutrition Data Systems for Research (NDSR) nutrient calculation software. NDSR is a computer based software application developed at the University of Minnesota that allows for direct entry of dietary data in a standardized fashion [43]. The multiple-pass interview technique was used to prompt for complete food recall and descriptions [44], [45]. A food amount booklet (mailed to participants during enrollment) was used to aid in estimating food amounts. All dietary interviews were conducted by staff trained and certified in the collection of dietary recalls using NDSR. For all breakfast meals reported, detailed information about meal location and the source of foods was ascertained. Diet Quality. Using the food and nutrient intakes estimated from the 24-h dietary recalls Healthy Eating Index 2010 (HEI) scores were calculated. The HEI is a standardized measure of diet quality as defined by the key diet-related recommendations of the 2010 Dietary Guidelines [46]. An individual total HEI score can be created ranging from 0 to 100. Code for creating HEI-2010 component scores is publicly available.
Secondary Aim 3
At the end of the first year of follow-up, compared to students in the control condition, high school students in the intervention condition will report receiving more support to eat school breakfast. Support will be social (increased peer and school support) or related to the school environment (satisfaction with serving locations and times, eating locations, foods and increased availability of low fat dairy, fruits and whole grains for breakfast).
The student survey included constructs that have been shown in the literature to be correlates or predictors of breakfast intake among adolescents including: eating and activity patterns, family meals, food security, and perceptions including the school food environment, barriers to eating the school breakfast and beliefs about the benefits to eating the school breakfast. Table 1 shows the primary scales and questions used in the survey, previous research documents the validity and reliability of many of the survey items [31], [35], [47], [48], [49], [50], [51], [52].
Table 1.
Selected breakFAST study survey items and sources.
| Domain and source | Question and response |
|---|---|
| Assessing general breakfast habits [48], [50] (adapted from original sources) |
During a normal school week, how many days PER WEEK do you …
|
| Intension to eat breakfast [50] (adapted from original source) |
I intend to eat school breakfast most days this school year
|
| Beliefs about breakfast [47] (adapted from original source) |
How strongly do you agree with the following statements?
|
| Perceptions of benefits of breakfast [48] (adapted from original source) |
By eating school breakfast, what do you think the likelihood is of …
|
| Confidence to eat breakfast [50] | How confident are you that you could change or maintain your eating habits to eat breakfast most days? Not at all confident; A little confident; Somewhat confident; Mostly confident; Very confident |
| Barriers to eating school breakfast [48], [50] (adapted from original sources) |
How strongly do you agree with the following statements?
|
| Social Support/Encouragement to Eat Breakfast [31] (adapted from original source) |
During a usual MONTH, how often do the following people encourage you to eat or continue to eat breakfast AT SCHOOL?
|
| Social Norms [50] | How strongly do you agree with the following statements?
|
| Family Breakfast Meals [51] (adapted from original source) |
22. During the PAST 7 DAYS, how many times did all or most of the people living in your home eat BREAKFAST together? [12] 23. During the PAST 7 DAYS, how many times was at least one of your parents/guardian in the room with you when you ate BREAKFAST? [13] |
| Family Breakfast Meal Norms [51] (adapted from original source) |
How strongly do you agree with the following statements about breakfast meals eaten together with your family?
|
| Family Breakfast Meal Beliefs [51] (adapted from original source) |
How strongly do you agree with the following statements about breakfast time in your family?
|
| Food Insecurity [49] |
|
2.7.3. Exploratory measures
School-wide aggregate and student-level cohort data on attendance, grade point averages, and disciplinary events were collected to allow for assessing the impact of increased breakfast eating on these various academic and behavioral outcomes. For the Wave 2 cohort, a question was added to the post-intervention survey to assess frequency of visits to the school health office in the prior year.
2.8. Protocol – student assessments
The following protocols related to administrative data and student assessments are available on the study website: z.umn.edu/projectbreakfast.
-
•
A detailed 22-page Manual of Procedures (MOP) was developed for assessing height, weight, and percent body fat assessment and data recording, including quality control checks.
-
•
Student Screener
-
•
Student Survey
-
•
Measurement completion tracking form
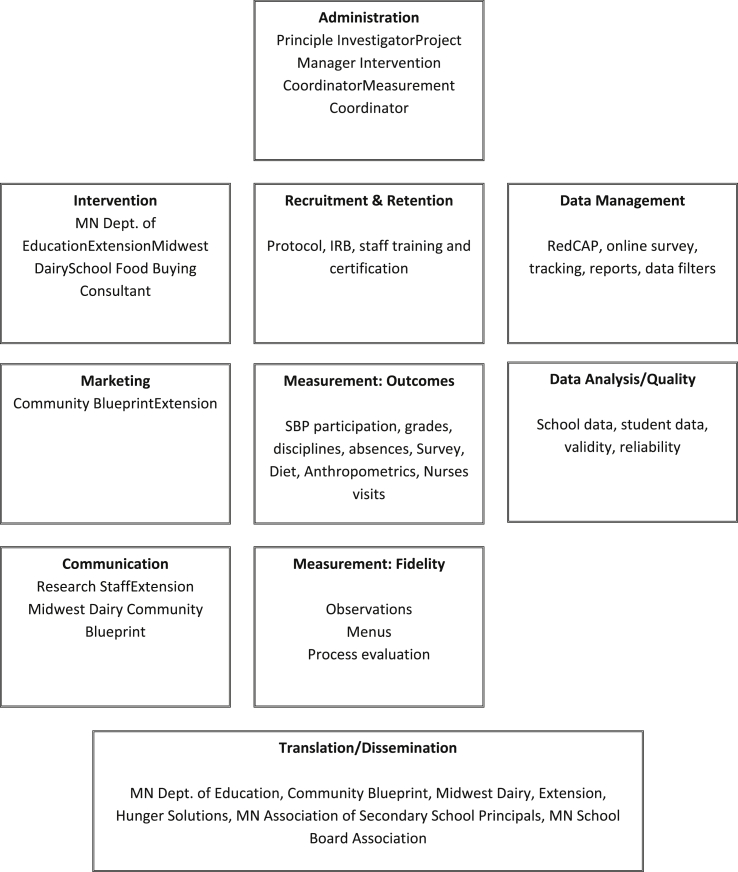
2.9. Project organization
Fig. 3 illustrates the organizing structure of the study, including dissemination partners.
Fig. 3.
Organizational chart.
2.10. Study hypotheses and statistical analysis plan
All statistical analyses will be performed on an intent-to-treat basis.
2.10.1. Primary aim
The primary outcome is change in the rate of SBP participation from baseline to post intervention. Rate of SBP participation is defined as the number of days a student received a school breakfast divided by attendance days. This administrative data will be reported on all students in the school for the baseline and post intervention periods. The change in rates from baseline to post intervention will be treated as a continuous variable, calculated at the school-level as mean rate of participation at follow-up minus mean rate of participation at baseline. Secondary analyses will be performed to adjust for any imbalances in the treatment groups for important baseline covariates not successfully addressed by randomization will be performed by linear regression. Since SBP are reported on the school level, additional adjustment for individual-level covariates can only be performed by school-level results, e.g. the proportion of the school that is female. Subgroup analyses by gender and free and reduced price meal status will be performed by restricting analyses to observations in each year with these statuses within each school.
2.10.2. Secondary aims
Since individual-level changes are available for the cohort of “breakfast skippers”, random effects models will be used to estimate changes in Healthy Eating Index scores, energy intake (kcal) and other continuous dietary outcomes, accounting for within school correlation. Poisson regression models will be used to analyze serving count data. If over dispersion is observed, a negative binomial model will be fit for these data instead. Change in BMI outcome will be analyzed both on the original scale, and also as age-sex adjusted percentiles based on national data. Otherwise, the methods of analysis for BMI data are similar to those for the continuous dietary outcomes. Binary outcomes, such as several of the social and environmental variables for Secondary Aim 3, will be analyzed by generalized linear models, using Generalized Estimating Equations to account for clustered data. Items measured on the Likert scale will be analyzed using a modified version of the Mann Whitney test for clustered data [53]; additionally, positive (strongly agree, agree) and negative categories (disagree, strongly disagree) will be collapsed and a modified chi-square test for clustered data [54] used to compare the resulting 2 × 3 tables (intervention group vs. positive-neutral-negative response categories).
2.11. Power and sample size justification
The primary outcome is change in average school breakfast participation evaluated within each individual school, computed as the average of the participation rate of each student (number of days breakfast purchased/number of attendance days) within the school. Because identifying information is not available for students across years in the administrative data provided by schools, the within-school data are in effect treated as two samples. The data set thus consists of 16 observations of change in average school breakfast participation with n = 8 schools in each treatment group.
Comparisons are based on a two-sample t-test with two-sided comparison and a type I error rate of 5%. Estimates of the variability in change in mean SBP in a control condition were based on pilot data in 4 schools with individual student-level identifiers. Based on these data, the estimated individual-level change in SBP in a control condition had a std deviation of less than 0.20 and within-school correlation of less than 0.05. School enrollments in 9th and 10th grade average approximately 200 in participating schools. Power estimates for a two-sample t-test based purely on school-level data were based on simulations of an individual level random effects model with random effect for school, subject to the above parameters in 8 schools, then analyzed using a school-level t-test. Based on these assumptions, power is estimated to be 80% to detect a treatment difference of change in mean SBP of 7% and 90% to detect a change in SBP of 8%.
For secondary outcomes in the cohort of self-identified “breakfast skippers”, individual identifiers are available. Power calculations are based on a cluster-randomized design in which sample size of a trial with independent observations is inflated by a factor of 1+(m−1)ρ, where m is the average cluster (school) size and ρ is the intraclass correlation coefficient. Estimates for variability in change in BMI on an absolute scale (sd = 1.01, ICC = 0.001) and as age-sex adjusted percentile (sd = 8.14, ICC = 0.01) were obtained from pilot study data, while variability of change in total energy in kcals (sd = 650, ICC = 0.10) was provided by estimates from the Nutrition Coordinating Center at the University of Minnesota. With these assumptions, power is estimated at 85% to detect a difference in mean change in BMI of 0.22 on an absolute scale or 2.2% points when measured as an age-sex adjusted percentile. There is an 82% power to detect a mean change in total energy of 325 kcals.
3. Results
Table 2 describes the sixteen rural high schools enrolled into the breakFAST study. Using the National Center of Educational Statistics and Rural Urban Commuting Area location codes [55], half of the study high schools were located in communities described as rural town fringe (e.g., closest to suburbs) and the other half more remote described as small town rural. One school was located in a city. Average SBP participation was 14% across all 16 study schools, ranging from 3% to 38%. On average 34% of students at the 16 schools were eligible for a free breakfast (20–58%). On average, only 28% took advantage of the free breakfast offered (13–57%).
Table 2.
Characteristics of breakFAST study high schools.
| Wave | Study high school | Grades | Total enrollment | % non-white | Eligible for free/reduced priced meals (%) | National school breakfast particiption (%) | Received a free breakfast (%) | High school locationc |
|---|---|---|---|---|---|---|---|---|
| Cambridge–Isanti High Schoola | 9–12 | 1508 | 7% | 33% | 7.8% | 18.2% | Rural/Town Fringe | |
| 1 | Hutchinson High Schoola | 9–12 | 869 | 7% | 20% | 3.2% | 12.7% | Town/Rural |
| 1 | Le Sueur–Henderson Secondarya | 9–12 | 302 | 17% | 32% | 11.2% | 25.8% | Town/Rural |
| 1 | Owatonna Seniora | 9–12 | 1514 | 19% | 30% | 12.6% | 29.0% | Town/Rural |
| 1 | St. James Secondarya | 7–12 | 583 | 14% | 39% | 16.8% | 32.6% | Town/Rural |
| 1 | Montevideo Seniora | 8–12 | 508 | 8% | 36% | 10.1% | 19.5% | Town/Rural |
| 1 | Apollo Seniora | 9–12 | 1223 | 33% | 58% | 16.7% | 28.3% | City |
| 1 | Albany Senior Higha | 9–12 | 539 | 2% | 21% | 8.0% | 20.9% | Rural/Town Fringe |
| 2 | Dassel–Cokato Seniorb | 9–12 | 649 | 3% | 30% | 7.4% | 13.1% | Rural/Town Fringe |
| 2 | New London–Spicer Seniorb | 9–12 | 416 | 3% | 23% | 15.5% | 37.8% | Town/Rural |
| 2 | Willmar Seniorb | 9–12 | 1166 | 20% | 55% | 37.9% | 57.3% | Rural/Town Fringe |
| 2 | Bemidji Seniorb | 9–12 | 1354 | 24% | 45% | 11.2% | 19.8% | Rural/Town Fringe |
| 2 | Brainerd Senior Highb | 9–12 | 1896 | 7% | 39% | 12.0% | 25.2% | Town/Rural |
| 2 | Morris Area Secondaryb | 7–12 | 495 | 7% | 24% | 18.2% | 35.8% | Rural/Town Fringe |
| 2 | Rocori High Schoolb | 9–12 | 746 | 3% | 24% | 13.7% | 39.2% | Rural/Town Fringe |
| 2 | Lincoln High School – Thief River Fallsb | 9–12 | 634 | 10% | 34% | 20.3% | 37.2% | Town/Rural |
School Year 2012/13 Data.
School Year 2013/14 Data.
Combines National Center of Educational Statistics (NCES) and Rural Urban Commuting Area (RUCA) codes data to assign one of 5 school location categories: City, Suburb, three Rural designations (in order of increasing rurality): Rural/Town Fringe, Town/Rural, Rural [55]. NCES location codes are assigned using school address and proximity to urban area. RUCA location codes are assigned using census tract (2000) population density, urbanization, and total daily commuting data.
The CONSORT diagram (Fig. 2) describes the results of the student screening, recruitment and enrollment process. Fifty-three percent of the 9th and 10th graders screened were ineligible for the study because they ate breakfast regularly from any source defined as 4 or more days in a normal school week. The total student enrollment goal was exceeded (904/880) and minority enrollment goal was met (30%). Overall refusal rates were 22% with parent refusal rate low (4%) and a student refusal rate of 18%. Baseline measurement protocol were successfully implemented where 98% of student enrolled in the breakFAST study completed heights, weights and percent body fat, 92% completed the survey, 82% completed at least 1 dietary recall. Seventy-nine percent of enrolled students completed height, weight, body fat, survey, and at least 1 dietary recall.
4. Discussion
The primary goal of the BreakFAST study is to evaluate an intervention designed to improve participation in the SBP among high school students. This study design represents a unique rural community clinical trial. The strengths of the community-based approach are translation of best practices in a real world setting, interventions based on local school context and assessment of outcomes relevant to multiple stakeholders. The community setting also allowed for many lessons learned.
First, due to the rural focus of the study, over 18,000 miles were covered by research staff, primarily related to measurement activities. Adaptation of planned protocols, such as conducting unannounced 24-h recall data collection on site, to accommodate completion of some study measures at the school site was necessary. While the onsite strategy was successful, the logistics added costs. An estimated additional $10,000 due to mileage costs to achieve higher measurement success rates was incurred.
Second, mid study, the University of Minnesota Extension program, which was the primary school intervention team liaison, was required to restructure its programs due to federal funding cuts imposed by the American Taxpayer Relief Act (2014) and an ongoing delay in passage of the Farm Bill during the 2014 legislative session. The restructure resulted in a 40% staffing downsize to a more regional model. Due to this interruption, new Extension staff was assigned to work on the breakFAST project, requiring additional training by UMN staff as well as increased mileage expenses for Extension because some were no longer serving schools in their local areas [56].
Third, schools utilize third party software companies to manage their massive amounts of data. Obtainment of student-level objective data from schools (e.g., attendance, SBP participation) required extra charges from software vendors for standardized filter development and data queries. Five unique software vendors provided services to the 16 study schools. Charges varied among vendors and $23,000 in unplanned costs for access to these data were incurred.
Finally, baseline data provided by the subsample identified that 57% of students were not eating breakfast because they were not hungry in the morning. Early in Wave 1 this data was provided to each intervention school along with the suggestion of considering a later grab and go breakfast, often called second chance or after the bell breakfast in the best practice literature. In addition, a summary of the scientific literature that described a biological change in sleep pattern preferences for staying up later (and waking up later) among adolescents as normal child development was presented. As a result of this data, each intervention school offered a second chance grab and go breakfast to improve accessibility of the SBP to their high school students. All Wave 2 schools initiated a second chance breakfast at the beginning of their intervention school year, including delayed intervention schools.
5. Limitations
The original randomization plan called for randomization to be fully stratified by wave: schools would be simultaneously assigned to wave and intervention/control in a manner that preserved balance between intervention and control within each wave and reduce the possible confounding of treatment difference by wave. However, randomization to waves was not fully implemented due to the withdrawal of 3 schools prior to randomization of Wave 1. Of the 16 schools originally agreeing to participate, these three schools underwent drastic administrative turn-over (superintendent or principal resignations) and so were no longer comfortable participating in the intervention. As described in the study design overview (2.3 above) three new schools were recruited to participate in Wave 2 prior to randomization for Wave 2. Because the selection of Wave 1 participants from the 13 available schools was determined by simple random sampling, and treatment condition was blocked within wave, the withdrawal of these three schools did not affect the validity of the randomization to intervention or control conditions. However, while balance between intervention and control conditions is balanced by the randomization within wave, the scheme as implemented lacks perfect random assignment of schools to wave as the three schools recruited after Wave 1 had started were not eligible to participate in Wave 1.
As a result, the analysis plan for the primary endpoint will be based on a permutation test where permutations will be randomly selected from among the admissible permutations for the randomization scheme as implemented. Likewise, a permutation test will be used to assess the significance of wave as a possible predictor of treatment outcome.
Collection of administrative data from schools required substantial quality control checks due to a lack of standard data reporting practices across study schools.
Additionally, the schools participating were intentionally recruited from rural high schools in Minnesota and results may not generalize to other settings, including schools in urban settings.
6. Summary
The breakFAST study successfully recruited 16 rural high schools and exceeded enrolling and measuring a cohort of students at baseline, including 30% minority students, into a randomized clinical trial. At the conclusion of the breakFAST study, we will be positioned to address a significant critique of the current breakfast literature [57] by engaging a study design with the ability to evaluate whether an intervention designed to increase school breakfast program participation is effective in changing behavior and nutrition outcomes (nutritional quality of diet, BMI, and percent body fat) among students. In addition, the focus on rural school food environments will provide a unique addition to the health disparities literature. Finally, the breakFAST study addresses concerns by three stakeholder groups: school food service directors and feasibility of improving participation in the SBP in high schools, school principals and other administrators (e.g., school boards) and the relationships among SBP and academic-related outcomes (e.g., grades, attendance, disciplinary events), and hunger advocates as they identify ways to successfully address students at risk for hunger.
Conflicts of interest
The Authors have no conflicts of interest to report.
Acknowledgment
The funding for this study is provided by the National Heart, Lung and Blood Institute of the National Institutes of Health (5R01-HL113235-03, PI: Nanney, MS) ClinicalTrials.gov unique ID: 1111S06384. The data for this study were managed through REDCap Grant Number UL1TR000114 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The following University of Minnesota team members contributed substantially to the methodologies described in this paper: Susan Lowry with data management and Extension Educators and Coordinators for logistical support.
Contributor Information
Marilyn S. Nanney, Email: msnanney@umn.edu.
Amy Shanafelt, Email: shanafel@umn.edu.
Qi Wang, Email: wangx890@umn.edu.
Robert Leduc, Email: robertl@ccbr.umn.edu.
Ellen Dodds, Email: dodd0039@umn.edu.
Mary Hearst, Email: mohearst@stkate.edu.
Martha Y. Kubik, Email: kubik002@umn.edu.
Katherine Grannon, Email: youn1286@umn.edu.
Lisa Harnack, Email: harna001@umn.edu.
References
- 1.Siega-Riz A.M., Popkin B.M., Carson T. Trends in breakfast consumption for children in the United States from 1965 to 1991. Am. J. Clin. Nutr. 1998;67(4) doi: 10.1093/ajcn/67.4.748S. [DOI] [PubMed] [Google Scholar]
- 2.Deshmukh-Taskar P., Nicklas T a, Radcliffe J.D., O'Neil C.E., Liu Y. The relationship of breakfast skipping and type of breakfast consumed with overweight/obesity, abdominal obesity, other cardiometabolic risk factors and the metabolic syndrome in young adults. Natl. Health Nutr. Exam. Surv. (NHANES) Public Health Nutr. 2012;16(11):1–10. doi: 10.1017/S1368980012004296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zapata L.B., Bryant C.A., McDermott R.J., Hefelfinger J.A. Dietary and physical activity behaviors of middle school youth: the youth physical activity and nutrition survey. J. Sch. Health. 2008;78(1):9–18. doi: 10.1111/j.1746-1561.2007.00260.x. quiz 65-67. [DOI] [PubMed] [Google Scholar]
- 4.Affenito S.G., Thompson D.R., Barton B.A. Breakfast consumption by African-American and white adolescent girls correlates positively with calcium and fiber intake and negatively with body mass index. J. Am. Diet. Assoc. 2005;105(6):938–945. doi: 10.1016/j.jada.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Stang J., Kong A., Story M., Eisenberg M.E., Neumark-Sztainer D. Food and weight-related patterns and behaviors of hmong adolescents. J. Am. Diet. Assoc. 2007;107(6):936–941. doi: 10.1016/j.jada.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 6.Moore L.L., Singer M.R., Qureshi M.M., Bradlee M.L. Dairy intake and anthropometric measures of body fat among children and adolescents in NHANES. J. Am. Coll. Nutr. 2008;27(6):702–710. doi: 10.1080/07315724.2008.10719747. [DOI] [PubMed] [Google Scholar]
- 7.Barton B. a., Eldridge A.L., Thompson D. The relationship of breakfast and cereal consumption to nutrient intake and body mass index: the national heart, lung, and blood institute growth and health study. J. Am. Diet. Assoc. 2005;105(9):1383–1389. doi: 10.1016/j.jada.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Ask A.S., Hernes S., Aarek I., Johannessen G., Haugen M. Changes in dietary pattern in 15 year old adolescents following a 4 month dietary intervention with school breakfast–a pilot study. Nutr. J. 2006;5:33. doi: 10.1186/1475-2891-5-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pedersen T., Meilstrup C., Holstein B.E., Rasmussen M. Fruit and vegetable intake is associated with frequency of breakfast, lunch and evening meal: cross-sectional study of 11-, 13-, and 15-year-olds. Int. J. Behav. Nutr. Phys. Act. 2012;9(1):9. doi: 10.1186/1479-5868-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Utter J., Scragg R., Mhurchu C.N., Schaaf D. At-home breakfast consumption among New Zealand Children: associations with body mass index and related nutrition behaviors{a figure is presented} J. Am. Diet. Assoc. 2007;107(4):570–576. doi: 10.1016/j.jada.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 11.Resnicow K. The relationship between breakfast habits and plasma cholesterol levels in schoolchildren. J. Sch. Health. 1991;61(2):81–85. doi: 10.1111/j.1746-1561.1991.tb03242.x. [DOI] [PubMed] [Google Scholar]
- 12.Gordon-Larsen P., The N.S., Adair L.S. Longitudinal trends in obesity in the United States from adolescence to the third decade of life. Obes. (Silver Spring) 2010;18(9):1801–1804. doi: 10.1038/oby.2009.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gleason P.M., Dodd A.H. School breakfast program but not school lunch program participation is associated with lower body mass index. J. Am. Diet. Assoc. 2009;109(2) doi: 10.1016/j.jada.2008.10.058. [DOI] [PubMed] [Google Scholar]
- 14.Szajewska H., Ruszczynski M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit. Rev. Food Sci. Nutr. 2010;50(2):113–119. doi: 10.1080/10408390903467514. [DOI] [PubMed] [Google Scholar]
- 15.Adolphus K., Lawton C.L., Dye L. The effects of breakfast on behavior and academic performance in children and adolescents. Front. Hum. Neurosci. 2013;7(August):425. doi: 10.3389/fnhum.2013.00425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoyland A., Dye L., Lawton C.L. A systematic review of the effect of breakfast on the cognitive performance of children and adolescents. Nutr. Res. Rev. 2009 doi: 10.1017/S0954422409990175. [DOI] [PubMed] [Google Scholar]
- 17.Basch C.E. Breakfast and the achievement gap among. J. Sch. Health. 2011;81(10):635–640. doi: 10.1111/j.1746-1561.2011.00638.x. [DOI] [PubMed] [Google Scholar]
- 18.Provasnik S., KewalRamani A., Coleman M.M., Gilbertson L., Herring W., Xie Q. Status of education in Rural America. NCES 2007-040. Natl. Cent. Educ. Stat. 2007:103. http://eric.ed.gov/?id=ED497509 [Google Scholar]
- 19.Johnson J., 3rd, Johnson A. Urban-rural differences in childhood and adolescent obesity in the United States: a systematic review and meta-analysis. Child. Obes. 2015;11(3):1–9. doi: 10.1089/chi.2014.0085. [DOI] [PubMed] [Google Scholar]
- 20.Nanney M.S., Davey C.S., Kubik M.Y. Rural disparities in the distribution of policies that support healthy eating in US secondary schools. J. Acad. Nutr. Diet. 2013;113(8):1062–1068. doi: 10.1016/j.jand.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Graves A., Haughton B., Jahns L., Fitzhugh E., Jones S.J. Biscuits, sausage, gravy, milk, and orange juice: school breakfast environment in 4 rural appalachian schools: research article. J. Sch. Health. 2008;78(4):197–202. doi: 10.1111/j.1746-1561.2008.00286.x. [DOI] [PubMed] [Google Scholar]
- 22.Schetzina K.E., Dalton W.T., Lowe E.F. Developing a coordinated school health approach to child obesity prevention in rural Appalachia: results of focus groups with teachers, parents, and students. Rural. Remote Health. 2009;9(4):1157. 1157 [pii] [PubMed] [Google Scholar]
- 23.Nollen N.L., Befort C., Davis A.M. Competitive foods in schools: availability and purchasing in predominately rural small and large high schools. J. Am. Diet. Assoc. 2009;109(5):857–864. doi: 10.1016/j.jada.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koplan J.P., Liverman C.T., Kraak V.I. Preventing childhood obesity: health in the balance: executive summary. J. Am. Diet. Assoc. 2005;105(1):131–138. doi: 10.1016/j.jada.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 25.Briefel R.R., Crepinsek M.K., Cabili C., Wilson A., Gleason P.M. School Food Environments and Practices Affect Dietary Behaviors of US Public School Children. J. Am. Diet. Assoc. 2009;109(2):S91–S107. doi: 10.1016/j.jada.2008.10.059. [DOI] [PubMed] [Google Scholar]
- 26.Story M., Kaphingst K.M., Robinson-O'Brien R., Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu. Rev. Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 27.McLeroy K.R., Bibeau D., Steckler A., Glanz K. An ecological perspective on health promotion programs. Health Educ. Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 28.Ajzen I. The theory of planned behavior. Organ Behav. Hum. Decis. Process. 1991;50(2):179–211. [Google Scholar]
- 29.Montaño D., Kasprzyk D. Health Behaviour and Health Education. Theory, Research, and Practice. 2008. Theory of reasoned action, theory of planned behaviour, and the integrated behavioral model; pp. 67–96. [Google Scholar]
- 30.Bogenschneider K. An ecological risk/protective theory for building prevention programs, policies, and community capacity to support youth. Fam. Relat. 1996;45(2):127–138. [Google Scholar]
- 31.Stanton C.A., Green S.L., Fries E.A. Diet-specific social support among rural adolescents. J. Nutr. Educ. Behav. 2007;39(4):214–218. doi: 10.1016/j.jneb.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berge J.M., Wall M., Larson N., Loth K. a., Neumark-Sztainer D. Family functioning: associations with weight status, eating behaviors, and physical activity in adolescents. J. Adolesc. Health. 2013;52(3):351–357. doi: 10.1016/j.jadohealth.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nanney M.S., Glatt C. Exploring implementation of the 2010 Institute of Medicine's Child and Adult Food Care Program recommendations for after-school snacks. Public Health Nutr. 2011:1–7. doi: 10.1017/S1368980011002722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Haesly B., Nanney M.S., Coulter S., Fong S., Pratt R.J. Impact on staff of improving access to the school breakfast program: A qualitative study. J. Sch. Health. 2014;84(4):267–274. doi: 10.1111/josh.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nanney M.S., Olaleye T.M., Wang Q., Motyka E., Klund-Schubert J. A pilot study to expand the school breakfast program in one middle school. Transl. Behav. Med. 2011;1(3):436–442. doi: 10.1007/s13142-011-0068-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nanney M., Olaleye T., Wang Q., Motyka E., Klund-Schubert J. Improving Middle School Breakfast Participation through Policy, Environment and Marketing Strategies. Society for Behavioral Medicine Annual Conference; Washington DC: 2011. [Google Scholar]
- 37.School Nutrition Association. Growing School Breakfast Participation: New Ways to Deliver Breakfast to Students on-the-Go.
- 38.USDA Food and Nutrition Services . 2013. Expanding Your School Breakfast Program. Washington, DC.http://www.fns.usda.gov/cnd/breakfast/expansion/default.htm [Google Scholar]
- 39.Rainville AJ, Carr DH. Best Practice Guide for In-classroom Breakfast.
- 40.Himes J.H., Dietz W.H. Guidelines for overweight in adolescent preventive services: recommendations from an expert committee. The Expert Committee on Clinical Guidelines for Overweight in Adolescent Preventive Services. Am. J. Clin. Nutr. 1994;59(2):307–316. doi: 10.1093/ajcn/59.2.307. [DOI] [PubMed] [Google Scholar]
- 41.Sung R.Y., Lau P., Yu C.W., Lam P.K., Nelson E.A. Measurement of body fat using leg to leg bioimpedance. Arch. Dis. Child. 2001;85(3):263–267. doi: 10.1136/adc.85.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tyrrell V.J., Richards G., Hofman P., Gillies G.F., Robinson E., Cutfield W.S. Foot-to-foot bioelectrical impedance analysis: a valuable tool for the measurement of body composition in children. Int. J. Obes. Relat. Metab. Disord. 2001;25(2):273–278. doi: 10.1038/sj.ijo.0801531. [DOI] [PubMed] [Google Scholar]
- 43.Lytle L.A., Murray D.M., Perry C.L. 2004. School-based Approaches to Affect Adolescents' Diets: Results from the TEENS Study. [DOI] [PubMed] [Google Scholar]
- 44.Tran K.M., Johnson R.K., Soultanakis R.P., Matthews D.E. In-person vs telephone-administered multiple-pass 24-hour recalls in women: validation with doubly labeled water. J. Am. Diet. Assoc. 2000;100(7):777–783. doi: 10.1016/S0002-8223(00)00227-3. [DOI] [PubMed] [Google Scholar]
- 45.Johnson R.K., Driscoll P., Goran M.I. Comparison of multiple-pass 24-hour recall estimates of energy intake with total energy expenditure determined by the doubly labeled water method in young children. J. Am. Diet. Assoc. 1996;96(11):1140–1144. doi: 10.1016/S0002-8223(96)00293-3. [DOI] [PubMed] [Google Scholar]
- 46.Guenther P.M., Casavale K.O., Reedy J. Update of the Healthy Eating Index: HEI-2010. J. Acad. Nutr. Diet. 2013;113(4):569–580. doi: 10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reddan J., Wahlstrom K., Reicks M. Children's perceived benefits and barriers in relation to eating breakfast in schools with or without Universal School Breakfast. J. Nutr. Educ. Behav. 1997;34(1):47–52. doi: 10.1016/s1499-4046(06)60226-1. [DOI] [PubMed] [Google Scholar]
- 48.Moser R.P., Green V., Weber D., Doyle C. Psychosocial correlates of fruit and vegetable consumption among African American men. J. Nutr. Educ. Behav. 2005;37(6):306–314. doi: 10.1016/s1499-4046(06)60161-9. [DOI] [PubMed] [Google Scholar]
- 49.Connell C.L., Nord M., Lofton K.L., Yadrick K. Food security of older children can be assessed using a standardized survey instrument. J. Nutr. 2004;134(10):2566–2572. doi: 10.1093/jn/134.10.2566. [DOI] [PubMed] [Google Scholar]
- 50.Kubik M.Y., Davey C., Fulkerson J.A., Sirard J., Story M., Arcan C. Alternative high school students: Prevalence and correlates of overweight. Am. J. Health Behav. 2009;33(5):600–609. doi: 10.5993/ajhb.33.5.13. [DOI] [PubMed] [Google Scholar]
- 51.Fulkerson J.A., Loth K., Bruening M., Berge J.M., Eisenberg M.E., Neumark-Sztainer D. Time 2 tlk 2nite: youths' use of electronic media during family meals and associations with demographic characteristics, family characteristics and foods served. J. Acad. Nutr. Diet. 2014;114(7):1053–1058. doi: 10.1016/j.jand.2013.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anfinson A., Measurement R., Learners H., Kinney A. 2010. 2010 Minnesota Student Survey County Tables. [Google Scholar]
- 53.Rosner B., Grove D. Use of the Mann-Whitney U-test for clustered data. Stat. Med. 1999;18(11):1387–1400. doi: 10.1002/(sici)1097-0258(19990615)18:11<1387::aid-sim126>3.0.co;2-v. 11<1387::AID-SIM126>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 54.Jung S.-H., Kang S.-H., Ahn C. Chi-square test for R x C contingency tables with clustered data. J. Biopharm. Stat. 2003;13(2):241–251. doi: 10.1081/BIP-120019269. [DOI] [PubMed] [Google Scholar]
- 55.Kehm B., Davey C., MS N., Kubik M. A comparison of the vending environment between among rural subtypes of secondary schools: town/rural fringe, town/rural distant, and remote rural. J. Hunger Environ. Nutr. 2015 doi: 10.1080/19320248.2015.1095147. (accepted 7/23/15) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sandve A. Univ Minnesota Teach Educ; 2013. UMN Extension Announces Restructuring of Statewide Nutrition Education Program.http://discover.umn.edu/news/teaching-education/umn-extension-announces-restructuring-statewide-nutrition-education-program (accessed 27.05.15) [Google Scholar]
- 57.Brown A.W., Brown M.M.B., Allison D.B. Belief beyond the evidence: using the proposed effect of breakfast on obesity to show 2 practices that distort scientific evidence. Am. J. Clin. Nutr. 2013;98(5):1298–1308. doi: 10.3945/ajcn.113.064410. [DOI] [PMC free article] [PubMed] [Google Scholar]