Abstract
Background
The database of the German Institute of Medical Documentation and Information makes it possible for the first time to compute statistics on diabetes for all insurees of the statutory health insurance scheme in Germany. Data from this comprehensive source are less likely to be biased by differences in the membership structures of individual insurance carriers or by the underrepresentation of persons over age 80 that is seen in most population-based studies.
Methods
International Classification of Diseases (ICD)–coded diagnosis data from the inpatient and outpatient sectors were used to define persons as having diabetes. Incidences were estimated from differences in prevalence from one year to the next and the expected mortality of persons with and without diabetes.
Results
A diabetes diagnosis was present in 6.4 million out of a total of 65.6 million insurees in 2009 and in 6.7 million out of 64.9 million insures in 2010. The corresponding age and sex standardized prevalences of diabetes were 9.7% in 2009 and 9.9% in 2010, respectively. The number of persons with type 2 diabetes was 4.6 million in 2009 and 4.7 million in 2010. The prevalence and incidence of type 2 diabetes rose steeply from age 50 to age 80. Peak incidence was at age 85, with 24 newly diagnosed cases of diabetes per 1000 person-years.
Conclusion
On the basis of these data, we estimate that 5.8 million persons with type 2 diabetes are living in Germany today. The database used in this study is a valuable complement to population-based studies for monitoring the prevalence of diabetes, particularly in persons over age 80.
The German Institute of Medical Documentation and Information (DIMDI, Deutsches Institut für Medizinische Dokumentation und Information) was commissioned through the Data Transparency Regulation of 2012 to collect and process data from different areas of routine health care (1). This new data set provides comprehensive routine data from German statutory health insurance funds for the first time. In the case of type 2 diabetes it is known that the prevalence varies among policyholders from different insurance companies. The nationwide, population-based German National Health Interview and Examination Survey for Adults (DEGS1, Studie zur Gesundheit Erwachsener in Deutschland) of the Robert Koch-Institute (RKI) estimated the overall prevalence of type 2 diabetes in the whole population between 18 and 79 years of age at a total of 7.4%, made up of 9.0% for policyholders of the AOK (a large general statutory health insurance fund) and 7.0% for policyholders of substitute health insurance funds (2). Older population groups over 80 years of age and individuals who are in nursing homes or hospitals at the time of investigation, however, are underrepresented in epidemiological studies, with the result that projections for the total population are inaccurate. In fact, according to the census of 2011, around 4.2 million people in Germany were over 80 years of age (3). Routine data, therefore, often provide the only way of depicting the situation of older and hospitalized population groups. By including data from multiple insurance companies as well as in people over 80, the DIMDI data set closes an important data gap for Germany by facilitating more comprehensive estimates of the prevalence of type 2 diabetes. The prevalence of type 1 diabetes can also be determined on the basis of the data provided by DIMDI. Thus, this data set complements registry data from Baden–Württemberg, North Rhine–Westphalia and Saxony, which are limited to children and young adults (1, 4).
The present study not only calculates the overall prevalence and incidence of diagnosed diabetes mellitus in Germany with a particular focus on type 2 diabetes, but also the age and sex specific prevalence and incidence including the age group of those over 80.
Methods
Information system, medical care data (DIMDI data set)
The Statutory Health Insurance Healthcare Provision Act (GKV-VStG, GKV-Versorgungsstrukturgesetz) passed on 22 December 2011 revised data transparency regulations (§§ 303a et seq. Code of Social Law V; SGB, Sozialgesetzbuch). With the data transparency regulation (Datentransparenzverordnung) issued on 10 September 2012 (Federal Law Gazette I p. 1895), DIMDI was finally commissioned to implement the regulations governing data transparency. The routine health insurance data on morbidity-related risk stratification reimbursement (Morbi-RSA, Morbiditäts-Risikostrukturausgleich) now flow into the information system of medical care data of DIMDI. These data are collected by the Federal Social Insurance Authority (BVA, Bundesversicherungsamt) and are passed on to DIMDI (2). Controls for the completeness and plausibility of the data are regulated in § 273 and § 268, paragraph 3, sentences 1, 2 and 14 SGB V and guaranteed by the BVA. DIMDI provides aggregated data in accordance with strict data protection regulations (5). This study analyzed diagnostic data from the ambulatory and hospital sector and reimbursements in 2010 and 2011 (report year), and included all policyholders who were insured for at least 360 days per year by one of the statutory health insurance funds (GKV). Using this criterion, policyholders who died, moved abroad, or changed to or from a private insurance fund during the report year, for example, were not included in the analysis (6). The dataset includes information from the four quarterly periods of the respective previous years (2009 and 2010). Overall, this study was able to analyze diagnostic data from approximately 80% of Germany’s resident population: The study included data of 65.6 million patients who were insured with a statutory health insurance fund for all four quarters of 2009, and data of 64.9 million insured patients respectively in 2010 (7, 8).
Definition of diabetes
The International Classification of Diseases (ICD) codes E10.0 to E14.0 were used to define type 2 diabetes:
E10.- Type 1 diabetes mellitus
E11.- Type 2 diabetes mellitus
E12.- Malnutrition related diabetes mellitus
E13.- Other specified diabetes mellitus, for example diabetes related to pancreatic insufficiency
E14.- Unspecified diabetes mellitus.
For data originating in the outpatient area, the additional ICD-tag “G” for a confirmed diagnosis was required in order to increase the diagnostic validity. An additional tag is obligatory in the out-patient area (9).
Multiple diagnoses (double diagnoses) could occur, due to the fact that different care providers such as primary care physicians, clinicians or experts assessing eligibility for welfare benefits made multiple diagnoses during the course of the four quarterly periods of the report year in some cases. The handling of double diagnoses will be explained in the eBox. All year-round policyholders were collectively assigned to one of the following six groups:
eBox. Method of incidence estimation.
The incidence was calculated using a differential equation in which the age and sex specific estimations of the prevalence as well as of the relative risk of mortality for the population with and without diabetes were taken into account (24).
i = (∂/ ∂ t + ∂/ ∂ a)p + m × PAR
where PAR = p(R-1)/[pR + (1-p)]
In the above equation, the incidence (i) is modelled from the time- (t) and age (a) dependent change of prevalence (∂/ ∂ t + ∂/ ∂a) p, the mortality (m) and the population attributable risk (PAR). The PAR can in turn be computed from the prevalence (p) and the ratio of mortality rates (R) for individuals with diabetes in comparison to those without.
This method has already been compared to further methods of incidence estimation, for example to the integrated hazard function and the person-year Method (25). It became apparent that the different methods compared well when the number of cases was high (N = 100 000). The method used in this study is therefore also suitable for narrowly defined age groups (for example one-year-groups like in Table 1), when the sample is big as in the case of the DIMDI dataset.
Handling of multiple diagnoses (double diagnoses): definition of type 1 and type 2 diabetes as well as further diagnoses of diabetes
Unspecified diabetes mellitus E14.- was frequently diagnosed in combination with type 2 diabetes mellitus (E11.-). E14.- diagnoses were defined as type 2 diabetes mellitus, if E11.- diagnoses were made as well in the remaining quarterly periods. The combination of the codes E14.- and E10.- resulted in the definition of type 1 diabetes. Double diagnoses from the areas E10.- and E11.- (type 1 and type 2 diabetes mellitus) also occurred. Incorrect processes at various points of data acquisition (for example at the point of data transfer or directly during data entry into medical software) as well as changes of diagnosis after more precise specification may be responsible for this. Since the majority of these double diagnoses of type 1 and type 2 diabetes mellitus probably refer to cases of type 2 diabetes, the frequency of these unclear diagnoses was assessed using sensitivity analyses or both diagnoses were integrated in the overall diagnosis of diabetes mellitus.
No diabetes: no diagnosis E10.- to E14.-
Type 2 diabetes mellitus: diagnosis ICD E11.- or (double diagnosis E11.- and E14.-)
Type 1 diabetes mellitus: diagnosis ICD E10.- or (double diagnosis E10.- and E14.-)
Unspecified diabetes: only diagnosis ICD E14.-
Unclear diabetes: double diagnosis E10.- and E11.-
Other diabetes: ICD E12.- or E13.-.
Gestational diabetes was left unconsidered (ICD O24.-).
Statistical analysis
Overall prevalence and corresponding confidence intervals were calculated for the entire sample of 2009 and 2010 respectively and standardized according to age and sex for the German population (status 31 December 2007). Incidence is commonly estimated using longitudinal studies of individuals. Since the prevalence of an illness or disease is a function of incidence and mortality, it is possible to estimate the incidence in cross-sectional studies, if—as in this case—the prevalence is known at two points in time and the mortality is known in the populations with and without disease (10). A more detailed description of the method of estimating the incidence can be found in the eBox.
The disease-specific mortality data of individuals with and without diabetes are not available in Germany; therefore estimates for the Danish population had to be used (11). Three different scenarios were chosen for the estimation of incidence: (a) the ratio of mortality rates in Germany more or less corresponds to the rates in Denmark, or (b) lies within a 15% range above or (c) below the values determined for Denmark (12, 13). The annual estimates of the mortality in Europe carried out by the World Health Organization (WHO) in both countries indicate a slightly lower (around 7%) age-standardized, overall and diabetes-related mortality in Germany for 2009 to 2012. This indicates a high degree of comparability of the ratio of mortality rates in both countries (13).
The calculated confidence intervals are only shown in Table 1 and 2, because they turned out very small due to the high number of cases of approximately 65 million policyholders. All analyses were conducted using the statistic software R, version 3.0.1 (The R Foundation of Scientific Computing).
Table 1. Prevalence (95%-confidence intervals) and incidence of type 2 diabetes for male and female policyholders of German statutory health insurance funds over 40 years of age (2009, 2010)*.
| Prevalence (%) | Incidence/1000 py | |||||
|---|---|---|---|---|---|---|
| Age group | 2009 | 2010 | Age | R | R–15’% | R+15’% |
| Men | ||||||
| 40–49 years | 1.5 [1.5; 1.6] |
1.6 [1.6; 1.7] |
45 years | 4 | 4 | 4 |
| 50–59 years | 5.5 [5.4; 5.5] |
5.7 [5.6; 5.7] |
55 years | 9 | 9 | 9 |
| 60–69 years | 14.0 [14.0; 14.1] |
14.5 [14.4; 14.5] |
65 years | 18 | 18 | 19 |
| 70–79 years | 21.1 [21.1; 21.2] |
21.9 [21.8; 21.9] |
75 years | 24 | 23 | 26 |
| 80–89 years | 25.1 [25.0; 25.2] |
26.3 [26.2; 26.4] |
85 years | 29 | 25 | 32 |
| 90–99 years | 23.4 [23.1; 23.6] |
24.1 [23.9; 24.4] |
95 years | 26 | 17 | 33 |
| ≥ 100 years | 17.4 [15.3; 19.6] |
16.5 [14.4; 18.6] |
105 years | 17 | 3 | 31 |
| Over 40 years | 7.03 [7.02; 7.04] |
7.41 [7.40; 7.42] |
Over 40 years | 16 | 15 | 17 |
| Women | ||||||
| 40–49 years | 1.2 [1.2; 1.2] |
1.3 [1.3; 1.3] |
45 years | 2 | 2 | 2 |
| 50–59 years | 3.4 [3.4; 3.5] |
3.6 [3.5; 3.6] |
55 years | 6 | 6 | 6 |
| 60–69 years | 9.7 [9.6; 9.7] |
10.0 [10.0; 10.1] |
65 years | 13 | 13 | 13 |
| 70–79 years | 16.5 [16.4; 16.5] |
16.9 [16.9; 17.0] |
75 years | 19 | 19 | 20 |
| 80–89 years | 23.2 [23.1; 23.2] |
24.0 [24.0; 24.1] |
85 years | 24 | 22 | 26 |
| 90–99 years | 24.4 [24.3; 24.5] |
24.9 [24.8; 25.0] |
95 years | 21 | 15 | 27 |
| ≥ 100 years | 17.0 [16.2; 17.7] |
17.7 [17.0; 18.5] |
105 years | 14 | 1 | 27 |
| Over 40 years | 6.65 [6.64; 6.66] |
6.97 [6.97; 6.98] |
Over 40 years | 13 | 12 | 14 |
*The prevalence has been calculated for age groups of 10 years. The estimation of the incidence refers to the mean age of the respective age group.
Py, person-years; R, incidence estimations based on the Danish ratio of mortality risk (individuals with and without diabetes); R±15%, mortality risk ratio 15% above respectively under the Danish estimates
Results
Diabetes (E10.- to E14.-) was diagnosed in a total of 6.4 of 65.6 million policyholders from statutory health insurance funds (from the age of 0 up) in 2009. This corresponds to a prevalence of 9.8%. In 2010 the disease affected 6.7 of the 64.9 million policyholders, representing 10.1%. Following standardization for the German population (31. December 2007), the total prevalence of diabetes was calculated to be 9.7% (2009) and 9.9% (2010) respectively. Type 1 diabetes accounted for 0.3% in both years, and the remaining diagnoses, i.e. of other as well as unclear diabetes, accounted for 2.5%. In 2009, 6.9% of policyholders from statutory health insurance funds were diagnosed with type 2 diabetes; 2010 it was 7.3%. After standardization, prevalences of 6.9% (2009) and 7.1% (2010) were derived.
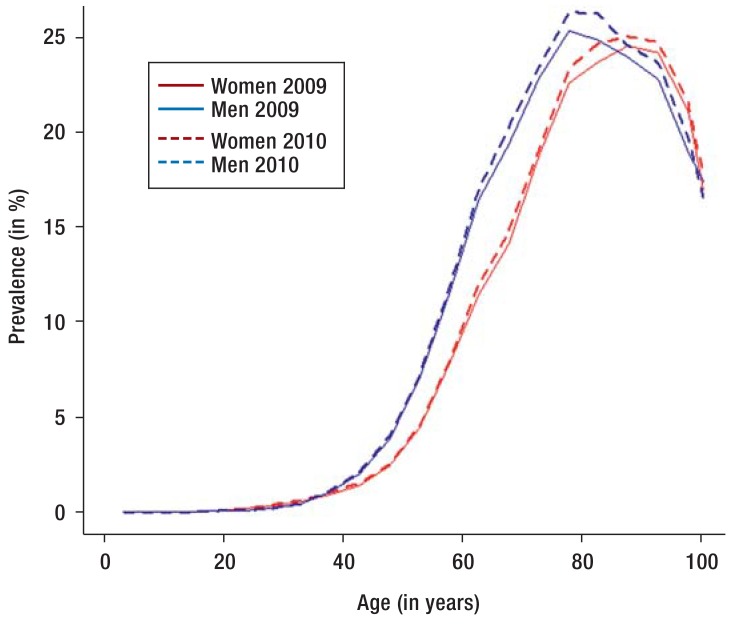
The Figure shows that the prevalence of type 2 diabetes increased markedly in both years of investigation starting approximately at the age of 50. The prevalence reached its peak at around 25% at age 80, among policyholders from statutory health insurance funds. The prevalence of type 2 diabetes was significantly higher for men than for women between the ages of 40 and 80 (Figure). In the over 80-year-olds, the prevalence for both sexes remained approximately equal and decreased after the age of 100 to 16.5% and 17.7% respectively (Figure).
Figure.
Prevalence of type 2 diabetes in female and male policyholders of statutory health insurance funds in Germany in 2009 and 2010
A slight increase of the prevalence of type 2 diabetes in comparison to the previous year was found for women (from 6.8% to 7.1%) and men (7.1% to 7.5%). This could be observed as a trend in all age groups (Table 1, Figure). The prevalence increased for women in the older age groups from 70 years on by 0.4–0.8% (Table 1).
For policyholders over 40, i.e. in the age groups with an increased risk of diabetes, the incidence of type 2 diabetes was derived from the prevalence and mortality. It became apparent that the incidence for men was higher than that for women in all age groups (Table 1). Between the ages of 50 and 89, women had an incidence rate which corresponded approximately to the one of men 10 years younger. The highest incidence for both sexes was between the ages of 80 and 99 (Table 1). The total incidence above 40 years only varied slightly between the three scenarios of the ratio of mortality rates.
The estimates of the prevalence of type 2 diabetes were initially made using a conservative approach in order to describe cases of diabetes that could be verified as well as possible. When unclear diagnoses of diabetes are included, however, the prevalence of type 2 diabetes is considerably higher. Additional cases of type 2 diabetes may, for example, be masked by the diagnosis of unspecified diabetes (E14.-). Table 2 shows the estimates of prevalence for all diagnostic groups (E10.- to E14.-) in three age groups, each of which is stratified according to sex and the year of observation. The combined diagnosis for type 1 and type 2 diabetes (inconsistent diagnosis) as well as the exclusive diagnosis of unspecified diabetes (E14.-) were particularly common in the age group above 80 years with a prevalence of approximately 3% each. Among the 20 to 79 year olds roughly 2.5% were attributable to each diagnostic group. The ICD-codes E12.- and E13.- (other diabetes) were seldom found in patients under 80. But they constituted roughly 1% for policyholders of statutory health insurance funds from the age of 80 on. Comparing both years, the differences were marginal for other, unclear and unspecified diabetes (E12.- to E14.-) (Table 2).
Table 2. Prevalence (95% confidence intervals) of type 2 and type 1 diabetes as well as unclear diagnosis of diabetes (figures in %)*.
| Age group | 2009 | 2010 | ||
|---|---|---|---|---|
| Men | Women | Men | Women | |
| Type 2 diabetes (only E11.- or double diagnosis E11.- and E14.-) | ||||
| 0–19 years | 0.03 [0.03; 0.03] | 0.04 [0.04; 0.04] | 0.03 [0.03; 0.03] | 0.04 [0.04; 0.04] |
| 20–79 years | 8.31 [8.30; 8.32] | 6.69 [6.68; 6.70] | 8.68 [8.67; 8.69] | 6.99 [6.98; 7.00] |
| ≥ 80 years | 24.39 [24.31; 24.47] | 23.94 [23.89; 23.99] | 25.55 [25.47; 25.63] | 24.68 [24.63; 24.73] |
| Type 1 diabetes (only E10.- or double diagnosis E10. and E14.-) | ||||
| 0–19 years | 0.19 [0.18; 0.19] | 0.17 [0.17; 0.18] | 0.19 [0.19; 0.20] | 0.18 [0.17; 0.18] |
| 20–79 years | 0.39 [0.39; 0.39] | 0.28 [0.28; 0.29] | 0.38 [0.38; 0.38] | 0.28 [0.28; 0.28] |
| ≥ 80 years | 0.47 [0.46; 0.48] | 0.50 [0.49; 0.51] | 0.44 [0.43; 0.45] | 0.43 [0.43; 0.44] |
| Unspecified diabetes (E14.-) | ||||
| 0–19 years | 0.05 [0.05; 0.05] | 0.06 [0.06; 0.06] | 0.05 [0.05; 0.05] | 0.06 [0.06; 0.07] |
| 20–79 years | 1.19 [1.18; 1.19] | 1.02 [1.01; 1.02] | 1.15 [1.15; 1.16] | 1.00 [0.99; 1.00] |
| ≥ 80 years | 3.51 [3.48; 3.55] | 3.55 [3.53; 3.58] | 3.39 [3.36; 3.43] | 3.39 [3.37; 3.42] |
| Other diabetes (E12.- and E13.-) | ||||
| 0–19 years | 0.01 [0.01; 0.01] | 0.01 [0.01; 0.01] | 0.01 [0.01; 0.01] | 0.01 [0.01; 0.01] |
| 20–79 years | 0.42 [0.42; 0.42] | 0.33 [0.33; 0.33] | 0.44 [0.44; 0.44] | 0.35 [0.35; 0.35] |
| ≥ 80 years | 1.09 [1.07; 1.11] | 0.99 [0.98; 1.01] | 1.15 [1.13; 1.17] | 1.04 [1.02; 1.05] |
| Unclear diabetes (double diagnosis E10.- and E11.-) | ||||
| 0–19 years | 0.04 [0.04; 0.04] | 0.04 [0.04; 0.05) | 0.04 [0.04; 0.04] | 0.04 [0.04; 0.04] |
| 20–79 years | 1.45 [1.45; 1.46] | 1.17 [1.16; 1.17] | 1.43 [1.43; 1.44] | 1.14 [1.14; 1.15] |
| ≥ 80 years | 3.46 [3.42; 3.49] | 3.03 [3.01; 3.05] | 3.42 [3.39; 3.46] | 2.92 [2.90; 2.94] |
*Number of policyholders of statutory health insurance funds in million in the age groups 0–19; 20–79; ≥ 80 years: 2009: women 6.1; 26.6; 2.4; men 6.4; 23.1; 1.0; 2010: women 5.9; 26.2; 2.5; men 6.2; 23.0; 1.1.
Definition of diabetes on the basis of the International Classification of Diseases (ICD) codes E10.- to E.14
Discussion
4.6 million of the 65.6 million policyholders (2009) and 4.7 million of the 64.9 million policyholders (2010) from statutory health insurance funds were diagnosed with type 2 diabetes. Hence the age and sex standardized prevalences were 6.9% (2009) and 7.1% (2010) respectively. Projected onto the whole German population in 2010, this equals 5.8 million people with diagnosed type 2 diabetes for the same year. Taking into account all diabetes diagnoses (E10.- to E14.-), the number of affected policyholders of statutory health insurance funds increased to 9.7% (2009) and 9.9% (2010). Projected onto the total German population, up to 8.1 million patients suffered from diabetes mellitus in 2010. Type 2 diabetes was rare under the age of 20, but increased rapidly between the ages of 50 and 79 from 4% to 17% for women and from 6% to 26% for men. Above the age of 80, the number of diagnosed cases stayed consistently high at 24.2% (2009) and 27.7% (2010) respectively. Furthermore, the highest incidence of diabetes was found around the age of 85.
The prevalence of type 2 diabetes in population-based studies
On the basis of type 2 diabetes self-reports obtained from patients, the prevalence of the disease in the population-based DEGS1 study of the Robert Koch Institute (RKI) conducted from 2008 to 2012 was estimated at 7.2% (women 7.4%, men 7.0%) for the age group between 18 and 79 years. The data were comparable in range with those of the study we are presenting here (2). The prevalence of diabetes for male policyholders of statutory health insurance funds between the age of 20 and 70 years was higher than that for women in the same age group (men: 2009: 8.3%; 2010: 8.7%; women: 2009: 6.7%; 2010: 7.0%). These findings differ from the results of the DEGS1, but correspond with data of other population-based studies such as the KORA study, the DIAB-CORE Consortium or the Diabetes Atlas of the International Diabetes Federation (IDF) (14– 18). Since the definition of diabetes in the DEGS1 was based on patient information without precise specification of the type of diabetes, it is possible that cases of gestational diabetes were included in the female population. This type of diabetes was excluded from the analysis of policyholders of statutory health insurance funds being reported here, or other population-based studies (KORA, DIAB-CORE).
Comparison with secondary data—prevalence above 80 years of age
Secondary data based solely on individual or regional health insurance funds are currently the only basis for comparative analyses with respect to patients over the age of 80. Only the Techniker Krankenkasse (TK) provided detailed analyses of age groups. For the policyholders between 80 and 90 years of age, 24% were identified with a type 2 diabetes (19). This result corresponds closely to the DIMDI dataset. The incidence (per 1000 person-years) for policyholders of statutory health insurance funds in all age groups, however, was at least twice as high as the incidence for TK policyholders (19). The differences can probably be explained by differences in the definition of type 2 diabetes as well as by the way multiple diagnoses were dealt with by the TK study. This could have led to an underestimation of the incidence. Across Germany as well as on the level of federal states (Hesse), the total prevalence of 4.7% in TK policyholders was significantly lower than that for policyholders of statutory health insurance funds and of the AOK health insurance company (20, 21). An age and sex standardized overall prevalence of 9.8% of diagnosed diabetes was determined for all AOK-policyholders in 2010 (20). The AOK studies show a close correspondence with the total prevalence of diabetes for policyholders from statutory health insurance funds as well as with the development of the disease with age. This can be said in spite of methodical differences such as the consideration of medication and outpatient diagnoses in three of four quarters (20, 22).
In international comparison, valid prevalence data for diabetes in older patients are only available for a few countries. The prevalence increased markedly up to the age of 70 in the Canadian Chronic Disease Surveillance System of the Public Health Agency of Canada as well as in the European DECODE study. Between the age of 70 and 85 years a peak became apparent with comparable rates of prevalence between 20 and 25% (23).
Limitations and strengths
The data set provided by DIMDI for policyholders of statutory health insurance funds shares the strengths and limitations of all secondary data sets. With around 65 million GKV-policyholders per year, a comprehensive picture of diagnosed diabetes in Germany evolves which includes patients over 80 years of age. On the basis of secondary data (without standardized glucose measurements or glycated hemoglobin values for persons without diagnosed diabetes), however, no statements can be made concerning the unknown number of unrecorded cases, i.e., diabetes that has not been detected or diagnosed. Furthermore, the types of diabetes are de facto defined using inconsistent standards with the result that the specification as well as the time of diagnosis are fraught with inaccuracies. Sensitivity analyses for all diabetes diagnoses were used to assess inaccuracies. Moreover, no statements can be made for individuals who died, moved abroad, or changed to a private insurance fund during the report year. Individuals with diabetes have an increased mortality risk in comparison with individuals without this disease. On the one hand, individuals who died during the report year potentially suffered from type 2 diabetes with disproportional frequency. This could have led to a slight underestimation of the prevalence of diabetes. On the other hand, young, employed and healthy individuals may have changed with disproportional frequency to a private insurer. Thus an overestimation of the prevalence of diabetes cannot be excluded either. Both distorting effects could, however, have canceled each other out.
The Danish mortality data used for the estimation of the incidence should be mentioned as further limitations. On the basis of comparable treatment options for individuals with type 2 diabetes in both neighboring countries, however, it can be assumed that the deviation remains within the mode’s margin for error of ± 15% (13).
Conclusion
At least 5.8 million individuals in Germany have received a medical diagnosis of type 2 diabetes. The incidence of type 2 diabetes between 80 and 89 years of age was the highest ranging at 29 for men and 24 for women respectively per 1000 person-years. Overall every fourth individual in Germany over 80 years of age suffers from type 2 diabetes. More information regarding the extent of necessary medical care, the risk of complications and the mortality of this large group of patients is urgently needed. All in all these DIMDI data may well be suited for the surveillance of diagnosed diabetes.
Key Messages.
Based on routine medical care data, up to 9.9% of policyholders of German statutory health insurance funds were diagnosed with diabetes in 2010.
In comparison with the previous year (2009), there was a slight increase of prevalence in all age groups.
The estimated incidence of type 2 diabetes is highest in the age group around 85 years of age and stands at 24 for women and 26 for men respectively per 1000 person-years.
With a prevalence of around 24% for persons aged 80 years and older, it can be assumed that there are approximately 1 million patients in this age group in Germany who suffer from type 2 diabetes.
Until now there has been little investigation of the need for special medical care, increased risk of complications, or the need for specific screening programs for patients over 80. Further investigation is needed in these areas.
Acknowledgments
Translated from the original German by Gabriel Seifert, MD and Miriam Seifert, MA.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.The DECODE study group. Age- and sex-specific prevalences of diabetes and impaired glucose regulation in 13 European cohorts. Diabetes Care. 2003;26:61–69. doi: 10.2337/diacare.26.1.61. [DOI] [PubMed] [Google Scholar]
- 2.Deutsches Institut für Medizinische Dokumentation und Information (DIMDI) Aktuell Informationssystem Versorgungsdaten. www.dimdi.de/static/de/versorgungsdaten/aktuelles/news_0364.html_319159480.html. (last accessed on 11 August 2015)
- 3.Heidemann C, Du Y, Schubert I, Rathmann W, Scheidt-Nave C. Prävalenz und zeitliche Entwicklung des bekannten Diabetes mellitus. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2013;56:668–677. doi: 10.1007/s00103-012-1662-5. [DOI] [PubMed] [Google Scholar]
- 4.Ehehalt S, Dietz K, Willasch AM, Neu A Baden-Württemberg Diabetes Incidence Registry (DIARY) Group. Epidemiological perspectives on type 1 diabetes in childhood and adolescence in Germany: 20 years of the Baden-Württemberg Diabetes Incidence Registry (DIARY) Diabetes Care. 2010;33:338–340. doi: 10.2337/dc09-1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deutsches Institut für Medizinische Dokumentation und Information (DIMDI) Beispieldatensatz. www.dimdi.de/static/de/versorgungsdaten/datensatzbeschreibung/beispieldatensatz.htm. (last accessed on 11 August 2015) [PubMed]
- 6.Deutsches Institut für Medizinische Dokumentation und Information (DIMDI) FAQ-Center Versorgungsdaten. www.dimdi.de/static/de/versorgungsdaten/faq/faq_0013.html. (last accessed on 30 April 2015)
- 7.Bendas A, Rothe U, Kiess W, et al. Trends in incidence rates during 1999-2008 and prevalence in 2008 of childhood type 1 diabetes mellitus in Germany—model-based national estimates. PLoS One. 2015;10 doi: 10.1371/journal.pone.0132716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bundesministerium für Gesundheit. Gesetzliche Krankenversicherung. Stand Januar 2015. www.bmg.bund.de/fileadmin/dateien/Downloads/Statistiken/GKV/Kennzahlen_Daten/KF2015Bund_Januar_2015.pdf. (last accessed on 30 April 2015)
- 9.Deutsches Institut für Medizinische Dokumentation und Information (DIMDI) FAQ-Center Klassifikationen: ICD-10. www.dimdi.de/static/de/klassi/faq/icd-10/icd-10-gm/faq_1010.htm_319159480.htm. (last accessed on 11 August 2015)
- 10.Brinks R, Landwehr S. A new relation between prevalence and incidence of a chronic disease. Math Med Biol. 2015 doi: 10.1093/imammb/dqu024. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carstensen B, Kristensen JK, Ottosen P, Borch-Johnsen K. Steering Group of the National Diabetes Register. The Danish National Diabetes Register: trends in incidence, prevalence and mortality. Diabetologia. 2008;51:2187–2196. doi: 10.1007/s00125-008-1156-z. [DOI] [PubMed] [Google Scholar]
- 12.Plass D, Vos T, Hornberg C, Scheidt-Nave C, Zeeb H, Krämer A. Trends in disease burden in Germany—results, implications and limitations of the Global Burden of Disease Study. Dtsch Arztebl Int. 2014;111:629–638. doi: 10.3238/arztebl.2014.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization (WHO) data.euro.who.int/dmdb/ European detailed mortality database. (last accessed on 11 August 2015) [Google Scholar]
- 14.Rathmann W, Haastert B, Icks A, et al. High prevalence of undiagnosed diabetes mellitus in Southern Germany: target populations for efficient screening. The KORA survey. 2000. Diabetologia. 2003;46:182–189. doi: 10.1007/s00125-002-1025-0. [DOI] [PubMed] [Google Scholar]
- 15.Meisinger C, Strassburger K, Heier M, et al. Prevalence of undiagnosed diabetes and impaired glucose regulation in 35-59-year-old individuals in Southern Germany: the KORA F4 Study. Diabet Med. 2010;27:360–362. doi: 10.1111/j.1464-5491.2009.02905.x. [DOI] [PubMed] [Google Scholar]
- 16.Schipf S, Werner A, Tamayo T, et al. Regional differences in the prevalence of known type 2 diabetes mellitus in 45-74 years old individuals: results from six population-based studies in Germany (DIAB-CORE Consortium) Diabet Med. 2012;29:e88–e95. doi: 10.1111/j.1464-5491.2012.03578.x. [DOI] [PubMed] [Google Scholar]
- 17.Schipf S, Ittermann T, Tamayo T, et al. Regional differences in the incidence of self-reported type 2 diabetes in Germany: results from five population-based studies in Germany (DIAB-CORE Consortium) J Epidemiol Community Health. 2014;68:1088–1095. doi: 10.1136/jech-2014-203998. [DOI] [PubMed] [Google Scholar]
- 18.Tamayo T, Rosenbauer J, Wild SH, et al. Diabetes in Europe: an update. Diabetes Res Clin Pract. 2014;103:206–217. doi: 10.1016/j.diabres.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 19.Wilke T, Ahrendt P, Schwartz D, Linder R, Ahrens S, Verheyen F. [Incidence and prevalence of type 2 diabetes mellitus in Germany: an analysis based on 54.3 million patients] Dtsch Med Wochenschr. 2013;138:69–75. doi: 10.1055/s-0032-1327394. [DOI] [PubMed] [Google Scholar]
- 20.Müller N, Heller T, Freitag MH, et al. Healthcare utilization of people with type 2 diabetes in Germany: an analysis based on health insurance data. Diabet Med. 2015;32:951–957. doi: 10.1111/dme.12747. [DOI] [PubMed] [Google Scholar]
- 21.Köster I, Schubert I, Huppertz E. [Follow up of the CoDiM-Study: cost of diabetes mellitus 2000-2009] Dtsch med Wochenschr. 2012;137:1013–1016. doi: 10.1055/s-0032-1304891. [DOI] [PubMed] [Google Scholar]
- 22.Hauner H, Köster I, Schubert I. Prevalence of diabetes mellitus and quality of care in Hesse, Germany, 1998-2004. Dtsch Arztebl. 2007;104:A 2799–A 2805. [Google Scholar]
- 23.Public Health Agency of Canada Diabetes in Canada. www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/pdf/facts-figures-faits-chiffres-eng.pdf. Ottawa: Chapter 1—The burden of diabetes in Canada; 2011. Facts and figures from a public health perspective. (last accessed on 11 August 2015) [Google Scholar]
- 24.Statistisches Bundesamt. www.destatis.de/DE/ZahlenFakten/GesellschaftStaat/Bevoelkerung/Sterbefaelle/AktuellPeriodensterbetafeln.html. (last accessed on 11 August 2015)
- 25.Brinks R, Landwehr S, Icks A, Koch M, Giani G. Deriving age-specific incidence from prevalence with an ordinary differential equation. Statistics in Medicine. 2013;32:2070–2078. doi: 10.1002/sim.5651. [DOI] [PubMed] [Google Scholar]