Abstract
Background
10–20% of children and adolescents have a mental health problem of some type. Manifestations such as attention deficits, cognitive disturbances, lack of motivation, and negative mood all adversely affect scholastic development. It is often unclear what factors associated with school affect children’s mental development and what preventive measures and interventions at school might be effective.
Methods
This review is based on systematic reviews, meta-analyses, and randomized and non-randomized controlled trials that were retrieved by a selective search in the PubMed, PsycInfo, and Google Scholar databases.
Results
The prevalence of hyperkinetic disorder is 1–6%. Its main manifestations are motor hyperactivity, an attention deficit, and impulsive behavior. Learning disorders such as dyscalculia and dyslexia affect 4–6% of children each, while 4–5% of children and adolescents suffer from depression, which is twice as prevalent in girls as in boys. Mental health problems increase the risk of repeating a grade, truancy, and dropping out of school. The risk of developing an internalizing or externalizing mental health problem can be lessened by changes in the school environment and by the implementation of evidence-based school programs.
Conclusion
Physicians, in collaboration with school social workers and psychologists, should help teachers recognize and contend with mental health problems among the children and adolescents whom they teach, to enable the timely detection of stress factors at school and the initiation of the necessary measures and aids. In particular, the school-entrance examination and screening for risk factors at school can make a positive contribution. Evidence-based preventive programs should be implemented in schools, and beneficial changes of the school environment should be a further goal.
The global prevalence of mental health problems affecting children and adolescents is 10–20% (1). According to the German Health Interview and Examination Survey for Children and Adolescents (KiGGS), the prevalence of mental health problems in Germany is stable and high, at 10% (2). These problems include anxiety disorders, depression, conduct disorders, and hyperkinetic disorder. However, only about one-third of acutely and chronically mentally ill children and adolescents are receiving medical treatment. The low uptake of healthcare services by mentally ill children and their families is a problem that is known internationally (3). The reasons are manifold:
Specialist healthcare is not sufficiently accessible
Fear of having a mental disorder and being stigmatized
Uncertainty among children and parents about whether the behavioral or mood changes actually require treatment
Little or no awareness of available healthcare services
Language barriers or cultural obstacles in families from a migration background.
One of the tasks of schools is to support children’s mentally healthy development while growing up (3), as school is where children and adolescents spend a large part of their time (4)—combined with social experiences and challenges, learning demands and mental overload, and psychological stress. On the basis that 11.1 million children and adolescents attended general and vocational schools in Germany in 2014/15 and that the prevalence of mental health problems is 10% (5), some 1.1 million of school-age children and adolescents have mental health problems requiring treatment.
To date in human medicine, it remains unknown which school-related factors increase the risk for developing mental health problems and which factors are protective and help children and adolescents grow up mentally healthy. The fundamental question that arises is how medicine and pedagogy can work together more closely in order to lower the risk of developing mental health problems and to look after and provide treatment for mentally ill children and adolescents from a holistic perspective. In view of the high rates of mental health problems, using preventive methods in school to reduce the risk of developing mental illness or its recurrence is an interdisciplinary challenge that cannot be met by using methods of pedagogy alone.
This review article aims to explain factors in the school setting that affect mental health and the importance of mental health problems for students’ school development. On the basis of a selective review we will review examples of empirical findings in common mental health problems (hyperkinetic disorder, specific developmental disorders of scholastic skills, depression) that show the association of school-related factors and mental health problems. Furthermore, we will explain the options of diagnostic evaluation, prevention, and intervention in the school setting. Our review is based on—where available— systematic reviews, meta-analyses, randomized controlled trials, and controlled trials. We searched the databases PubMed, PsycINFO, and Google Scholar for the time period 1990–2015. The search terms covered the specialisms of mental health and mental illness (depression, dyslexia, dyscalculia, disorder of arithmetic skills, hyperkinetic disorder, and attention deficit-hyperactivity disorder), school-related factors, prevention, support, treatment, and children and adolescents.
Hyperkinetic disorder
Hyperkinetic disorder (HKD) (6) is one of the most common mental health problems, with a prevalence of 1–6% (7, 8). The key symptoms include pronounced hyperactivity, attention deficit disorder, and increased impulsivity. Children with HKD are easily distracted, jump up in class, shout out into the classroom, are able to focus their attention for a short timespan only, miss important information in class, disrupt their fellow students, drop class materials, or topple over with their chairs. The basic school requirement of being able to adhere to structured behavior over several hours and to focus their attention is asking too much from children with HKD. Teachers experience and describe hyperkinetic behavior as disruptive and stressful. Children with HKD suffer greatly when they notice that they are “different” and not able to control their behavior. They are teased by their fellow students and get into rows. If the symptoms persist, such children often become socially isolated; their fellow students do not invite them to play, and adults punish them for their behavior. In the school entry examination, parents and children should be given advice on the diagnostic and therapeutic options if there are indications of HKD.
The school career of children with HKD is notably impaired (9) (Table 1). The support and disciplinary measures incur substantial costs (9, 10), which in the school setting are clearly higher than in the healthcare sector. A meta-analysis (11) with a focus on the school success of children and adolescents with HKD found significant performance impairments for reading (d=0.73), arithmetical skills (d=0.67), and spelling (d=0.55). In view of the high rate of school dropouts (10–12%) and the increased risk of such youngsters for further mental health problems—for example, conduct disorders in combination with delinquent behaviors (12)—it is necessary for children with HKD to receive treatment from a medical specialist. The complexity of the disorder with the most common comorbidities will need to be taken into account for the diagnostic evaluation and treatment.
Table 1. School career, support measures and disciplinary measures, and the costs of measures in hyperkinetic disorder.
| School career of children with HKD (e2) | Frequency and duration of school measures in HKD (10) | Frequency of disciplinary incidents across grades involving children with HKD (10) | Estimated cost of a school disciplinary act (9, 10) |
|---|---|---|---|
| Lower school leaving level | 0 years: 47.6% | 5.8% of children with HKD once a week (0.0% of controls) |
Additional annual costs of attending a different school ($ 4181) |
| Grade retention (e3) | 1–3 years: 18% | 29.6% of children with HKD once a month (2.5% of controls) |
For repeating a year ($ 222) |
| Suspension and expulsion from school | 4–6 years: 12.2% | 45.5% of children with HKD once a quarter (7.9% of controls) |
For disciplinary measures ($ 604) |
| Absenteeism/truancy | >7 years 22.2% | 19.1% of children withHKD less than once a quarter (89.6% of controls) |
Additional annual costs incurred to the school system in the USA by HKD $13.4 billion |
| School drop-out | £4155,03 per year school-related costs (compared with total costs from healthcare expenditure of £5492.63) incur 75% of the total cost of HKD (9) |
HKD, hyperkinetic disorder
The school report or the teacher’s diagnostic assessment should have a special role in the medical specialist’s diagnostic evaluation of HKD. The International Classification of Diseases (ICD-10) requires for the purposes of a diagnosis that the symptoms occur in more than one situation—for example, at home and at school. Thus, the teacher’s observations are a vital ingredient in the diagnostic process. Qualitative (descriptions of a child’s attention, motor restlessness, impulsivity, performance ability, and social competence) and quantitative standardized behavior and observation sheets at school—such as the Child Behavior Checklist (CBCL)—are used (13).
Many teachers are uncertain about how to deal with children with HKD. Because of their hyperactive behavior during lessons and breaks, children with HKD require treatment that includes the school. A recently published systematic review of 54 studies (14) shows the methods that can be used at school and that are effective. The studies investigated the effectiveness of school-based interventions for the key symptoms of HKD, social skills, children’s self-awareness, and teachers’ perceptions of school success. Overall the effects are small (Table 2). The analysis of whether different intervention methods have a differential effect did not yield a significant result. This includes behavior modification by means of reward/punishment with or without amplification, cognitive-behavioral self instruction with problem-solving strategies, social skills training, and encouraging children to recognize and control their own feelings. During childhood, social competence training was found to be effective; in adolescence, strategies for structuring work and learning were found to deliver the best results. Methods for the direct modification of behaviors by the teacher, by using a daily report card, on which the designated changes were described, were effective on the whole (15).
Table 2. School-based intervention in children with hyperkinetic disorder*.
| Symptom | Informant | Number of studies/sample (total) | Cohen’s d | 95% confidence interval | p value |
|---|---|---|---|---|---|
| Inattention | Parent | 7 (384) | 0.13 | [–0.14; 0.40] | 0.33 |
| Teacher | 12 (548) | 0.60 | [0.14; 1.06] | <0.001 | |
| Child | 7 (292) | 0.44 | [0.18; 0.70] | 0.32 | |
| Hyperactivity/impulsivity | Parent | 7 (285) | 0.16 | [–0.07; 0.39] | 0 |
| Teacher | 16 (700) | 0.23 | [–0.03; 0.49] | 0.08 | |
| Child | 8 (411) | 0.33 | [0.13; 0.53] | 0.001 | |
| HKD symptoms combined | Parent | 3 (110) | 0.14 | [–0.46; 0.75] | 0.65 |
| Teacher | 6 (218) | 0.16 | [–0.22; 0.54] | 0.42 |
*Effect sizes of randomized controlled studies on measures of hyperkinetic disorder (14)
HKD, hyperkinetic disorder
Specific developmental disorders of scholastic skills
The ICD-10 and the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classify substantial problems in learning to read, arithmetic skills, and spelling under the specific developmental disorders of scholastic skills (ICD-10) and specific learning disorders (DSM-5) (16). These learning disorders occur at a rate of 4–6%, respectively. In specialist medical practice, children often present with severe headache or abdominal pain, for which no physical correlate is identified during the subsequent examination. In a pronounced developmental disorder, affected students often avoid attending school, with the result that several weeks of absence may accrue. A meta-analysis (17) focusing on the rates of anxiety in children and adolescents with learning disorders (reading and/or spelling disorder, disorder of arithmetic skills) showed that anxiety was significantly more common (d=0.61; P<0.001), independently of sex or grade. Furthermore, the meta-analysis showed higher rates of comorbidities with depressive disorders, HKD, conduct disorders, and emotional disorders. The disease course is characterized as follows:
A stubborn persistence of the key symptoms
Notably worse school exit examination results than might have been expected on the basis of a student’s cognitive performance ability
A need to repeat school years
Frequent dropping out of school
Changing schools
Psychological stress
A higher risk for depressive disorders and anxiety disorders (18).
An integrated medical-pedagogical approach for treating such young people is therefore urgently needed. If a comorbid psychological disorder is present the therapy should consider pedagogical support and psychosocial integration, in addition to the relevant child and adolescent psychiatric and psychotherapeutic treatment guidelines (19).
In instructing students with learning disorders it is of great importance to identify anxieties, low mood, or negative thoughts in students, and to initiate support measures, in a timely manner. Identifying any potential school-related links to the mental health problems is greatly important (20). The school-based support systems include—in addition to teachers—school social workers and school psychologists. Medical specialists’ central task is to coordinate the different support systems for every child and to supervise them. This includes giving advice on the symptoms and on how to deal with mental health problems at school.
Depressive disorders
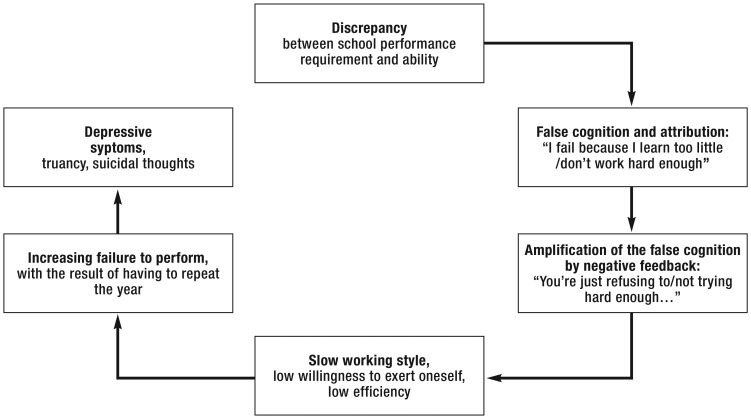
Worldwide, the prevalence of depressive disorders in childhood and adolescence is 4–5% (21). Girls are affected twice as often as boys (22). The main symptoms include difficulties in concentrating, lack of self worth, low mood, joylessness, a loss of activities and interests, social withdrawal, giving up leisure activities, changes in appetite, sleep disruption, and—in moderate to severe forms—suicidal thoughts and acts. Depression in adolescence is one of the greatest risk factors for suicide in this age group (23). Depression affects the psychosocial and school-related development of adolescents in a major way. They increase the risk of having to repeat a year, dropping out of school, and being placed in special education (24, 25). The reasons may be the neurocognitive impairments that often accompany depression—such as reduced attention, an impaired ability to organize one’s work, and impaired memory function (26). These reinforce the changed self-perception regarding one’s own capability that accompanies the depression (Figure). Affected students experience their inability to perform as a personal failure, and having to repeat a year is interpreted as punishment, which triggers additional stress. Because of their depression, such students cannot compensate for the learning impairment. This cycle is amplified by the fact that adolescents are less likely to seek help (27); consequently, support and relief regarding their school-related demands mostly comes too late for those affected.
Figure.
Developmental model of depressive symptoms in academic failure
School-based factors that moderate the mutual influence between depressive disorder and school career include the school climate and a student’s school connectedness (Table 3). If both factors are weakly expressed then the risk of developing a depressive disorder is increased (12, 28). In a representative longitudinal study from the US, which included 11 852 adolescents, significant associations were seen between a poor attachment to the school (r=-0.33), a poor attachment to teachers (r=-0.20), and more pronounced depressive symptoms (29).
Table 3. School climate: School-related factors that influence students’ mental health development.
| Factor | Examples | Importance for mental health development |
|---|---|---|
| Safety at school (social-emotional and physical safety [e4] owing to standards and rules) |
Adherence to social rules, Control of availability of weapons and drugs in schools, Teaching and monitoring behavioral rules and standards, Managing conflict and strengthening students’ problem solving skills |
Poor safety increases the risk for experiencing violence, violence against fellow students (bullying/mobbing), disciplinary measures taken against students, absenteeism/truancy, and less success at school. |
| Connectedness to school (29, e5) | I am happy to be at this school! I think I am a part of this school! I feel safe at this school! I feel attached to my fellow students! The teachers treat me with fairness! |
Low school connectedness increases the risk (e5) for depressive symptoms, anxiety, violence, and bullying/mobbing whereas high school connectedness reduces that risk. A close social bond with fellow students further reduces the risk of developing mental health problems. High school connectedness supports students’ individual successful learning. |
| Relationship/interaction between teacher and student | How strongly do you feel that your teacher takes care of you/worries about you? How often during this school year have you had trouble/conflict with your teacher? |
If a teacher cares about a student this correlates with fewer symptoms of depression in students (29). A conflicted relationship between teacher and student increases the risk for abnormal behaviors and learning problems. A teacher’s emotionally supportive, committed, and responsible attitude towards their student results in less disruptive behavior and fewer internalizing disorders (e6). |
| Learning environment at school (e7) | Collaborative group work with a common aim, Feelings of belonging and attachment are shaped by mutual trust in the group of students | Great willingness to cooperate and achieving aims together improve the climate in the classroom and yield greater learning success. |
Depressive disorders in childhood and adolescence should be treated according to the current S3 guidelines (30). Evidence based treatment methods include psychotherapy and psychopharmacotherapy; both are recommended. In a mild depressive episode, outpatient treatment is the preferred option. If the patient is managing in everyday life, supportive counseling with regular controls may be offered. Cooperation and collaboration between medical specialists and schools/teachers can contribute substantially to achieving a supportive and stress-reducing attitude of teacher to student, by means of psychoeducation and advice on how to handle suicidal ideation from/in students.
Screening in schools
The diagnostic quality of screening methods for psychological stress—for example, emotional problems, attention deficit disorders and hyperactivity, problems in dealing with peers, and abnormal behaviors—has been repeatedly studied in schools (31– 33). The strengths and difficulties questionnaire (SDQ) is a popular screening instrument (34– 36) that is used in the previously mentioned settings of teachers, parents, and professionals in the healthcare sector (37). In an epidemiological sample (37) of 7984 students aged 5–15 years, 70% of students with conduct disorders, hyperactivity, depressive symptoms, and anxiety disorders were correctly diagnosed by using the SDQ, compared with the ICD-10 diagnoses. The specificity for mental health problems was 94.6% (95% CI [94.1%; 95.1%]), the sensitivity was 63.3% [59.7%; 66.9%]. Comparing the teacher’s rating with the parental one showed that teachers identified HKD more often and parents were better at identifying anxiety disorders and depression. The best screening result was reached by combining the parents’ and teachers’ ratings. In specialist medical care, questionnaires are time-saving instruments for assessing—in a valid and reliable manner—in at-risk children or adolescents with unexplained symptoms whether they are experiencing the symptoms of a depressive disorder or HKD (31, 38). For the school entry exam (32), screening instruments could be useful in identifying early exposures that may trigger mental health problems. For the examination between the ages of 7 and 8 years, it would be necessary to extend the screening areas by including emotional stress and symptoms of depression. In this way, early stress factors for the child—which occur in school in some cases—can be identified and the required help and treatment can be initiated in a timely manner. The use of questionnaires in schools should remain the preserve of school psychologists or school doctors, who can recommend and initiate the necessary measures depending on the result.
School-based prevention and intervention
Under the title “Mental Health Program or Promotion,” prevention and intervention measures have been conducted in schools worldwide, at different levels, with the entire school, at class level, or with risk groups, in order to strengthen children and adolescents’ mental health in general and in the school setting in particular (39). Weare and Nind (39) summarize the results of 52 systematic reviews (Box). Global school concepts that includes the changes in school life—including the atmosphere/climate, architectural aspects, extracurricular support systems, and acceptance in the city or municipality—have, in spite of their increasing popularity, shown hardly any effects or none at all (39, e8). Possible reasons may be unclear and unfocused objectives, an absence of clear guidelines for implementation, a lack of instruction manuals, insufficient instruction and training of those in positions of responsibility for undertaking the program, and lacking implementation and quality controls (40). The effect sizes of the school-based prevention and intervention programs in terms of strengthening mental health, reducing psychological pressures/stress, reducing bullying/mobbing, and promoting prosocial behavior are low to moderate. Universal programs to reduce violence and improve conflict resolution in the context of bullying/mobbing had a very low effect size. This is notably higher when the prevention and intervention method target students with an increased risk for mental health problems, such as anxiety or depression, or target groups of students who display violent behaviors. It should be emphasized that only a sustained implementation of programs with quality assurance, qualified advanced and extended training for those conducting the programs, and an improvement of a school’s atmosphere/climate will lead to sustained success in prevention and intervention in schools. A summarized overview of German-language programs for preventing mental health problems and behavioral problems in children and adolescents was presented by Röhrle (e1).
Box. Evidence and recommendation for school-based prevention and intervention*.
Topics
Recommendations for changes to a school’s climate (attitudes, convictions, and values); strengthening of social and emotional competencies combined with positive feedback if students achieve their learning objectives, universal and selective prevention in order to reduce the risk of developing internalizing disorders (anxiety, depression) and externalizing disorders (conduct disorders, violence, bullying/mobbing).
Advanced and extended training
Specific advanced training in prevention and intervention measures is required, to raise awareness of mental health and illness in children and adolescents. Such training should be delivered by qualified experts—for example, school psychologists, school social workers, and teachers. Cooperation and collaboration with health professionals is recommended.
Methods
Interventions based on the methods of cognitive-behavioral therapy; interactive, class-based, and group-based methods, measures directed at target groups; strengthening of individual resources, exclusively information-based methods not recommended.
Networking
Close cooperation with parents, authorities, and partners from the social, educational, and healthcare sectors is recommended.
Implementation
Programs should have a clear structure, clearly formulated objectives, verifiable benchmarks to assess whether they are being conducted at a high quality level, and achieving objectives, clear instructions, quality assurance, and an implementation plan; monitoring of implementation and achieving of objectives is strongly recommended.
Temporal aspects
Measures should start early and should be initiated in primary school children;
Interventions should be undertaken for the long term (longer than a year); booster sessions are recommended to make the effects of the intervention permanent or even strengthen them.
*For the purposes of promoting mental health and reducing the risk of developing mental health problems (according to 39).
Challenges and solutions
In view of the high prevalence rates of mental health problems in children and adolescents and their importance for young people’s scholastic development, and in view of the low uptake of the relevant services provided by the healthcare system, the risks of mental health problems should be identified at an early stage and reduced by means of preventive measures. Children, adolescents, and their families should be informed about the options available in the healthcare system, and access to such services should be improved. The school as a central institution in the education system, with its support systems in the psychosocial area (school social workers, school psychologists) can take a central role in this, in cooperation with services provided by the healthcare system (public health services; general practitioners; outpatient, part-inpatient, and inpatient child and adolescent psychiatric and psychosomatic services, as well as psychotherapeutic and medical services for children and adolescents) and by youth welfare services, by implementing the following measures:
Screenings
Preventive measures
Changes in class and school climate
Advanced training for teachers.
Key Messages.
Stress factors at school—such as unempathetic and unsupportive teacher-student relationships and a poor classroom or school climate—increase the risk for children and adolescents of developing mental health problems.
Mental health problems in young persons—for example, hyperkinetic disorder, depressive episodes, and specific developmental disorders of scholastic skills (specific reading and/or spelling disorder, specific disorder of arithmetic skills)—impair children’s and adolescents’ performance and notably increase the risk for absenteeism/truancy from and dropping out of school.
By cooperating with schools and by seeking support from and collaborating with school social workers and school psychologists, doctors can help teachers to identify stress factors in the school setting and reduce risks for children and adolescents in that setting.
School-based prevention programs have low to moderate effect sizes in reducing young persons’ risk for developing mental health problems.
Mental health programs in school have so far shown very little effect or none at all. Qualified advanced training of teachers at all types of schools on the subject of mental health problems and disorders in children and adolescents with mental health problems is recommended.
Acknowledgments
Translated from the original German by Birte Twisselmann, PhD.
Footnotes
Conflict of interest statement
The author declares that no conflict of interest exists.
References
- 1.Kieling C, Baker-Henningham H, Belfer M, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378:1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 2.Ravens-Sieberer U, Otto C, Kriston L, et al. The longitudinal BELLA study: design, methods and first results on the course of mental health problems. Eur Child Adolesc Psychiatry. 2015;24:651–663. doi: 10.1007/s00787-014-0638-4. [DOI] [PubMed] [Google Scholar]
- 3.Green J, McLaughlin K, Alegría M. School mental health resources and adolescent mental health service use. J Am Acad Child Psychiatry. 2013;52:501–510. doi: 10.1016/j.jaac.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rutter M. Cambridge, MA USA: Harvard University Press; 1982. Fifteen thousand hours: secondary schools and their effects on children. [Google Scholar]
- 5.Statistisches Bundesamt. Zahl der Schüler im Schuljahr 2014/2015 um 0,7 % gesunken. www.destatis.de/DE/PresseService/Presse/Pressemitteilungen2015/03/PD15_093_211pdf. (last accessed on 3 November 2015) [Google Scholar]
- 6.World Health Organization. World Health Organization. 1992. The ICD-10 classification of mental and behavioral disorders: clinical discriptions and diagnostic guidelines. [Google Scholar]
- 7.Polanczyk G, Willcutt E, Salum G, Kieling C, Rohde L. ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int J Epidemiol. 2014:1–9. doi: 10.1093/ije/dyt261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schuber I, Köster I, Lehmkuhl G. The changing prevalence of attention-deficit/hyperactivity disorder and methylphenidate prescriptions: a study of data from a random sample of insurees of the AOK Health Insurance Company in the German State of Hesse, 2000-2007. Dtsch Arztebl Int. 2010;107:615–621. doi: 10.3238/arztebl.2010.0615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Telford C, Green C, Logan S, Langley K, Thapar A, Ford T. Estimating the costs of ongoing care for adolescents with attention-deficit hyperactivity disorder. Soc Psychiatry Psychiatr Epidemiol. 2013;48:337–344. doi: 10.1007/s00127-012-0530-9. [DOI] [PubMed] [Google Scholar]
- 10.Robb J, Sibley M, Pelham W, et al. The estimated annual cost of ADHD to the US education system. School Ment Health. 2011;3:169–177. doi: 10.1007/s12310-011-9057-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frazier T, Youngstrom E, Glutting J, Watkins M. ADHD and achievement: meta-analysis of the child, adolescent, and adult literatures and a concomitant study with college students. J Learn Disabil. 2007;40:49–65. doi: 10.1177/00222194070400010401. [DOI] [PubMed] [Google Scholar]
- 12.Kuperminc G, Leadbetter B, Blatt S. School social climate and individual differences in vulnerability to psychopathology among middle school students. J School Psychol. 2001;39:141–159. [Google Scholar]
- 13.Döpfner M, Plück J, Kinnen C. Elternfragebogen über das Verhalten von Kindern und Jugendlichen (CBCL/6-18R), Lehrerfragebogen über das Verhalten von Kindern und Jugendlichen (TRF/6-18R), Fragebogen für Jugendliche (YSR/11-18R) Göttingen: Hogrefe; 2014. CBCL/6-18R, TRF/6-18R, YSR/11-18R. Deutsche Schulalter-Formen der Child Behavior Checklist von Thomas M. Achenbach. [Google Scholar]
- 14.Richardson M, Moore D, Gwernan-Jones R, et al. Non-pharmacological interventions for attention-deficit/hyperactivity disorder (ADHD) delivered in school settings: systematic reviews of quantitative and qualitative research. Health Technol Assess. 2015;19:1–470. doi: 10.3310/hta19450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fabiano G, Vujnovic R, Pelham W, et al. Enhancing the effectiveness of special education programming for children with ADHD using a daily report card. School Psychol Rev. 2010;39:219–239. [Google Scholar]
- 16.Schulte-Körne G. Spezifische Lernstörungen. Z Kinder- Jugendpsychiatr Psychother. 2014;42:369–374. doi: 10.1024/1422-4917/a000312. [DOI] [PubMed] [Google Scholar]
- 17.Nelson J, Harwood H. Learning disabilities and anxiety: a meta-analysis. J Learn Disabil. 2011;44:3–17. doi: 10.1177/0022219409359939. [DOI] [PubMed] [Google Scholar]
- 18.Wilson A, Armstrong C, Furrie A, Walcot E. The mental health of Canadians with self-reported learning disabilities. J Learn Disabil. 2009;42:24–40. doi: 10.1177/0022219408326216. [DOI] [PubMed] [Google Scholar]
- 19.Galuschka K, Schulte-Körne G. Clinical practice guideline: Diagnosing and treating reading and spelling disorders in children an adolescents. Dtsch Arztebl Int. 2016 doi: 10.3238/arztebl.2016.0279. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schulte-Körne G. The prevention, diagnosis, and treatment of dyslexia. Dtsch Arztebl Int. 2010;107:718–726. doi: 10.3238/arztebl.2010.0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Costello E, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44:972–986. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 22.Hyde J, Mezulis A, Abramson L. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychol Rev. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- 23.Windfuhr K, While D, Hunt I, et al. National confidential inquiry into suicide and homicide by people with mental illness. Suicide in juveniles and adolescents in the United Kingdom. J Child Psychol Psychiat. 2008;49:1155–1165. doi: 10.1111/j.1469-7610.2008.01938.x. [DOI] [PubMed] [Google Scholar]
- 24.Quiroga C, Janosz M, Lyons J, Morin A. Grade retention and seventh-grade depression symptoms in the course of school dropout among high-risk adolescents. Psychology. 2012;3:749–755. [Google Scholar]
- 25.Robles-Piña A, Defrance E, Cox D. Self-concept, early childhood depression and school retention as predictors of adolescent depression in urban hispanic adolescents. School Psychol Int. 2008;29:426–441. [Google Scholar]
- 26.Owens M, Stevenson J, Hadwin J, Norgate R. Anxiety and depression in academic performance: an exploration of the mediating factors of worry and working memory. School Psychol Int. 2012;33:433–449. [Google Scholar]
- 27.Allgaier AK, Schiller Y, Schulte-Körne G. Wissens- und Einstellungsänderungen zu Depression im Jugendalter: Entwicklung und Evaluation einer Aufklärungsbroschüre. Kindheit und Entwicklung. 2011;20:247–255. [Google Scholar]
- 28.Ross A, Shochet I, Bellair R. The role of social skills and school connectedness in preadolescent depressive symptoms. J Clin Child Adolesc Psychol. 2010;39:269–275. doi: 10.1080/15374410903532692. [DOI] [PubMed] [Google Scholar]
- 29.Joyce H, Early T. The impact of school connectedness and teacher support on depressive symptoms in adolescents: a multilevel analysis. Child Youth Serv. 2014;39:101–107. doi: 10.1016/j.childyouth.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dolle K, Schulte-Körne G. The treatment of depressive disorders in children and adolescents. Dtsch Arztebl Int. 2013;110:854–860. doi: 10.3238/arztebl.2013.0854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Frühe B, Allgaier AK, Pietsch K, et al. Children’s depression screener (ChilD-S): development and validation of a depression screening instrument for children in pediatric care. Child Psychiat Hum Dev. 2012;43:137–151. doi: 10.1007/s10578-011-0254-1. [DOI] [PubMed] [Google Scholar]
- 32.Essex M, Kraemer H, Slattery M, et al. Screening for childhood mental health problems: outcomes and early identification. J Child Psychol Psychiat. 2009;50:562–570. doi: 10.1111/j.1469-7610.2008.02015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pietsch K, Allgaier AK, Frühe B, et al. Screening for depression in adolescent paediatric patients: validity of the new Depression Screener for Teenagers (DesTeen) J Affect Disord. 2011;133:69–75. doi: 10.1016/j.jad.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 34.Goodman A, Goodman R. Strengths and difficulties questionnaire as a dimensional measure of child mental health. J Am Acad Child Adolesc Psychiat. 2009;48:400–403. doi: 10.1097/CHI.0b013e3181985068. [DOI] [PubMed] [Google Scholar]
- 35.Woerner W, Becker A, Rothenberger A. Normative data and scale properties of the German parent SDQ. Eur Child Adolesc Psychiatry. 2004 13;(Suppl 2):3–10. doi: 10.1007/s00787-004-2002-6. [DOI] [PubMed] [Google Scholar]
- 36.Woerner W, Hasselhorn M, Banaschewski T, Rothenberger A. Validation of the parent and teacher SDQ in a clinical sample. Eur Child Adolesc Psychiatry. 2004 13;(Suppl 2):11–16. doi: 10.1007/s00787-004-2003-5. [DOI] [PubMed] [Google Scholar]
- 37.Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiat. 2000;177:534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- 38.Pietsch K, Allgaier AK, Frühe B, et al. Screening for depression in adolescent paediatric patients: validity of the new Depression Screener for Teenagers (DesTeen) J Affect Disord. 2011;133:69–75. doi: 10.1016/j.jad.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 39.Weare K, Nind M. Mental health promotion and problem prevention in schools: what does the evidence say? Health Prom Int. 2011;26(S1):i29–i69. doi: 10.1093/heapro/dar075. [DOI] [PubMed] [Google Scholar]
- 40.Durlak J, Weissberg R, Dymnicki A, Taylor R, Schellinger K. The impact of enhancing students’ social and emotional learning: a meta-analysis of school-based universal interventions. Child Dev. 2011;82:474–501. doi: 10.1111/j.1467-8624.2010.01564.x. [DOI] [PubMed] [Google Scholar]
- e1.Röhrle B. Prävention und Gesundheitsförderung, Band III für Kinder und Jugendliche. Tübingen: DGVT-Verlag. 2007 [Google Scholar]
- e2.Kent K, Pelham W, Molina B, et al. The academic experience of male high school students with ADHD. J Abnorm Child Psychol. 2011;39:451–6S2. doi: 10.1007/s10802-010-9472-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e3.Langberg J, Molina B, Arnold L, et al. Patterns and predictors of adolescent academic achievement and performance in a sample of children with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2011;40:519–531. doi: 10.1080/15374416.2011.581620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e4.Thapa A, Cohen J, Guffey S, Higgins-D’Alessandro A. A review of school climate research. Rev Educ Res. 2013;83:357–385. [Google Scholar]
- e5.Bond L, Butler H, Thomas L, et al. Social and school connectedness in early secondary school as predictors of late teenage substance use, mental health, and academic outcomes. J Adolesc Health. 2007;40 doi: 10.1016/j.jadohealth.2006.10.013. [DOI] [PubMed] [Google Scholar]
- e6.Way N, Reddy R, Rhodes J. Students’ perceptions of school climate during the middle school years: associations with trajectories of psychological and behavioral adjustment. Am J Comm Psychol. 2007;40:194–213. doi: 10.1007/s10464-007-9143-y. [DOI] [PubMed] [Google Scholar]
- e7.Stewart E. School structural characteristics, student effort, peer associations, and parental involvement: the influence of school- and individual-level factors on academic achievement. Educ Urban Soc. 2008;40:179–204. [Google Scholar]
- e8.Kidger J, Araya R, Donovan J, Gunnell D. The effect of the school environment on the emotional health of adolescents: a systematic review. Pediatrics. 2012;129:925–949. doi: 10.1542/peds.2011-2248. [DOI] [PubMed] [Google Scholar]