Abstract
Objectives:
We describe the process of identifying and defining nocturnal sleep-related variables (for example, movement/non-movement indicators of sleep efficiency, waking episodes, midpoint and so on) using the unique 24-h waist-worn free-living accelerometer data collected in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE).
Methods:
Seven consecutive days of 24-h waist-worn accelerometer (GT3X+, ActiGraph LLC) data were collected from over 500 children at each site. An expert subgroup of the research team with accelerometry expertize, frontline data collectors and data managers met on several occasions to categorize and operationally define nocturnal accelerometer signal data patterns. The iterative process was informed by the raw data drawn from a sub set of the US data, and culminated in a refined and replicable delineated definition for each identified nocturnal sleep-related variable. Ultimately based on 6318 participants from all 12 ISCOLE sites with valid total sleep episode time (TSET), we report average clock times for nocturnal sleep onset, offset and midpoint in addition to sleep period time, TSET and restful sleep efficiency (among other derived variables).
Results:
Nocturnal sleep onset occurred at 2218 hours and nocturnal sleep offset at 0707 hours. The mean midpoint was 0243 hours. The sleep period time of 529.6 min (8.8 h) was typically accumulated in a single episode, making the average TSET very similar in duration (529.0 min). The mean restful sleep efficiency ranged from 86.8% (based on absolute non-movement of 0 counts per minute) to 96.0% (based on relative non-movement of <100 counts per minute).
Conclusions:
These variables extend the potential of field-based 24-h waist-worn accelerometry to distinguish and categorize the underlying robust patterns of movement/non-movement signals conveying magnitude, duration, frequency and periodicity during the nocturnal sleep period.
Introduction
In 2012, Meltzer et al.1 published an excellent review of the use of actigraphy (defined as ambulatory devices that estimate sleep–wake patterns from activity levels) for assessment in the pediatric sleep research. They also offered recommendations for standardizing assessment methods, including providing standardization for the definition and scoring of commonly reported variables. Actigraphy is a more objective measure than parent-proxy or child self-reported sleep behaviors and can be used to assess sleep–wake periods for extended periods of time in a child's free-living environment. Sleep researchers have relied primarily on wrist-worn accelerometry-based devices (although waist-worn devices can provide similar estimates of total sleep time as those worn on the wrist)2 and largely ignored the possibility for detecting daytime movements and non-movements.
Although actigraphy is the preferred term to describe monitoring devices in nocturnal sleep research, accelerometry is the preferred term to describe the same type of monitoring devices used to study free-living physical activity and sedentary behavior accumulated during waking hours.3 Accelerometer-based assessment of free-living humans more traditionally relies on the waist attachment site, which provides better estimates of energy expenditure,4, 5 moderate-to-vigorous physical activity,5 sedentary behavior5 and steps per day6 than a wrist attachment site. Further, decision rules, cut points and variable definitions exist for defining sedentary time and various intensities of physical activity based on waist-worn accelerometry,7 whereas the same interpretive infrastructure is comparatively limited for the wrist attachment site.
Free-living accelerometry originally focused on movement and non-movement patterns only during waking hours (protocols included instructions to remove the device for sleep);8 however, there has been a recent push to collect multiple 24-h days of continuous wear.9 The device remains at the waist for the full 24 h to minimize compliance problems associated with moving the device from one attachment site to another.10 The differences in detected movement and non-movement patterns of waist-worn acccelerometry tracings collected during waking hours and during the nocturnal sleep period time are visually distinct. Algorithms2, 9, 11 have been produced, validated and ultimately refined to fully automate the capture of sleep onset and offset and thus define total sleep episode time (TSET) for the nocturnal time period.12 Within TSET, however, there are also visually distinct signal patterns that could be further quantified (considering magnitude, duration, frequency and periodicity) to infer movement/non-movement-defined parameters associated with nocturnal sleep and wake cycles. Although Meltzer et al.1 did propose a number of variables to capture episodes and patterns of night waking in pediatric sleep research detected using the wrist-based actigraphy data, we know of no research at this time that has attempted to identify and define similar nocturnal sleep-related variables from the waist-worn free-living accelerometry data.
The purpose of this article is to describe the process of distinguishing and categorizing nocturnal sleep-related variables (for example, movement/non-movement indicators of sleep efficiency, wake episodes, midpoint and so on) using the unique 24-h waist-worn free-living accelerometer data collected from children participating in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE).13 Our intent is to provide a clear presentation and rationale for the derived nocturnal sleep-related variables and their definitions to promote future analysts' use of these important data portraying the full breadth of children's 24-h objectively monitored movement/non-movement behaviors.
Materials and methods
Overview of ISCOLE study design
ISCOLE is a cross-sectional study of ~7000 children (9–11 years of age) from Australia, Brazil, Canada, China, Colombia, Finland, India, Kenya, Portugal, South Africa, the United Kingdom and the United States of America. A detailed methods paper has been published.13 Included among the measures was the distribution of accelerometers (GT3X+, ActiGraph LLC, Pensacola, FL, USA) through local schools to over 500 children at each site. Seven consecutive days of the 24-h waist-worn data were collected and electronically transferred to the US-based study coordinating center's secure website. Quality control checks and data management and treatment decisions leading to the ultimate site-specific locked data sets have also been previously published.10 The 24-h wearing regimen is an ISCOLE protocol feature permitting extraction of distinctive nocturnal sleep-related movement/non-movement patterns separate from the physical activity and sedentary behaviors detected during waking hours.
Definitions of sleep-related variables
We have previously published two detailed explications of the process (with links to the relevant publically available SAS syntax, SAS Institute Inc., Cary, NC, USA) of delineating the nocturnal sleep period time9 and ultimately TSET.12 Herein we expand this process to demarcate additional nocturnal sleep-related variables evident from distinctive accelerometer data signal patterns (defined by their magnitude, duration, frequency and/or periodicity) contained within TSET. Magnitude is inferred from the value of activity counts per minute observed, duration is a measure of accumulated minutes in movement/non-movement, frequency is a count of events during the TSET and periodicity is the apparent tendency to appear at regular intervals.
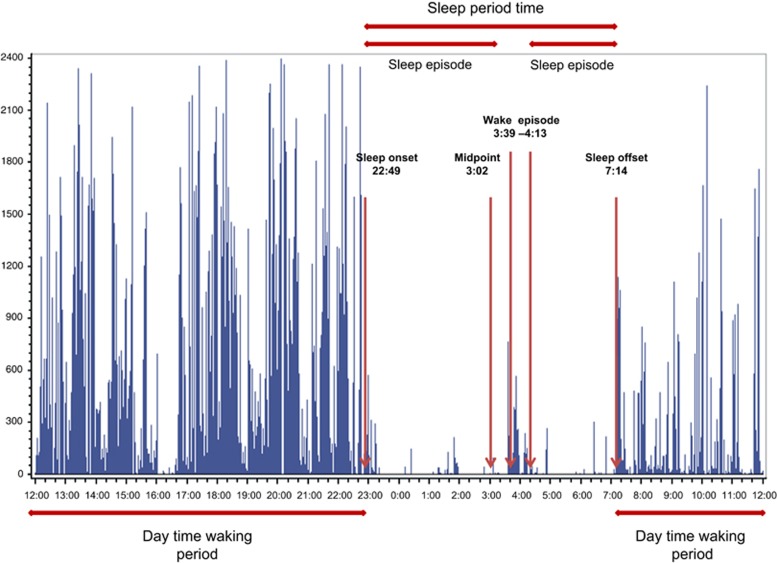
An expert subgroup of the research team, including investigators with accelerometry expertize, frontline data collectors and data managers, met on several occasions to study and categorize ISCOLE participants' waist-worn nocturnal accelerometer signal data patterns in the context of wrist-worn actigraphy scoring and naming conventions and methods.1, 14 It was imperative that the clock time variables associated with sleep onset, sleep offset and midpoint could be clearly defined for children with varying sleep habits. Duration variables of sleep period time, sleep episodes (and their antonymous reflection and wake episodes), TSET (and its reflection and total wake episode time), restful sleep (associated with non-movement), detected movements during sleep and total disrupted sleep (including waking episode and movement during sleep) were also indicated. Finally, efficiency variables that considered the relationship between specific duration variables captured estimates of sleep episode efficiency and restful sleep efficiency. The exact definitions presented in Table 1 evolved from careful scrutiny of the ISCOLE data, following an iterative process of sifting through raw data queries to identify reoccurring digital themes and distinguish emergent patterns, revising scoring parameters until ultimately a refined and replicable delineation of sleep-related variables were achieved. All definitions were initially developed using a randomly drawn sub set of the US children's data; Figure 1 is an illustrative example of some of these definitions using one night's data drawn from a single US child. Application of these definitions to the data collected in other ISCOLE country sites led to additional refinements.9, 12 The descriptive data presented here are based on these finalized definitions.
Table 1. Nocturnal sleep-related variables, their definitions and descriptive data based on 24-h waist-worn accelerometer movement/non-movement data signals captured across all 12 ISCOLE country sites.
| Variable | Definition | Mean±s.d. (range) across sites and range if applicable |
|---|---|---|
| Nocturnal sleep onset | The clock time of the first of 5 consecutive SIA-scored sleep minutes between the clock times of 1900 and 0559 hours | 2218±0059 (1940–0307) hours |
| Nocturnal sleep offset | The clock time of the first minute of 20 consecutive minutes (between 2140 and 0459 hours) or 10 consecutive minutes (between 0500 and 1158 hours) scored as wake using SIA taken from the last sleep episode occurring during sleep period time | 0707±0050 (0242–1109) hours |
| Midpoint | Mean clock time between nocturnal sleep onset and sleep offset; used to chronotype individuals as early or late sleepers (Table 2) | 0243±0050 (2346–0626) hours |
| Sleep period time | Duration of time (minutes) from nocturnal sleep onset to nocturnal sleep offset, including all minutes scored as sleep/wake after onset using SIA | 529.6±53.5 (316–809) |
| Sleep episode | Continuity of movement/non-movement patterns (⩾160 min) scored as SIA-defined sleep, including isolated SIA-scored minutes of wake, ends with the first of 10 consecutive minutes (between 0500 and 1158 hours) or 20 consecutive minutes (between 0940 and 0459 hours) of SIA-scored wake minutes | Frequency of nights with 1 sleep episode: 42 008 (91.7%) 2 sleep episodes: 3641 (7.9%) 3 sleep episodes: 172 (0.4%) 4 sleep episodes: 3 (0%) |
| Total sleep episode time (TSET) | Total minutes from all sleep episodes (including isolated wake minutes contained within sleep episodes) occurring during the sleep period time | 529.0±53.7 (316–809) |
| Wake episode | An occurrence of ⩾20 consecutive SIA-scored wake minutes preceded and followed by a sleep episode; ends with 1 min classified as sleep | Frequency of nights with 0 wake episodes: 42 008 (91.7%) 1 wake episode: 3641 (7.9%) 2 wake episodes: 172 (0.4%) 3 wake episodes: 3 (0%) |
| Total wake episode time | Total minutes from all wake episodes occurring during TSET | 0.6±4.0 (0–116.7) |
| Sleep episode efficiency | Total sleep episode time divided by sleep period time (expressed in %) | 99.9±0.7% (78.7–100%) |
| Total restful (non-movement) sleep time | Accumulated minutes at 0 or <100 activity counts per minute during sleep episodes | Cutoff =0: 459.5±49.2 (237.6–764.3) Cutoff <100: 508.6±52.0 (301.2–797.3) |
| Sleep episode movements | Accumulated minutes >0 or ⩾100 activity counts per minute occurring during sleep episodes | Cutoff>0: 69.5±17.6 (9.3–164.8) Cutoff ⩾100: 20.4±7.6 (2.3–60.7) |
| Total disrupted sleep | Accumulated minutes >0 or ⩾100 activity counts per minute from all wake episodes plus activity-count defined sleep episode movements | Cutoff>0: 70.1±18.0 (9.3–164.8) Cutoff⩾100: 21.0±8.6 (2.3–128.9) |
| Restful sleep efficiency | Total restful sleep time at 0 or <100 activity counts per minute divided by sleep period time (expressed in %) | Cutoff=0: 86.8±3.1% (60.2–98.7%) Cutoff<100: 96.0±1.6% (76.5–99.5%) |
Note: SIA denotes a Sadeh+inclinometer algorithm, described in detail in Barreira et al.12
Figure 1.
Visual depiction of select 4-h free-living waist-worn accelerometer nocturnal sleep-related variables using one night's data drawn from a single US child participating in ISCOLE.
Of particular note, a clear definition of non-movement was needed to subsequently define other accelerometry-based variables. Non-movement was defined in two ways. Absolute non-movement was defined by an accelerometer signal registering 0 activity counts per minute and not otherwise categorized as non-wear during original data processing. Relative non-movement was defined as an accelerometer signal registering <100 activity counts per minute and not otherwise categorized as non-wear. The selection of <100 activity counts per min as a cut point for relative non-movement was based on its widespread acceptance as an indicator of day time sedentary behaviors.15
Descriptive data for sleep-related variables
The descriptive data presented herein are based on finalized definitions and represent all ISCOLE country sites. All study sites' data sets were focused on nocturnal sleep using a noon-to-noon 24-h data format, and a refined algorithm based on scoring any minute as sleep using the Sadeh algorithm11 and then considering the accelerometer inclinometer function to identify the probability of sleep or wake for each minute according to a Sadeh+inclinometer algorithm.12 This enabled the identification of clock times associated with nocturnal sleep onset and sleep offset, midpoint (mean clock time between sleep onset and sleep offset), the sleep period time (time of sleep onset to sleep offset, including all episodes of sleep and wakefulness after onset) and TSET (allowing us to exclude extended periods of wakefulness from sleep period time). This was a detailed process described more thoroughly by Barreira et al.12 Non-wear during TSET was subsequently separated using a second algorithm before further processing. Those additional details are also available in the ISCOLE Accelerometer Manual of Operations published as an electronic supplement to a separate article.10 In brief, non-wear during TSET was defined as any sequence of ⩾90 consecutive minutes of 0 activity counts. If ⩾90% of the sleep episode was classified as non-wear, the whole sleep episode was reclassified as non-wear.16
Data were then summarized at the participant level to categorize a valid night and valid case according to an estimate of evidentiary sufficient wear. A valid night was defined as having at least 160 min of sleep, and a valid case was defined as a participant accumulating ⩾3 valid nights, including 1 weekend night. The analytical data set was comprised of 6318 valid cases (688 excluded with invalid data) comprising 34 820 valid nights of data. Participant-level means were created (only for cases with valid sleep and only nights with valid sleep) by systematically applying each of the definitions for the selected sleep-related variables presented in Table 1. Finally, descriptive data were produced by averaging participant-level means. Table 1 presents the identified nocturnal sleep-related variables and their definitions based on 24-h waist-worn accelerometer movement/non-movement data signals.
As a single example of the potential utility of these variables, we compared ‘early' and ‘late' sleepers (as defined relative to the sample's average midpoint clock time considering all days) using independent t-tests and the magnitude of the effect size (Cohen's d) for nocturnal sleep onset and offset, average sleep period time, TSET, sleep episode efficiency and restful sleep efficiency (both absolute- and relative-based definitions).
Results
Table 1 presents the identified nocturnal sleep-related variables and their definitions based on 24-h waist-worn accelerometer movement/non-movement data signals. Table 1 also presents descriptive data for identified sleep-related variables across all ISCOLE country sites.
Overall, 9–11-year-old children in ISCOLE experienced an accelerometer-determined nocturnal sleep onset at the clock time of 2218 hours and a nocturnal sleep offset at 0707 hours. The mean midpoint clock time was 0243 hours (the median was 0239 hours). The sleep period time of 529.6 min (8.8 h) was typically accumulated in a single episode, making the average TSET very similar to sleep period time in duration (529.0 min). The occurrence of sleep episode and wake episodes were naturally antonymous reflections of each other. The difference between the sleep period time and the TSET was therefore the summed duration of total wake episodes. The resulting estimate of sleep episode efficiency was almost whole (99.9%) on average in this children's sample.
Descriptive data based on identification of movement versus non-movement differed depending on the specific cutoff employed to describe absolute (0 activity counts per minute) versus relative non-movement (<100 activity counts per minute). A mean estimate of restful sleep efficiency ranged from 86.8% (based on absolute non-movement of 0 activity counts per minute) to 96.0% (based on relative non-movement of <100 activity counts per minute).
Table 2 presents the comparison of select accelerometer-determined sleep-related variables stratified relative to the sample's average midpoint clock time (02:43) considering all days. P-values suggested significant differences in all variables in this large sample, however, effect size magnitudes indicated that only the nocturnal sleep onset and offset are meaningfully different between early and late sleepers.
Table 2. Comparison of select accelerometer-determined sleep-related variables stratified relative with the sample's average midpoint clock time considering all days.
| Variable (definitions in Table 1) | ‘Early' sleepers (midpoint <0243-hour clock time) | ‘Late' sleepers (midpoint ⩾0243-hour clock time) | P-value | Cohen'sd |
|---|---|---|---|---|
| Nocturnal sleep onset | 2139 (0035) (1939–2348) hours | 2302 (0047) (2032–0306) hours | <0.0001 | 2.14 |
| Nocturnal sleep offset | 0636 (0034) (0242–0852) hours | 0741 (0042) (0530–1108) hours | <0.0001 | 1.76 |
| Sleep period time | 538.2 (48.4) (316.3–756.3) | 520.0 (57.3) (316.0–809.0) | <0.0001 | 0.36 |
| Total sleep episode time | 537.7 (48.5) (316.3–756.3) | 519.2 (57.4) (316.0–809.0) | <0.0001 | 0.36 |
| Sleep episode efficiency | 99.9±0.5% (85.1–100%) | 99.9±0.9% (78.7–100%) | 0.0038 | 0.09 |
| Restful sleep efficiency | Cutoff=0: 86.4±3.1% (60.2–95.6%) Cutoff<100: 95.9±1.5% (81.3–99.5%) | 87.2±3.0% (71.4–98.7%) 96.2±1.6% (76.5–99.6%) | <0.0001 <0.0001 | 0.29 0.21 |
Discussion
The ISCOLE accelerometer data set provides a unique opportunity to study children's 24-h physical activity, sedentary time and sleep-related behaviors in relation to each other, and also in relation to other lifestyle behaviors, the environment and obesity. The purpose of this methodological paper was to explicate the process leading to the definition of sleep-related variables representing the visually distinctive nocturnal sleep-related accelerometer movement/non-movement signals. Although sleep researchers have provided similar direction with regard to scoring wrist-worn actigraphy data,1 it is not directly applicable to 24-h waist-worn accelerometry data. Thus, this process was a necessary first step towards classifying the evident and reoccurring nocturnal sleep-related patterns in children's waist-worn accelerometer data, separate and distinct from physical activity and sedentary time collected during waking hours.
Polysomnography is considered the gold standard to study sleep patterns17 but its utility is largely confined to clinical and laboratory settings, making it less relevant to large-field and epidemiological studies. Actigraphy (conventionally at the wrist) and accelerometry (conventionally at the waist) are both known to underestimate sleep duration relative to polysomnography because they process evidence of movement/non-movement, which may or may not be exactly tied to underlying encephalographic patterns and disturbances.11 Nonetheless, normative data for polysomnography-determined sleep period time among similarly aged children averages 504–540 min, with extremes ranging from 388 to 692 min.17 Although our range is somewhat broader (a desirable state for epidemiological analyses) in this large and global field-based sample, our average value is well within these normative values. Previous estimates of total sleep time derived from waist-worn ActiGraph accelerometry in 10-year-old Danish children ranged from 533.1 to 562.5 min, depending on the specific algorithm and instrument filter used; values for concurrent wrist-worn accelerometry ranged from 467.9 to 498.1 min.18 Our own ISCOLE waist-worn accelerometry data are also in agreement with these similarly collected Danish data and perform in an expected manner relative to the wrist-worn data collection, as it is known that the arms may move more during sleep than the torso.19 Compared with self-reported behavior of similarly aged children,20 the accelerometer-determined average sleep period time for ISCOLE children was less (8.8 versus 10.2 h per night) than the average sleep duration (time in bed) of similarly aged children, and the calculated midpoint of sleep was also later (0243 versus 0136 hours). The National Sleep Foundation21 recommends that school-aged children accumulate 9–11 h of sleep per night (although the evidential basis of this recommendation has been questioned22). In ISCOLE, 57.7% of the sample accumulated less than this recommended range and 7.8% accumulated more than this range based on these waist-worn accelerometer-determined data.
The TSET (which excludes nocturnal wake episodes in its calculation) actually agreed almost completely with the overall estimate of total sleep period time (which includes all waking episodes occurring between the nocturnal sleep onset and offset clock times). The lack of apparent difference between these two variables may be particularly characteristic of 9–11-year-old children; it is plausible that there will be more discrepancy in these two variables in older samples and clinical populations. Although calculated sleep episode efficiency suggests almost perfectly peaceful sleep among ISCOLE participants worldwide, our proposed restful sleep efficiency parameter displays a greater diversity of values (and therefore may prove to be ultimately more useful) depending on the use of an absolute versus a relative definition of non-movement during the TSET in ostensibly healthy and young children.
As a single illustrative example, we compared select accelerometer-determined sleep-related variables split by the sample's midpoint clock time. Large effect size differences were evident between dichotomously chronotyped early and late sleepers for nocturnal sleep onset and offset. Future analyses may consider the combined and separate effects of sleep duration indicators (for example, sleep period time and TSET) with chronotype (perhaps more extremely defined than a simple mean split) or other sleep-related variables relative to various health indictors, including relative obesity. Polysomnography has shown reduced sleep amount and quality variables in overweight 10-year-old children.23 In addition, accelerometer-determined short sleep duration has been shown to be a risk factor for overweight and obesity in a sample of children with a mean age of 9.6 years.24
We maximized the utility of the ISCOLE 24-h waist-worn accelerometry data collected in over 7000 children worldwide to make inferences about sleep/wake durations and patterns based on digital evidence of movement/non-movement. This approach clearly differs from clinical assessment of sleep using polysomnography, which comprises a broad and simultaneously collected array of electroencephalography, electrooculography, electromyography and electrocardiography inputs. This obvious methodological discrepancy does not in itself discredit either the need or the opportunity to study sleep-related behaviors in large-field-based epidemiological studies. Ignoring the wealth of data collected in ISCOLE as a result of implementing a 24-h protocol would be unethical given the contributions of the volunteer research participants and the efforts of the legion of scientists and staff involved in similar projects. As little infrastructure existed to organize, categorize and present sleep-related variables collected using a 24-h waist-worn accelerometry protocol, we have been compelled to provide a clear presentation and rationale for the derived nocturnal sleep-related variables and their definitions building off the work of scientists who have built a similar infrastructure for wrist-based nighttime actigraphy.1 ISCOLE is a study of 9–11-year-old children; however, the suggested sleep-related accelerometer-based variables amassed in Table 1 should also be relevant to other population groups and will likely evolve in the future when additional information and consensus arise.
Evaluation of children's sleep duration and patterns is relevant to the study of obesity and metabolic syndrome (among other pediatric health concerns) and is therefore a meaningful pursuit to the advancement of children's health.25 Pediatric sleep researchers have reported nocturnal sleep-related variables applicable to wrist-worn actigraphy data; however, this is the first attempt to identify and define similar variables from children's waist-worn 24-h free-living accelerometry data. These variables extend the study of accelerometer-determined sleep period time (anchored by nocturnal sleep onset and offset) by distinguishing and categorizing the underlying robust patterns of accelerometer data characterized by evident movement/non-movement signals conveying magnitude, duration, frequency and periodicity during the nocturnal TSET. It is important to acknowledge that this approach is not sensitive to daytime napping behaviors and makes broad assumptions about the generally nocturnal nature of sleep in a population. Our hope is that future analysts will evaluate and continue to improve upon these variables, ultimately advancing the study of whole-human behavior (including sleep, physical activity and sedentary time) across the closed system of the 24-h day.
Acknowledgments
We thank the ISCOLE External Advisory Board and the ISCOLE participants and their families who made this study possible. A membership list of the ISCOLE Research Group and External Advisory Board is included in Katzmarzyk et al. (this issue). ISCOLE was funded by The Coca-Cola Company.
Footnotes
MF has received a research grant from Fazer Finland and has received an honorarium for speaking for Merck. AK has been a member of the Advisory Boards of Dupont and McCain Foods. RK has received a research grant from Abbott Nutrition Research and Development. VM is a member of the Scientific Advisory Board of Actigraph and has received an honorarium for speaking for The Coca-Cola Company. TO has received an honorarium for speaking for The Coca-Cola Company. The remaining authors declare no conflict of interest.
References
- Meltzer LJ, Montgomery-Downs HE, Insana SP, Walsh CM. Use of actigraphy for assessment in pediatric sleep research. Sleep Med Rev 2012; 16: 463–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinder JR, Lee KA, Thompson H, Hicks K, Topp K, Madsen KA. Validation of a hip-worn accelerometer in measuring sleep time in children. J Pediatr Nurs 2012; 27: 127–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cain KL, Sallis JF, Conway TL, Van Dyck D, Calhoon L. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health 2013; 10: 437–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swartz AM, Strath SJ, Bassett Jr DR, O'Brien WL, King GA, Ainsworth BE. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Med Sci Sports Exerc 2000; 32: S450–S456. [DOI] [PubMed] [Google Scholar]
- Rosenberger ME, Haskell WL, Albinali F, Mota S, Nawyn J, Intille S. Estimating activity and sedentary behavior from an accelerometer on the hip or wrist. Med Sci Sports Exerc 2013; 45: 964–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor-Locke C, Barreira TV, Schuna Jr JM. Comparison of step outputs for waist and wrist accelerometer attachment sites. Med Sci Sports Exerc 2015; 47: 839–842. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Camhi SM, Troiano RP. A catalog of rules, variables, and definitions applied to accelerometer data in the National Health and Nutrition Examination Survey, 2003-2006. Prev Chronic Dis 2012; 9: E113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 2008; 40: 181–188. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Barreira TV, Schuna JM Jr., Mire EF, Katzmarzyk PT. Fully automated waist-worn accelerometer algorithm for detecting children's sleep period time separate from 24-hour physical activity or sedentary behaviors. Appl Physiol Nutr Metab 2014; 39: 53–57. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Barreira TV, Schuna Jr JM, Mire EF, Chaput JP, Fogelholm M et al. Improving wear time compliance with a 24-hour waist-worn accelerometer protocol in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE). Int J Behav Nutr Phys Act 2015; 12: 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A, Sharkey KM, Carskadon MA. Activity-based sleep-wake identification: an empirical test of methodological issues. Sleep 1994; 17: 201–207. [DOI] [PubMed] [Google Scholar]
- Barreira TV, Schuna Jr JM, Mire EF, Katzmarzyk PT, Chaput JP, Leduc G et al. Identifying Children's Nocturnal Sleep Using 24-h Waist Accelerometry. Med Sci Sports Exerc 2015; 47: 937–943. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput J-P, Fogelholm M et al. The International Study of Childhood Obesity Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health 2013; 13: 900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Westin AM. A comparison of actigraphy scoring rules used in pediatric research. Sleep Med 2011; 12: 793–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR et al. Amount of time spent in sedentary behaviors in the United States, 2003-2004. Am J Epidemiol 2008; 167: 875–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mark AE, Janssen I. Dose-response relation between physical activity and blood pressure in youth. Med Sci Sports Exerc 2008; 40: 1007–1012. [DOI] [PubMed] [Google Scholar]
- Scholle S, Beyer U, Bernhard M, Eichholz S, Erler T, Graness P et al. Normative values of polysomnographic parameters in childhood and adolescence: quantitative sleep parameters. Sleep Med 2011; 12: 542–549. [DOI] [PubMed] [Google Scholar]
- Hjorth MF, Chaput JP, Damsgaard CT, Dalskov S, Michaelsen KF, Tetens I et al. Measure of sleep and physical activity by a single accelerometer: can a waist-worn actigraph adequately measure sleep in children. Sleep Biol Rhythms 2012; 10: 328–335. [Google Scholar]
- Galland B, Meredith-Jones K, Terrill P, Taylor R. Challenges and emerging technologies within the field of pediatric actigraphy. Front Psychiatry 2014; 5: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbabi T, Vollmer C, Dorfler T, Randler C. The influence of chronotype and intelligence on academic achievement in primary school is mediated by conscientiousness, midpoint of sleep and motivation. Chronobiol Int 2015; 32: 349–357. [DOI] [PubMed] [Google Scholar]
- Hirshkowitz M, Whiton K, Albert SM, Alessi CA, Bruni O, DonCarlos L et al. National Sleep Foundation's sleep time duration recommendations: methodology and results summary. Sleep Health 2015; 1: 40–43. [DOI] [PubMed] [Google Scholar]
- Matricciani L, Blunden S, Rigney G, Williams MT, Olds TS. Children's sleep needs: is there sufficient evidence to recommend optimal sleep for children? Sleep 2013; 36: 527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamorro R, Algarin C, Garrido M, Causa L, Held C, Lozoff B et al. Night time sleep macrostructure is altered in otherwise healthy 10-year-old overweight children. Int J Obes (Lond) 2014; 38: 1120–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Lambert M, Gray-Donald K, McGrath JJ, Tremblay MS, O'Loughlin J et al. Short sleep duration is independently associated with overweight and obesity in Quebec children. Can J Public Health 2011; 102: 369–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazaratou H, Soldatou A, Dikeos D. Medical comorbidity of sleep disorders in children and adolescents. Curr Opin Psychiatry 2012; 25: 391–397. [DOI] [PubMed] [Google Scholar]