Abstract
OBJECTIVES:
Reports of inverse associations between breakfast frequency and indices of obesity are predominantly based on samples of children from high-income countries with limited socioeconomic diversity. Using data from the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE), the present study examined associations between breakfast frequency and adiposity in a sample of 9–11-year-old children from 12 countries representing a wide range of geographic and socio-cultural variability.
METHODS:
Multilevel statistical models were used to examine associations between breakfast frequency (independent variable) and adiposity indicators (dependent variables: body mass index (BMI) z-score and body fat percentage (BF%)), adjusting for age, sex, and parental education in 6941 children from 12 ISCOLE study sites. Associations were also adjusted for moderate-to-vigorous physical activity, healthy and unhealthy dietary patterns and sleep time in a sub-sample (n=5710). Where interactions with site were significant, results were stratified by site.
RESULTS:
Adjusted mean BMI z-score and BF% for frequent breakfast consumers were 0.45 and 20.5%, respectively. Frequent breakfast consumption was associated with lower BMI z-scores compared with occasional (P<0.0001, 95% confidence intervals (CI): 0.10–0.29) and rare (P<0.0001, 95% CI: 0.18–0.46) consumption, as well as lower BF% compared with occasional (P<0.0001, 95% CI: 0.86–1.99) and rare (P<0.0001, 95% CI: 1.07–2.76). Associations with BMI z-score varied by site (breakfast by site interaction; P=0.033): associations were non-significant in three sites (Australia, Finland and Kenya), and occasional (not rare) consumption was associated with higher BMI z-scores compared with frequent consumption in three sites (Canada, Portugal and South Africa). Sub-sample analyses adjusting for additional covariates showed similar associations between breakfast and adiposity indicators, but lacked site interactions.
CONCLUSIONS:
In a multinational sample of children, more frequent breakfast consumption was associated with lower BMI z-scores and BF% compared with occasional and rare consumption. Associations were not consistent across all 12 countries. Further research is required to understand global differences in the observed associations.
Introduction
The prevalence of overweight and obesity among children is a major global health concern1 that now extends beyond high-income nations to low- and middle- income nations.2 Childhood overweight and obesity is the result of a complex interaction of behavioral, biological and environmental factors that impact long-term energy balance. There is a common belief that one such factor, breakfast consumption, is the ‘most important meal of the day', providing potential nutritional and health-related benefits. While rates of childhood overweight and obesity remain high in most high-income nations,3 around a third of children and adolescents (young people) report regularly skipping breakfast.4 Similar rates of breakfast skipping have been reported more recently in low-income nations, where overweight and obesity are rising.5, 6
Cross-sectional studies have consistently shown the frequency of breakfast consumption to be inversely associated with measures of overweight and obesity (most often quantified via body mass index (BMI)) in young people.7, 8, 9 Since results from interventions are unclear,9, 10, 11 the question remains as to whether consuming breakfast regularly causes a reduction in BMI or whether breakfast consumption is an indicator of healthy lifestyle habits (for example, higher physical activity) related to lower body weight.9
Indeed, it may be expected that more frequent breakfast consumption would add to daily energy intake and thus be associated with a higher BMI in some cases. In particular, it is possible that associations between breakfast consumption and BMI may not be consistent across different regions of the world in children with diverse cultural and socioeconomic backgrounds.
Multinational studies have shown that the inverse relationship between breakfast frequency and measures of overweight and obesity is consistent among adolescents from nine European countries,12 and that ‘daily' compared with ‘less than daily' breakfast consumption was the only dietary factor of those assessed (that is, daily fruit, vegetable and soft drink consumption) to be consistently and inversely associated with overweight in 11–15-year olds from 41 countries, including Europe, the United States, Canada and Israel.13 However, to date, no multinational study of the association between breakfast frequency and adiposity has included a truly global range of countries beyond these regions.
Although single country studies have shown similar associations between breakfast and measures of overweight and obesity in India,5 Iran,14 Brazil,15 China16 and Oran (Algeria),17 a meta-analysis of Asian and Pacific regions noted that the strength of these associations was heterogeneous.18 Moreover, it is often not possible to directly compare the findings of single-nation studies owing to methodological inconsistencies. In particular, between-study differences in the definition of ‘breakfast consumption' may affect reported associations with BMI.19
Using data from the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE), the purpose of the present study was twofold. First, to describe the frequency of breakfast consumption in 9–11-year olds from study sites in 12 countries spread across all major geographic regions of the world (Asia, Africa, Europe, the Americas and Oceania) and, second, to examine associations between breakfast frequency and adiposity indicators across these 12 countries.
Materials and methods
Participants and study design
The ISCOLE sites were located in 12 different countries representing a wide range of economic development (low-to-high income), Human Development Index (0.509 in Kenya to 0.929 in Australia) and inequality (GINI coefficient; 26.9 in Finland to 63.1 in South Africa).20 The Pennington Biomedical Research Center Institutional Review Board approved the ISCOLE protocol with ethical review boards at each site approving local protocols. All sites followed the standardized protocol with all study personnel undergoing training and certification in the data collection methods; the design and methods used for data collection are described in more detail elsewhere.20 Recruitment targeted a sex-balanced sample of 500 children from each site aged between 9 and 11 years. By design, the intent was not to have nationally representative samples, rather a sample deliberately stratified by socioeconomic status was used in each site to maximize variability. Of the 7372 children who participated in ISCOLE in total, 6841 remained in the present analytic sample after excluding participants with missing data for weekday or weekend day breakfast frequency (n=165) and highest level of parental education (n=366). A sub-sample of 5710 participants were analyzed after excluding those with additional missing data for moderate-to-vigorous physical activity (MVPA; n=678), healthy and unhealthy dietary patterns (n=95) and sleep time (n=358).
Assessment of adiposity indicators
A battery of anthropometric measurements was taken by local research staff trained in the ISCOLE protocol.20 Standing height was measured to the nearest 0.1 cm with the participant standing without shoes, their head in the Frankfort Plane and at the end of a deep inhalation using a Seca 213 portable stadiometer (Seca Corporation, Hamburg, Germany). Body mass and body fat percentage (BF%) were measured to the nearest 0.1 kg and 0.1%, respectively, using a portable Tanita SC-240 Body Composition Analyzer (TANITA Corporation, Tokyo, Japan). Subsequently, BMI (body mass (kg)/height (m2)) and BMI z-score were calculated according to the World Health Organization21 criteria.
Assessment of breakfast frequency
Breakfast frequency was assessed by asking participants the following question: ‘How often do you usually have breakfast (more than a glass of milk or fruit juice)?' Participants were asked to indicate their response separately for weekdays and for weekend days. Response categories were ‘never' to ‘five days' for the week, and ‘never' to ‘two days' for the weekend. Subsequently, weekly breakfast frequency (0 to 7 days per week) was calculated as the sum of weekday and weekend day breakfast frequency.
Due to inconsistencies in the definition of ‘breakfast consumption' adopted in previous research,5, 7, 13 we employed two different definitions:
Three-category definition: weekly breakfast frequency was recoded to make clear comparisons among rare (consume breakfast on 0–2 days per week), occasional (consume breakfast on 3–5 days per week) and frequent (consume breakfast on 6–7 days per week) breakfast consumers.
Two-category definition: weekly breakfast frequency was recoded as less than daily (consume breakfast on 0–6 days per week) or daily (consume breakfast on 7 days per week).
The three-category definition was the primary variable for our analyses, to allow us to distinguish between the effects of rare, occasional and frequent consumption. The main purpose of including the two-category definition of ‘less than daily' and ‘daily' consumption was to enable direct comparisons of our data to that of a previous multinational study.4, 13
Covariates
Demographic questionnaires completed by parents were used to determine age, sex and the highest level of parental education for each participant; full details have been published elsewhere.20 Response categories for level of parental education were: less than high school, some high school, completed high school, some college degree, bachelor's degree or postgraduate degree (master's or PhD). Subsequently, highest level of parental education was recoded into three categories: did not complete high school, completed high school or some college and completed bachelor's or postgraduate degree.
The children reported their usual consumption frequency of 23 different food groups using a validated food frequency questionnaire.22 To identify existing dietary patterns among the children, principal components analysis using the food frequency questionnaire food groups as input variables were carried out. More information about the dietary assessment methods and the identification of dietary patterns can be found elsewhere.22, 23 Briefly, two components were chosen then rotated with an orthogonal varimax transformation to enhance the interpretation, and named as ‘unhealthy dietary pattern' (characterized by high intakes of, for example, fast foods, ice cream, fried food, French fries and potato chips) and ‘healthy dietary pattern' (including dark-green vegetables, orange vegetables, vegetables in general and fruits and berries). Standardized principal component scores were used for both dietary patterns.
The Actigraph GT3X+ accelerometer (ActiGraph LLC, Pensacola, FL, USA) was used to objectively monitor physical activity and nightly sleep duration (sleep time), across 7 days; full details have been published elsewhere.20 Participants were encouraged to wear the accelerometer 24 h per day for at least 7 days, including 2 weekend days. The minimal amount of accelerometer data that was considered acceptable to determine time in MVPA was 4 days with at least 10 h of awake wear time per day, including at least 1 weekend day. After determining non-wear time and sleep time,24 time in MVPA was calculated using the Evenson cut-offs.25 Sleep time was estimated from the accelerometry data using a fully automated algorithm for 24-h waist-worn accelerometers that was recently validated for ISCOLE.26 Weekly total sleep time averages were calculated using only days where valid sleep was accumulated (total sleep episode time ⩾160 min) and only for participants with at least 3 nights of valid sleep, including 1 weekend night (Friday or Saturday).
Statistical analyses
SAS 9.1 (SAS Institute, Cary, NC, USA) was used for statistical analyses. For descriptive purposes, the characteristics of the study population and frequencies of breakfast consumption (using the two definitions) were produced for all participating sites. Multilevel models (SAS PROC MIXED) with participants (level 1) nested within schools (level 2) and country (level 3) (three-level random intercept model) were used to examine associations between breakfast frequency (independent variable) and adiposity indicators (dependent variables; BMI z-score and BF%), adjusting for age, sex and highest parental education (model 1 covariates). In a sub-sample of participants, we also adjusted for MVPA, healthy and unhealthy dietary patterns, and sleep time (model 2 covariates). The use of multilevel models controlled for the hierarchical nature of variables at levels 2 and 3, thus allowing for estimation of random intercepts (that is, allowing the dependent variable to vary between sites) and the examination of interactions with site. Where interactions were significant, results were stratified by site. All analyses were performed with the two different definitions of breakfast consumption. Statistical significance was set at P⩽0.05.
Results
Participants and frequency of breakfast consumption
Descriptive statistics of the participants according to site are displayed in Table 1. The sites with the lowest BMI were Kenya, Colombia and Finland and the sites with the highest were Brazil, Portugal and the United States. BF% was lowest in Kenya and Finland and highest in Brazil and the United States. South Africa and Colombia had the lowest levels of parental education, with India and Canada having the highest.
Table 1. Descriptive characteristics of the sample stratified by site.
| Site (n) |
Sex (%)a |
Age (years)b | Height (cm)b | Body mass (kg)b | BMI (kg m−2)b | BMI z-score (WHO)b | BF%b |
Highest level of parental education (%)a |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys | Girls | High | Medium | Low | |||||||
| Australia | 54 | 46 | 10.7 | 144.8 | 40.1 | 18.9 | 0.62 | 21.7 | 41 | 48 | 12 |
| (n=513) | (0.4) | (7.1) | (9.4) | (3.3) | (1.12) | (7.3) | |||||
| Brazil | 51 | 49 | 10.5 | 144.0 | 41.4 | 19.8 | 0.87 | 23.1 | 24 | 53 | 24 |
| (n=492) | (0.5) | (7.3) | (11.8) | (4.4) | (1.40) | (9.2) | |||||
| Canada | 58 | 42 | 10.5 | 143.8 | 38.0 | 18.2 | 0.39 | 20.5 | 72 | 26 | 2 |
| (n=533) | (0.4) | (7.2) | (9.1) | (3.3) | (1.19) | (7.4) | |||||
| China | 47 | 53 | 9.9 | 141.2 | 38.1 | 18.9 | 0.71 | 20.5 | 23 | 45 | 33 |
| (n=545) | (0.5) | (7.0) | (10.8) | (4.1) | (1.50) | (8.0) | |||||
| Colombia | 50 | 50 | 10.5 | 137.7 | 33.6 | 17.6 | 0.21 | 20.0 | 17 | 51 | 32 |
| (n=915) | (0.6) | (7.0) | (7.1) | (2.5) | (1.04) | (5.8) | |||||
| Finland | 52 | 48 | 10.5 | 144.3 | 37.2 | 17.8 | 0.26 | 18.9 | 42 | 55 | 3 |
| (n=491) | (0.4) | (6.5) | (7.7) | (2.7) | (1.07) | (6.8) | |||||
| India | 53 | 47 | 10.4 | 141.1 | 36.0 | 18.0 | 0.24 | 21.7 | 74 | 22 | 5 |
| (n=601) | (0.5) | (6.8) | (8.5) | (3.3) | (1.37) | (7.5) | |||||
| Kenya | 53 | 47 | 10.2 | 139.0 | 33.8 | 17.3 | 0.05 | 16.6 | 41 | 45 | 14 |
| (n=540) | (0.7) | (7.5) | (8.3) | (3.1) | (1.23) | (7.8) | |||||
| Portugal | 56 | 44 | 10.4 | 143.3 | 40.2 | 19.4 | 0.87 | 22.8 | 21 | 33 | 47 |
| (n=686) | (0.3) | (6.9) | (9.3) | (3.4) | (1.15) | (7.5) | |||||
| South Africa | 60 | 40 | 10.3 | 138.6 | 35.0 | 18.0 | 0.30 | 21.1 | 13 | 39 | 47 |
| (n=439) | (0.7) | (7.6) | (9.2) | (3.6) | (1.29) | (8.0) | |||||
| UK | 55 | 45 | 10.9 | 145.2 | 39.3 | 18.5 | 0.41 | 20.8 | 45 | 52 | 3 |
| (n=469) | (0.5) | (7.3) | (8.9) | (3.1) | (1.11) | (7.0) | |||||
| US | 57 | 43 | 10.0 | 141.1 | 38.5 | 19.1 | 0.80 | 23.1 | 47 | 44 | 9 |
| (n=617) | (0.6) | (7.6) | (11.0) | (4.1) | (1.31) | (8.3) | |||||
| All sites | 54 | 46 | 10.4 | 141.7 | 37.4 | 18.4 | 0.48 | 20.9 | 38 | 42 | 20 |
| (n=6841) | (0.6) | (7.6) | (9.6) | (3.5) | (1.26) | (7.7) | |||||
Abbreviations: BF%, body fat percentage; BMI, body mass index; WHO, World Health Organization.
Values are frequencies (%) for categorical variables.
Values are means (s.d.) for continuous variables.
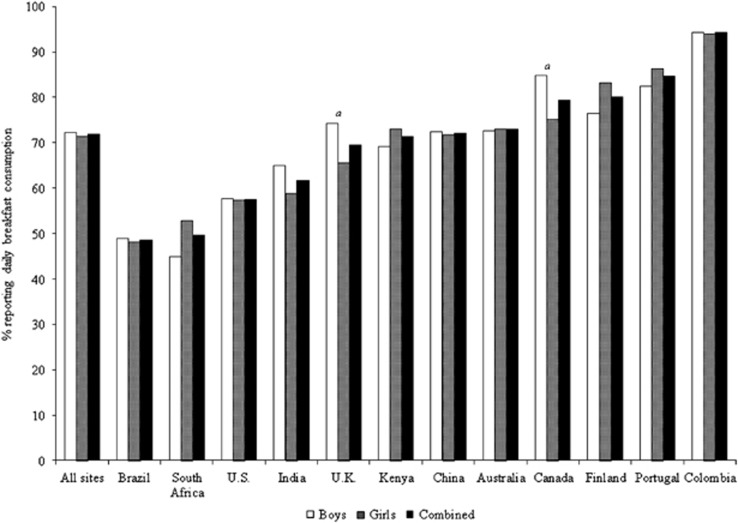
Table 2 shows the number of days (mean (standard deviation)) participants reported consuming breakfast for weekdays, weekend days and across the week, and the percentage of participants within each breakfast frequency category (using the two definitions), stratified by site and sex. To provide a clear direct comparison with a previous multinational study,4 Figure 1 compares the ranking of the sites according to the percentage of children reporting daily breakfast consumption (using the two-category definition). Weekday, weekend day and weekly breakfast consumption were lowest in Brazil and highest in Colombia. Using the two-category definition, daily breakfast consumption ranged from <50% in South Africa and Brazil to >80% in Portugal, Colombia and Finland. Using the three-category definition, the two sites with the lowest percentage of frequent breakfast consumers were Brazil and South Africa (<65%) and the two sites with the highest were Colombia and Portugal (>90%), the percentage of occasional consumers was lowest in Colombia and Portugal (<5%) and highest in Brazil and South Africa (>20%), and the percentage of rare breakfast consumers was lowest in Colombia and in Finland (<2%) and highest in Brazil and India (>15%).
Table 2. Frequency of breakfast consumption stratified by site and sex.
| Site |
Days of breakfast consumptiona |
Three-category breakfast definitionb |
Two-category breakfast definitionb |
|||||
|---|---|---|---|---|---|---|---|---|
| Weekday | Weekend | Weekly | Rare (%) | Occasional (%) | Frequent (%) | Less than daily (%) | Daily (%) | |
| Australia | ||||||||
| Boys | 4.5 (1.2)c | 1.8 (0.6) | 6.3 (1.5) | 4.6 | 13.1 | 82.3 | 27.4 | 72.6 |
| Girls | 4.3 (1.5) | 1.8 (0.5) | 6.1 (1.8) | 8.7 | 12.7 | 78.6 | 26.8 | 73.2 |
| Combined | 4.4 (1.4) | 1.8 (0.5) | 6.2 (1.7) | 6.8 | 12.9 | 80.3 | 27.1 | 72.9 |
| Brazil | ||||||||
| Boys | 3.8 (3.6)c | 1.6 (1.5) | 5.4 (2.1) | 15.8 | 21.2 | 63.1 | 51.0 | 49.0 |
| Girls | 3.5 (3.2) | 1.6 (1.6) | 5.1 (2.2) | 17.5 | 27.5 | 55.0 | 51.8 | 48.2 |
| Combined | 3.6 (1.8) | 1.6 (0.7) | 5.2 (2.1) | 16.7 | 24.4 | 58.9 | 51.4 | 48.6 |
| Canada | ||||||||
| Boys | 4.7 (1.0)c | 1.9 (1.8) | 6.6 (1.2) | 2.7 | 7.6 | 89.8 | 15.1 | 84.9d |
| Girls | 4.5 (1.2) | 1.9 (1.8) | 6.4 (1.3) | 4.2 | 11.0 | 84.7 | 24.7 | 75.3 |
| Combined | 4.6 (1.1) | 1.9 (0.4) | 6.5 (1.3) | 3.6 | 9.6 | 86.9 | 20.6 | 79.4 |
| China | ||||||||
| Boys | 4.5 (1.2) | 1.8 (0.5) | 6.3 (1.5) | 4.8 | 12.4 | 82.8 | 27.6 | 72.4 |
| Girls | 4.5 (1.2) | 1.8 (0.5) | 6.3 (1.4) | 3.5 | 14.1 | 82.4 | 28.2 | 71.8 |
| Combined | 4.5 (1.2) | 1.8 (0.5) | 6.3 (1.5) | 4.2 | 13.2 | 82.6 | 27.9 | 72.1 |
| Colombia | ||||||||
| Boys | 4.9 (0.7) | 2.0 (0.2) | 6.9 (0.7) | 1.3 | 2.2 | 96.5 | 5.7 | 94.3 |
| Girls | 4.8 (0.8) | 2.0 (0.1) | 6.8 (0.8) | 2.2 | 3.0 | 94.8 | 5.9 | 94.1 |
| Combined | 4.9 (0.8) | 2.0 (0.2) | 6.8 (0.8) | 1.8 | 2.6 | 95.6 | 5.8 | 94.2 |
| Finland | ||||||||
| Boys | 4.5 (1.1) | 1.9 (0.3) | 6.4 (1.2) | 2.6 | 12.4 | 85.0 | 23.5 | 76.5 |
| Girls | 4.7 (0.9) | 2.0 (0.2)e | 6.7 (0.9)e | 1.2 | 9.3 | 89.5 | 16.7 | 83.3 |
| Combined | 4.6 (1.0) | 1.9 (0.3) | 6.5 (1.1) | 1.8 | 10.8 | 87.4 | 20.0 | 80.0 |
| India | ||||||||
| Boys | 4.0 (3.8)c | 1.8 (0.4) | 5.8 (1.9) | 12.8 | 13.5 | 73.8 | 35.1 | 64.9 |
| Girls | 3.6 (3.4) | 1.9 (0.4) | 5.5 (2.1) | 16.6 | 18.5 | 64.9 | 41.1 | 58.9 |
| Combined | 3.8 (1.9) | 1.9 (0.4) | 5.7 (2.0) | 14.8 | 16.1 | 69.1 | 38.3 | 61.7 |
| Kenya | ||||||||
| Boys | 4.2 (1.5) | 1.8 (0.4) | 6.0 (1.7) | 6.3 | 18.6 | 75.1 | 30.8 | 69.2 |
| Girls | 4.3 (1.4) | 1.9 (0.4) | 6.2 (1.6) | 3.5 | 16.4 | 80.1 | 26.8 | 73.2 |
| Combined | 4.3 (1.4) | 1.9 (0.4) | 6.1 (1.6) | 4.8 | 17.4 | 77.8 | 28.7 | 71.3 |
| Portugal | ||||||||
| Boys | 4.8 (4.7) | 1.8 (0.4) | 6.6 (1.2) | 3.0 | 5.0 | 92.0 | 17.6 | 82.4 |
| Girls | 4.8 (4.7) | 1.9 (0.4)e | 6.7 (1.0) | 2.1 | 3.9 | 94.0 | 13.5 | 86.5 |
| Combined | 4.8 (0.9) | 1.9 (0.4) | 6.7 (1.1) | 2.5 | 4.4 | 93.2 | 15.3 | 84.7 |
| South Africa | ||||||||
| Boys | 3.8 (3.5) | 1.6 (0.6) | 5.4 (1.9) | 12.5 | 25.6 | 61.9 | 55.1 | 44.9 |
| Girls | 3.9 (3.8) | 1.7 (0.6) | 5.6 (1.8) | 9.5 | 23.6 | 66.9 | 47.2 | 52.9 |
| Combined | 3.9 (1.6) | 1.7 (0.6) | 5.6 (1.9) | 10.7 | 24.4 | 64.9 | 50.3 | 49.7 |
| UK | ||||||||
| Boys | 4.5 (1.2)c | 1.8 (0.5) | 6.3 (1.5) | 4.8 | 11.9 | 83.3 | 25.7 | 74.3d |
| Girls | 4.2 (1.4) | 1.8 (0.5) | 6.0 (1.7) | 6.6 | 17.0 | 76.5 | 34.4 | 65.6 |
| Combined | 4.3 (1.3) | 1.8 (0.5) | 6.1 (1.6) | 5.8 | 14.7 | 79.5 | 30.5 | 69.5 |
| US | ||||||||
| Boys | 4.2 (1.5) | 1.7 (0.6) | 5.9 (1.8) | 9.4 | 18.0 | 72.7 | 42.3 | 57.7 |
| Girls | 4.1 (1.5) | 1.7 (0.5) | 5.8 (1.8) | 8.6 | 20.9 | 70.6 | 42.6 | 57.4 |
| Combined | 4.1 (1.5) | 1.7 (0.6) | 5.8 (1.8) | 8.9 | 19.6 | 71.5 | 42.5 | 57.5 |
| All sites | ||||||||
| Boys | 4.4 (1.3)c | 1.8 (0.48)e | 6.2 (1.6) | 6.3 | 12.4 | 81.4 | 27.7 | 72.3 |
| Girls | 4.3 (1.4) | 1.8 (0.44) | 6.1 (1.6) | 6.7 | 14.0 | 79.4 | 28.4 | 71.6 |
| Combined | 4.4 (1.4) | 1.8 (0.5) | 6.2 (1.6) | 6.5 | 13.2 | 80.3 | 28.1 | 71.9 |
Values are means (s.d.) for continuous variables.
Values are frequencies (%) for categorical variables.
Higher in boys compared with girls at the site level using independent t-tests (P<0.05).
Higher in boys compared with girls at the site level using χ2 tests (P<0.05).
Higher in girls compared with boys at the site level using independent t-tests (P<0.05).
Figure 1.
Ranking of the frequency of daily breakfast consumption (%) stratified by site and sex. aSignificant difference between boys and girls.
When all sites were combined, boys consumed breakfast on more weekdays than girls (t=2.70; P=0.007), whereas girls consumed breakfast on more weekend days (t=−2.75; P=0.006); there was no significant difference in the prevalence of breakfast consumption between boys and girls using the two-category (χ2=0.50; P=0.478) or three-category (χ2=4.54; P=0.103) definitions. Site-specific analyses revealed that weekday breakfast frequency was higher in boys than in girls in Australia (t=2.05; P=0.040), Brazil (t=1.99; P=0.047), Canada (t=2.05; P=0.041), India (t=2.16; P=0.031) and the United Kingdom (t=2.07; P=0.039). Weekend breakfast frequency was higher in girls than in boys in Finland (t=−2.89; P=0.004) and Portugal (t=−2.05; P=0.041). Weekly breakfast frequency was higher in girls compared with boys in Finland (t=−2.23; P=0.026). Using the two-category definition of breakfast consumption, daily breakfast consumption was higher in boys compared with girls in Canada (χ2=7.26; P=0.007) and the United Kingdom (χ2=4.09; P=0.043), but there was no difference in the frequency of rare, occasional and frequent consumption when applying the three-group definition.
Associations between breakfast frequency and adiposity indicators
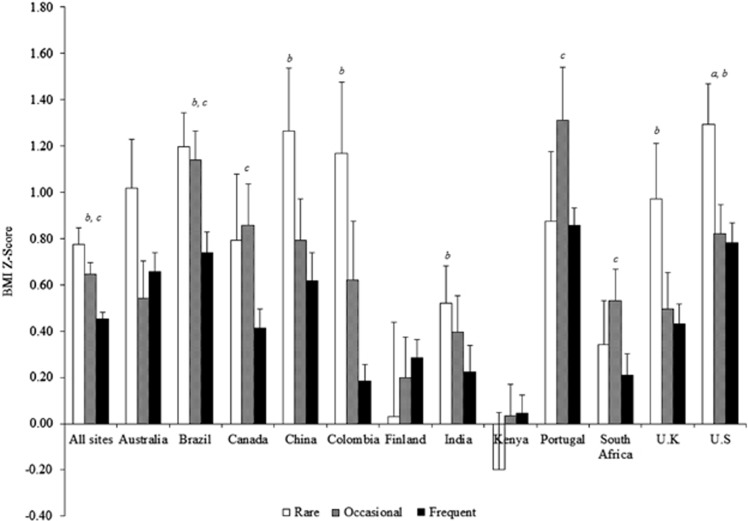
Multilevel analysis of associations between breakfast frequency using the three-category definition and adiposity indicators are presented in Table 3. There was a main effect on BMI z-score and BF% both indicators of adiposity were higher in rare versus frequent breakfast consumers, and in occasional versus frequent breakfast consumers, but not different between rare versus occasional breakfast consumers. Significant interactions by site were found for BMI z-score, but not BF%. Subsequently, analyses for BMI z-score were stratified by site and shown in Figure 2.
Table 3. Multilevel modeling analysis of differences in adiposity indicators between rare (consume breakfast on 0–2 days per week), occasional (consume breakfast on 3–5 days per week) and frequent (consume breakfast on 6–7 days per week) breakfast consumers.
|
Full sample (n=6841) |
Sub-sample (n=5710) |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Adjusteda |
P-value for main effects |
P-value (95% CI) for differences between breakfast categoriesb |
Adjusteda |
P-value for main effects |
P-value (95% CI) for differences between breakfast categoriesb |
|||||||||||
| Rare (n=445) | Occasional (n=904) | Frequent (n=5492) | Breakfast main effect | Breakfast × site interaction | Rare versus frequent | Occasional versus frequent | Rare versus occasional | Rare (n=362) | Occasional (n=714) | Frequent (n=4634) | Breakfast main effect | Breakfast × site interaction | Rare versus frequent | Occasional versus frequent | Rare versus occasional | |
| Model 1c | ||||||||||||||||
| BMI Z-score (WHO) | 0.77 (0.63–0.92) | 0.65 (0.55–0.74) | 0.45 (0.40–0.51) | <0.0001 | 0.033 | <0.0001 (0.18–0.46) | <0.0001 (0.10–0.29) | 0.131 (−0.04–0.30) | 0.80 (0.64–0.96) | 0.65 (0.55–0.76) | 0.42 (0.37–0.47) | <0.0001 | 0.211 | <0.0001 (0.22–0.54) | <0.0001 (0.13–0.34) | 0.135 (−0.04–0.33) |
| BF% | 22.4 (21.6–23.3) | 21.9 (21.3–22.5) | 20.5 (20.2–20.9) | <0.0001 | 0.088 | <0.0001 (1.07–2.76) | <0.0001 (0.86–1.99) | 0.324 (−0.48–1.47) | 22.5 (21.5–23.4) | 21.9 (21.3–22.6) | 20.3 (20.0–20.1) | <0.0001 | 0.073 | <0.0001 (1.19–3.08) | <0.0001 (0.95–2.21) | 0.317 (−0.54–1.65) |
| Model 2d | ||||||||||||||||
| BMI Z-score (WHO) | NA | 0.80 (0.64–0.95) | 0.68 (0.58–0.78) | 0.44 (0.39–0.49) | <0.0001 | 0.334 | <0.0001 (0.20–0.51) | <0.0001 (0.13–0.34) | 0.201 (−0.06–0.30) | |||||||
| BF% | 22.5 (21.6–23.4) | 22.1 (21.5–22.7) | 20.5 (20.2–20.9) | <0.0001 | 0.094 | <0.0001 (1.03–2.87) | <0.0001 (0.95–2.17) | 0.472 (−0.67–1.45) | ||||||||
Abbreviations: BF%, body fat percentage; BMI, body mass index; CI, confidence intervals; NA, not applicable; WHO, world health organization.
Significance accepted at P⩽0.05.
Values are least squares means (95% CI).
Values are differences of least squares means between the breakfast consumption categories.
Model 1 adjusts for age, sex and highest level of parental education.
Model 2 adjusts for age, sex, highest level of parental education, moderate-to-vigorous physical activity, healthy and unhealthy dietary patterns and sleep time.
Figure 2.
Multilevel modeling analysis of differences in BMI z-score (WHO) between rare (consume breakfast on 0–2 days per week), occasional (consume breakfast on 3–5 days per week) and frequent (consume breakfast on 6–7 days per week) breakfast consumers stratified by site. Values are least squares means (error bars indicate the s.e.m.) adjusted for age, sex and highest level of parental education. aSignificant difference between rare and occasional; bsignificant difference between rare and frequent; csignificant difference between occasional and frequent (P⩽0.05).
Using the two-category definition of breakfast consumption demonstrated similar results when all sites were combined: BMI z-score (0.45 versus 0.63; P<0.0001; 95% CI: 0.12–0.26) and BF% (20.5% versus 21.8% P<0.0001; 95% CI: 0.91–1.74) were lower in daily breakfast consumers compared with those who consumed breakfast less than daily, and significant interactions with site for BMI z-score (P=0.030), but not BF% (P=0.074), were found. At the site level, however, differences were found for BMI z-score in the Brazil, Canada and Colombia sites only (all P⩽0.05).
Sub-sample analyses
Sub-sample analyses for participants with valid data for MVPA, healthy and unhealthy dietary patterns and sleep time (n=5710) are presented in Table 3. Similar to the full sample, when using model 1 to adjust for age, sex and highest parental education only, there was a main effect of breakfast on BMI z-score and BF% both indicators of adiposity were higher in rare versus frequent breakfast consumers, and in occasional versus frequent breakfast consumers, but not different between rare versus occasional breakfast consumers. These differences remained significant when using model 2 to adjust for the additional covariates of MVPA, healthy and unhealthy dietary patterns and sleep time (Table 3). Interactions with site were not significant for BMI z-score or BF% when applying either model 1 or 2 to the sub-sample; the non-significant interaction when applying model 1 to BMI z-score indicated that a lack of statistical power, rather than the adjustment for MVPA, healthy and unhealthy dietary patterns and sleep time, limited the ability of model 2 to detect interactions with site (when compared with analyses of the full sample).
Using the two-category definition of breakfast consumption, applying both models 1 and 2 demonstrated that BMI z-score (model 1: P<0.0001; 95% CI: 0.14 to 0.30; model 2: P<0.0001; 95% CI: 0.15 to 0.30) and BF% (model 1: P<0.0001; 95% CI: 0.15 to 0.30; model 2: P<0.0001; 95% CI: 1.02 to 1.91) were lower in daily breakfast consumers compared with those who consumed breakfast less than daily. Significant interactions with site were found when applying both models for BMI z-score (model 1: P=0.035; model 2: P=0.030) and BF% (model 1: P=0.027; model 2: P=0.011). At the site level, daily breakfast consumers had a lower BMI z-scores compared with less than daily consumers in Brazil, Canada, Colombia and India (all P⩽0.05), and a lower BF% in Brazil, Canada, China, Colombia, India and Kenya (all P⩽0.05).
Discussion
This study is the first to use standardized measures to examine associations between breakfast frequency and adiposity indicators in children from a wide range of geographic and socio-cultural backgrounds. Indeed, associations were examined across sites from all major geographic regions of the world (Asia, Africa, Europe, the Americas and Oceania). Our findings showed frequent breakfast consumption (6–7 days per week) to be associated with lower BMI z-scores and BF% compared with both occasional (3–5 days per week) and rare (0–2 days per week) consumption independent of age, sex and parental education (and MVPA, healthy and unhealthy dietary patterns, and objectively measured sleep time in our sub-sample analyses). However, relationships were not consistently observed across the 12 study sites; some showed no association (Australia, Finland and Kenya), and others showed that occasional, but not rare, consumption was associated with higher BMI z-scores compared with frequent consumption (Canada, Portugal and South Africa).
The lack of a universal definition of the frequency of breakfast consumption has been a major criticism of previous research examining associations with adiposity.7 To this end, we employed two definitions to increase potential for direct comparisons with previous literature. Overall, 71.9% of the sample reported consuming breakfast on a daily basis, with 80.3% being categorized as frequent (6–7 days per week), 13.2% occasional (3–5 days per week) and 6.5% rare (0–2 days per week) breakfast consumers. These values are consistent with previous reviews reporting that 10–30% of young people in Europe and the United States regularly skip breakfast.7 Daily breakfast consumption rates were 7–29% higher (depending on the country) than were reported for older children (that is, 11–15-year olds) in a previous multinational study,4 supporting findings of more frequent breakfast consumption in children compared with adolescents.7, 8 In line with studies showing variability in daily breakfast consumption between European nations, the United States, Canada and Israel,4, 27 daily breakfast consumption in our sample ranged from 48.6% in Brazil to 94.2% in Colombia. Although differences did not appear to be related to the Human Development Index of the country, cultural practices, socioeconomic factors and availability of school-breakfast programs may have contributed disparities in breakfast frequency across countries. For example, many children attending public schools in Colombia receive breakfast on a daily basis during school days as part of the National School Feeding Program,28, 29 which may partly explain the high breakfast frequencies in this site. As only low-to-middle-income children qualify for the program, it should be noted that the Columbian sample was proportional to the distribution of socioeconomic status of the city (80% of the schools had the program). Although systematic reviews report less frequent breakfast consumption in girls compared with boys,7 no between-sex difference was found in 10–12-year olds from 7 European countries30 and minimal differences were apparent in the present sample with the exceptions being lower consumption in girls in Canada and the United Kingdom using the two-category definition.
Consistent with past work,12, 13 most sites showed an inverse association between breakfast frequency and adiposity indicators (BMI z-score and BF%). Furthermore, our sub-sample analyses showed these associations to be independent of MVPA, healthy and unhealthy dietary patterns and sleep time, in addition to age, sex and parental education. However, associations were by no means uniform across all sites. In six sites, frequent breakfast consumers had lower BMI z-scores than rare consumers (China, Colombia, India and the United Kingdom) or compared with both rare and occasional consumers (Brazil), or rare consumers had higher BMI z-scores compared with both occasional and frequent consumers (the United States). In contrast, three sites (Canada, Portugal and South Africa) showed occasional but not rare consumption to be associated with higher BMI z-scores, and no associations were evident in another three sites (Australia, Finland or Kenya). Comparing ‘daily' and ‘less than daily' consumption revealed similar findings when all sites were combined, but this definition was not sensitive enough to isolate the effects of rare and occasional consumption. As a result, fewer associations were apparent at the site level (that is, for Brazil, Canada and Colombia only) with the application of this dichotomized definition versus the three-category definition. To emphasize, using only two categories to define breakfast frequency appeared to be insufficient to examine the site-level associations in our sample.
Differing associations in the relationship between breakfast frequency and adiposity indicators between sites might reflect differences in cultural and/or nutritional practices, including reasons for skipping breakfast and breakfast composition. For example, non-significant associations in Kenya may be partly attributed to a lack of food at home being the most commonly reported reason for skipping breakfast in Kenyan adolescents,6 whereas common reasons cited by young people in high-income countries include lack of hunger or dieting to lose weight, indicating that skipping breakfast could be a consequence of obesity in these countries.31, 32, 33 Furthermore, ready-to-eat cereals have a particularly strong link with lower obesity risk compared with ‘other' breakfasts, thus associations may be stronger in countries where these cereals are consumed.34 The higher BMI z-scores in occasional, but not rare, breakfast consumers relative to frequent breakfast consumers in some sites could relate to occasional consumption being an indicator of meal ‘irregularity' and household chaos, factors associated with higher BMI and a host of health-related behaviors in children.35, 36 It is also possible that the small sample size within the ‘rare' breakfast category reduced the likelihood of detecting significant differences within some sites, but there was no clear evidence of this. Indeed, even fewer site-level differences were significant when using the two-category definition (which did not include ‘rare' consumption) and the sites with limited associations were not necessarily those with the lowest numbers of rare breakfast consumers (for example, Australia had the 8th highest number of rare consumers). Finally, the relatively low BMI z-scores across all breakfast frequency categories in Kenya and Finland may have contributed to non-significant associations in these sites specifically. With this in mind, when considering our findings collectively, rather than being associated with ‘lower' obesity status, it may be more appropriate to conclude that frequent breakfast consumption was more consistently associated with ‘healthy' adiposity status (for example, BMI z-scores closer to zero) in children from a diverse range of cultures across the globe.
Greater insight into the mechanisms by which the practice of having a regular breakfast supports a healthy level of adiposity could be gained through exploring possible sources of heterogeneity in the association between breakfast frequency and adiposity indicators between countries, which was beyond the scope of this study. Ultimately, the mechanism must relate to daily energy intake and expenditure. Therefore, studies assessing associations between breakfast, dietary variables and physical (in)activity in children living in countries that are socio-culturally diverse would be valuable in extending the findings reported here.
Limitations
The cross-sectional design of our study does not allow us to infer causality. Although a 5-year prospective study in children and adolescents from the United States reported a dose-response inverse relationship between breakfast consumption and weight gain,37 others have reported differences in these associations based on a child's weight status; for example, never consuming breakfast has been associated with reduced BMI in overweight and increased BMI in non-overweight children from the United States.38 Further longitudinal research in globally representative samples of children would be valuable in evaluating the longer term effects of breakfast frequency on adiposity indicators, while experimental research would provide a more definitive answer to whether frequent breakfast consumption can improve adiposity status. Since we assessed breakfast frequency via questionnaire, our results may have been affected by possible variations in the validity of the question across countries, and we did not assess the quality (for example, macronutrient composition), quantity (for example, energy content) or location of breakfast consumption, only its presence. In addition, it is important to realize that ISCOLE samples were not nationally representative, hence these results are applicable to children living in urban and semi-urban environments.39 The exclusion of participants with missing data may have also resulted in a degree of bias in the final sample, favouring those children and parents who were more compliant with study procedures.
Conclusion
Across 12 sites varying in geographic region and socio-cultural backgrounds, frequent breakfast consumption was associated with lower BMI z-scores and BF% compared with both occasional and rare consumption. However, these relationships were not uniformly observed in all 12 study sites, with occasional rather than rare breakfast consumption being associated with higher BMI z-scores compared with frequent consumption in three sites, and no associations in three other sites. Using only a two-category definition of breakfast frequency lacked the sensitivity to isolate the effects of rare and occasional consumption, thus using three categories was preferred. Future research is required to investigate factors explaining global differences in the strength, direction, and nature of associations between breakfast frequency and adiposity indicators in children.
Acknowledgments
We thank the ISCOLE External Advisory Board and the ISCOLE participants and their families who made this study possible. A membership list of the ISCOLE Research Group and External Advisory Board is included in Katzmarzyk et al. (this issue). ISCOLE was funded by The Coca-Cola Company. MF has received a research grant from Fazer Finland. RK has received a research grant from Abbott Nutrition Research and Development.
MF has received a research grant from Fazer Finland and has received an honorarium for speaking for Merck. AK has been a member of the Advisory Boards of Dupont and McCain Foods. RK has received a research grant from Abbott Nutrition Research and Development. VM is a member of the Scientific Advisory Board of Actigraph and has received an honorarium for speaking for the Coca-Cola Company. TO has received an honorarium for speaking for the Coca-Cola Company. JZ has received a grant from The British Academy/Leverhulme Trust. The remaining authors declare no conflict of interest.
References
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011; 378: 815–825. [DOI] [PubMed] [Google Scholar]
- Gupta N, Goel K, Shah P, Misra A. Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr Rev 2012; 33: 48–70. [DOI] [PubMed] [Google Scholar]
- Olds T, Maher C, Zumin S, Péneau S, Lioret S, Castetbon K et al. Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes 2011; 6: 342–360. [DOI] [PubMed] [Google Scholar]
- Vereecken C, Dupuy M, Rasmussen M, Kelly C, Nansel TR, Al Sabbah H et al. Breakfast consumption and its socio-demographic and lifestyle correlates in schoolchildren in 41 countries participating in the HBSC study. Int J Public Health 2009; 54: 180–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora M, Nazar GP, Gupta VK, Perry CL, Reddy KS, Stigler MH. Association of breakfast intake with obesity, dietary and physical activity behavior among urban school-aged adolescents in Delhi, India: results of a cross-sectional study. BMC Public Health 2012; 12: 881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doku D, Koivusilta L, Raisamo S, Rimpelä A. Socio-economic differences in adolescents' breakfast eating, fruit and vegetable consumption and physical activity in Ghana. Public Health Nutr 2013; 16: 864–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rampersaud GC, Pereira MA, Girard BL, Adams J, Metzl JD. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc 2005; 105: 743–760. [DOI] [PubMed] [Google Scholar]
- Szajewska H, Ruszczynski M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit Rev Food Sci Nutr 2010; 50: 113–119. [DOI] [PubMed] [Google Scholar]
- Brown AW, Bohan Brown MM, Allison DB. Belief beyond the evidence: using the proposed effect of breakfast on obesity to show 2 practices that distort scientific evidence. Am J Clin Nutr 2013; 98: 1298–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr 2014; 100: 539–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhurandhar EJ, Dawson J, Alcorn A, Larsen LH, Thomas EA, Cardel M et al. The effectiveness of breakfast recommendations on weight loss: a randomized controlled trial. Am J Clin Nutr 2014; 100: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallström L, Labayen I, Ruiz JR, Patterson E, Vereecken CA, Breidenassel C et al. Breakfast consumption and CVD risk factors in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutr 2013; 16: 1296–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haug E, Rasmussen M, Samdal O, Iannotti R, Kelly C, Borraccino A et al. Overweight in school-aged children and its relationship with demographic and lifestyle factors: results from the WHO-Collaborative Health Behaviour in School-aged Children (HBSC) study. Int J Public Health 2009; 2: 167–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatami M, Taib MN, Jamaluddin R, Saad HA, Djazayery A, Chamari M et al. Dietary factors as the major determinants of overweight and obesity among Iranian adolescents. A cross-sectional study. Appetite 2014; 82: 194–201. [DOI] [PubMed] [Google Scholar]
- Duncan S, Duncan EK, Fernandes RA, Buonani C, Bastos KD, Segatto AF et al. Modifiable risk factors for overweight and obesity in children and adolescents from São Paulo, Brazil. BMC Public Health 2011; 11: 585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tin SP, Ho SY, Mak KH, Wan KL, Lam TH. Location of breakfast consumption predicts body mass index change in young Hong Kong children. Int J Obes 2012; 36: 925–930. [DOI] [PubMed] [Google Scholar]
- Raiah M, Talhi R, Mesli MF. Overweight and obesity in children aged 6-11 years: prevalence and associated factors in Oran. Sante Publique 2012; 24: 561–571. [PubMed] [Google Scholar]
- Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med 2011; 53: 260–267. [DOI] [PubMed] [Google Scholar]
- Dialekakou KD, Vranas PB. Breakfast skipping and body mass index among adolescents in Greece: whether an association exists depends on how breakfast skipping is defined. J Am Diet Assoc 2008; 108: 1517–1525. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M et al. The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health 2013; 13: 900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ 2007; 85: 660–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloheimo T, González SA, Erkkola M, Milauskas DM, Meisel JD, Champagne CM et al. The reliability and validity of a short food frequency questionnaire among 9 to 11-year-olds: a multinational study on 3 middle income and high income countries. Int J Obes Suppl 2015. (this issue). [DOI] [PMC free article] [PubMed]
- Mikkilä V, Vepsäläinen H, Saloheimo T, González SA, Meisel JD, Hu G et al. An international comparison of dietary patterns in 9-11-year-old children. Int J Obes Suppl 2015. (this issue). [DOI] [PMC free article] [PubMed]
- Tudor-Locke C, Barreira TV, Schuna JM Jr, Mire EF, Katzmarzyk PT. Fully automated waist-worn accelerometer algorithm for detecting children's sleep-period time separate from 24-h physical activity or sedentary behaviors. Appl Physiol Nutr Metab 2014; 39: 53–57. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci 2008; 26: 1557–1565. [DOI] [PubMed] [Google Scholar]
- Barreira TV, Schuna JM Jr, Mire EF, Katzmarzyk PT, Chaput JP, Leduc G et al. Identifying children's nocturnal sleep using a 24-h waist accelerometry. Med Sci Sports Exerc 2015; 47: 937–943. [DOI] [PubMed] [Google Scholar]
- Manios Y, Moschonis G, Androutsos O, Filippou C, Van Lippevelde W, Vik FN et al. Family sociodemographic characteristics as correlates of children's breakfast habits and weight status in eight European countries. The ENERGY (EuropeaN Energy balance Research to prevent excessive weight Gain among Youth) project. Public Health Nutr 2014; 14: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmiento OL, Parra DC, González SA, González-Casanova I, Forero AY, Garcia J. The dual burden of malnutrition in Colombia. Am J Clin Nutr 2014; 100: 1628S–1635S. [DOI] [PubMed] [Google Scholar]
- Instituto Colombiano de Bienestar Familiar ICBF. Programa de Alimentación Escolar. Available at http://www.icbf.gov.co/portal/page/portal/PortalICBF/Bienestar/ProgramasyEstratégias/AlimentaciónEscolar (accessed on 4 September 2013).
- Brug J, van Stralen MM, Te Velde SJ, Chinapaw MJ, De Bourdeaudhuij I, Lien N et al. Differences in weight status and energy-balance related behaviors among schoolchildren across Europe: the ENERGY-project. PLoS One 2012; 7: e34742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddan J, Wahlstrom K, Reicks M. Children's perceived benefits and barriers in relation to eating breakfast in schools with or without Universal School Breakfast. J Nutr Educ Behav 2002; 34: 47–52. [DOI] [PubMed] [Google Scholar]
- Shaw ME. Adolescent breakfast skipping: an Australian study. Adolescence 1998; 33: 851–861. [PubMed] [Google Scholar]
- Sjöberg A, Hallberg L, Höglund D, Hulthén L. Meal pattern, food choice, nutrient intake and lifestyle factors in The Göteborg Adolescence Study. Eur J Clin Nutr 2003; 57: 1569–1578. [DOI] [PubMed] [Google Scholar]
- Deshmukh-Taskar PR, Nicklas TA, O'Neil CE, Keast DR, Radcliffe JD, Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999–2006. J Am Diet Assoc 2010; 110: 869–878. [DOI] [PubMed] [Google Scholar]
- Kamp Dush CM, Schmeer KK, Taylor M. Chaos as a social determinant of child health: reciprocal associations? Soc Sci Med 2013; 95: 69–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleddens EF, Gerards SM, Thijs C, de Vries NK, Kremers SP. General parenting, childhood overweight and obesity-inducing behaviors: a review. Int J Pediatr Obes 2011; 6: e12–e27. [DOI] [PubMed] [Google Scholar]
- Timlin MT, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens). Pediatrics 2008; 121: e638–e645. [DOI] [PubMed] [Google Scholar]
- Berkey CS, Rockett HR, Gillman MW, Field AE, Colditz GA. Longitudinal study of skipping breakfast and weight change in adolescents. Int J Obes Relat Metab Disord 2003; 27: 1258–1266. [DOI] [PubMed] [Google Scholar]
- LeBlanc AG, Katzmarzyk PT, Barreira TV, Broyles ST, Chaput J-P, Church TS et al. Are participant characteristics from ISCOLE study sites comparable to the rest of their country? Int J Obes Suppl 2015. (this issue). [DOI] [PMC free article] [PubMed]