Abstract
Background:
Hospitals in which a high volume of arthroplasty procedures are performed have been observed to have better outcomes. As the number of arthroplasties has increased, it is not known whether surgical cases have shifted to high-volume hospitals. In this study, we examined the change in the volume of arthroplasties to provide a contemporary definition of “high-volume” centers, quantified surgical volume that shifted to high-volume centers, and investigated the resulting effect on complications.
Methods:
Data from the National (Nationwide) Inpatient Sample (2000 to 2012) were used to quantify trends in total hip arthroplasty (THA) and total knee arthroplasty (TKA) volume. Elective primary THAs and TKAs were identified and grouped by hospital by utilizing the hospital identifier, which indicates the geographic location of the hospital. County geographic and population data were obtained from the U.S. Census, and the distances between hospitals and the centroids of counties were calculated. Risk-standardized surgical complication rates for hospitals (2009 to 2012) were obtained from Medicare Hospital Compare and grouped by hospital volume.
Results:
From 2000 to 2012, there was a marked increase in the number of hospitals that performed a combined volume of ≥400 elective primary THAs and TKAs. The number of elective primary TKAs and THAs performed annually increased from 343,000 to 851,000. In 2012, 65.5% of the arthroplasties were performed in high-volume hospitals (≥400 arthroplasties annually), and 26.6% of the arthroplasties were performed in very high-volume hospitals (≥1,000 procedures annually). The proportion of arthroplasties performed in low-volume hospitals (<100 arthroplasties annually) shrank from 17.9% to 5.4%. Very high-volume hospitals had the lowest complication rates (2.745 per 100; 95% confidence interval [CI], 2.56 to 2.93), and low-volume hospitals had the highest complication rates (3.610 per 100; 95% CI, 3.58 to 3.64; p < 0.0001) (odds ratio, 1.327; 95% CI, 1.26 to 1.40). Our analysis showed that 81.9% of the U.S. population lived within 50 miles of a high-volume hospital.
Conclusions:
Arthroplasty patients are electing to have their procedures at higher-volume hospitals in the United States. Each successively higher hospital volume category manifested a lower complication rate.
Previous studies of hip and knee replacements have established that lower rates of complications, lower rates of revisions, and better outcomes are observed for hospitals and surgeons performing greater numbers of these procedures1-7. As a result, many have argued for regionalization of these procedures at high-volume hospitals4,8,9. Most of this previous work defined “very high-volume” centers as hospitals completing ≥200 total joint arthroplasties a year; however, the annual number of total joint arthroplasties has drastically increased in recent years10,11. As a result of this change in procedure volume, it is unclear whether previous definitions of “high-volume” hospitals still hold true today, and it is possible that previous associations between procedure volume and outcomes may have changed. Furthermore, it is unknown whether the increase in arthroplasty volume occurred because more hospitals began performing total joint replacements or because existing hospitals increased their capacity.
We performed an epidemiological study of total hip and knee arthroplasty in the United States. We sought to reexamine the definition of “high-volume” centers and confirm that hospital volume remains associated with complication rates. We further studied the geographic distribution of high-volume centers and examined trends in the distribution of arthroplasties over time to investigate whether geographic distance is a limitation of access to high-volume centers.
Materials and Methods
To examine the historical trends of joint replacements, we used the National (Nationwide) Inpatient Sample (NIS) to identify elective primary total knee and total hip arthroplasty procedures from 2000 to 201212,13. The NIS is a statistically validated, all-payer database of inpatient care containing annual, nationally representative data based on more than 8 million hospital stays from approximately 1,000 hospitals. The NIS is conducted as part of the federal Healthcare Cost and Utilization Project (HCUP) and is sponsored by the Agency for Healthcare Research and Quality (AHRQ). Starting in 2012, the NIS was changed from consisting of a sample of all discharges from 20% of hospitals nationwide to consisting of a sample of 20% of discharges from all short-term-stay hospitals in the United States. The NIS contains statistical trend weighting files for the standardization of data for longitudinal analysis, which also account for the sampling changes in the 2012 NIS data14. Clinical diagnoses and surgical procedures are recorded in the NIS using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). We used ICD-9-CM codes 81.51 and 81.54 to identify, respectively, primary total hip arthroplasty (THA) and total knee arthroplasty (TKA) and selected only procedures categorized by the NIS as elective. Hospitals were divided into four groups on the basis of the annual number of elective primary TKAs and THAs. The final model resulted in the following four groupings by volume: low (a combined volume of <100 TKAs and THAs annually), intermediate (100 to 399), high (400 to 999), and very high volume (≥1,000). The low, the intermediate, and the high combined with very high-volume categories divide hospitals approximately into tertiles based on their TKA and THA procedure volume in 2012. Because several hospitals had a much larger procedure volume than 400 TKAs and THAs per year, the “very high-volume” category was created to analyze the trends of these very high-volume hospitals separately.
To compare the complication rates of primary THA and TKA procedures between hospitals, we used the hip and knee surgical complication rate data from July 1, 2009, to March 31, 2012, from the Medicare Hospital Compare database15. This risk-standardized complication rate (per 100 procedures) measures the likelihood of any of 8 complications occurring within a specific time period. The 8 complications include 3 measures within 7 days of admission (acute myocardial infarction, pneumonia, or sepsis), 3 within 30 days of admission (surgical site bleeding, pulmonary embolism, or death), and 2 within 90 days of admission (mechanical complications or periprosthetic joint infection or wound infection). These complications can occur or be treated at any facility. Hospitals with <25 eligible cases are excluded from analysis by Hospital Compare. To calculate the volume cutoffs for the Medicare Hospital Compare data, hospital data from the NIS over the same time period were used to categorize hospitals on the basis of procedure volume of all patients and of Medicare patients only. Medicare volume cutoffs were then selected, which minimized the number of hospitals that were incorrectly categorized when compared with categorization on the basis of procedure volume of all patients. These volume cutoffs were scaled by 33/12 to account for the Medicare Hospital Compare data spanning 33 months.
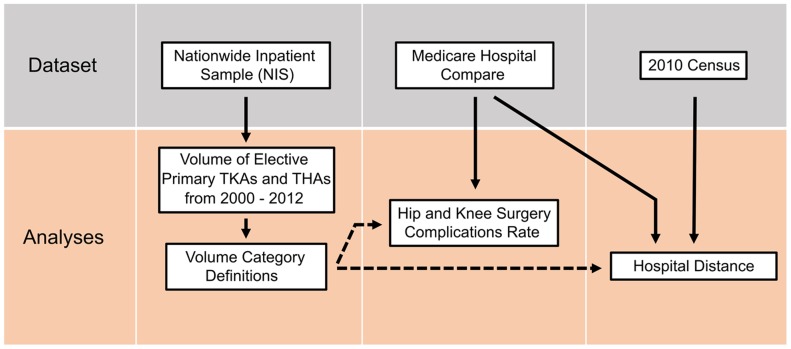
Geographic distribution was determined using U.S. county location and population data from the 2010 U.S. Census16 and the annual hospital volume calculated from the Medicare Hospital Compare database. The distribution of the U.S. population living within 50 or 100 miles (approximately 80 or 160 km) of hospitals in the highest three volume categories (≥100, ≥400, and ≥1,000 annual primary TKAs or THAs) was calculated. The population centroid of each county and the geographic location of each hospital were used to calculate the distance from the hospital. Figure 1 provides an overview of the analyses and databases used.
Fig. 1.
Schematic showing the analyses performed and the data sets used. Solid arrows indicate data used in the analysis. Dashed arrows indicate that data were not directly used, but results from the analysis were used.
The statistical analysis involved two-tailed t tests with a significance threshold of 0.05. Because multiple comparisons were made between the complication rates of the hospital-volume categories, p values were corrected using the Bonferroni method.
Results
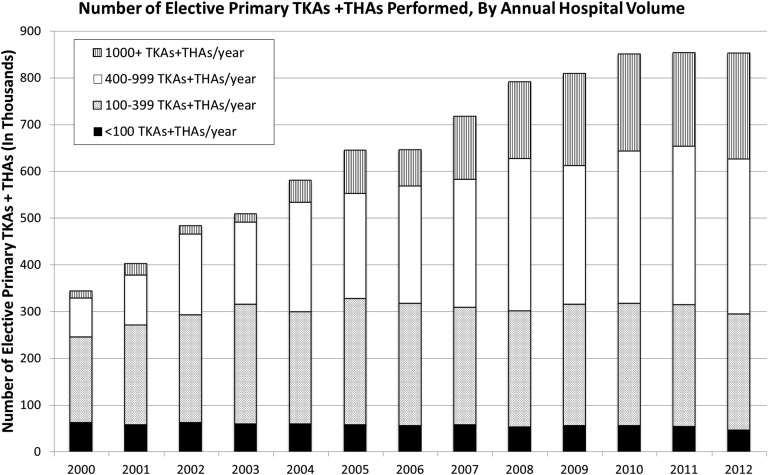
From 2000 to 2012, there was a marked increase in the number of primary elective THAs and TKAs performed (Fig. 2). An estimated 343,000 of these procedures (95% confidence interval [CI], 311,000 to 375,000) were performed in 2000. The number of arthroplasties rose steadily to 851,000 (95% CI, 765,000 to 936,000) in 2010, and remained steady, with 853,000 (95% CI, 813,000 to 893,000) performed in 2012.
Fig. 2.
Annual number of elective primary THA and TKA procedures performed. Hospitals were grouped into one of four categories on the basis of their combined THA and TKA annual procedure volume.
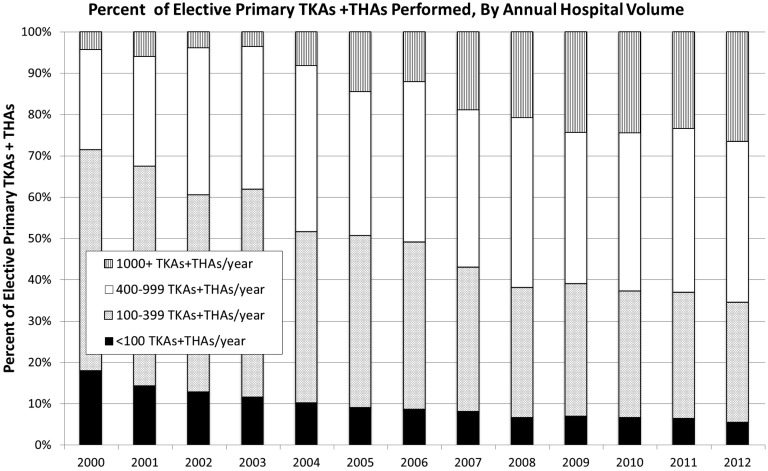
While the number of arthroplasties from 2000 to 2012 increased overall, the proportion of those procedures performed in high or very high-volume hospitals markedly increased (Fig. 3). In 2000, only 28.5% (95% CI, 19.5% to 37.5%) of elective TKAs and THAs were performed in high or very high-volume hospitals. In 2012, 65.5% (95% CI, 60.7% to 70.4%) of elective arthroplasties were performed in high or very high-volume hospitals. In addition, the proportion of procedures performed annually in low-volume hospitals (<100 procedures) decreased considerably, from 17.9% (95% CI, 15.9% to 19.9%) of TKAs and THAs performed in 2000 to 5.4% (95% CI, 5.0% to 5.7%) in 2012. However, these low-volume hospitals still represented 38.9% of all hospitals that performed an elective TKA or THA in 2012. The percentage of arthroplasties performed annually by very high-volume hospitals (≥1,000) grew from 4.3% in 2000 to 26.6% (95% CI, 22.0% to 31.1%) in 2012. These very high-volume hospitals represented just 4.9% of all hospitals that had performed an elective primary THA or TKA in 2012.
Fig. 3.
Percentage of annual number of elective primary THA and TKA procedures performed by the four hospital-volume categories. Hospitals were grouped into one of four categories on the basis of their combined THA and TKA annual procedure volume.
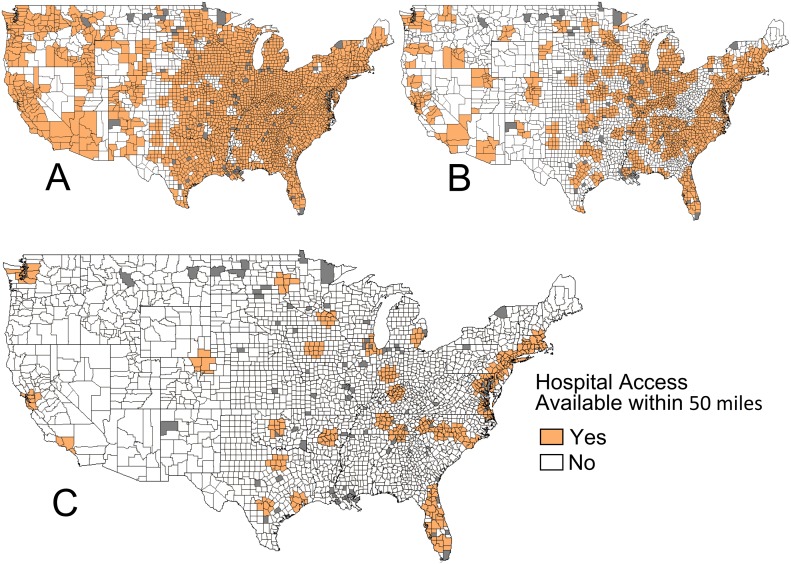
The majority of the U.S. population had access geographically to a high-volume hospital. Our analysis showed that 97.6% of the U.S. population lived within 50 miles of a hospital performing at least an intermediate volume of procedures (≥100 arthroplasties per year), 81.9% lived within 50 miles of a high or very high-volume hospital (≥400 arthroplasties per year), and 44.2% lived within 50 miles of a very high-volume hospital (≥1,000 arthroplasties per year) (Fig. 4).
Fig. 4.
Geographic accessibility to hospitals performing a high volume of arthroplasties, using a 50-mile radius. As shown by the counties in orange, 97.6% of the U.S. population was within 50 miles of a hospital that performed ≥100 THAs or TKAs per year (Fig. 4-A), 81.9% of the U.S. population was within 50 miles of a hospital that performed ≥400 arthroplasties per year (Fig. 4-B), and 44.2% of the U.S. population was within 50 miles of a hospital that performed ≥1,000 arthroplasties per year (very high-volume hospital) (Fig. 4-C). Volume was based on the 2009 to 2012 Medicare Hospital Compare data. Counties in gray were excluded because of a mismatch between location and population data.
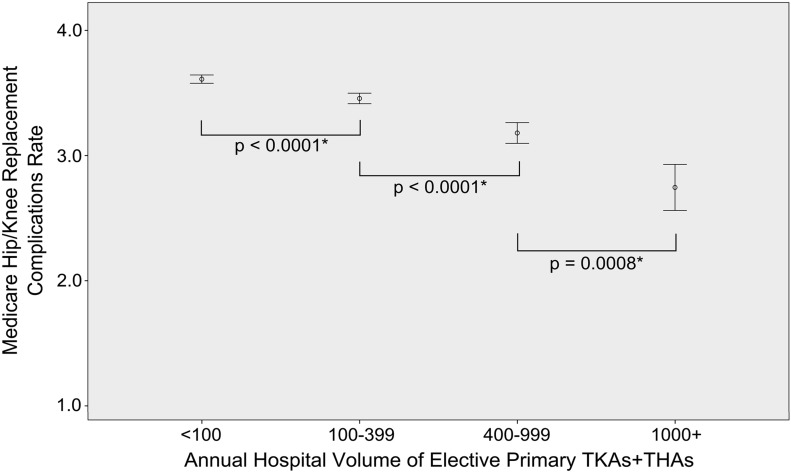
Our findings confirmed a strong association between hospital volume and publicly reported surgical complication rates. Medicare surgical complication rates for elective THAs and TKAs differed significantly according to hospital procedure-volume categories. The complication rates were lowest (2.745 per 100; 95% CI, 2.56 to 2.93) for very high-volume hospitals and were highest (3.610 per 100; 95% CI, 3.58 to 3.64) for low-volume hospitals (p < 0.0001) (Fig. 5) (odds ratio, 1.327; 95% CI, 1.26 to 1.40). We noted a significant reduction in complication rates for each increase in volume category.
Fig. 5.
The complication rate (per 100 procedures) for patients undergoing primary knee or hip arthroplasty per hospital, based on Medicare Hospital Compare data measured from 2009 to 2012. The hospitals were grouped on the basis of their annual combined elective primary TKA and THA volume. There was a significant decrease in the rate of complications as procedure volume increased. P values were corrected for multiple comparisons using the Bonferroni method. The I bars indicate the 95% CI.
Discussion
We found that, from 2002 to 2012, there was a shift of arthroplasties toward higher-volume hospitals in the United States. Although many hospitals have increased their annual cases, higher-volume hospitals still demonstrated a lower rate of publicly reported complications. Our findings challenge those of previous studies that suggested that the majority of THAs and TKAs were not being performed in high-volume hospitals17,18.
Our analysis of the NIS data shows that procedures have shifted toward high-volume hospitals. This shift toward high-volume hospitals could be due to a combination of factors, including the influence of published studies on physician referral habits and the use of the Internet for research by patients. A movement of arthroplasty surgeons to high-volume hospitals may also be a factor. Furthermore, we found that high-volume hospitals have accommodated higher volumes of procedures while still maintaining low complication rates compared with those of lower-volume centers.
TKA and THA volume increased 148% between 2002 and 2012 (Fig. 2) while the U.S. population increased only 11.6%. Previous work concluded that the increase in volume during the mid-2000s did not seem to result from an increase in the number of arthroplasty programs19. Among Medicare beneficiaries, the increase in procedures stems from increases in both the number of Medicare enrollees as well as per capita utilization20. Our analysis of the NIS data, however, differs from a recent model created by Kurtz et al.11: our finding that primary TKAs and THAs plateaued from 2010 through 2012 is not reflected in their model. The NIS underwent a sampling change for 2012 that resulted in approximately 4.3% fewer discharges for 2012, which may account for part of this plateau14. However, more data are needed to determine whether this reflects a true change in the trend regarding TKAs and THAs performed each year.
The significant reduction in complications seen for higher-volume hospitals is likely related to several factors. As hospitals increase volume, their surgeons perform more procedures and become more familiar with them. Previous work has established that higher surgeon volume is associated with better outcomes and fewer complications1,3,8,21,22. Increased hospital staff proficiency in the supportive care of patients as procedure volume increases may also contribute to the decrease in complications. However, the authors of previous work have argued that it is not necessarily the increase in procedure volume but an increase in orthopaedic specialization of hospitals that contributes to their improved outcomes23.
An important area for additional study is an examination of the differences in practices between very high-volume and high-volume hospitals. Very high-volume hospitals had a lower risk-stratified complication rate than high-volume hospitals (p = 0.0008) even though it would have been expected that the elements of patient selection, clinical pathways, and standardization had already been maximized in high-volume hospitals.
We know of no generally accepted criteria for establishing the cut-off of high versus low-volume hospitals in orthopaedics. The authors of previous studies have used percentile-based hospital groupings to define high-volume hospitals4,24,25, while others have used hard-number thresholds1,3,6-8,18,22. The authors of those previous studies chose cutoffs to determine high-volume hospitals at ranges of >100 THAs, >200 TKAs, and >200 combined TKAs and THAs. For our cutoffs, based on elective primary TKA and THA volume combined, we chose 4 volume categories: low (<100 procedures), intermediate (100 to 399), high (400 to 999), and very high (≥1,000). The low, the intermediate, and the high combined with very high-volume categories roughly divide the hospitals into tertiles for 2012, but we decided to use hard numbers to facilitate comparison over the years. Furthermore, it is thought that lower complication rates are related to the level of competency developed by hospitals performing a threshold number of procedures. As such, static hard-number cutoffs make more sense than percentile-based volume cutoff levels that change every year with overall procedure volume. Regardless of the cutoffs chosen, the lower complications and shift toward higher volume were robust.
Geographically, high-volume hospitals are readily available to the majority of the U.S. population. We initially considered a 100-mile radius as an appropriate travel distance in the United States for these procedures because it approximates a two-hour drive. However, other work has found that 95% of patients undergoing TKAs traveled <50 miles from their place of residence26. Using 50 miles as a radius, the percentage of the U.S. population living near a high or very high-volume hospital (≥400 TKAs and THAs) was still 81.9%, well above the 65.5% of procedures performed at high-volume hospitals. Our data indicate that approximately 130,000 patients annually forwent an arthroplasty procedure at a high-volume hospital despite there being a high-volume center available in their geographic area. Factors in addition to geographic distance appear to influence patient decisions about hospital selection for THA and TKA procedures27.
There were several limitations to our study. Our complication data were based only on the Medicare patient population and may not have represented the entire arthroplasty population. However, the majority of arthroplasties are performed on patients who are over the age of sixty-five years. Additionally, the Medicare Hospital Compare data do not include hospitals claiming <25 elective THAs and TKAs during the 33-month data period, so hospitals with extremely low volume were not included. Low-volume hospitals represented <6% of the procedures performed in 2012. Finally, Medicare Hospital Compare data may be subject to observational bias in reporting. Additional research is needed to analyze trends in hospital volume for revision knee and hip arthroplasty procedures.
The shift of arthroplasty case volume to high-volume hospitals represents an interesting example of the invisible hand of the market combined with evidenced-based medicine to effect positive change in health care.
Footnotes
Investigation performed at the Clinical and Investigative Orthopedic Surgery Unit, National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health, Bethesda, Maryland
A commentary by David W. Manning, MD, is linked to the online version of this article at jbjs.org.
Disclosure: This study was funded by the Intramural Research Program at the National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institutes of Health. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article.
References
- 1.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004. September;86(9):1909-16. [DOI] [PubMed] [Google Scholar]
- 2.Katz JN, Phillips CB, Baron JA, Fossel AH, Mahomed NN, Barrett J, Lingard EA, Harris WH, Poss R, Lew RA, Guadagnoli E, Wright EA, Losina E. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003. February;48(2):560-8. [DOI] [PubMed] [Google Scholar]
- 3.Katz JN, Mahomed NN, Baron JA, Barrett JA, Fossel AH, Creel AH, Wright J, Wright EA, Losina E. Association of hospital and surgeon procedure volume with patient-centered outcomes of total knee replacement in a population-based cohort of patients age 65 years and older. Arthritis Rheum. 2007. February;56(2):568-74. [DOI] [PubMed] [Google Scholar]
- 4.Cram P, Lu X, Callaghan JJ, Vaughan-Sarrazin MS, Cai X, Li Y. Long-term trends in hip arthroplasty use and volume. J Arthroplasty. 2012. February;27(2):278-285.e2. Epub 2011 Jul 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res. 2007. April;457:35-41. [DOI] [PubMed] [Google Scholar]
- 6.Singh JA, Kwoh CK, Boudreau RM, Lee GC, Ibrahim SA. Hospital volume and surgical outcomes after elective hip/knee arthroplasty: a risk-adjusted analysis of a large regional database. Arthritis Rheum. 2011. August;63(8):2531-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manley M, Ong K, Lau E, Kurtz SM. Total knee arthroplasty survivorship in the United States Medicare population: effect of hospital and surgeon procedure volume. J Arthroplasty. 2009. October;24(7):1061-7. Epub 2008 Nov 1. [DOI] [PubMed] [Google Scholar]
- 8.Dy CJ, Marx RG, Ghomrawi HM, Pan TJ, Westrich GH, Lyman S. The potential influence of regionalization strategies on delivery of care for elective total joint arthroplasty. J Arthroplasty. 2015. January;30(1):1-6. Epub 2014 Sep 6. [DOI] [PubMed] [Google Scholar]
- 9.Dudley RA, Johansen KL, Brand R, Rennie DJ, Milstein A. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000. March 1;283(9):1159-66. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007. April;89(4):780-5. [DOI] [PubMed] [Google Scholar]
- 11.Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014. April 16;96(8):624-30. [DOI] [PubMed] [Google Scholar]
- 12.Healthcare Cost and Utilization Project HCUP National Inpatient Sample (NIS). 2000-2011. http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 2015 Dec 15.
- 13.Healthcare Cost and Utilization Project HCUP National Inpatient Sample (NIS). 2012. http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 2015 Dec 15.
- 14.Houchens R, Elixhauser A. Using the HCUP Nationwide Inpatient Sample to estimate trends. HCUP Methods Series Report #2006-05. 2006. https://www.hcup-us.ahrq.gov/reports/methods/2006_05_NISTrendsReport_1988-2004.pdf. Accessed 2015 Dec 15.
- 15.Medicare.gov | Hospital Compare. Complication rate for hip/knee replacement patients. https://www.medicare.gov/hospitalcompare/Data/Surgical-Complications-Hip-Knee.html. Accessed 2015 Dec 15.
- 16.United States Census 2010. http://www.census.gov/2010census/. Accessed 2015 Dec 15.
- 17.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007. March;89(3):526-33. [DOI] [PubMed] [Google Scholar]
- 18.Manley M, Ong K, Lau E, Kurtz SM. Effect of volume on total hip arthroplasty revision rates in the United States Medicare population. J Bone Joint Surg Am. 2008. November;90(11):2446-51. [DOI] [PubMed] [Google Scholar]
- 19.Lu X, Hagen TP, Vaughan-Sarrazin MS, Cram P. The impact of new hospital orthopaedic surgery programs on total joint arthroplasty utilization. J Bone Joint Surg Am. 2010. June;92(6):1353-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012. September 26;308(12):1227-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz JN, Losina E, Barrett J, Phillips CB, Mahomed NN, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Association between hospital and surgeon procedure volume and outcomes of total hip replacement in the United States Medicare population. J Bone Joint Surg Am. 2001. November;83(11):1622-9. [DOI] [PubMed] [Google Scholar]
- 22.Hervey SL, Purves HR, Guller U, Toth AP, Vail TP, Pietrobon R. Provider volume of total knee arthroplasties and patient outcomes in the HCUP-Nationwide Inpatient Sample. J Bone Joint Surg Am. 2003. September;85(9):1775-83. [DOI] [PubMed] [Google Scholar]
- 23.Hagen TP, Vaughan-Sarrazin MS, Cram P. Relation between hospital orthopaedic specialisation and outcomes in patients aged 65 and older: retrospective analysis of US Medicare data. BMJ. 2010;340:c165. Epub 2010 Feb 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bozic KJ, Maselli J, Pekow PS, Lindenauer PK, Vail TP, Auerbach AD. The influence of procedure volumes and standardization of care on quality and efficiency in total joint replacement surgery. J Bone Joint Surg Am. 2010. November 17;92(16):2643-52. [DOI] [PubMed] [Google Scholar]
- 25.Doro C, Dimick J, Wainess R, Upchurch G, Urquhart A. Hospital volume and inpatient mortality outcomes of total hip arthroplasty in the United States. J Arthroplasty. 2006. September;21(6)(Suppl 2):10-6. [DOI] [PubMed] [Google Scholar]
- 26.FitzGerald JD, Soohoo NF, Losina E, Katz JN. Potential impact on patient residence to hospital travel distance and access to care under a policy of preferential referral to high-volume knee replacement hospitals. Arthritis Care Res (Hoboken). 2012. June;64(6):890-7. Epub 2012 Jan 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Losina E, Barrett J, Baron JA, Levy M, Phillips CB, Katz JN. Utilization of low-volume hospitals for total hip replacement. Arthritis Rheum. 2004. October 15;51(5):836-42. [DOI] [PubMed] [Google Scholar]