Abstract
Background
The aim of this study was to test the usefulness of the Cognitive and Language scales Bayley‐III in the early assessment of cognitive and language functions in the context of an autism spectrum disorder (ASD) diagnosis. This paper focuses on the application of the Bayley‐III and studies the predictive value of the test result in children with ASD with different levels of verbal ability.
Method
A sample of 135 children (121 boys, 14 girls) with a confirmed ASD diagnosis at age 4 years were assessed with the Bayley‐III before 42 months of age (m = 36.49, s = 4.46) and later with other rating scales of different psychological and psycholinguistic functions as part of a longitudinal study [McCarthy Scales of Children's Abilities (MSCA) (n = 48, 90% boys), Kaufman Assessment Battery for Children (K‐ABC) (n = 38, 87% boys) or Illinois Test of Psycholinguistic Abilities (ITPA) (n = 44, 89% boys)]. Age assessment in months: MSCA (m = 48.80, s = 3.33), K‐ABC (m = 51.80, s = 7.17) and ITPA (m = 54.48, s = 3.34).
Results
Lower scores on the cognitive and language Bayley‐III scales before 3.5 years of age predicted lower cognitive and oral language levels at 4 years of age. A significant correlation was found between the Cognitive Bayley‐III Scale and the General Cognitive MSCA Scale, and with the Compound K‐ABC Mental Processing. An association between the nonverbal cognitive level and oral language level acquired at 4 years of age was found.
Conclusions
The Bayley‐III is a useful instrument in cognitive and language assessment of ASD.
Keywords: autism spectrum disorder, Bayley‐III, cognitive ability, oral language
Introduction
The diagnosis of autism spectrum disorder (ASD), according to the Diagnostic and Statistical Manual of Mental Disorders (DSM)‐5th edition, American Psychiatric Association (APA 2013) criteria, must specify whether it is accompanied or not by an intellectual disability (ID) and/or language impairment, if it is associated with a medical or genetic condition or a known environmental factor, and if it is associated with other neurological, mental or behavioural development disorders. This new approach offered by the DSM‐5 allows for the establishment of different subtypes within ASD (Grzadzinski et al. 2013). Current studies report that the most common disorders associated with ASD are language problems (78%) and ID (49%) (Höglund Carlsson et al. 2013).
Early detection and diagnosis of ASD are important because of the implications on access to therapeutic care. When diagnosing younger children, assessment of cognitive and language ability is essential to contextualise the emerging ASD symptoms in the global profile of development, as many of the interaction problems that may arise will be influenced by a child's language level and mental age. It is believed that cognitive level and early intervention are the most significant variables effecting outcomes for children with ASD (Harris & Handleman 2000; Dawson 2008; Rogers et al. 2012).
Research on the use of the Bayley Scales in children with ASD goes back to the 1980s and has continued to the present. Previous studies on this topic have provided evidence on the stability of cognitive and linguistic parameters in autism (Freeman et al. 1985; Lord & Schopler 1989), and on the role of age at assessment, developmental level and assessment type in the stability of intelligence scores in young children with autism (Lord & Schopler 1989). The Bayley Scales of Infant Development—Third Edition (Bayley‐III; Bayley 2006) included a group of children with ASD in the standardisation process of special groups. Recently, other studies (Long et al. 2011) provide information regarding the cognitive skills of young children with and without ASD using the Bayley‐III. The Spanish adaptation of the Bayley‐III (Bayley 2015) also includes a study with Spanish‐speaking children with ASD, and the results are consistent with the USA studies.
The main contribution of the current study is to evaluate the predictive validity of the Spanish translation of the Bayley‐III (Bayley 2015) among children with ASD.
Objectives of the study
The purpose of this study was to evaluate the predictive validity and usefulness of the Bayley‐III Cognitive and Language scales in the early assessment of cognitive ability and language of Spanish infants and toddlers with a confirmed ASD diagnosis at age 4 years. This study focuses on the application of the Bayley‐III and studies the predictive value of the test result in children with ASD with different levels of verbal ability.
For some analyses, individual participants were categorised by intelligence scores according to levels of cognitive scores as measured on the Bayley‐III: subgroup 1: typical nonverbal cognitive level IQ ≥85 and subgroup 2: nonverbal cognitive level inferior to a standard deviation below the mean score (100 points) IQ <85. Although not all children in the second group had ID, they were considered to be at risk of presenting a more severe cognitive and language evolution than the group with typical nonverbal cognitive level. This continuous variable was dichotomised in order to ease interpretation of the Bayley‐III scores. Nonverbal IQ has been identified as an important predictor of later functioning (Lord et al. 2006) and may be used as a reference to decide appropriate intervention strategies.
Individual participants were categorised by functional oral language level acquired at the age of 4 years according to the following criteria: subgroup 1: absence of language or single words and subgroup 2: phrases or fluent. These criteria are described in the DSM‐5 (p. 53) as severity specifiers of language impairment and in the Application Manual of the Autism Diagnostic Observation Schedule (ADOS) (Lord et al. 2000; Lord et al. 2004). The description in the ADOS manual is used to determine the most appropriate module of the ADOS to administer. The language level acquired at the age of 4 years is not relevant when establishing different subtypes of ASD; however, the study of the predictive capacity of the Bayley‐III before 42 months in relation to the communicative competence expected at 4 years of age is extremely important to understand the prognosis and to establish intervention packages adjusted to each child's needs.
In the context of the earlier text, the following objectives were proposed:
To study the predictive ability of the scores obtained by children with ASD on the Bayley‐III Cognitive and Language scales in two developmental stages: (1) between 24 and 35 months of age and (2) between 36 and 42 months of age.
To assess the predictive ability of the scores on the Bayley‐III Cognitive and Language scales for children with ASD between 36 and 42 months old, in relation to specific external criteria such as subsequent performance, between 4 and 5 years of age in other scales measuring similar skills.
To assess the relationship between the nonverbal cognitive level before 3.5 years of age and functional oral language level acquired at age 4 years in children with a clinical diagnosis of ASD at this age.
To determine if there are significant differences in the scores obtained between 36 and 42 months old, in the Cognitive and Language scales of the Bayley‐III, between two subgroups of children with a clinical diagnoses of ASD classified according to the following criteria: subgroup 1: typical nonverbal cognitive level IQ ≥85 and subgroup 2: nonverbal cognitive level inferior to a standard deviation below the mean score (100 points) IQ <85.
To determine whether there are significant differences in the scores obtained between 36 and 42 months old, in the Cognitive and Language scales of the Bayley‐III between two subgroups of children with clinical diagnoses of ASD classified according to the functional level of oral language acquired at 4 years of age according to the following criteria: subgroup 1: absence of language or single words and subgroup 2: phrases or fluent.
Method
Participants
The sample consisted of a total of 135 children (121 boys, 14 girls). The sample represents children with a confirmed diagnosis of ASD at age 4 according to DSM‐5 criteria, who were referred to the Centre for Child Development and Early Intervention (CDIAP) Corporació Sanitària Parc Taulí before 3.5 years of age for consultation regarding their development. All children had their first diagnostic appointment at CDIAP between January 2008 and December 2013. Participants were born between January 2006 and May 2010. The proportion of children in this study represents 0.7% of children born in the same period in the reference area of CDIAP (4375 births per year), according to the Institut d'Estadística de Catalunya (Idescat 2012), which covers a geographical area of 11 municipalities in Vallès Occidental (Barcelona). Twenty children with suspected diagnoses of ASD, whose diagnoses were not yet confirmed, and three children who could not be assessed with the Bayley‐III at any tracking appointment because of the severity of their ID were not included in the study. Eleven children did not continue with the study (five because of a change of address and six because they stopped attending the appointments).
The inclusion criteria were as follows: a minimum of 12 months of follow‐up and consensus between a neurologist and a clinical psychologist regarding the clinical diagnosis of ASD. In this study, children with other associated disorders such as ID, language disorder, attention deficit disorder/hyperactivity and possible biological, psychological or social risk factors were included. Children were excluded if they had a motor disorder and/or a sensory deficit because these difficulties might have interfered with performance on the tests that required manipulative ability and visual–auditory perceptive capacity.
Children in the sample were classified according to their cognitive nonverbal level and their oral language level acquired at 4 years of age. Regarding the cognitive level, children were classified into two subgroups according to their cognitive level obtained before 3.5 years of age measured by the Cognitive Bayley‐III Scale, subgroup 1: typical nonverbal cognitive level IQ ≥85 (n = 92, 88% boys) and subgroup 2: nonverbal cognitive level below the standard deviation to the mean score (100 points) IQ <85 (n = 43, 91% boys).
Regarding the level of oral language acquired at age 4 years, children were classified into four subgroups according to the criteria of the DSM‐5 (APA 2013) and the ADOS (Lord et al. 2000; Lord et al. 2004). Subgroup 1: no words (n = 8, 88% boys), children with absence of language. Subgroup 2: single words (n = 40, 87% boys), children with inconsistent use of language without sentence construction. Subgroup 3: phrases (n = 68, 88% boys), children with language phrases, defined as three non‐repetitive word expressions, which sometimes would include a verb and which are combinations of the child's own words, spontaneous and with a meaning. Subgroup 4: fluent (n = 19, 100% boys), children with expressive language of a typical 4‐year‐old producing a wide range of types of sentences and grammatical structures, using language to convey information about situations outside the immediate context and producing some logical connections within sentences despite some grammatical errors.
The sample for this study was part of a larger study to validate the Spanish adaptation of the Bayley‐III Scales that ‘Pearson Education, SA’ leased to the ‘Fundació Parc Taulí’, which was published in 2015.
The study was approved by the Ethics Committee for Scientific Research from the ‘Fundació Parc Taulí’.
Instruments
Bayley Scales of Infant and Toddler Development (Bayley‐III; Bayley 2006) are intended to assess the developmental functioning of infants and children between 1 and 42 months. They consist of five scales: Cognitive (Cog), Language (Lang) [including the Receptive (RC) and Expressive (EC) communication subtests], Motor (including the Fine and Gross Motor subtests), Socio‐emotional and Adaptive Behaviour. The composite scores are normalised with a mean score of 100 and a standard deviation of 15. The subtest scores are normalised with a mean score of 10 and a standard deviation of 3. The English language version (Bayley 2006) has reported reliability coefficients of: 0.91 (Cog), 0.93 (Lang), 0.87 (RC) and 0.91 (EC). The reliability coefficients for special groups are as follows: 0.96 (Cog), 0.95 (RC) and 0.96 (EC). In this study, the Spanish adaptation of the Bayley‐III Scales was used (Bayley 2015).
McCarthy Scales of Children's Abilities (MSCA; McCarthy 2006) are a battery of tasks organised into six scales: Verbal (VS), Perceptual‐Performance (P‐PS), Quantitative (QS), General Cognitive (GCS), Memory (MS) and Motor (MS). They evaluate the skills profile of children between 2.5 and 8.5 years of age. The GCS score is normalised with a mean score of 100 and a standard deviation of 15. The VS, P‐PS, QS and MS scores are normalised with a mean score of 50 and a standard deviation of 10. The Spanish adaptation was used in this study and the reliability coefficient is 0.94 for the GCS.
Kaufman Assessment Battery for Children (K‐ABC; Kaufman & Kaufman 2005) provides a measurement of intelligence and knowledge. The battery measures the degree of skill in two domains of information processing (sequential‐simultaneous) on a Sequential Processing Scale and a Simultaneous Processing Scale. The two scales form a Mental Processing Scale Composite (MPC). It also has an Achievement Scale (ACH) and Nonverbal Scale (NV). Application range: from 2.5 to 12.5 years of age. The MPC, ACH and NV scores are normalised with a mean score of 100 and a standard deviation of 15. The Spanish adaptation was used in this study, and its reliability coefficients are 0.93 (MPC) and 0.93 (ACH).
Illinois Test of Psycholinguistic Abilities (ITPA; Kirk et al. 2004) evaluates the psycholinguistic functions involved in the communication process. It distinguishes between psycholinguistic skills when information flows through the auditory‐vocal channel or through the visual‐motor channel. It also distinguishes between the representational level and the automatic level of the psycholinguistic functions. Ages of application range: from 3 to 10 years of age. All the typical scores are normalised with a mean score of 36 and a standard deviation of 6. The Spanish adaptation was used in this study and its reliability coefficients values are higher than 0.90 for the 30% of the evaluated indexes for all age ranges. The Receptive Communication and Grammatical Closure indexes are the ones with greater reliability.
Procedure
All children who were evaluated had received a clinical diagnosis of ASD, based on the DSM‐5 criteria (APA 2013). Diagnostic processes and tests used by clinicians follow the ‘Guía de buena práctica para el diagnóstico de los trastornos del espectro autista (Best practice Guidelines for the diagnosis of ASD)’ (Díez‐Cuervo et al. 2005).
A complete clinical history was obtained from the parents or guardian of each participant. The clinical history included information regarding personal and family medical information, neurodevelopmental history and specific ASD symptomatology.
The process of diagnosis and therapeutic monitoring in CDIAP for children with a suspected ASD diagnosis consisted of a periodic evaluation (every 6 months) by a neurologist and a clinical psychologist specialising in neurodevelopment, and during treatment sessions that occurred between one and three times a week, depending on the needs of the child and the family. The psychological evaluation procedure included a psychometric assessment. Before the age of 3.5 years, the Cognitive and Language scales of Bayley‐III were used. Subsequently, from 4 to 4.5 years of age the MSCA and/or K‐ABC were used, and after 4.5 years of age the ITPA was used. The study used scores from assessments performed as part of an ongoing clinical service, so tests were not randomly assigned to participants in the follow‐up assessment. Children were given the most chronologically age‐appropriate test on which they could receive a basal score. This constraint limits the interpretation of the results because chronological age, cognitive level (and therefore, severity of delay) and choice of tests are not independent factors.
The children were classified into three groups based on the ages at which the Bayley‐III scales were administered: group 1: evaluated between 36 and 42 months old (n = 105, 76%); group 2: evaluated only between 24 and 35 months old (n = 30, 22%); and group 3: evaluated two times with Bayley‐III, the first evaluation between 24 and 35 months and next between 36 and 42 months old (n = 58, 42%). Each evaluation had a minimum period of 6 months between one assessment and the next. Subsequently, of the 105 participants evaluated with Bayley‐III between 36 and 42 months, they were reevaluated with one or various of the following instruments: (1) MSCA (n = 48, 90% boys), age assessment in months, m = 48.80, s = 3.33; (2) K‐ABC (n = 38, 87% boys), age assessment in months, m = 51.80, s = 7.17; or (3) ITPA (n = 44, 89% boys), age assessment in months, m = 54.48, s = 3.34. 44 participants (31%) could not be assessed with MSCA, K‐ABC or ITPA because of a lack of understanding of the tasks required.
The clinical diagnosis of ASD was agreed by a psychologist and a neurologist from the same diagnosis team with access to the complete clinical history of the participants. This was done according to DSM‐5 criteria and supplemented with the ADOS (Lord et al. 2000; Lord et al. 2004) in complex cases (n = 41, 30%). All tests were administered by a team of six psychologists who specialised in psychodiagnosis in early childhood. All psychologists were certified to administer the ADOS and share clinical and technical criteria. The Bayley‐III (Cognitive and Language scales), K‐ABC, MSCA and ITPA were administered in two sessions. By distributing the test between two sessions, the children's ability to participate in the neuropsychological assessments was increased. The sessions were separated by a maximum of a two weeks.
Data analysis
spss.20 (Chicago, IL, USA) was used to (1) obtain general descriptive statistics; (2) compare means between ASD groups; and (3) obtain Pearson's correlations and simple linear regressions between the results obtained through Bayley‐III and those obtained through the MSCA, K‐ABC and ITPA. The equation that describes this relation is shown with the regression. The continuous variables of the Bayley‐III cognitive scores were dichotomised to favour a more interpretative approach, although less analytical. Chi square was used to analyse this dichotomised variable.
Results
In relation to the first objective, a simple linear regression was calculated for scores obtained on the Cognitive and Language Bayley‐III scales to predict scores at 36‐42 months based on scores obtained between 24 and 35 months. The hypothesis that scores on the Cognitive and Language scales are positively related was also tested. Values for the Cognitive Scale, R 2 = 0.54 (y = 0.74× – 25.21), and Language Scale, R 2 = 0.62 (y = 0.79× – 22.87), indicated that more than half of the variability in scores between 36 and 42 months of age was explained by the obtained scores between 24 and 35 months.
With regard to the second objective, a good predictive capacity was found for the Bayley‐III Cognitive and Language scales in relation to other scales that measure similar skills. The results of the linear regression showed a significant correlation between the Bayley‐III Cognitive Scale and the MSCA's General Cognitive Scale [R 2 = 0.494 (y = 1.22× – 23.82)] and the K‐ABC's MPC Scale [R 2 = 0.431 (y = 1.56× – 47.45)]. A significant correlation between the Bayley‐III Language Scale and the MSCA's Verbal Scale (r = 0.709), the K‐ABC's Achievement Scale (r = 0.850) and all of Auditory‐Vocal subtests of the ITPA Channel: Auditory Reception (r = 0.526), Auditory Association (r = 0.666), Verbal Expression (r = 0.528), Grammatical Closure (r = 0.675) and Auditory Sequential Memory (r = 0.538) was also obtained (Tables 1, 2, 3).
Table 1.
Correlations between the Bayley‐III before 3.5 years old and MSCA at 4–4.5 years old
| Autism spectrum disorder (n = 48) | |||||||
|---|---|---|---|---|---|---|---|
| Correlation Bayley‐III/MSCA and mean scores MSCA (μ = 50, σ = 10) EGC (μ = 100, σ = 15) | Bayley‐III (μ = 10, σ = 3) (μ = 100, σ = 15) | ||||||
| Composite/subtest | VS | P‐PS | QS | GCS | MS | Mean | SD |
| Cog | 0.582** | 0.549** | 0.635** | 0.703** | 0.544** | 89.90 | 8.38 |
| Lang | 0.709** | 0.441** | 0.513** | 0.661** | 0.527** | 85.44 | 14.08 |
| RC | 0.592** | 0.502** | 0.506** | 0.649** | 0.507** | 7.63 | 2.56 |
| EC | 0.660** | 0.308* | 0.443** | 0.574** | 0.483** | 7.33 | 2.57 |
| Mean MSCA | 39.92 | 47.97 | 43.25 | 87.05 | 42.12 | ||
| SD | 10.52 | 8.49 | 11.34 | 14.48 | 9.18 | ||
Significance < 0.05,
Significance < 0.01.
Cog, Cognitive; Lang, Language Composite; RC, Receptive Communication; EC, Expressive Communication; VS, Verbal Scale; P‐PS, Perceptual‐Performance Scale; QS, Quantitative Scale; MS, Memory Scale; GCS, General Cognitive Scale (VS + P‐PS + QS); SD, standard deviation.
Table 2.
Correlations between the Bayley‐III before 3.5 years old and K‐ABC at 4–4.5 years old
| Autism spectrum disorder (n = 38) | |||||||
|---|---|---|---|---|---|---|---|
| Correlation Bayley‐III/K‐ABC and mean scores K‐ABC (μ = 100, σ = 15) |
Bayley‐III (μ = 10, σ = 3) (μ = 100, σ = 15) |
||||||
| Composite/subtest | Sequ. Pr | Simul. Pr | MPC | ACH | NV | Mean | SD |
| Cog | 0.391* | 0.643** | 0.656** | 0.727** | 0.578** | 88.68 | 6.54 |
| Lang | 0.515** | 0.539** | 0.662** | 0.850** | 0.679** | 85.33 | 13.51 |
| RC | 0.541** | 0.574** | 0.711** | 0.852** | 0.516** | 7.55 | 2.67 |
| EC | 0.438** | 0.377* | 0.504** | 0.759** | 0.561** | 7.10 | 2.29 |
| Mean K‐ABC | 87.24 | 98.37 | 91.41 | 90.46 | 93.26 | ||
| SD | 16.11 | 14.40 | 14.85 | 14.32 | 13.73 | ||
Significance < 0.05,
Significance < 0.01.
Cog, Cognitive; Lang, Language Composite; RC, Receptive Communication; EC, Expressive Communication; Sequ. Pr, Sequential Processing; Simul. Pr, Simultaneous Processing; MPC, Mental Processing Composite; ACH, Achievement; NV, Nonverbal; SD, standard deviation.
Table 3.
Correlations between the Bayley‐III before 3.5 years old and auditory‐vocal channel ITPA at 4.5 years old
| Autism spectrum disorder (n = 44) | |||||||
|---|---|---|---|---|---|---|---|
| Correlation Bayley‐III/ITPA and mean scores ITPA (μ = 36, σ = 6) | Bayley‐III (μ = 10, σ = 3) (μ = 100, σ = 15) | ||||||
| Composite/subtest | Representational level | Automatic level | Mean | SD | |||
| AR | AA | VE | GC | ASM | |||
| Cog | 0.410** | 0.574** | 0.269 | 0.510** | 0.637** | 89.20 | 7.39 |
| Lang | 0.526** | 0.666** | 0.528** | 0.675** | 0.538** | 84.26 | 13.75 |
| RC | 0.570** | ,685** | 0.436* | 0.610** | 0.461** | 7.42 | 2.40 |
| EC | 0.416** | 0.542** | 0.498* | 0.668** | 0.508** | 7.08 | 2.61 |
| Mean ITPA | 29.79 | 31.49 | 30.59 | 30.47 | 32.50 | ||
| SD | 4.80 | 5.52 | 7.00 | 5.47 | 5.64 | ||
Significance < 0.05,
Significance < 0.01.
Cog, Cognitive; Lang, Language Composite; RC, Receptive Communication; EC, Expressive Communication; AR, Auditory Reception; AA, Auditory Association; VE, Verbal Expression; GC, Grammatical Closure; ASM, Auditory Sequential Memory; SD, standard deviation.
The third aim was to assess the relationship between the variables nonverbal cognitive level and functional level of oral language acquired at 4 years of age. The results of the chi‐squared test (χ 2 (2) = 40.49, P < 0.001) show that both variables are related (Fig. 1).
Figure 1.
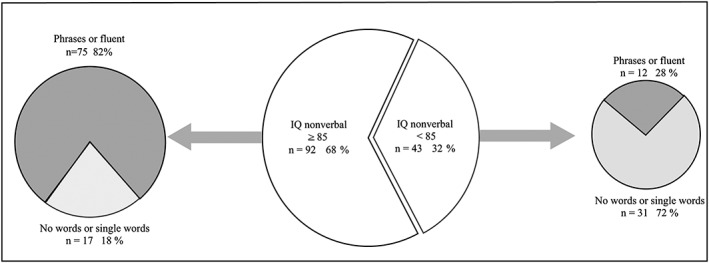
Level of oral Language acquired at age 4 according to nonverbal cognitive level.
Regarding the fourth objective, as expected, the results show that the subgroup of children with typical nonverbal cognitive ability scored significantly higher on both the Cognitive Scale (m = 91.69, s = 6.43) [95% CI (10.48, 16.11)] and on the Bayley‐III Language Scale (m = 89.03, s = 11.72) [95% CI (17.72, 28.59)], relative to the scores obtained by the subgroup of children with nonverbal cognitive level below the SD of the mean, who obtained lower scores on both scales: Cognitive Scale (m = 78.39, s = 7.12) and Language Scale (m = 65.44, s = 11.36). The results of the comparison of mean scores obtained by these two ASD subgroups show that these discrepancies are higher in the Language Scale (23.16‐point scale) than in the Cognitive Scale (13.30‐point scale), each with a significance of P < 0.001.
Finally, with respect to the fifth objective, the data show that the subgroup of children with ASD who had acquired a level of functional oral language of ‘phrases or fluent’ at age 4 years scored significantly higher on both the Cognitive Scale (m = 91.21, s = 6.99) [95% CI (7.25, 13.46)] and the Bayley‐III Language Scale (m = 88.19, s = 12.35), [95% CI (9.16, 27.47)], compared with those in the subgroup of children with language level ‘no words or single words,’ who received lower scores on both scales: Cognitive Scale (m = 80.85, s = 8.61) and Language Scale (m = 66.40, s = 12.63). The results of the comparison of mean scores obtained by these two ASD subgroups show significant differences in all subtests and Bayley‐III composite. Discrepancies between the scores of the two subgroups are higher in the Language Scale (21.78‐point scale) than in the Cognitive Scale (10.35‐point scale), all with significance <0.001.
The differences between the results obtained in the Cognitive Scale and the Language Scale for each of the groups studied were also calculated. Looking at the ability profile of each of the subgroups studied, less severe ASD subgroups have a more homogeneous profile with no significant differences between yields on the Cognitive Scale and the Language Scale: (1) phrases or fluent = 2.52‐point‐scale and (2) average nonverbal cognitive level = 3.03‐point‐scale. However, the most severe ASD subgroups present a non‐harmonic profile with significant differences between yields on the Cognitive Scale and the Language Scale: (1) no words or single words = 13.96‐point scale and (2) nonverbal cognitive level at an SD below the mean = 12.70‐pont scale (Table 4).
Table 4.
Differences in scores between the Bayley‐III's Cognitive Scale and Language Scale before age 3.5 years
| n | Cog | SD | Lang | SD | DIF. | 95% CI | t | Sig | ||
|---|---|---|---|---|---|---|---|---|---|---|
| LL | UL | |||||||||
| Less severe ADS subgroups | ||||||||||
| IQ nonverbal ≥85 | 62 | 91.85 | 6.15 | 88.79 | 12.12 | 3.03 | 0.69 | 5.43 | 2.59 | 0.012 |
| Phrases or fluent | 62 | 90.89 | 6.98 | 88.37 | 12.34 | 2.52 | 0.32 | 4.71 | 2.29 | 0.025 |
| Most severe ADS subgroups | ||||||||||
| IQ nonverbal <85 | 27 | 78.15 | 7.61 | 65.44 | 11.36 | 12.70 | 8.98 | 16.42 | 7.02 | <0.001 |
| No words or single words | 27 | 80.37 | 9.39 | 66.41 | 12.63 | 13.96 | 10.22 | 17.70 | 7.63 | <0.001 |
Cog, Cognitive; Lang, Language Composite; SD, standard deviation; LL, lower limit; UL, upper limit.
Discussion and conclusions
The results of this longitudinal study show that the Bayley‐III Spanish translation (Bayley 2015) is a very useful instrument in psychometric assessment of cognition and language of children with ASD before 42 months of age. These results align with other studies using the English language version (Bayley 2006; Long et al. 2011), that reported that the language scores were more significantly delayed than cognitive skills for children with ASD.
Our results indicate that between 36 and 42 months of age, the Bayley‐III detected significant deficits in the Language Scale in the two subgroups of children with ASD and that this was associated with a worse prognosis, including profiles of nonverbal cognitive ability at an SD below the mean (m = 65.44, s = 11.36) and/or presenting a level of oral language at 4 years of age characterised by no words or of single words (m = 66.40, s = 12.63). These results align with those of other studies that provide evidence that communication scores at 3 years of age were a stronger predictor of language at age 5 for children with autism (Thurm et al. 2007).
Although results from the Bayley‐III were applied between 36 and 42 months of age to provide greater consistency in the interpretation of data, analyses that show the good predictive ability of the Bayley‐III between 24 and 35 months have also been presented, in relation to subsequent reevaluations between 36 and 42 months. The stability in the early and later Bayley‐III scores supports the reliability of the measure over time.
Likewise, the results of the application of the Bayley‐III between 36 and 42 months with children with typical nonverbal cognitive level IQ ≥85 have proved useful as predictors of the results subsequently obtained with other scales measuring cognitive skills such as the MSCA and K‐ABC. The analyses of the cognitive development profiles obtained from the MSCA at 4.5 years (n = 48) show a tendency for the perceptual‐performance organisational capabilities to remain within the typical range (n = 44, 92%), while difficulties persist in verbal areas, quantitative areas, and memory associated with language. Among the 48 children assessed with MSCA, only 60% (n = 29) sustained an IQ ≥85 on the GCS. Moreover, among the 38 children assessed with KABC (an instrument designed to put minimal demands on oral language), 87% (n = 33) sustained an IQ ≥85 on the MPC, [63% (n = 24) on the Sequential Processing Scale and 95% (n = 36) on the Simultaneous Processing Scale].
Our findings show that nonverbal cognitive level and level of oral language acquired at age 4 years are closely related. At 4 years of age, no child with ASD and nonverbal cognitive SD ability below the mean acquired a fluent level of speech, 72% remained without words or at a single‐word level. However, no child with ASD and typical nonverbal cognitive ability remained without oral language at 4 years; 82% acquired a level of phrases or were fluent.
Although our study shows the relationship between cognitive level and language level, we should be cautious in the interpretation of the results of the Cognitive Bayley‐III Scale when predicting the level of language that a child can acquire in the future. On one hand, a small number of children with ASD that have a good nonverbal cognitive level can show a severe associated language disorder leading to a lower language level than expected. On the other hand, the children in the study received intervention that might have attenuated the observed associations.
Limitations
One limitation of the study is that the percentage of boys (n = 121, 89.6%) is higher than the percentage of girls (n = 14, 10.4%), which means the results correspond more closely to the developmental profile of boys. The large discrepancy suggests that girls probably have more subtle symptoms at an early age that may go unnoticed and not trigger a referral for a consultation in a specialised center before 42 months of age.
This study refers to the symptoms of ASD, but the analysis of the severity of ASD symptoms was not taken into account.
Another limitation of this study is that it analyses the correlation between the time points but not the changes in the scores. More systematic hypotheses or a more thorough evaluation of reliability and validity is needed to assess whether the scores tend to increase, decrease or stay the same. Finally, co‐occurring conditions with ASD were not included or analysed in this study.
Conclusions and future directions
This study shows that lower scores on the Cognitive and Language Bayley‐III scales before 3.5 years of age predicted lower cognitive and oral language levels at 4 years of age. A significant correlation between the Cognitive Bayley‐III Scale and the General Cognitive MSCA Scale, and with the Compound K‐ABC Mental Processing was found. We conclude that Bayley‐III is a useful instrument in cognitive and language assessment of ASD.
Further research is needed to define and analyse different developmental trajectories of ASD, the co‐occurring conditions, the severity of ASD symptoms and their etiological correlation. A detailed clinical diagnosis of children with ASD from infancy could contribute to further advancements in the understanding of various symptomatic expressions of ASD and also the development, treatment and prevention of ASD.
Torras‐Mañá, M. , Gómez‐Morales, A. , González‐Gimeno, I. , Fornieles‐Deu, A. , and Brun‐Gasca, C. (2016) Assessment of cognition and language in the early diagnosis of autism spectrum disorder: usefulness of the Bayley Scales of infant and toddler development, third edition. Journal of Intellectual Disability Research, 60: 502–511. doi: 10.1111/jir.12291.
References
- American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th edn ; DSM‐5. American Psychological Association, Washington, DC. [Google Scholar]
- Bayley N. (2006) Bayley‐III: Bayley Scales of Infant and Toddler Development, Third edn. Pearson, San Antonio, TX. [Google Scholar]
- Bayley N. (2015) Spanish Adaptation of the Bayley Scales of Infant and Toddler Development, Third edn. Pearson Educación S.A, Madrid. [Google Scholar]
- Dawson G. (2008) Early behavioral intervention, brain plasticity, and the prevention of autism spectrum disorder. Development and Psychopathology 20, 775–803. [DOI] [PubMed] [Google Scholar]
- Díez‐Cuervo A., Muñoz‐Yunta J., Fuentes‐Biggi J., Canal‐Bedia R., Idiazábal‐Aletxa M., Ferrari‐Arroyo M. et al (2005) Guía de buena práctica para el diagnóstico de los trastornos del espectro autista [Best practice Guidelines for the diagnosis of autistic spectrum disorders]. Rev Neurol 41, 299–310. [PubMed] [Google Scholar]
- Freeman B., Ritvo E. R., Needleman R. & Yokota A. (1985) The stability of cognitive and linguistic parameters in autism: a five‐year prospective study. Journal of the American Academy of Child Psychiatry 24, 459–64. [DOI] [PubMed] [Google Scholar]
- Grzadzinski R., Huerta M. & Lord C. (2013) DSM‐5 and autism spectrum disorders (ASDs): an opportunity for identifying ASD subtypes. Molecular Autism 4, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris S. L. & Handleman J. S. (2000) Age and IQ at intake as predictors of placement for young children with autism: a four‐to six‐year follow‐up. Journal of Autism and Developmental Disorders 30, 137–42. [DOI] [PubMed] [Google Scholar]
- Höglund Carlsson L., Norrelgen F., Kjellmer L., Westerlund J., Gillberg C. & Fernell E. (2013) Coexisting disorders and problems in preschool children with autism spectrum disorders. The Scientific World Journal 2013, 1–6. DOI: 10.1155/2013/213979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idescat (2012) Censo de población: sexo, edad y estado civil (2011). Población según nivel de instrucción por sexo y edad [Census of population: sex, age and marital status (2011). Polulation by educational attainment by sex and age]. Barcelona: Institut d'Estadística de Catalunya de la Generalitat de Catalunya. Available online: http://www.idescat.cat/territ/BasicTerr?TC=5&V0=3&V1=0&V3=319&V4=16&ALLINFO=TRUE&PARENT=1&CTX=B (retrieved 9 January 2013).
- Kaufman A. & Kaufman N. (2005) K‐ABC: Batería de evaluación de Kaufman para niños [Kaufman Assessment Battery for Children]. TEA, Madrid. [Google Scholar]
- Kirk S., McCarthy J. & Kirk W. (2004) ITPA:Test Illinois de aptitudes psicolingüísticas [Illinois Test of Psycholinguistic Abilities]. TEA, Madrid. [Google Scholar]
- Long C., Gurka M. J. & Blackman J. (2011) Cognitive skills of young children with and without autism spectrum disorder using the BSID‐III. Autism Research and Treatment 2011, 1–7. DOI: 10.1155/2011/759289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord C., Risi S., DiLavore P. S., Shulman C., Thurm A. & Pickles A. (2006) Autism from 2 to 9 years of age. Archives of General Psychiatry 63, 694–701. [DOI] [PubMed] [Google Scholar]
- Lord C., Risi S., Lambrecht L., Cook E. H., Jr. , Leventhal B. L., DiLavore P. C. et al (2000) The autism diagnostic observation schedule—generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders 30, 205–23. [PubMed] [Google Scholar]
- Lord C., Risi S. & Pickles A. (2004) Trajectory of language development in autistic spectrum disorders.
- Lord C. & Schopler E. (1989) The role of age at assessment, developmental level, and test in the stability of intelligence scores in young autistic children. Journal of Autism and Developmental Disorders 19, 483–99. [DOI] [PubMed] [Google Scholar]
- McCarthy D. (2006) MSCA: Escalas McCarthy de Aptitudes y Psicomotricidad [McCarthy Scales of Children's Abilities]. TEA, Madrid. [Google Scholar]
- Rogers S. J., Estes A., Lord C., Vismara L., Winter J. & Dawson G. (2012) Effects of a brief Early Start Denver Model (ESDM)–based parent intervention on toddlers at risk for autism spectrum disorders: a randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry 51, 1052–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thurm A., Lord C., Lee L.‐C. & Newschaffer C. (2007) Predictors of language acquisition in preschool children with autism spectrum disorders. Journal of Autism and Developmental Disorders 37, 1721–34. [DOI] [PubMed] [Google Scholar]


