Abstract
Plasmacytoma is a neoplastic production of a single line of plasma cells, usually forming monoclonal immunoglobulin. It most often occurs in the bone marrow; however, in 3% of the cases, solitary extramedullary plasmacytoma arises, which is a proliferation in the soft tissue, outside the bone marrow. In only 10% of the cases is the gastrointestinal tract involved. A 77-year-old female presented with lethargy, abdominal fullness, bilious vomiting, and clay-colored stools. The patient was anemic with initial laboratory results showing increased total and direct bilirubin with elevated transaminases. Despite conservative management, liver function tests (LFTs) continued to increase. On endoscopic ultrasound (EUS), there was mild diffuse mucosal thickening consistent with possible infiltrative disease of the gastric body without any obvious focal lesions. There was a 1.7 cm × 1.8 cm hypoechoic heterogeneous lesion noted in the porta hepatis and fine needle aspiration (FNA) was performed. Cytology showed infiltrative plasma cells. The patient was then taken for computed tomography (CT)-guided biopsy of the liver. Pathology showed liver involvement by atypical plasma cells in a nodular and sinusoidal pattern. Immunohistochemical staining appropriately identified the solitary extramedullary plasmacytoma. Plasma cell neoplasm is essentially a clonal disease of differentiated B-cells that can encompass a broad spectrum and present as asymptomatic monoclonal gammopathy of undetermined significance to plasma cell neoplasms or multiple myeloma. Five percent of patients with multiple myelomas are diagnosed with extramedullary plasmacytomas, and even less than that are diagnosed as a primary lesion. When the liver is affected, either as a direct diffuse neoplastic plasma cell infiltration, or as a single or multiple space occupying lesion as plasmacytomas, symptomatic features include extrahepatic biliary obstruction, jaundice, or ascites. In our case, the patient was diagnosed via EUS-guided FNA (EUS-FNA) bringing to light an alternative method to its diagnosis.
Keywords: Endoscopic ultrasound-guided fine needle aspiration biopsy (EUS-FNA), liver, solitary extramedullary plasmacytoma
INTRODUCTION
Plasmacytoma is a neoplastic production of a single line of plasma cells, usually forming monoclonal immunoglobulin. These tumors most often originate in the bone marrow, but extramedullary proliferation can occur in 3% of cases.[1,2] There is a male predominance at a ratio of 3:2 to females and median age of diagnosis is often in the sixth decade of life.[3,4,5] Whereas, upper respiratory involvement is common, gastrointestinal associated solitary extramedullary plasmacytomas (SEPs) are rare, accounting for only 10% of the cases. SEP refers to a solitary nonosseous plasma cell neoplasm in the absence of any other sign of multiple myeloma, and often presents a diagnostic challenge. We present a rare SEP diagnosed by endoscopic ultrasound-guided fine needle aspiration biopsy (EUS-FNA).
CASE REPORT
A 77-year-old female presented with lethargy, abdominal fullness, bilious vomiting, and clay-colored stool. The patient was anemic with initial laboratory results showing total bilirubin of 4.1 mg/dL (Normal 0.4-1.1 mg/dL), direct bilirubin 2.4 mg/dL (Normal 0.1-0.2 mg/dL), aspartate transaminase (AST) 87 IU/L (Normal 14-34 IU/L), alanine aminotransferase (ALT) 40 IU/L (Normal 7-58 IU/L), and alkaline phosphatase 523 IU/L (Normal 27-87). Ultrasound of the liver and computed tomography (CT) showed a distended gallbladder with a stone and sludge in the fundus and gallbladder wall thickening without intrahepatic or extrahepatic duct dilatation. Conservative management with intravenous (IV) fluids and antibiotics were initiated for acute cholecystitis with close monitoring of the liver function panel. Liver function tests (LFTs) continued to increase despite the instituted therapy, and endoscopic ultrasound was performed. On EUS, there was mild diffuse mucosal thickening consistent with possible infiltrative disease of the gastric body without any obvious focal lesion. There was a 1.7 cm × 1.8 cm hypoechoic heterogeneous lesion noted in the porta hepatis [Figure 1]. FNA was performed transduodenally with a 22 gauge Boston Scientific needle using suction technique after the instillation of 5 ccs of normal saline and replacement of the stylet with two passes. The aspirate was fixed in 50% alcohol and centrifuged to extract the tissue cells. They were fixed in formalin, infiltrated with paraffin to solidify the cells, sliced, and stained. Cytology and biopsy showed infiltrative plasma cells [Figures 2 and 3]. Immunohistochemical staining of the aspirate and the tissue biopsy showed positive staining for CD138 and monoclonal staining positive for kappa and negative for lambda [Figure 4]. These results were consistent with the diagnosis of solitary extramedullary plasmacytoma of the liver and radiation therapy was initiated.
Figure 1.
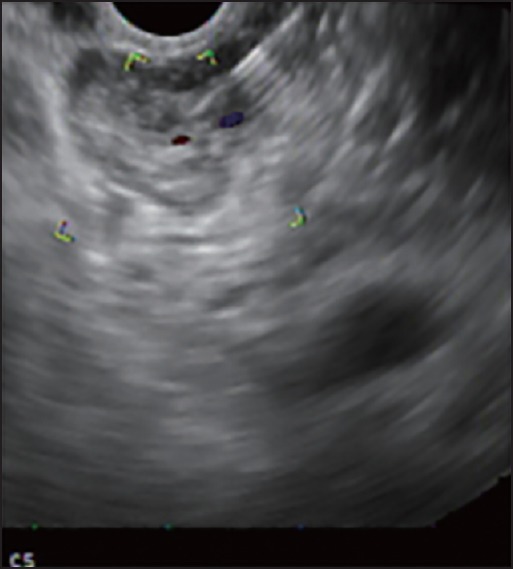
Mass in the porta hepatis
Figure 2.
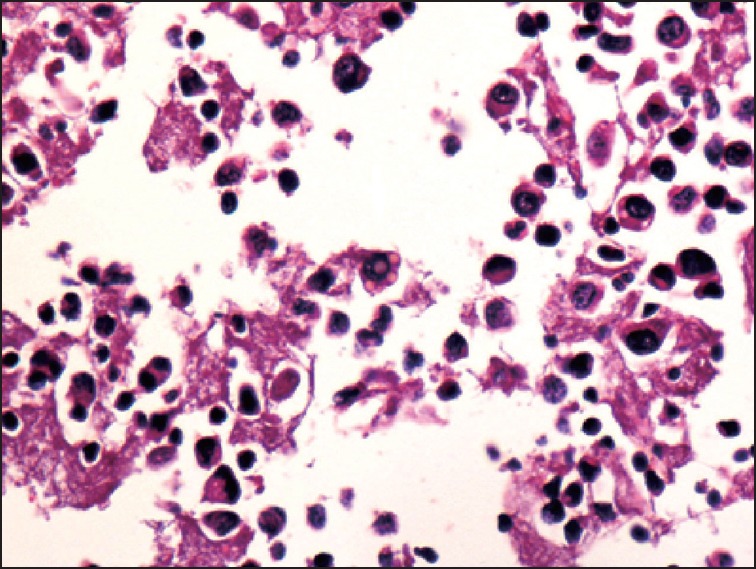
Plasma cells in sinusoids, H&E, 40×
Figure 3.
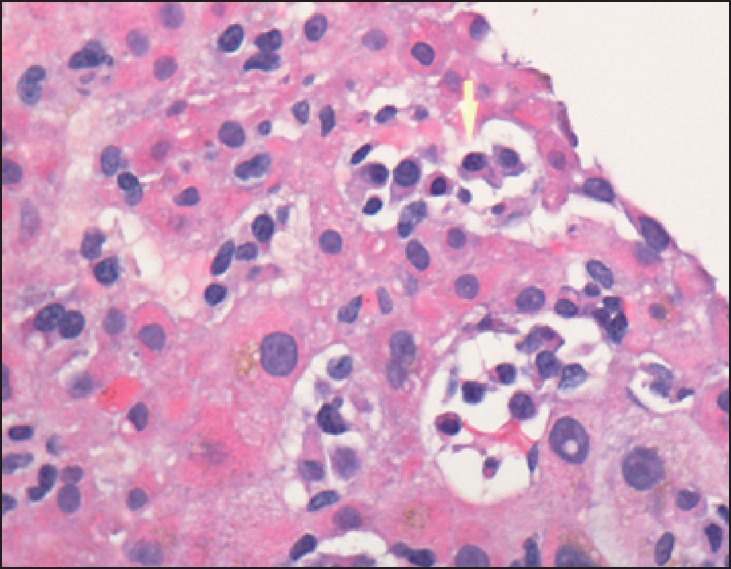
Plasma cells in sinusoids, H&E, 40×
Figure 4.
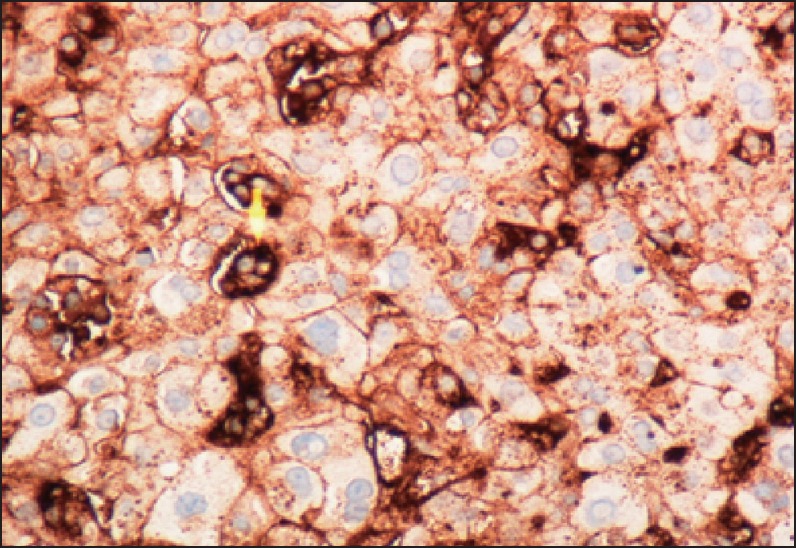
Plasma cells in sinusoids, Immunostain for kappa light chains, 40×
DISCUSSION
Plasma cell neoplasm are essentially a clonal disease of differentiated B-cells that can encompass a broad spectrum and present as asymptomatic monoclonal gammopathy of undetermined significance to plasma cell neoplasms or multiple myeloma.[3] Five percent of patients with multiple myelomas are diagnosed with extramedullary plasmacytomas, and even less than that are diagnosed as a primary lesion.[6] Most patients with SEP present with symptoms related to the location of the mass. Less common sites of involvement include the gastrointestinal tract, liver, lymph nodes, testes, skin, and the central nervous system. When the liver is affected via direct diffuse neoplastic plasma cell infiltration, or as a single or multiple space occupying lesions as plasmacytomas, it can present with symptomatic features such as extrahepatic biliary obstruction, jaundice, or ascites.[7] In our case, there was no evidence of diffuse infiltration of the liver on EUS or CT findings. The derangement of liver tests was attributed to a compilation of the mass with the underlying diagnosis of nonalcoholic fatty liver diseases. Furthermore, multiple myeloma was ruled out with an inconclusive plasma protein electrophoresis. When the liver is affected, the microscopic plasma cell infiltration patterns that have been described include diffuse versus nodular patterns, with diffuse including the sinusoidal, portal, and mixed types.[8] Perez-Soler et al. looked at 128 patients with multiple myeloma and found histologic findings in the liver of 16% of that population. Of that subset, roughly 50% had a microscopic finding of diffuse plasma cell infiltration of the liver, with no cases of nodular pattern detected.[9,10] Our case proves that EUS can be an important modality in diagnosing SEP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Padda MS, Milles T, Adeniran AJ, et al. Pancreatic and gastric plasmacytoma presenting with obstructive jaundice, diagnosed with endoscopic ultrasound-guided fine needle aspiration. Case Rep Gastroenterol. 2010;4:410–5. doi: 10.1159/000321050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coss A, Zhou C, Byrne MF, et al. Relapse of multiple myeloma presenting with biliary obstruction. Can J Gastroenterol. 2010;24:237–8. doi: 10.1155/2010/593859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miljkovic’ M, Senadhi V. Use of endoscopic ultrasound in diagnosing plasmacytoma of the pancreas. JOP. 2012;13:26–9. [PubMed] [Google Scholar]
- 4.Pinto-Marques P, Martins C, Mendonça E, et al. Pancreatic head mass of unusual etiology: Multiple myeloma diagnosed by endoscopic ultrasound-guided fine needle aspiration. Endoscopy. 2010;42(Suppl 2):E263–4. doi: 10.1055/s-0030-1255659. [DOI] [PubMed] [Google Scholar]
- 5.Liu W, Sun S, Ge N, et al. Rupture of a duodenal stromal tumor during EUS-FNA: A case report. Endosc Ultrasound. 2012;1:53–5. doi: 10.7178/eus.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woodruff RK, Whittle JM, Malpas JS. Solitary plasmacytoma. I: Extramedullary soft tissue plasmacytoma. Cancer. 1979;43:2340–3. doi: 10.1002/1097-0142(197906)43:6<2340::aid-cncr2820430625>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 7.Yagci M, Sucak GT, Akyol G, et al. Hepatic failure due to CD3+ plasma cell infiltration of the liver in multiple myeloma. Acta Haematol. 2002;107:38–42. doi: 10.1159/000046628. [DOI] [PubMed] [Google Scholar]
- 8.Thomas FB, Clausen KP, Greenberger NJ. Liver disease in multiple myeloma. Arch Intern Med. 1973;132:195–202. [PubMed] [Google Scholar]
- 9.Pal S, Chattopadhyay B, Chatterjee A, et al. Lambda light chain myeloma presenting as nodular hepatic lesion: A clinical rarity. J Cancer Res Ther. 2014;10:191–3. doi: 10.4103/0973-1482.131409. [DOI] [PubMed] [Google Scholar]
- 10.Perez-Soler R, Esteban R, Allende E, et al. Liver involvement in multiple myeloma. Am J Hematol. 1985;20:25–9. doi: 10.1002/ajh.2830200105. [DOI] [PubMed] [Google Scholar]


