Abstract
Peribulbar block, though safe, can cause serious complications such as globe perforation and peribulbar hemorrhage. Hyaluronidase is an enzyme that is used as an adjuvant in peribulbar anesthesia, and it helps in rapid penetration of the anesthetic agent. Hypersensitivity to hyaluronidase is a rare but potentially sight-threatening complication. We report a case of hyaluronidase hypersensitivity following peribulbar injection for cataract surgery mimicking as peribulbar hematoma in the immediate postinjection phase and as orbital cellulitis 48 h later.
Keywords: Anaesthesia, hyaluronidase, hypersensitivity, peribulbar
Peribulbar block is an effective way of achieving complete akinesia and anesthesia for intraocular surgeries and has very low risk of complications such as globe perforation.[1] Hyaluronidase is added as an adjunct to the anesthetic mixture, and it helps in rapid spreading of the anesthetic agent in the periocular space. It also helps in reducing the incidence of postoperative strabismus and risk of myotoxicity from the anesthetic agents.[1] Adverse events due to addition of hyaluronidase in the anesthetic mixture have been rarely reported and include increase in intraocular pressure (IOP), optic disc hemorrhage, eye pain, orbital and lid edema, hypersensitivity reactions, and orbital inflammation.[2]
Case Report
A 50-year-old woman who had undergone uneventful cataract surgery with intraocular lens (IOL) implantation in her left eye 1 year back was planned for small incision cataract surgery (SICS) with IOL implantation in the right eye under peribulbar anesthesia. Her systemic hypertension was well-controlled. A test dose of lignocaine was given 1 day before surgery which did not show any hypersensitivity reactions.
On the day of surgery, the patient developed lid edema with tight lids, conjunctival chemosis, and axial proptosis immediately after peribulbar injection (3 ml of 2% lignocaine + 1 ml of 0.5% bupivacaine + 1500 IU of hyaluronidase). The peribulbar block was given with a 26-gauge needle in the inferotemporal orbit. A diagnosis of peribulbar hemorrhage was made; the surgery was deferred, and the patient was managed with intravenous dexamethasone and mannitol, oral acetazolamide, and cold compress.
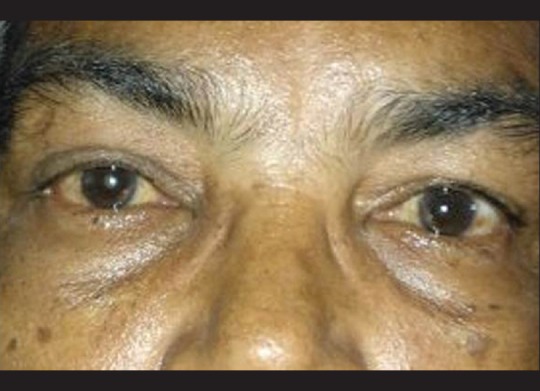
The chemosis and periorbital edema had partially resolved by 24 h. However, at 48 h postperibulbar injection, she developed increasing proptosis, lid edema, and tight eyelids with increasing chemosis [Fig. 1]. Anterior segment examination under slit lamp showed a brisk pupillary response. The posterior segment revealed no abnormalities. In view of increasing proptosis, orbital cellulitis was suspected, and the patient was started on intravenous cefotaxime although the patient was afebrile and had no systemic symptoms. Computerized tomography (CT) scan of orbit was planned.
Figure 1.

Periorbital edema, chemosis, and proptosis 48 h after peribulbar injection
In view of atypical symptoms of absence of systemic signs, a review of literature was done which prompted us to consider a diagnosis of delayed hyaluronidase allergy. An intradermal test with bupivacaine, lignocaine, and low dose of hyaluronidase 15 IU/0.1 ml was done. There was no reaction at the site of lignocaine and bupivacaine injection, but the patient developed an immediate hypersensitivity response in the form of erythema and wheal within a few seconds that disappeared in a minute, thus confirming the diagnosis of hyaluronidase hypersensitivity [Fig. 2]. She received intravenous dexamethasone 8 mg immediately followed by oral prednisolone 60 mg which was tapered over 2 weeks. She responded well to steroids with rapid resolution of lid edema and chemosis by 24 h prompting us to stop intravenous antibiotic and continue only oral steroid. CT scan of the orbit was not performed. Complete resolution of the proptosis was observed by 4 days [Fig. 3].
Figure 2.

Immediate wheal response after intradermal test with hyaluronidase
Figure 3.
Significant resolution of periorbital inflammation after systemic steroids
She developed a delayed hypersensitivity response with induration (10 mm × 12 mm) at the site of intradermal injection after 48 h which was treated with local application of hydrocortisone cream. This established the diagnosis of both immediate and delayed hypersensitivity to hyaluronidase in this patient. She underwent an uncomplicated phacoemulsification with foldable IOL implantation under topical anesthesia 1-month later.
Discussion
Hyaluronidase is an enzyme that breaks down hyaluronic acid, a glycosaminoglycan found in connective tissues. When the hyaluronic acid is broken down, there is a transient increase in permeability of the connective tissues. Hyaluronidase is frequently used as an adjunct in combination with anesthetic agents for ophthalmologic surgery (e.g., retrobulbar block, peribulbar block, and sub-Tenon's block). The rationale behind its addition to the local anesthesia techniques is to increase the dispersion of anesthetic agents in the ocular region and hasten its onset of action. Further, its use in ophthalmic anesthesia includes smaller increases in IOP, less distortion of the surgical site, decreased incidence of postoperative strabismus, and potential for limiting local anesthetic myotoxicity because of quicker spread.[2]
Allergy to hyaluronidase is a rare entity and a great mimicker of orbital inflammation as well. Both immediate and delayed reactions have been reported with use of hyaluronidase.[3,4,5,6,7,8] Kirby et al. reported the first case of immediate hypersensitivity to hyaluronidase with periorbital edema and chemosis developing within a few minutes of administering the anesthetic mixture containing hyaluronidase as one of the constituents.[3] Quhill et al. reported a delayed onset hyaluronidase allergy following peribulbar anesthesia presenting as orbital inflammation.[8] Musa et al. reported a rare case of IgE-mediated hypersensitivity to hyaluronidase that presented after 36 h following a sub-Tenon's anesthesia.[9]
In the case being reported, she developed proptosis immediately after peribulbar injection which was confused with a peribulbar hemorrhage. After 48 h, the increase in proptosis and lid edema was mimicking orbital cellulitis. The absence of systemic symptoms and rapid response to steroids along with positive intradermal test confirmed the hypersensitivity to hyaluronidase. This case showed both an immediate Type I and a delayed Type IV hypersensitivity response similar to protein contact dermatitis described by Hjorth and Roed-Petersen.[10]
This case is being reported for its rarity in nature and unique feature of both immediate and delayed responses in the same patient. The other reports are of immediate or delayed reaction only. The importance of SICS in reducing the cataract load in India and the use of peribulbar block for the same cannot be overemphasized. This rare complication of peribulbar block should be considered a possibility when we suspect peribulbar hemorrhage or orbital inflammation following peribulbar block with hyaluronidase as an adjuvant.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Malik A, Fletcher EC, Chong V, Dasan J. Local anesthesia for cataract surgery. J Cataract Refract Surg. 2010;36:133–52. doi: 10.1016/j.jcrs.2009.10.025. [DOI] [PubMed] [Google Scholar]
- 2.Silverstein SM, Greenbaum S, Stern R. Hyaluronidase in ophthalmology. J Appl Res. 2012;12:1–13. [Google Scholar]
- 3.Kirby B, Butt A, Morrison AM, Beck MH. Type I allergic reaction to hyaluronidase during ophthalmic surgery. Contact Dermatitis. 2001;44:52. doi: 10.1034/j.1600-0536.2001.440107-19.x. [DOI] [PubMed] [Google Scholar]
- 4.Minning CA., Jr Hyaluronidase allergy simulating expulsive choroidal hemorrhage. Arch Ophthalmol. 1994;112:585–6. doi: 10.1001/archopht.1994.01090170029012. [DOI] [PubMed] [Google Scholar]
- 5.Taylor IS, Pollowitz JA. A little-known phenomenon: Allergic reaction to hyaluronidase. Ophthalmology. 1984;91:1003. [PubMed] [Google Scholar]
- 6.Varma D, Metcalfe TW. Orbital cellulitis after peribulbar anaesthesia for cataract surgery. Eye (Lond) 2003;17:105–6. doi: 10.1038/sj.eye.6700238. [DOI] [PubMed] [Google Scholar]
- 7.Kumar V, Saunders D. Orbital cellulitis after phacoemulsification and intraocular lens implantation. J Cataract Refract Surg. 2004;30:918–20. doi: 10.1016/j.jcrs.2003.11.026. [DOI] [PubMed] [Google Scholar]
- 8.Quhill F, Bowling B, Packard RB. Hyaluronidase allergy after peribulbar anesthesia with orbital inflammation. J Cataract Refract Surg. 2004;30:916–7. doi: 10.1016/j.jcrs.2003.08.024. [DOI] [PubMed] [Google Scholar]
- 9.Musa F, Srinivasan S, King CM, Kamal A. Raised intraocular pressure and orbital inflammation: A rare IgE-mediated allergic reaction to sub-Tenon's hyaluronidase. J Cataract Refract Surg. 2006;32:177–8. doi: 10.1016/j.jcrs.2005.11.024. [DOI] [PubMed] [Google Scholar]
- 10.Hjorth N, Roed-Petersen J. Occupational protein contact dermatitis in food handlers. Contact Dermatitis. 1976;2:28–42. doi: 10.1111/j.1600-0536.1976.tb02975.x. [DOI] [PubMed] [Google Scholar]


