Abstract
Survival from ARDS has increased substantially in the last twenty years as a result of key advances in lung-protective ventilation and resuscitation. Similarly, clinical practice improvements have contributed to an impressive decline in nosocomial ARDS incidence. Personalizing mechanical ventilation for further lung protection is a top research priority for the years ahead. However, the ARDS research agenda must be broader in scope. The clinical syndrome of ARDS includes a heterogeneous assemblage of pathophysiological processes leading to lung injury. Further understanding of these varied, complex biological underpinnings of ARDS pathogenesis is needed to inform therapeutic discovery and tailor management strategy to the individual patient. While some therapies may be applicable broadly to all ARDS patients, others may benefit only certain biologically distinct subsets. The twenty-year ARDSne(x)t research agenda calls for bringing personalized medicine to ARDS, asking simultaneously both whether a treatment affords clinically meaningful benefit and for whom. This expanded scope necessitates acquisition of highly granular biological, physiological, and clinical data as the new standard across studies. Tremendous investment in research infrastructure and global collaboration will be vital to fulfilling this agenda.
INTRODUCTION
Survival from ARDS has increased substantially in the last twenty years as a result of key advances in lung-protective ventilation and resuscitation. Simply adapting mechanical ventilation to reduce mechanical stress on the lungs has improved patient outcomes [1]. Personalizing mechanical ventilation for further lung-protection is a top research priority for the years ahead. Yet, the ARDS research agenda must be broader in scope. The clinical syndrome of ARDS includes a heterogeneous assemblage of pathophysiological processes leading to lung injury. Further understanding of these varied, complex biological underpinnings of ARDS pathogenesis is needed to inform therapeutic discovery and tailor management strategy to the individual patient. While some therapies may be broadly applicable to all ARDS patients, others may benefit only certain biologically distinct subsets. The twenty-year ARDSne(x)t research agenda (Table 1) calls for bringing personalized medicine to ARDS, asking simultaneously both whether a treatment affords clinically meaningful benefit and for whom.
Table 1.
Overview of the 2035 ARDSne(x)t Research Agenda
| Research Category | Areas for Future Investigation |
|---|---|
| Defining ARDS | |
| Oxygenation assessment | Standardized ventilator settings during PaO2:FiO2 measurement |
| Use of SpO2:FiO2 when blood gas unavailable | |
| Criteria for high-flow oxygen without positive pressure ventilation | |
| Respiratory mechanics | Value added by including respiratory mechanics criteria |
| Alternative imaging modalities | Lung ultrasound; electrical impedance tomography |
| Origin of edema | Biomarkers of inflammation and vascular permeability, PET scan |
| Biological heterogeneity | Define and incorporate biologically distinct subphenotypes |
| Epidemiology | |
| Temporal & regional differences | Link practice variation to incidence and outcomes |
| Mortality attributable to ARDS per se and not comorbidities | |
| Global burden of disease | Unique precipitating factors in low/middle income countries |
| Validate alternative diagnostic criteria for resource-limited settings | |
| Long-term functional outcomes | Preferred measures for long-term physical, neurocognitive, psychological outcomes |
| Predictors during critical illness of long-term outcomes | |
| Patient Assessment | |
| Early recognition | Automated screening/detection systems |
| Detect early lung injury prior to overt respiratory failure | |
| LUS, EIT, esophageal pressure, & transpulmonary thermodilution |
Standardized measures for between-patient comparisons |
| Determine added value for diagnosis, prognosis, management | |
| Molecular endotypes | Biomarkers to identify biologically distinct subphenotypes |
| Prevention | |
| Identifying at-risk patients | Refine clinical prediction scores |
| Physiological/biological measures to improve predictive ability | |
| Prevention targets | Mechanical injury prevention by optimizing tidal volume, PEEP, and non-invasive respiratory support strategies |
| Best practice benchmarks for iatrogenic ARDS prevention | |
| Pharmacologic prophylaxis targeted to underlying biology | |
| Management | |
| Tidal volume | Scaled to functional “ARDS baby lung” size |
| PEEP titration | Mechanics-based approach to promote recruitment, homogeneous strain distribution; minimize overdistension, cyclic atelectasis |
| Spontaneous breathing | Patient-specific risk:benefit assessment of spontaneous breathing |
| Risk mitigation strategies when heavy sedation/paralysis required | |
| Extracorporeal support | Identify which patients require/benefit from extracorporeal support |
| Criteria for initiation/weaning | |
| Ventilator and anticoagulation management | |
| Prone positioning | Precise mechanisms of effect to inform subgroups who benefit |
| Potential synergy with PEEP | |
| Pharmacotherapy | Target patient-specific pathogenesis |
| Rescue therapy | Identify unique late-stage processes for therapeutic targeting |
| Trial Design | |
| Powering | Adaptive sample size re-estimation |
| Study population enrichment strategies | |
| Mechanism | Incorporate biological and physiological measures to identify mechanisms and predictors of therapeutic response |
| Outcomes | Patient-centered outcomes measures for prevention trials |
| Identification of validated surrogate outcomes for small pilot trials | |
| Long-term functional outcomes measures among survivors | |
Abbreviations: LUS, lung ultrasound; EIT, electrical impedance tomography; PET, positron emission tomography
REDEFINING ARDS, AGAIN
A reliable clinical definition of ARDS that is readily measurable and sufficiently specific is crucial to understanding underlying biology and will shape future research directions and clinical practice. ARDS as currently defined represents a constellation of individually nonspecific findings precipitated by a wide range of pulmonary insults. The 2012 Berlin consensus definition of ARDS offers several major advances over previous definitions [2]. Still, fewer than half of patients with Berlin-definition ARDS have diffuse alveolar damage [3], the histopathological correlate of ARDS.
Non-standardized assessment of oxygenation, radiographic interpretation, origin of edema, and biological heterogeneity remain issues in defining ARDS. PaO2:FiO2 can vary considerably with PEEP and FiO2 titration [4]. Future research must validate standardizing ventilator settings during PaO2:FiO2 measurement when evaluating for ARDS [5] and determine whether incorporating measures of respiratory mechanics adds value to the definition. Criteria must be developed and validated to diagnose ARDS in patients receiving high-flow oxygen without positive pressure ventilation.
Because interobserver agreement on roentgenographic findings consistent with ARDS is poor [6], alternative bedside diagnostic tools should be evaluated—lung ultrasound [7], electrical impedance tomography [8, 9], and thermodilution-estimated extravascular lung water [10], among others. Objective, validated criteria for findings consistent with ARDS must be developed before these techniques can be incorporated into a future definition, along with addressing modality availability.
Finally, while clinically focused definitions of ARDS have facilitated identification of lung-protective strategies proven to decrease mortality, inherent limitations remain because of diverse underlying biology. Thus, future definitions may specify biologically distinct ARDS subphenotypes, identified via shared underlying precipitating factor(s), common respiratory physiology, or biomarker panels of alveolar epithelial and pulmonary vascular endothelial injury and inflammation [11–13]. The tension between generalizability and performance of future definitions will remain but may ease as diagnostics become more affordable and accessible over time.
EPIDEMIOLOGY
Temporal and Regional Differences in ARDS Incidence, Risk Factors, and Outcomes
ARDS incidence appears to vary considerably over time and across regions. At least in some regions, the incidence of nosocomial ARDS has declined steadily in recent years, while that of community-acquired ARDS (onset near time of hospital admission) appears unchanged [14]. Linking temporal and regional practice variation to ARDS incidence and outcomes—in essence a natural experiment—will inform development of evidence-based strategies for broader dissemination. Combining increasingly granular datasets from ICU electronic health records across institutions and regions may facilitate these efforts. Estimates of mortality attributable to ARDS per se, and not comorbid conditions, are lacking, but are critical for understanding ARDS as a public health issue and for powering clinical trials.
The recently completed LUNG-SAFE study [15] offers the most global assessment of ARDS prevalence and care patterns to date: nearly one-third of patients were enrolled outside of Europe and North America. Further analyses of this cohort will provide insights into geographic variation in disease burden and management. Future studies should identify precipitating factors for ARDS in low-and-middle-income countries, where HIV/AIDS, malaria, tuberculosis, diarrheal illness, malnutrition, and trauma are among the leading causes of death. Alternative diagnostic criteria for ARDS, employing modalities more widely available in resource-limited settings, must be validated [16].
Clinical Phenotypes & Biology
Identifying reliable biomarkers may be useful to characterize distinct biological subgroups of ARDS, detect at-risk patients, prognosticate in established ARDS, and identify molecular mediators for drug targeting. Recent work has revealed different histopathological correlates [17], genetic risk factors [18], and biomarker profiles [12] for ARDS precipitated by pulmonary (direct) or extrapulmonary (indirect) insults. Additional molecular and genetic epidemiologic studies are needed to detail this association between readily apparent clinical phenotypes and underlying biology. Such work should be incorporated into future ARDS clinical trials to gain understanding of variations in biological response to the therapy studied. Ultimately, linking anticipated therapeutic response to clinically evident biology will permit individualized management approaches that optimize risk:benefit profiles.
PATIENT ASSESSMENT
Early Recognition
Recognition of ARDS in research and practice remains variable [15, 19], in part because diagnosis requires a constellation of findings. Increased adoption of electronic medical records allows for automated warning systems to be developed that may improve early recognition of ARDS [20] and facilitate earlier implementation of proven therapies. Diagnosing ARDS before mechanical ventilation is required may afford new opportunities for earlier intervention. Development of “smart ventilators” that detect changes in respiratory system compliance or SpO2:FiO2, which may suggest ARDS onset, also should be explored.
Clinical prediction scores to identify early lung injury [21, 22] must be optimized and proven to enhance preventive/early treatment efforts. Whether measures of respiratory mechanics add predictive value should be evaluated. Validating SpO2:FiO2 as an alternative to PaO2:FiO2 for ARDS screening may limit delays in diagnosis, although SpO2:FiO2 may be less reliable in patients with high SpO2 receiving respiratory support. Future research should evaluate whether SpO2:FiO2 performance improves by down-titrating supplemental oxygen until SpO2 decreases to 88–95% or support is weaned entirely.
Bedside Monitoring
Lung ultrasound (LUS) already is employed widely to evaluate for pulmonary edema, atelectasis, consolidation, pleural effusion, and pneumothorax [7, 23]. LUS may be useful for real-time assessment of lung recruitment during ventilator adjustments but cannot reliably identify overdistension [23]. Given its near-ubiquitous availability in ICUs, LUS warrants further investigation for its potential to improve diagnostic evaluation of ARDS [16] (Table 2).
Table 2.
Bedside Monitoring Techniques for Further Study
| Modality | Acquisition | Potential Applications | Key Limitations |
|---|---|---|---|
| Lung ultrasound | Probe placed on chest transmits sound waves, records reflections back to probe |
|
|
| Electrical impedance tomography |
Electrodes on chest to monitor regional changes in electrical resistivity during ventilation |
|
|
| Esophageal pressure |
Small-diameter esophageal balloon catheter inserted via oral or nasal route |
|
|
| Single-indicator transpulmonary thermodilution extravascular lung water |
Temperature change, measured with femoral artery thermistor, following chilled saline bolus given via central venous catheter |
|
|
Electrical impedance tomography (EIT), which plots real-time changes in electrical resistivity due to ventilation, appears to concur with computed tomography in identifying regional differences in aeration [9]. EIT-based parameters have been developed to quantify real-time changes in lung parenchymal inhomogeneity, recruitment, and overdistension [8, 24], and should be evaluated for potential to individualize ventilator management. Concerns about required precision of electrode placement and diaphragmatic interference in caudal planes must be addressed adequately before expanding this technique beyond the research setting.
Esophageal pressure, used to estimate pleural pressure in the mid-chest, is measured with a thin-walled balloon catheter inserted at bedside via the nasal or oral route. Transpulmonary pressure (airway minus pleural pressure), the distending pressure of the lung, is readily calculated with esophageal manometry [25]. Measuring esophageal pressure allows for distinguishing between lung and chest wall contributions to total respiratory system mechanics, immediately relevant to individualizing lung-protective ventilation strategies. Esophageal pressure has been proposed to estimate global lung stress, guide PEEP titration, measure work of breathing, and understand patient-ventilator dyssynchronies [25–28]. The ongoing multicenter EPVent2 trial (NCT01681225) is evaluating esophageal pressure-guided PEEP titration in ARDS. Future studies should explore the role for esophageal pressure to individualize tidal volume, quantify occult dyssynchrony, determine prognostic value of lung stress, and evaluate etiology of failed spontaneous breathing trials.
Single-indicator transpulmonary thermodilution extravascular lung water (EVLW) estimates EVLW from the arterial blood temperature change profile following a chilled saline bolus administered through a central vein. Thermodilution EVLW has been validated in animal studies against the gold standard gravimetric method [29], and correlates with lung injury severity [10] and mortality [30] in small human studies. Further work should identify the optimal indexing factor for between-patient comparisons (e.g. height, actual/predicted body weight), evaluate potential confounding of PEEP titration, determine added prognostic value, and explore its potential role in guiding fluid management.
Molecular Endotypes
ARDS as currently defined captures a heterogeneous set of patients with distinct biological and clinical features, divergent natural histories, and differential treatment responses. This approach has yielded major improvements in patient outcomes with the evolution of lung-protective ventilation and supportive care practices. Tailoring select ARDS research and management approaches to biologically distinct endotypes may facilitate additional therapeutic discovery [11]. Recent findings linking biological endotypes to readily available clinical data [12] offer immediate opportunities for testing therapies in an enriched ARDS subgroup that can be identified clinically. Future studies should leverage “-omics” analyses of biologic samples coupled with detailed clinical and physiological data to better define endotypes and evaluate for differential treatment responses. These approaches require development of large cohorts of patients with and at risk for ARDS.
PERSONALIZED PREVENTION
Identifying At-Risk Patients
Surprisingly little is known of the biological processes preceding overt ARDS, a top priority for future study. Because ARDS does not develop in most patients with identifiable risk factors [21], subgroups at highest risk of developing ARDS must be identified. Clinical prediction scores for risk of developing ARDS [21, 31] should be refined periodically as clinical practice and epidemiology evolve. Recent data have suggested plasma biomarkers such as angiopoietin-2 may enhance prediction of ARDS onset among critically ill patients without ARDS on admission [32]. These promising results warrant independent validation. Ultimately, rapid on-site testing will be required to incorporate biomarker profiles into eligibility requirements for prevention trials unless clinical predictors of underlying biology can be developed. Increased EVLW, as estimated by thermodilution, similarly may be useful to identify early lung injury before clinically apparent ARDS [33], but current technology requires both a central venous catheter and femoral artery catheter for measurement, limiting its use.
Preventive Therapies Under Consideration
ARDS prevention strategies may be grouped broadly into two categories: improvements to existing care delivery processes to prevent iatrogenic ARDS (e.g. aspiration precautions, timely sepsis resuscitation), and new co-therapies prescribed specifically for the purpose of ARDS prevention (e.g. medication prescribed for ARDS prophylaxis). Timely antimicrobials and hemodynamic resuscitation for sepsis, restrictive transfusion practices, and aspiration precautions may prevent nosocomial ARDS, though optimal implementation of these strategies still requires study. Respiratory-support interventions that warrant further study include: scaling tidal volume to degree of risk for developing lung injury [34]; closed-loop ventilator systems for at-risk patients [35], PEEP titration among at-risk patients [36]; and, for non-intubated patients, high-flow oxygen nasal cannula or facemask/helmet noninvasive ventilation [37]. Candidate targets for pharmacologic prophylaxis are many and have been reviewed elsewhere [38]. Pharmacologic prophylaxis development requires further understanding of how each patient’s unique biology contributes to risk of clinical lung injury.
Unique Challenges for Prevention Trials
ARDS prevention trials must overcome key challenges related to their preventive focus. Most patients develop ARDS within 48 hours of admission [21], necessitating early recognition and trial enrollment promptly after initial hospital presentation to allow time for biological action of any intervention. Better understanding early pathophysiological changes precipitating ARDS onset may permit identifying biologically homogenous cohorts for trial enrollment and novel candidate therapies for testing [32]. In the interim, trials could focus on patients with similar risk factors, not just similar risk scores, to ensure some level of biological homogeneity. Because many risk factors for developing ARDS (e.g. septic shock) increase risk of death independent of ARDS, simply restricting the study population to patients at highest risk of ARDS may be ineffective. Thus, future work should aim to identify those patients at high risk of ARDS for whom developing ARDS worsens patient-centered outcomes—the very population to benefit meaningfully from prevention. Additionally, consensus is needed regarding the appropriate primary outcome for prevention trials. Powering for mortality will require large sample sizes given the low event rate. While intuitive, ARDS incidence is not clearly patient-centered, and it is possible a therapy may appear to “prevent” ARDS by increasing mortality prior to ARDS onset. Patient-centered outcomes, such as respiratory failure requiring positive pressure ventilation or neurocognitive/functional testing, may be more appropriate. Quality-adjusted life-years and other cost-effectiveness outcomes should also be considered given that most patients with identifiable risk factors do not develop ARDS [21].
INDIVIDUALIZING MANAGEMENT
Tidal Volume
In ARDS, the volume of aerated lung available for gas exchange and mechanical insufflation is reduced due to dense atelectasis of dependent lung regions [39]. Thus, lower tidal volumes are protective in part because the functional lung volume being ventilated itself is reduced, a conceptual model termed the “ARDS baby lung.” For this same reason, scaling tidal volumes to “diseased functional lung size” rather than predicted “healthy” lung size (i.e. 6 mL/kg predicted body weight) may improve lung protection. Individualized lung-protective strategies proposed recently include scaling tidal volume to respiratory system compliance (i.e. airway driving pressure) [40, 41], lung compliance (i.e. tidal stress) [25], functional residual capacity (measured via helium dilution or nitrogen washout) [27], or “baby lung” inspiratory capacity (measured during a recruitment maneuver) [26] (Table 3). Additional studies are needed to develop each strategy into a clinical protocol for superiority testing against current standard of care. These approaches also may help identify patients (1) for whom lung mechanics simply preclude safe mechanical ventilation, justifying extracorporeal support, and (2) for whom tidal volume may be liberalized, minimizing undue discomfort or heavy sedation.
Table 3.
Potential Strategies for Personalized Management of ARDS
| Therapy | Personalized Approach |
|---|---|
| Tidal volume |
Scale to “ARDS baby lung” size
|
| Positive end-expiratory pressure |
Titrate to patient-specific respiratory mechanics
|
| Neuromuscular blockade |
Target to therapeutic mechanism for duration at risk
|
| Prone positioning |
Institute when mechanism of benefit likely
|
| Extracorporeal support |
Graded introduction when safe mechanical ventilation parameters yield insufficient gas exchange
|
| Pharmacotherapy |
Inhibit biotrauma propagation
|
PEEP Titration
Past large-scale randomized trials comparing “higher” versus “lower” PEEP strategies based on PEEP-FiO2 titration tables [42, 43] found no survival benefit from “higher” PEEP across the broad ARDS population. The degree of lung recruitment versus overdistension afforded by increasing PEEP may vary considerably between patients, by volume history, and with use of recruitment maneuvers, influencing whether increasing PEEP is lung-protective for an individual [44–46]. At a minimum, future PEEP titration trials should incorporate measures of lung recruitability, overdistension, and heterogeneity (stress raisers) [47] to permit pre-specified subgroup analyses testing for an interaction with study arm. Physiological response to a test dose of increased PEEP could inform patient selection for entrance into trials [48]. Individualizing PEEP based on respiratory mechanics may minimize overdistension and cyclic atelectasis, increase aerated lung available for tidal insufflation, and promote more uniform strain distribution [47]. Several mechanics-based PEEP titration strategies have been proposed, including highest respiratory system compliance [49], esophageal pressure-guided titration [25], stress index [50], ExPress PEEP [51], and pressure-volume curve lower inflection point (Pflex) [52]. Adequately powered trials are required to determine which approaches, if any, afford additional lung protection over previously studied oxygenation-based approaches that do not incorporate mechanics.
Spontaneous Breathing Effort
Whether spontaneous breathing effort is protective or deleterious in ARDS likely depends on several patient-specific factors: degree of existing lung injury, risk of further injury, homogeneity of lung mechanics, and risks of sedatives/paralytics (e.g. weakness, delirium, etc.). Spontaneous breathing can promote alveolar recruitment, stimulate surfactant production, and attenuate diaphragm disuse atrophy, while avoiding risks of heavy sedation and neuromuscular blockade [53, 54]. However, spontaneous breathing effort also can produce high tidal volumes, breath stacking dyssynchrony, regional overdistension, and tidal recruitment, potentiating lung injury risk [55, 56]. Neuromuscular blockade was associated with improved ARDS survival in a prior multicenter trial [57]; the ongoing ROSE-PETAL trial (NCT02509078) aims to validate these findings. Still, important questions remain unanswered. What is the preferred approach to monitor spontaneous breathing effort? How might patient-specific risk:benefit assessments of spontaneous breathing be performed? What impact does short-term neuromuscular blockade have on diaphragmatic and other skeletal muscle function, and do early changes predict long-term functional outcomes? Strategies to blunt spontaneous breathing effort apart from neuromuscular blockade and heavy sedation also merit exploration. For cases where heavy sedation or neuromuscular blockade is needed, strategies to prevent diaphragm & other skeletal muscle atrophy warrant evaluation.
Automated Closed-Loop Ventilation
Automated closed-loop ventilation describes several techniques by which patient physiology is fed back continuously to the ventilator, which in response adjusts support real-time by applying automated algorithms. Closed-loop ventilation has appeal to reduce demands on critical care staffing in regions with workforce shortages. Additionally, automation should be evaluated further to expedite ventilator weaning in recovering patients [35]. Algorithms to minimize patient-ventilator dyssynchrony should be developed and tested. Future studies must continue to develop technologies and refine algorithms. The relevant physiological measures by which to titrate ventilator support in ARDS remain controversial, irrespective of automation, and must be characterized before automation can be considered for ARDS. As lung-protective ventilation practices evolve, closed loop algorithms will require periodic updating to prevent automated use of outdated approaches. Fully automated systems are in development but may be of limited use in patients with ARDS in whom multiorgan failure necessitates ventilator adjustment in the context of other organ systems and co-interventions.
Extracorporeal Support
Veno-venous extracorporeal membrane oxygenation (VV-ECMO) use for ARDS has increased steadily in recent years following major technical improvements. Still, ECMO remains a complex, high-risk, staffing-intensive, and costly procedure for which indications, timing, and optimal management are unclear. CESAR [58], the only multicenter ECMO trial of the modern era, demonstrated referral to an ECMO center improved survival without severe disability at six months compared to usual care. However, one-fourth of patients in the referral arm never received ECMO, and low tidal volume ventilation was less frequent in the control arm, preventing definitive conclusions about ECMO efficacy per se. The ongoing EOLIA trial (NCT01470703) aims to address these issues via randomization to ECMO treatment (rather than to an ECMO referral center) and protocolized ventilator management of both study arms. Uncertainty remains regarding which patients may benefit from ECMO [59], with the answer a moving target as both lung-protective ventilation and ECMO technologies improve in coming years. Optimal management of mechanical ventilatory support, anticoagulation, spontaneous breathing, and other co-interventions while on ECMO, as well as timing of ECMO weaning, must be evaluated.
For patients in whom oxygenation can be maintained with conventional respiratory support, extracorporeal CO2 removal (ECCO2R) may be a more readily scalable alternative. Lower blood flow requirements permit use of smaller catheters that can be inserted more easily. Preliminary data suggest ECCO2R is safe and effective, and should be studied for its potential to enhance prevention of ventilator-induced lung injury by permitting “ultra-low” tidal volumes and respiratory rate without extreme hypercapnia [60, 61]. The potential roles for ECCO2R to facilitate weaning and, paired with noninvasive high-flow oxygen, to prevent endotracheal intubation deserve continued exploration [62, 63]. Improving ECCO2R efficiency, possibly by blood acidification [64] and electrodialysis [65], may further reduce invasiveness and associated complications, expanding potential applications. Anticoagulation requirements must be delineated, including the role of regional anticoagulation. As with ECMO, future studies must identify ARDS subgroups likeliest to benefit and preferred timing of application.
Pharmacotherapy
Failure of countless pharmacotherapies to translate promising preclinical findings to demonstrable patient benefit [66, 67] may be explained in part by the heterogeneous biological responses underpinning ARDS. By contrast, all patients with ARDS regardless of biology appear at risk of ventilator-induced lung injury. To advance ARDS pharmacotherapy development, efforts to characterize distinct biological endotypes must continue [11, 12], with particular emphasis on rapid endotype recognition for use in clinical trial eligibility criteria.
Broadly speaking, targets for drug discovery include enhanced protection against mechanical lung injury, promotion of lung repair, fibroproliferative resolution, and inhibition of systemic “biotrauma” mediators that contribute to extrapulmonary organ failure. Pharmacotherapies tested before the lung-protective ventilation era, applied more than 24–48 hours after ARDS onset, or inclusive of all ARDS rather than the biologically relevant subgroup, may warrant reconsideration. As examples, inhaled pulmonary vasodilators may be effective in the ARDS subgroup with cor pulmonale, and corticosteroids/immunomodulators may be effective if initiated early in the subgroup with severe inflammation [11]. Studies of medications targeting alveolar epithelial and vascular endothelial injury could be restricted to ARDS of direct and indirect origin, respectively [12]. Mesenchymal stem cells are appealing in part for their many paracrine effects (secretion of endothelial and epithelial growth factors, anti-inflammatory cytokines, and antimicrobial peptides) that may act on multiple biological endotypes; early trials are underway to assess whether these biological effects translate to clinical benefit [68]. Effective drug delivery methods must be evaluated for pharmacotherapies administered via inhalation or intratracheal/intrabronchial installation. Candidate therapies at various stages of preclinical and clinical exploration are reviewed elsewhere [66, 67].
Other Interventions
Prone positioning was shown in a recent multicenter trial to improve survival from severe ARDS [69]. Key effects of proning and PEEP on lung mechanics—promoting homogenous strain distribution, recruitment, and ventilation-perfusion matching—may be synergistic and deserve study [70]. The contribution of enhanced tracheobronchial secretion drainage with proning is underexplored. Uncleared proteinaceous or bacteria-containing secretions may contribute to regional inflammation and mechanical heterogeneity, predisposing to further lung injury [71]. Patient positioning, PEEP, and inspiratory:expiratory flow ratio may influence secretion clearance/disbursement [72, 73]; their contribution to lung injury propagation should be explored further.
ADVANCING STUDY DESIGN
Preclinical Studies
Translation of basic research findings to clinical practice remains daunting due to the heterogeneity and complexity of ARDS. Recent basic studies have done well to mirror the multiple-hit hypothesis for ARDS pathogenesis, which states that lung injury occurs most readily with concomitant physiological insults that prime the immune system for an amplified response to mechanical lung stress. However, young, typically healthy animals are managed right after ARDS onset for limited time in these studies. Future animal models should reproduce the comorbidities, risk factors for multiorgan failure, and prolonged critical illness common in patients with ARDS.
Clinical Trial Design
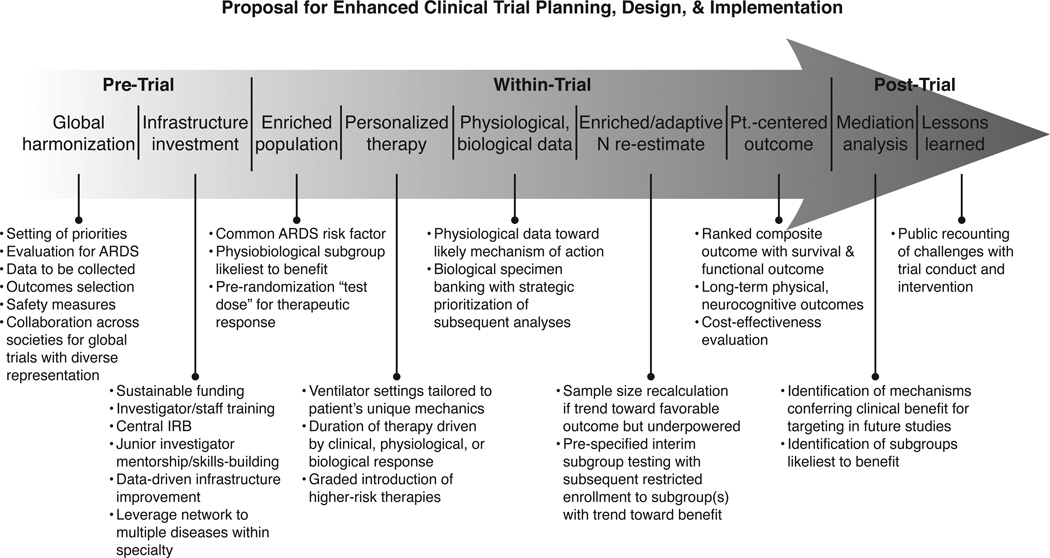
Effective clinical trial design for ARDS (Figure 1) also faces several hurdles to be reconciled in the coming years. ARDS trials are expensive, labor-intensive, and time-consuming to conduct—all the greater a threat to advancing ARDS management given shrinking research budgets across the globe. The need for large-scale trials with many participating sites poses logistical challenges, requires enhanced research infrastructure investment, and adds variability owing to local practice preferences for pertinent co-interventions. As feasibility permits, every effort must be made to collect mechanistic physiological and biological data during the trials, to answer not just whether a treatment is beneficial but why and for whom.
Figure 1.
Proposal for enhanced clinical trial planning, design, and implementation
Compounding sample size issues is the need to focus therapeutic testing in certain cases on ARDS endotypes with the most relevant biological perturbations. Simply grouping patients by severity of oxygenation impairment may not reliably distinguish distinct underlying biological or physiological mechanisms for whom prognosis and therapeutic response may differ. Enrolling patients that share a common clinical risk factor for ARDS is a simple approach to improving biological homogeneity within the study cohort. Point-of-care assays may be needed to analyze biological specimens on-site in real-time before incorporating biomarkers into eligibility criteria.
Adaptive sample size re-estimation with enrichment offers remedy for some powering issues. In adaptive sample size re-estimation, preplanned interim data analyses are used to update power calculations and increase enrollment targets if effect size is slightly underestimated but a favorable trend observed [74]. With adaptive enrichment, prespecified subgroup testing also occurs during interim analyses, after which subsequent enrollment is restricted to the subgroup(s) that appear likeliest to benefit at the interim look [74].
The appropriate control arm for ARDS trials also remains unknown. Trialists must choose between rigidly protocolized co-interventions aimed at best practice, but that limit generalizability, versus usual care arms that risk nonadherence to established practice guidelines. Study protocols’ influence on clinical practice may shift usual care irrespective of ongoing protocol use, helping to circumvent this tension. Usual care arms risk succumbing to the Hawthorne effect, in which care temporarily improves because of the trial’s attention. When usual care arms are employed, additional data may be required to quantify precisely how that arm was managed. Analysis plans must address use of the intervention of study in the usual care arm, which may complicate trial analysis and threaten ability to determine whether the intervention indeed benefits patients.
Intervention design itself may be improved. When relevant, therapeutic duration should be individualized based on clinical response: as the patient improves clinically, the therapy should be de-escalated. This strategy of response-dependent treatment duration was employed in a recent, successful trial of prone positioning [69] but is generally underutilized.
Long-Term Outcomes
Long-term physical, neurocognitive, and psychological morbidities are common among ARDS survivors [75, 76] and should be measured in future trials. Tools for post-ICU physical, neurocognitive, psychological, and independence testing need further development, as do measures early during critical illness that predict these long-term outcomes. Long-term outcomes should be incorporated routinely into ARDS clinical trials, and may help detect clinically relevant treatment effects when mortality does not differ. Added power and clinical relevance may be gained by adopting patient-centered primary outcomes measures in which survival and functional outcomes are combined into a single primary outcome measure, such as the modified Rankin scale or Cerebral Performance Category, both of which are employed routinely in stroke and cardiac arrest trials [77]. Importantly, such measures are not conventional composite outcomes that treat death as equivalent with another outcome. Instead, they simply rank functional status among survivors for further patient-centered granularity of treatment effect. Finally, practice variation in post-discharge management among ARDS survivors should be explored and likely will present additional opportunities for targeted interventions to improve long-term quality of life.
CONCLUSIONS
The previous twenty years have seen considerable increase in ARDS survival. Similarly, clinical practice improvements may have contributed to a decline in nosocomial ARDS incidence. The next twenty years of ARDS research require we ask not just whether novel preventive or therapeutic interventions work, but also in whom. This subtle expansion in scope necessitates acquisition of highly granular biological, physiological, and clinical data as the new standard across studies. Tremendous investment in research infrastructure and cross-institutional collaboration will be vital to fulfilling this agenda.
Acknowledgments
Dr. Schmidt received honoraria for lectures from Maquet. Dr. Spieth received honoraria for lectures from Baxter and Maquet. Dr. Calfee received grants from and consulted for Glaxo Smith Kline, and had travel paid by Boehringer Ingelheim.
Footnotes
Potential Conflicts of Interest: Drs. Beitler, Goligher, Zanella, Martin-Loeches, and Cavalcanti report no potential conflicts of interest.
REFERENCES
- 1.Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 2.ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 3.Thille AW, Esteban A, Fernández-Segoviano P, et al. Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy. Am J Respir Crit Care Med. 2013;187:761–767. doi: 10.1164/rccm.201211-1981OC. [DOI] [PubMed] [Google Scholar]
- 4.Villar J, Pérez-Méndez L, López J, et al. An early PEEP/FIO2 trial identifies different degrees of lung injury in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2007;176:795–804. doi: 10.1164/rccm.200610-1534OC. [DOI] [PubMed] [Google Scholar]
- 5.Villar J, Pérez-Méndez L, Blanco J, et al. A universal definition of ARDS: the PaO2/FiO2 ratio under a standard ventilatory setting--a prospective, multicenter validation study. Intensive Care Med. 2013;39:583–592. doi: 10.1007/s00134-012-2803-x. [DOI] [PubMed] [Google Scholar]
- 6.Rubenfeld GD, Caldwell E, Granton J, et al. Interobserver variability in applying a radiographic definition for ARDS. Chest. 1999;116:1347–1353. doi: 10.1378/chest.116.5.1347. [DOI] [PubMed] [Google Scholar]
- 7.Baldi G, Gargani L, Abramo A, et al. Lung water assessment by lung ultrasonography in intensive care: a pilot study. Intensive Care Med. 2013;39:74–84. doi: 10.1007/s00134-012-2694-x. [DOI] [PubMed] [Google Scholar]
- 8.Costa E, Borges JB, Melo A, et al. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35:1132–1137. doi: 10.1007/s00134-009-1447-y. [DOI] [PubMed] [Google Scholar]
- 9.Victorino JA, Borges JB, Okamoto VN, et al. Imbalances in regional lung ventilation: a validation study on electrical impedance tomography. Am J Respir Crit Care Med. 2004;169:791–800. doi: 10.1164/rccm.200301-133OC. [DOI] [PubMed] [Google Scholar]
- 10.Berkowitz DM, Danai PA, Eaton S, et al. Accurate characterization of extravascular lung water in acute respiratory distress syndrome. Crit Care Med. 2008;36:1803–1809. doi: 10.1097/CCM.0b013e3181743eeb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Calfee CS, Delucchi K, Parsons PE, et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2:611–620. doi: 10.1016/S2213-2600(14)70097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Calfee CS, Janz DR, Bernard GR, et al. Distinct molecular phenotypes of direct vs indirect ARDS in single-center and multicenter studies. Chest. 2015;147:1539–1548. doi: 10.1378/chest.14-2454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vincent JL, Santacruz C. Do we need ARDS? Intensive Care Med. 2016;42:282–283. doi: 10.1007/s00134-015-4120-7. [DOI] [PubMed] [Google Scholar]
- 14.Li G, Malinchoc M, Cartin-Ceba R, et al. Eight-year trend of acute respiratory distress syndrome: a population-based study in Olmsted County, Minnesota. Am J Respir Crit Care Med. 2011;183:59–66. doi: 10.1164/rccm.201003-0436OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 16.Riviello ED, Kiviri W, Twagirumugabe T, et al. Hospital incidence and outcomes of the acute respiratory distress syndrome using the Kigali modification of the Berlin definition. Am J Respir Crit Care Med. 2016;193:52–59. doi: 10.1164/rccm.201503-0584OC. [DOI] [PubMed] [Google Scholar]
- 17.Thille AW, Esteban A, Fernández-Segoviano P, et al. Chronology of histological lesions in acute respiratory distress syndrome with diffuse alveolar damage: a prospective cohort study of clinical autopsies. Lancet Respir Med. 2013;1:395–401. doi: 10.1016/S2213-2600(13)70053-5. [DOI] [PubMed] [Google Scholar]
- 18.Tejera P, Meyer NJ, Chen F, et al. Distinct and replicable genetic risk factors for acute respiratory distress syndrome of pulmonary or extrapulmonary origin. J Med Genet. 2012;49:671–680. doi: 10.1136/jmedgenet-2012-100972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubenfeld GD, Cooper C, Carter G, et al. Barriers to providing lung-protective ventilation to patients with acute lung injury. Crit Care Med. 2004;32:1289–1293. doi: 10.1097/01.ccm.0000127266.39560.96. [DOI] [PubMed] [Google Scholar]
- 20.Koenig HC, Finkel BB, Khalsa SS, et al. Performance of an automated electronic acute lung injury screening system in intensive care unit patients. Crit Care Med. 2011;39:98–104. doi: 10.1097/CCM.0b013e3181feb4a0. [DOI] [PubMed] [Google Scholar]
- 21.Gajic O, Dabbagh O, Park PK, et al. Early identification of patients at risk of acute lung injury: evaluation of lung injury prediction score in a multicenter cohort study. Am J Respir Crit Care Med. 2011;183:462–470. doi: 10.1164/rccm.201004-0549OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Levitt JE, Calfee CS, Goldstein BA, et al. Early acute lung injury: criteria for identifying lung injury prior to the need for positive pressure ventilation. Crit Care Med. 2013;41:1929–1937. doi: 10.1097/CCM.0b013e31828a3d99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bouhemad B, Brisson H, Le-Guen M, et al. Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med. 2011;183:341–347. doi: 10.1164/rccm.201003-0369OC. [DOI] [PubMed] [Google Scholar]
- 24.Zhao Z, Möller K, Steinmann D, et al. Evaluation of an electrical impedance tomography-based Global Inhomogeneity Index for pulmonary ventilation distribution. Intensive Care Med. 2009;35:1900–1906. doi: 10.1007/s00134-009-1589-y. [DOI] [PubMed] [Google Scholar]
- 25.Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med. 2008;359:2095–2104. doi: 10.1056/NEJMoa0708638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beitler JR, Majumdar R, Hubmayr RD, et al. Volume delivered during recruitment maneuver predicts lung stress in acute respiratory distress syndrome. Crit Care Med. 2016;44:91–99. doi: 10.1097/CCM.0000000000001355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chiumello D, Carlesso E, Cadringher P, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med. 2008;178:346–355. doi: 10.1164/rccm.200710-1589OC. [DOI] [PubMed] [Google Scholar]
- 28.Akoumianaki E, Maggiore SM, Valenza F, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med. 2014;189:520–531. doi: 10.1164/rccm.201312-2193CI. [DOI] [PubMed] [Google Scholar]
- 29.Katzenelson R, Perel A, Berkenstadt H, et al. Accuracy of transpulmonary thermodilution versus gravimetric measurement of extravascular lung water. Crit Care Med. 2004;32:1550–1554. doi: 10.1097/01.ccm.0000130995.18334.8b. [DOI] [PubMed] [Google Scholar]
- 30.Craig TR, Duffy MJ, Shyamsundar M, et al. Extravascular lung water indexed to predicted body weight is a novel predictor of intensive care unit mortality in patients with acute lung injury. Crit Care Med. 2010;38:114–120. doi: 10.1097/CCM.0b013e3181b43050. [DOI] [PubMed] [Google Scholar]
- 31.Levitt JE, Bedi H, Calfee CS, et al. Identification of early acute lung injury at initial evaluation in an acute care setting prior to the onset of respiratory failure. Chest. 2009;135:936–943. doi: 10.1378/chest.08-2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Agrawal A, Matthay MA, Kangelaris KN, et al. Plasma angiopoietin-2 predicts the onset of acute lung injury in critically ill patients. Am J Respir Crit Care Med. 2013;187:736–742. doi: 10.1164/rccm.201208-1460OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chew MS, Ihrman L, During J, et al. Extravascular lung water index improves the diagnostic accuracy of lung injury in patients with shock. Crit Care. 2012;16:R1. doi: 10.1186/cc10599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Serpa Neto A, Cardoso SO, Manetta JA, et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome: a meta-analysis. JAMA. 2012;308:1651–1659. doi: 10.1001/jama.2012.13730. [DOI] [PubMed] [Google Scholar]
- 35.Lellouche F, Bouchard P-A, Simard S, et al. Evaluation of fully automated ventilation: a randomized controlled study in post-cardiac surgery patients. Intensive Care Med. 2013;39:463–471. doi: 10.1007/s00134-012-2799-2. [DOI] [PubMed] [Google Scholar]
- 36.The PROVE Network Investigators, for the Clinical Trial Network of the European Society of Anaesthesiology. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014 doi: 10.1016/S0140-6736(14)60416-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frat J-P, Thille AW, Mercat A, et al. High-Flow Oxygen through Nasal Cannula in Acute Hypoxemic Respiratory Failure. N Engl J Med. 2015 doi: 10.1056/NEJMoa1503326. [DOI] [PubMed] [Google Scholar]
- 38.Beitler JR, Schoenfeld DA, Thompson BT. Preventing ARDS: Progress, Promise, and Pitfalls. Chest. 2014;146:1102–1113. doi: 10.1378/chest.14-0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pelosi P, D’Andrea L, Vitale G, et al. Vertical gradient of regional lung inflation in adult respiratory distress syndrome. Am J Respir Crit Care Med. 1994;149:8–13. doi: 10.1164/ajrccm.149.1.8111603. [DOI] [PubMed] [Google Scholar]
- 40.Amato MBP, Meade MO, Slutsky AS, et al. Driving pressure and survival in acute respiratory distress syndrome. N Engl J Med. 2015;372:747–755. doi: 10.1056/NEJMsa1410639. [DOI] [PubMed] [Google Scholar]
- 41.Martin-Loeches I, de Haro C, Dellinger RP, et al. Effectiveness of an inspiratory pressure-limited approach to mechanical ventilation in septic patients. Eur Respir J. 2013;41:157–164. doi: 10.1183/09031936.00221611. [DOI] [PubMed] [Google Scholar]
- 42.National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–336. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 43.Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:637–645. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 44.Caironi P, Cressoni M, Chiumello D, et al. Lung opening and closing during ventilation of acute respiratory distress syndrome. Am J Respir Crit Care Med. 2010;181:578–586. doi: 10.1164/rccm.200905-0787OC. [DOI] [PubMed] [Google Scholar]
- 45.Goligher EC, Kavanagh BP, Rubenfeld GD, et al. Oxygenation response to positive end-expiratory pressure predicts mortality in acute respiratory distress syndrome: a secondary analysis of the LOVS and ExPress Trials. Am J Respir Crit Care Med. 2014;190:70–76. doi: 10.1164/rccm.201404-0688OC. [DOI] [PubMed] [Google Scholar]
- 46.Suzumura EA, Figueiró M, Normilio-Silva K, et al. Effects of alveolar recruitment maneuvers on clinical outcomes in patients with acute respiratory distress syndrome: a systematic review and meta-analysis. Intensive Care Med. 2014;40:1227–1240. doi: 10.1007/s00134-014-3413-6. [DOI] [PubMed] [Google Scholar]
- 47.Cressoni M, Cadringher P, Chiurazzi C, et al. Lung inhomogeneity in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2014;189:149–158. doi: 10.1164/rccm.201308-1567OC. [DOI] [PubMed] [Google Scholar]
- 48.Goligher EC, Kavanagh BP, Rubenfeld GD, Ferguson ND. Physiologic Responsiveness Should Guide Entry into Randomized Controlled Trials. Am J Respir Crit Care Med. 2015;192:1416–1419. doi: 10.1164/rccm.201410-1832CP. [DOI] [PubMed] [Google Scholar]
- 49.Kacmarek RM, Villar J, Sulemanji D, et al. Open lung approach for the acute respiratory distress syndrome: a pilot, randomized controlled trial. Crit Care Med. 2016;44:32–42. doi: 10.1097/CCM.0000000000001383. [DOI] [PubMed] [Google Scholar]
- 50.Grasso S, Stripoli T, De Michele M, et al. ARDSnet ventilatory protocol and alveolar hyperinflation: role of positive end-expiratory pressure. Am J Respir Crit Care Med. 2007;176:761–767. doi: 10.1164/rccm.200702-193OC. [DOI] [PubMed] [Google Scholar]
- 51.Mercat A, Richard J-CM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:646–655. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 52.Amato MB, Barbas CS, Medeiros DM, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:347–354. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 53.Spieth PM, Carvalho AR, Pelosi P, et al. Variable tidal volumes improve lung protective ventilation strategies in experimental lung injury. Am J Respir Crit Care Med. 2009;179:684–693. doi: 10.1164/rccm.200806-975OC. [DOI] [PubMed] [Google Scholar]
- 54.Goligher EC, Fan E, Herridge MS, et al. Evolution of diaphragm thickness during mechanical ventilation: impact of inspiratory effort. Am J Respir Crit Care Med. 2015;192:1080–1088. doi: 10.1164/rccm.201503-0620OC. [DOI] [PubMed] [Google Scholar]
- 55.Yoshida T, Torsani V, Gomes S, et al. Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med. 2013;188:1420–1427. doi: 10.1164/rccm.201303-0539OC. [DOI] [PubMed] [Google Scholar]
- 56.Pohlman MC, McCallister KE, Schweickert WD, et al. Excessive tidal volume from breath stacking during lung-protective ventilation for acute lung injury. Crit Care Med. 2008;36:3019–3023. doi: 10.1097/CCM.0b013e31818b308b. [DOI] [PubMed] [Google Scholar]
- 57.Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 58.Peek GJ, Mugford M, Tiruvoipati R, et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet. 2009;374:1351–1363. doi: 10.1016/S0140-6736(09)61069-2. [DOI] [PubMed] [Google Scholar]
- 59.Schmidt M, Zogheib E, Rozé H, et al. The PRESERVE mortality risk score and analysis of long-term outcomes after extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. Intensive Care Med. 2013;39:1704–1713. doi: 10.1007/s00134-013-3037-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bein T, Weber-Carstens S, Goldmann A, et al. Lower tidal volume strategy (≈3 ml/kg) combined with extracorporeal CO2 removal versus “conventional” protective ventilation (6 ml/kg) in severe ARDS: the prospective randomized Xtravent-study. Intensive Care Med. 2013;39:847–856. doi: 10.1007/s00134-012-2787-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Terragni PP, Del Sorbo L, Mascia L, et al. Tidal volume lower than 6 ml/kg enhances lung protection: role of extracorporeal carbon dioxide removal. Anesthesiology. 2009;111:826–835. doi: 10.1097/ALN.0b013e3181b764d2. [DOI] [PubMed] [Google Scholar]
- 62.Abrams DC, Brenner K, Burkart KM, et al. Pilot study of extracorporeal carbon dioxide removal to facilitate extubation and ambulation in exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2013;10:307–314. doi: 10.1513/AnnalsATS.201301-021OC. [DOI] [PubMed] [Google Scholar]
- 63.Hoeper MM, Wiesner O, Hadem J, et al. Extracorporeal membrane oxygenation instead of invasive mechanical ventilation in patients with acute respiratory distress syndrome. Intensive Care Med. 2013;39:2056–2057. doi: 10.1007/s00134-013-3052-3. [DOI] [PubMed] [Google Scholar]
- 64.Zanella A, Mangili P, Redaelli S, et al. Regional blood acidification enhances extracorporeal carbon dioxide removal: a 48-hour animal study. Anesthesiology. 2014;120:416–424. doi: 10.1097/ALN.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 65.Zanella A, Castagna L, Salerno D, et al. Respiratory electrodialysis: a novel, highly efficient extracorporeal CO2 removal technique. Am J Respir Crit Care Med. 2015;192:719–726. doi: 10.1164/rccm.201502-0289OC. [DOI] [PubMed] [Google Scholar]
- 66.Duggal A, Ganapathy A, Ratnapalan M, Adhikari NK. Pharmacological treatments for acute respiratory distress syndrome: systematic review. Minerva Anestesiol. 2015;81:567–588. [PubMed] [Google Scholar]
- 67.Spieth PM, Zhang H. Pharmacological therapies for acute respiratory distress syndrome. Curr Opin Crit Care. 2014;20:113–121. doi: 10.1097/MCC.0000000000000056. [DOI] [PubMed] [Google Scholar]
- 68.Wilson JG, Liu KD, Zhuo H, et al. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir Med. 2015;3:24–32. doi: 10.1016/S2213-2600(14)70291-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Guerin C, Reignier J, Richard J-C, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368:2159–2168. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 70.Beitler JR, Guerin C, Ayzac L, et al. PEEP titration during prone positioning for acute respiratory distress syndrome. Crit Care. 2015;19:436. doi: 10.1186/s13054-015-1153-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Graf J, Marini JJ. Do airway secretions play an underappreciated role in acute respiratory distress syndrome? Curr Opin Crit Care. 2008;14:44–49. doi: 10.1097/MCC.0b013e3282f2f4cb. [DOI] [PubMed] [Google Scholar]
- 72.Zanella A, Cressoni M, Epp M, et al. Effects of tracheal orientation on development of ventilator-associated pneumonia: an experimental study. Intensive Care Med. 2012;38:677–685. doi: 10.1007/s00134-012-2495-2. [DOI] [PubMed] [Google Scholar]
- 73.Zanella A, Bellani G, Pesenti A. Airway pressure and flow monitoring. Curr Opin Crit Care. 2010;16:255–260. doi: 10.1097/MCC.0b013e328337f209. [DOI] [PubMed] [Google Scholar]
- 74.Mehta C, Gao P, Bhatt DL, et al. Optimizing trial design: sequential, adaptive, and enrichment strategies. Circulation. 2009;119:597–605. doi: 10.1161/CIRCULATIONAHA.108.809707. [DOI] [PubMed] [Google Scholar]
- 75.Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 76.Mikkelsen ME, Christie JD, Lanken PN, et al. The adult respiratory distress syndrome cognitive outcomes study: long-term neuropsychological function in survivors of acute lung injury. Am J Respir Crit Care Med. 2012;185:1307–1315. doi: 10.1164/rccm.201111-2025OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Becker LB, Aufderheide TP, Geocadin RG, et al. Primary outcomes for resuscitation science studies: a consensus statement from the American Heart Association. Circulation. 2011;124:2158–2177. doi: 10.1161/CIR.0b013e3182340239. [DOI] [PMC free article] [PubMed] [Google Scholar]