INTRODUCTION
Gastric stump cancer was first reported as a disease entity by Balfour in 19221 , 6. It was defined initially as cancer that arises in the remnant stomach after five years of gastrectomy for benign disease such as peptic ulcer1 , 6 , 8. Another opinion includes ten-year latency period after primary operation for benign or malignant disease. Cancer recurrence in the stump after ten years of gastrectomy is rare9.
The anatomical region most commonly affected is next to the anastomosis, gastric side. With a prevalence of 1-9% among cases of stomach cancer, it affects between 0.8-8.9% of patients who underwent partial gastric resection for peptic ulcer1.
Reduction in the prevalence of peptic ulcer gastrectomy is reported4 , 8 , 10 due to therapeutic advances, among them drug treatment by Helicobacter pylori infection8 , 10. However, surgery continues to be performed for the complications of peptic ulcer disease, such as perforation, bleeding or stenosis8.
In this article, the authors report two cases of gastric stump cancer after Billroth II gastrectomy for peptic ulcer disease.
CASE REPORTS
Case 1
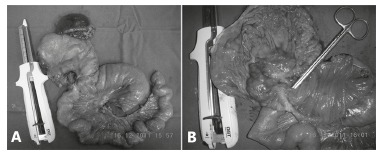
Man, 58, was admitted with hemodynamic instability episodes due to hematemesis and melena, about two weeks. Endoscopy revealed ulcerative-vegetative lesion with elevated borders and infiltrated in gastric stump, with a history of partial gastrectomy Billroth II for more than 20 years for bleeding peptic ulcer. Biopsy revealed invasive gastric adenocarcinoma. He underwent total gastrectomy for gastric remnant (Figure 1) and reconstruction by esophagojejunal terminolateral anastomosis with circular stapler and jejunojejunal laterolateral with linear stapler, and lymphadenectomy, splenectomy and hepatectomy wedge, as a result of tumor infiltration in the left hepatic lobe. Patient died after 10 months of postoperative follow-up.
FIGURE 1. - Product of gastrojejunal resection: A) before the opening of the surgical specimen, and B) with mucosal exposure.
Case 2
Man, 71, underwent partial gastrectomy Billroth II for more than 30 years due to gastric ulcer. It was admitted complaining bloating, vomiting, epigastric pain and weight loss of 5 kg in two months. Endoscopy showed infiltrative lesion in anastomotic edge and biopsy showed moderately differentiated adenocarcinoma. Underwent total gastrectomy, lymphadenectomy to D2, splenectomy, omentectomy and enterectomy in block. The reconstruction of the digestive tract was done through esophagojejunal terminolateral anastomosis with circular stapler, and enteroanastomosis jejunojejunal 5 cm from the duodenojejunal angle done manually. On the 1st day of postoperative period progressed with hemodynamic instability and was referred to the intensive care unit. Underwent endoscopy that showed presence of signs suggestive of ischemia in esophagojejunal anastomosis. It was decided to keep him in conservative medical treatment and total parenteral nutrition, but died on the 30th day after surgery.
DISCUSSION
Partial gastrectomy for peptic ulcer disease is a risk factor for gastric cancer8. The main pathogenesis of gastric stump cancer is biliary-pancreatic reflux causing chronic inflammation of the remaining mucosa, developing into atrophic gastritis, intestinal metaplasia and displasia1. Other possible causes are: 1) hypo- or achlorhydria, resulting in bacterial overgrowth and increased exposure of carcinogenic agents, for example, nitrosamines7 , 8; 2) effect of hormonal regulation after vagotomy and hipogastrinemia7; 3) presence of surgical suture1; and 4) Epstein-Barr virus. The latter occurs most commonly in the gastric stump, unlike Helicobacter pylori infection, more frequent in the intact stomach8.
The H. pylori infection is considered the main risk factor for adenocarcinoma2. However, its role in gastric stump cancer is unlikely, since the infection rate in these patients is lower. Furthermore, the gastric remnant is unfavorable environment for the colonization of microorganisms because of biliopancreatic alcaline reflux5 , 6.
There is a larger number of cases of gastric stump cancer after reconstruction Billroth II, when compared to Billroth I. This is explained by the fact that in the first place inflammation and regeneration of the gastric mucosa, the persistent contact of the anastomosis of gastric stump with the biliary acids9.
The most common location of the tumor in the remnant stomach depends on the type of operation carried out previously. When the technique is Billroth II, it is more frequent in the anastomosis area, while in Billroth I in non anastomotic9.
The interval between initial gastrectomy and diagnosis of gastric cancer stump is greater when the first operation was due to benign disease, than to malignant6 , 9 , 10. This observation is probably a result of the difference in age of the patient when the initial gastrectomy was done, in both groups, as peptic ulcer usually occurs in younger patients than cancer6 , 10.
Survey conducted in 95 institutions in Japan found more cases between 10-15 years of operation in patients whose initial lesion was malignant. In gastrectomy for peptic ulcer disease the peak incidence occurred around the fourth decade after operation9.
Gastric stump cancer surgically treated has bad prognosis. Was observed lower five-year survival in patients with gastric stump cancer than those with primary gastric cancer10. The treatment of choice is surgical D2 resection of remaining stomach, plus lymphadenectomy including organs and other adjacent lymph nodes resection3.
To improve results is necessary early diagnose. Therefore, endoscopic surveillance should be considered10. However, there is no consensus in the literature on the screening of gastric stump cancer after gastrectomy. For some, the endoscopic surveillance program should start one year till at least ten years6. For others, gastrectomy for peptic ulcer disease should continue beyond ten years4 , 6 , 10. But everyone agrees on the need for early cancer detection and appropriate follow-up program10.
Footnotes
Financial source: none
REFERENCES
- 1.Carrasco AL, Bresciani CJ, Perez RO, Zilberstein B, Cecconello I. Influência da invasão tumoral da linha de anastomose na sobrevivência de pacientes com câncer de coto gástrico. ABCD Arq. Bras. Cir. Dig. 2008;21(2):55–60. [Google Scholar]
- 2.Coelho LG, Maguinilk I, Zaterka S, Parente JM, Passos MC, Morais- JP., Filho 3rd Brazilian Consensus on Helicobacter pylori. Arq Gastroenterol. 2013;50(2):81–96. doi: 10.1590/S0004-28032013005000001. [DOI] [PubMed] [Google Scholar]
- 3.Hu X, Tian DY, Cao L, Yi Y. Progression and prognosis of gastric stump cancer. J. Surg. Oncol. 2009;100:472–476. doi: 10.1002/jso.21370. [DOI] [PubMed] [Google Scholar]
- 4.Lagergren J, Lindam A, Mason RM. Gastric stump cancer after distal gastrectomy for benign gastric ulcer in a population-based study. Int. J. Cancer. 2012;131:E1048–E1052. doi: 10.1002/ijc.27614. [DOI] [PubMed] [Google Scholar]
- 5.Monés J. Role of Helicobacter pylori in gastric cancer following partial gastrectomy for benign ulcer. Rev. Esp. Enferm. Dig. 2005;97(11):767–777. doi: 10.4321/s1130-01082005001100001. [DOI] [PubMed] [Google Scholar]
- 6.Namikawa T, Kitagawa H, Iwabu J, Okabayashi T, Kobayashi M, Hanazaki K. Tumors arising at previous anastomotic site may have poor prognosis in patients with gastric stump cancer following gastrectomy. J. Gastrointest. Surg. 2010;14:1923–1930. doi: 10.1007/s11605-010-1298-4. [DOI] [PubMed] [Google Scholar]
- 7.Safatle-Ribeiro AV, Ribeiro U, Jr, Sakai P, Iriya K, Ishioka S, Gama-Rodrigues J. Gastric stump mucosa: is there a risk for carcinoma? Arq. Gastroenterol. 2001;38(4):227–231. doi: 10.1590/s0004-28032001000400004. [DOI] [PubMed] [Google Scholar]
- 8.Sitarz R, Maciejewski R, Polkowski WP, Offerhaus GJ. Gastroenterostoma after Billroth antrectomy as a premalignant condition. World J. Gastroenterol. 2012;18(25):3201–3206. doi: 10.3748/wjg.v18.i25.3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tanigawa N, Nomura E, Lee SW, Kaminishi M, Sugiyama M, Aikou T, Kitajima M, The Society for the Study of Postoperative Morbidity after Gastrectomy Current state of gastric stump carcinoma in Japan: based on the results of a nationwide survey. World J. Surg. 2010;34:1540–1547. doi: 10.1007/s00268-010-0505-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tokunaga M, Sano T, Ohyama S, Hiki N, Fukunaga T, Yamada K, Yamaguchi T. Clinicopathological characteristics and survival difference between gastric stump carcinoma and primary upper third gastric cancer. J. Gastrointest. Surg. 2013;17:313–318. doi: 10.1007/s11605-012-2114-0. [DOI] [PubMed] [Google Scholar]


