Abstract
This study aims to assess the efficacy of a radiation therapy (RT) education video for patients referred for treatment. The investigators produced a 23-min guide to radiation therapy DVD, combining didactic material and patient narratives. Patients (n=32) had not yet received their initial consultation. Baseline awareness about cancer and treatment was assessed by surveys including the rapid estimate of adult literacy in medicine. Knowledge about RT was assessed before and after viewing the video with a separate 21 question survey. Differences in benefit for sociodemographic subgroups including age, gender, ethnicity, income, education, and health literacy level were explored. Baseline assessments identified 78 % of patients regardless of sociodemographic status had “little” to “no” basic knowledge of RT. The mean number of correct responses in the 21 question survey assessing how RT works improved from 9.8 to 11.1 after watching the video (p<0.0001; 95 % CI: 1.3–3.0), a statistically significant benefit that was present among all sociodemographic subgroups, but more prominent among those with a greater than high school education (p=0.002). Patient satisfaction with the video was high. Knowledge among cancer patients regarding RT is poor, regardless of sociodemographic factors. This pilot study demonstrates the utility of a brief video to universally improve patient awareness about RT. While patients may ultimately learn about RT during their course of treatment, we advocate for any tools that can improve patient knowledge at the time of initial consultation as this is typically the time they are asked to acknowledge informed consent for treatment.
Keywords: Radiation therapy, Video/film, Patient education
Introduction
According to the American Society for Radiation and Oncology, two thirds of cancer patients will receive radiation at some point during the course of their care [1]. Each year, this represents approximately one million cancer patients, with 23.4 million visits to 2,010 hospitals and radiation centers [1]. Initial consults with radiation oncologists are often confusing due to the technical nature of the treatment. Unfortunately, many patients are often unaware of what to expect with radiation therapy (RT; e.g., some believe it may be a painful procedure like surgery) and may not be able to absorb the amount of information typically provided at time of consultation with a radiation oncologist [2, 3]. Additionally, the radiotherapy treatment machines can be overwhelming or frightening to patients who are not prepared, and the procedures may be alarming (e.g., the idea of a mask placed on the head or needing to stay still during the daily procedure, fear of radioactivity, burns, and other toxicity).
To address the challenges of educating patients at time of consultation, the supplemental role of a patient-oriented educational video has been previously explored. Several investigators have reported high levels of satisfaction with this strategy and demonstrated their value for patients [2–4]. Research in cancer care has tested educational videos as interventions for increasing screening knowledge and decision-making participation of patients with prostate cancer, aiding in the transition from patient to survivor for women with breast cancer, increasing participation in clinical trials for both breast cancer and lung cancer patients, and improving pain education in minority cancer patients [5–7]. Three studies included an educational video for radiation oncology patients [2–4]. In each study, participants reported high levels of satisfaction with the video and felt that it provided necessary information. However, there remains a paucity of evidence in the literature to support its widespread use. In particular, many radiation oncology clinics may have limited staff or time to develop and/or distribute educational videos to cancer patients. Thus, we studied the value of viewing an educational video before the initial radiation oncology consultation. Surveys were used to measure its impact on increasing knowledge about important issues for patients undergoing radiation therapy for their cancers.
Methods and Materials
Patients
Patients referred for a radiation oncology consultation were recruited before their initial evaluation. Individuals eligible to participate in this study had never received radiation therapy, were 18 years and older, and fluent in English. This was a small pilot of a general informational DVD appropriate for any patient scheduled for an RT consultation, thus data on cancer type and stage were not collected, as power was inadequate for any meaningful analyses. Participants were paid $25 upon study completion. This study was approved by the Virginia Commonwealth University Institutional Review Board.
Materials
While the purpose of this study is to evaluate the effectiveness of an RT information video in general, the use of a specific video created by the investigators ensured congruence between the information presented and patients’ treatment. Previous studies by Matsuyama identified a need for educational materials that were not reliant on the written word [8–11]. In recent focus groups and in-depth interviews, cancer patients identified content that was meaningful to them for inclusion in a video (unpublished data). The investigators then produced a 23-min “Guide to Radiation Therapy” DVD developed using these data collected from cancer patients and co-written by a Radiation Oncologist (DM) and expert in patient information needs (RM0). A professional actor narrated the written script which overviewed essential knowledge related to radiation therapy, and actors with nonspeaking roles helped walk the viewer through various phases of RT treatment planning and delivery. Real patients who had received RT were interviewed on film, and invited to share their stories. The DVD was supplemented with animation and music, and professionally edited. Topics covered by the video included an introduction to cancer and discussions about the importance of adhering to prescribed treatment, attending to side effects, nutrition, having a support system, and importance of asking questions from healthcare providers. The DVD was divided into chapters so patients can view or re-view specific topics without having to watch the entire film.
Assessments
Baseline assessments included three surveys: (1) sociodemographics; (2) assessment of health literacy using the Rapid Estimate of Adult Literacy in Medicine (REALM) [12], a test that stratifies patients into grade levels of below third grade, fourth–sixth grade, seventh–eighth grade, and greater than or equal to ninth grade; and (3) an eight-item questionnaire to assess patients’ understanding of “How RT is Delivered” (see Appendix 1).
To assess the value of the DVD, a separate 21-item questionnaire assessing patients’ understanding of “How RT Works” was developed and administered before (pre-test) and after (post-test) viewing the DVD, which included 15 topics covered in the video (Appendix 2). Due to logistical challenges of conducting the study in a busy clinic, the post-test survey was administered either immediately (66 %) or 1 week (34 %) after viewing the DVD. As no differences in correct responses were identified, these two sets of post-test assessments were combined for analysis.
Finally, a six-question satisfaction survey was administered which included three open-ended questions (Appendix 3). With the exception of the REALM (which requires the participant to read a list of words aloud), measures were verbally administered by research staff.
Statistics
The pre- and post-test scores and differences for the 15 RT knowledge questions were summarized with means, standard deviations, and 95 % confidence intervals. A paired t test was used to test the hypothesis that there was a change in RT knowledge after viewing the DVD.
Analysis was stratified by age (18–45, 46–65, and 65+), gender (male and female), ethnicity (Caucasian-American and African-American), income (≤100 % poverty level, 100–300 % poverty level, >300 % poverty level) [13], health literacy (sixth grade or below and seventh grade or above), and education (high school diploma or less and greater than high school diploma). An equal-variance ANOVA was used to determine any differences regarding pre-test, baseline scores within subgroups. An ANCOVA model was used for each subgroup to determine any difference in test scores from pre- to post-test controlling for significant differences in baseline scores as determined by the associated ANOVA model. The model examined the relationship between pre-test score, subgroup, and the interaction of the two variables with the dependent variable of change in test score from pre- to post-test. If significance was determined for the model, but there was no significant interaction between subgroups and pre-test scores, then the predicted change in test scores between subgroup was compared using the group main effect centered at the overall pre-test score mean. Predicted follow-up measurements and their differences were summarized with means, standard errors, and 95 % confidence intervals if a significant difference was determined. For all analyses, significance was determined at the level of α=0.05. SAS JMP version 9 was used for all summaries and analyses [14].
Results
Participant Characteristics
Participants (n=32) included 13 (41 %) African Americans, 18 (56 %) Caucasian Americans, and 1 (3 %) multiracial (Table 1). The mean age was 54 (range, 21–82 years), 53 % were female, and 63 % had at least a high school (HS) education. The majority of participants (81 %) scored above seventh grade on the REALM. Nearly half of participants (44 %) reported incomes below the US poverty level (PL) of ≤$11,170 annual income [13], and only 24 % had an income greater than $33,510 (≥301 % PL).
Table 1.
Sociodemographic characteristics of participants
| N=32 | Frequency | Percent |
|---|---|---|
| Gender | ||
| Male | 15 | 46.9 |
| Female | 17 | 53.1 |
| Total | 32 | 100.0 |
| Age (years) | ||
| 18–45 | 9 | 28.1 |
| 46–65 | 16 | 50.0 |
| 66+ | 7 | 21.9 |
| Total | 32 | 100 |
| Ethnicity | ||
| African American | 13 | 40.6 |
| White | 18 | 56.3 |
| Multi-racial | 1 | 3.1 |
| Total | 32 | 100.0 |
| Education | ||
| Less than or equal to high school diploma | 12 | 37.5 |
| Greater than high school diploma | 20 | 62.5 |
| Total | 32 | 100.0 |
| REALM equivalence | ||
| Sixth grade or below | 6 | 18.7 |
| Seventh grade or above | 26 | 81.3 |
| Total | 32 | 100.0 |
| Personal income (past 12 months) | ||
| ≤$11,170 (≤100 % poverty level (PL)) | 11 | 44.0 |
| $11,171–33,510 (101–≥300 % PL) | 8 | 32.0 |
| >$33,511 (>300 % PL) | 6 | 24.0 |
| Total | 25 | 100.0 |
Baseline RT Understanding of “How Radiation Therapy is Delivered”
The majority of patients reported limited understanding of how RT is delivered. A total of 78 % rated their understanding of external beam RT as “a little bit” or “not at all”. Similarly, the vast majority reported “a little bit” to “not at all” understanding of differences between external beam radiation and brachytherapy (91 %), the purpose of radiation tattoos (81 %), how radiation is administered (71 %), and the role of the radiation oncologist (63 %). In contrast, the majority of patients reported good (“quite a bit” or “very much”) understanding of how communicating with the clinical team helps (72 %), what cancer is (65 %), and the role of nutrition during RT (65 %).
Understanding How Radiation Therapy Works and Impact of Video
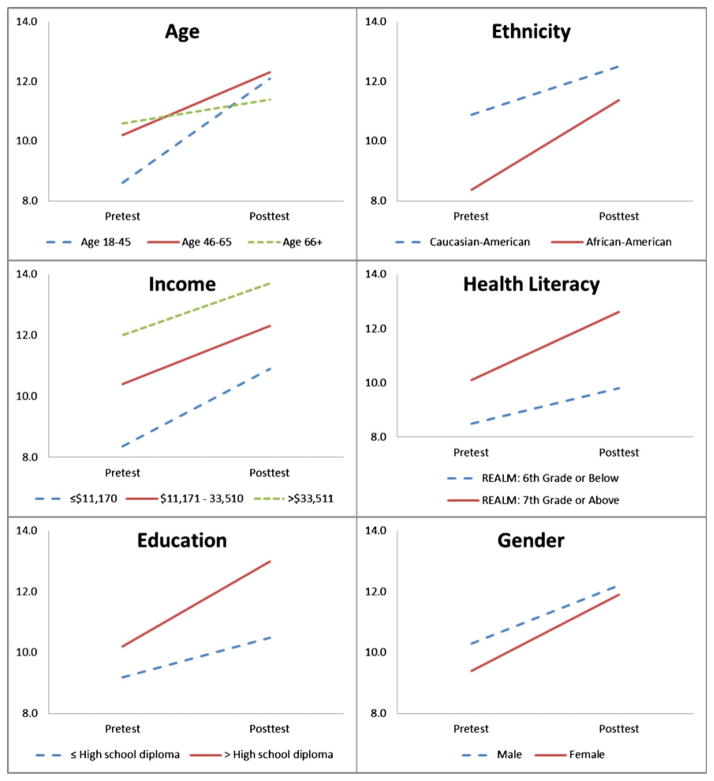
The mean RT knowledge score of all subjects prior to watching the video (pre-test) was 9.8 (SD=2.67) and subsequently increased 2.3 units at post-test (improved score 95 % CI: 1.3–3.0, p<0.0001). A statistically significant improvement was identified among each of the six sociodemographic groups (see Fig. 1 and Table 2). Interaction testing demonstrated patients benefited equally regardless of age, gender, ethnicity, income, or health literacy. Meanwhile, although both patients with less than and greater than a HS diploma benefited, the improvement was more pronounced among patients with a higher than HS education (p=0.0024).
Fig. 1.
Change in mean RT Knowledge score from pre- to post-test by group
Table 2.
RT knowledge score pre-test and change for each group
| Group | n | Pre-test mean score
|
Change in score from pre to post
|
|||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95 % CI | Mean | SD | 95 % CI | p value | ||
| Total | 32 | 9.8 | 2.67 | 8.9, 10.8 | +2.30 | 2.09 | 1.5, 3.0 | <0.0001a |
| Age (years) | ||||||||
| 18–45 | 9 | 8.6 | 2.19 | 6.9, 10.2 | +3.60 | 2.60 | 1.6, 5.6 | 0.0156b |
| 46–65 | 16 | 10.2 | 2.99 | 8.6, 11.8 | +2.10 | 1.63 | 1.3, 3.0 | 0.0004a |
| 66+ | 7 | 10.6 | 2.15 | 8.6, 12.6 | +0.90 | 1.46 | −0.5, 2.2 | 0.2500 |
| Difference | 0.2167 | |||||||
| Gender | ||||||||
| Male | 15 | 10.3 | 2.81 | 8.7, 11.8 | +1.90 | 1.83 | 0.9, 2.9 | 0.0020a |
| Female | 17 | 9.4 | 2.55 | 8.1, 10.7 | +2.50 | 2.32 | 1.3, 3.7 | 0.0006a |
| Difference | 0.7136 | |||||||
| Ethnicitya | ||||||||
| African American | 13 | 8.4 | 2.81 | 6.7, 10.1 | +3.00 | 1.87 | 1.9, 4.1 | 0.0002a |
| Caucasian American | 18 | 10.9 | 2.14 | 9.8, 12.0 | +1.60 | 2.12 | 0.6, 2.7 | 0.0065a |
| Difference | 0.5508 | |||||||
| Reported incomes below | ||||||||
| ≤$11,170 (≤100 % Poverty Level) | 11 | 8.4c | 2.42 | 6.7, 10.0 | +2.50 | 2.11 | 1.1, 4.0 | 0.0078a |
| $11,171–33,510 (100>×≥300 % PL) | 8 | 10.4 | 2.97 | 7.9, 12.9 | +1.90 | 2.17 | 0.1, 3.7 | 0.0625 |
| >$33,511 (>300 % PL) | 6 | 12.0c | 1.55 | 10.4, 13.6 | +1.70 | 1.86 | −0.3, 3.6 | 0.1250 |
| Difference | 0.0934 | |||||||
| Health literacy | ||||||||
| Sixth grade or below | 6 | 8.5 | 3.15 | 5.2, 11.8 | +1.30 | 1.37 | −0.1, 2.8 | 0.1250 |
| Seventh grade or above | 26 | 10.1 | 2.52 | 9.1, 11.1 | +2.50 | 2.20 | 1.6, 3.3 | 0.0001a |
| Difference | 0.0527 | |||||||
| Education | ||||||||
| ≤High school diploma | 12 | 9.2 | 2.79 | 7.4, 10.9 | +1.30 | 1.97 | 0.1, 2.6 | 0.0449b |
| >High school diploma | 20 | 10.2 | 2.59 | 9.0, 11.4 | +2.80 | 2.02 | 1.9, 3.7 | 0.0001a |
| Difference | 0.0024a | |||||||
Denotes significance at α=0.05
Denotes significance at α=0.01
Difference between “≤100 % PL” and “>300 % PL” significant at Tukey’s adjusted α=0.05
Patient Satisfaction and Feedback
All participants (100 %) reported they learned new information from the DVD and felt they were better prepared for RT than before watching it. Seven reported they had additional questions after watching it. Three participants found the DVD boring and no participants found the DVD frightening. Overall, patients’ responses to the DVD were enthusiastic and there were few suggestions for change, with the exception of shortening the DVD by about 5 min. Patients’ suggestions were incorporated in the final production edit of the DVD. When asked the three most important things they learned, participants most frequently cited: the importance of not missing any RT appointments, possible side effects, asking questions during appointments, having a support system, and general understanding of RT and its effects on cancer cells.
Discussion
Research has demonstrated patients derive great value from health information that can help them better understand the biology of their malignancy, make decisions, and cope with treatments [15–18]. In the current study, nearly 80 % of patients described limited to no knowledge of basic principles related in radiation therapy at their baseline assessment, a finding that was similar across all six sociodemographic subgroups. Meanwhile, trying to learn all the aspects of radiation therapy at the time of initial consultation can be overwhelming for a patient diagnosed with either potentially curative or terminal cancer. Despite a traditionally lengthy initial consultation, patients referred for RT often remain uninformed despite having received the necessary information. Recently, Guleser, Tasci, and Kaplan reported over half of radiation oncology patients perceived they had not received adequate treatment information prior to treatment, and over 83 % of patients with treatment complications wanted more information [19].
While physicians are the primary and most influential sources of information, they cannot deliver all, or even most, of the cancer care information that may be required by patients, and generally do not tailor their delivery of information to the knowledge levels of their patients [20]. Depending on clinical resources, patients may have access to alternative learning strategies including other healthcare providers (e.g., nurses), informal social networks, and the Internet. However, this is not always the case, and a potentially optimal and more cost-effective strategy may include the use of educational videos, which have been shown to be useful for educating patients. Along with the aforementioned use in oncology, educational video interventions have also been effectively used in a variety of health-oriented settings for different purposes, including improving knowledge of disease, enhancing patient–physician communication in patients with diabetes, improving older adults’ ability to comprehend and recall cholesterol information, and increasing medication adherence behaviors in patients with HIV/AIDS [21–23].
The presented proof of concept study demonstrates a patient-oriented video such as this one co-written by a radiation oncologist and expert in patient health literacy can significantly improve patient understanding of how radiation therapy works. With an improvement seen across all socioeconomic subgroups, these findings suggest the vast majority of patients may benefit from this simple and effective educational tool that may better prepare them for their initial radiation oncology consultation, and subsequent journey through the highly complicated treatment planning and delivery process. With the widespread availability of DVD players and computers in clinics, the use of an educational video has the potential for easy distribution, and could even be viewed through websites for those who have access to the internet.
The authors acknowledge the limitations associated with any pilot study with a small sample size. Also, knowledge assessment was completed with a measure developed for this study that was not previously evaluated for validity and reliability. Additionally, post-test evaluations were done soon after viewing the video, and thus information retention long-term cannot be determined. Results may have also been confounded by the 34 % of patients who completed the post-test 1 week after viewing the video. However, a separate analysis did not identify any difference in correct response rates among those patients and the 66 % who were assessed immediately after viewing the video. Other limitations include the unknown influence of background information before watching the video. However, it once again appeared all patients benefited from the video, regardless of prior knowledge. Ultimately, it remains unknown if use of a video provides any supplemental value in addition to the face-to-face physician consultation; a question which will be further explored. The authors are planning a randomized clinical trial with adequate power to assess the long-term effects of the video on knowledge retention, patient satisfaction, and adherence to treatment. The suggestions of patients who have completed radiation treatment will be incorporated into future versions of the film.
Conclusion
A deficit in knowledge about basic principles related to radiation therapy was demonstrated among over three quarters of patients referred for treatment, a finding that was uniform regardless of age, gender, ethnicity, income, education, or health literacy level. This pilot study successfully demonstrates the utility of a brief video presented before the initial radiation oncology consultation to significantly improve health literacy across all socioeconomic subgroups, suggesting educational videos may be universally beneficial for all radiation oncology patients. While patients may ultimately learn about RT during their course of treatment, we advocate for any tools that can improve patient knowledge at the time of initial consultation, as this is typically the time they are asked to provide informed consent for treatment.
Acknowledgments
Funding in part by: Massey Cancer Center, Richmond, VA, USA and The American Cancer Society (MSRGT-08-143-01-CPPB #).
Appendix 1. Understanding how radiation treatment is delivered
| Not at all | A little bit | Somewhat | Quite a bit | Very well | |
|---|---|---|---|---|---|
| 1. I understand how external beam radiation works | 0 | 1 | 2 | 3 | 4 |
| 2. I understand what cancer is | 0 | 1 | 2 | 3 | 4 |
| 3. I understand the role of the radiation oncologist | 0 | 1 | 2 | 3 | 4 |
| 4. I understand the purpose of tattoos for radiation | 0 | 1 | 2 | 3 | 4 |
| 5. I understand the differences between external beam radiation and brachytherapy | 0 | 1 | 2 | 3 | 4 |
| 6. I understand how radiation is administered | 0 | 1 | 2 | 3 | 4 |
| 7. I understand how communicating with the doctor and radiation team helps | 0 | 1 | 2 | 3 | 4 |
| 8. I understand the role of nutrition during therapy | 0 | 1 | 2 | 3 | 4 |
Appendix 2. Understanding how radiation therapy works
-
1
Which of the following best describes radiation therapy?
X-rays that destroy cancer cells
Drugs that destroy cancer cells
Surgery that removes a tumor
-
2
When cancer is called “inoperable”, what does that mean?
Radiation therapy cannot be used
Surgery cannot be used
Chemotherapy cannot be used
-
3
Radiation can injure both healthy and cancer cells.
True
False
-
4
When cancer cells are growing, they are at their weakest.
True
False
-
7
External beam radiation therapy makes people radioactive after treatment is over.
True
False
-
10
Once radiation therapy is complete, there is no benefit for a patient to see their radiation oncologist.
True
False
-
11
“Palliative” radiation is used to:
Cure cancer
Reduce symptoms, without trying to cure
Stop infection
-
13
Side effects from radiation therapy can develop years after treatment is complete.
True
False
-
14
Radiation can temporarily make cancers grow faster.
True
False
-
15
Missing a few treatments during radiotherapy does not make a difference, as long as all treatments are completed.
True
False
-
16
Radiation treatment using radioactive seeds is an option for all cancers.
True
False
-
18
It is a good idea to try to lose weight during radiation therapy.
True
False
-
19
Radiation works by:
Treating all cancers throughout the entire body
Selectively targeting only precise spots in the body
-
20
Radiation cannot be given all at one time because it would make a patient too sick.
True
False
-
21
Cancer cells can take months to die after radiation treatment is completed.
True
False
Appendix 3. Satisfaction with the video
-
I learned things about radiation therapy that I did not know before.
True
False
-
I found the video scary.
True
False
-
I found the video depressing.
True
False
-
I feel like I better understand what to expect with radiation therapy.
True
False
-
I had more questions at the end of the video than before I watched it.
True
False
-
I found the video boring.
True
False
What were the three most important things you learned from the video
What did you like about the video?
What did you dislike about the video?
Please suggest changes that would improve the video.
Contributor Information
Robin K. Matsuyama, Email: rmatsuyama@vcu.edu, Massey Cancer Center, Virginia Commonwealth University, Richmond, VA, USA. Department of Social and Behavioral Health, School of Medicine, Virginia Commonwealth University, PO Box 980149, Richmond, VA 23298-0149, USA
Laurie J. Lyckholm, Hematology/Oncology and Palliative Care, School of Medicine, Virginia Commonwealth University, Richmond, VA, USA
Anthony Molisani, Department of Social and Behavioral Health, School of Medicine, Virginia Commonwealth University, PO Box 980149, Richmond, VA 23298-0149, USA.
Drew Moghanaki, Department of Radiation Oncology, School of Medicine, Virginia Commonwealth University, Richmond, VA, USA.
References
- 1. [Accessed 18 Feb 2013];The American Society for Radiation Oncology Fast Facts About Radiation Therapy. https://www.astro.org/News-and-Media/Media-Resources/FAQs/Fast-Facts-About-Radiation-Therapy/Index.aspx.
- 2.Dunn J, Steginga SK, Rose P, Scott J, Allison R. Evaluating patient education materials about radiation therapy. Patient Educ Couns. 2004;52:325–332. doi: 10.1016/S0738-3991(03)00108-3. [DOI] [PubMed] [Google Scholar]
- 3.Jahraus D, Sokolosky S, Thurston N, Guo D. Evaluation of an education program for patients with breast cancer receiving radiation therapy. Cancer Nurs. 2002;25:266–275. doi: 10.1097/00002820-200208000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Hahn CA, Fish LJ, Dunn RH, Halperin EC. Prospective trial of a video educational tool for radiation oncology patients. Am J Clin Oncol. 2005;28:609–612. doi: 10.1097/01.coc.0000182417.94669.a0. [DOI] [PubMed] [Google Scholar]
- 5.Du W, Mood D, Gadgeel S, Simon MS. An educational video to increase clinical trials enrollment among breast cancer patients. Breast Cancer Res Treat. 2009;117:339–347. doi: 10.1007/s10549-009-0311-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Partin M, Nelson D, Radosevich D, Nugent S, Flood A, Dillon N, Holtzman J, Haas M, Wilt T. Randomized trial examining the effect of two prostate cancer screening educational interventions on patient knowledge, preferences, and behaviors. J Gen Intern Med. 2004;19:835. doi: 10.1111/j.1525-1497.2004.30047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stanton AL. Outcomes from the Moving Beyond Cancer psychoeducational, randomized, controlled trial with breast cancer patients. J Clin Oncol. 2005;23:6009. doi: 10.1200/JCO.2005.09.101. [DOI] [PubMed] [Google Scholar]
- 8.Matsuyama RK, Grange C, Lyckholm LJ, Utsey SO, Smith TJ. Cultural perceptions in cancer care among African-American and Caucasian patients. J Natl Med Assoc. 2007;99(10):1113–1119. [PMC free article] [PubMed] [Google Scholar]
- 9.Matsuyama RK, Grange C, Lyckholm LJ, Smith TJ. African-American and Caucasian female patients’ cancer and treatment information needs and preferred information sources. J Clin Oncol. ASCO Annual Meeting Proceedings Part I. 2007;25(18S ):9073. June 20 Supplement. [Google Scholar]
- 10.Matsuyama RK, Wilson-Genderson M, Kuhn L, Moghanaki D, Vachhani H, Paasche-Orlow M. Education level, not health literacy, associated with information needs for patients with cancer. Patient Educ Couns. 2011;85(3):e229–e236. doi: 10.1016/j.pec.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 11.Matsuyama RK, Kuhn LA, Molisani A, Wilson-Genderson MC. Cancer patients’ information needs the first nine months after diagnosis. Patient Educ Couns. 2013;90:96–102. doi: 10.1016/j.pec.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 12.Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, Bairnsfather LE. Rapid assessment of literacy levels of adult primary care patients. Fam Med. 1991;23:433–435. [PubMed] [Google Scholar]
- 13.Department of Health and Human Services. Annual update of the HHS poverty guidelines. Fed Regist. 2012;77:4034. [Google Scholar]
- 14.SAS Institute Inc. SAS 9.1. 2004. [Google Scholar]
- 15.Rutten LJ, Squiers L, Hesse B. Cancer-related information seeking: hints from the 2003 Health Information National Trends Survey (HINTS) J Health Commun. 2006;11(Suppl 1):147–156. doi: 10.1080/10810730600637574. [DOI] [PubMed] [Google Scholar]
- 16.Squiers L, Finney Rutten LJ, Treiman K, Bright MA, Hesse B. Cancer patients’ information needs across the cancer care continuum: evidence from the cancer information service. J Health Commun. 2005;10(Suppl 1):15–34. doi: 10.1080/10810730500263620. [DOI] [PubMed] [Google Scholar]
- 17.Smith TJ, Dow LA, Virago E, Khatcheressian J, Lyckholm LJ, Matsuyama R. Giving honest information to patients with advanced cancer maintains hope. Oncology (Williston Park) 2010;24:521–525. [PubMed] [Google Scholar]
- 18.Smith TJ, Dow LA, Virago EA, Khatcheressian J, Matsuyama R, Lyckholm LJ. A pilot trial of decision aids to give truthful prognostic and treatment information to chemotherapy patients with advanced cancer. J Support Oncol. 2011;9:79–86. doi: 10.1016/j.suponc.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guleser GN, Tasci S, Kaplan B. The experience of symptoms and information needs of cancer patients undergoing radio-therapy. J Cancer Educ Off J Am Assoc Cancer Educ. 2012;27:46–53. doi: 10.1007/s13187-011-0254-7. [DOI] [PubMed] [Google Scholar]
- 20.Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns. 2006;62:355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Brock TP, Smith SR. Using digital videos displayed on personal digital assistants (PDAs) to enhance patient education in clinical settings. Int J Med Inform. 2007;76:829–835. doi: 10.1016/j.ijmedinf.2006.09.024. [DOI] [PubMed] [Google Scholar]
- 22.O’Hara L, Shue C, Marini D, Flanagan J, McKenzie J. Diabetes and low health literacy: designing a mediated intervention to enhance patient–physician communication. Comm Ed. 2008;59(3):360–373. [Google Scholar]
- 23.Pepe MV, Chodzko-Zajko WJ. Impact of older adults’ reading ability on the comprehension and recall of cholesterol information. J Health Educ (USA) 1997;28:21–27. [Google Scholar]