Abstract
Background:
Trace elements and specially minerals are critical for the development of fetus. Many minerals are transferred to the fetus for fetal stores in the latter part of the pregnancy. It has been shown that various trace elements such as Zinc, Iron, Calcium and Magnesium are metabolically interrelated and there is alteration in their concentration during pregnancy. Beyond pregnancy is associated with increased demand of all the nutrients and deficiency of any of these could affect pregnancy, delivery and outcome of pregnancy.
Aim:
To study the levels of trace elements namely zinc, iron, magnesium and calcium in maternal and umbilical cord blood and their association with pregnancy outcome.
Methods:
Sixty pregnant women in Zabol, Iran were selected from those who had registered their names for the prenatal care and who had followed up till the 3rd trimester of pregnancy ending in child birth. Biochemical parameters analyzed with help of the biochemical laboratory. Data were analyzed by SPSS software.
Results:
The mean biochemical profile such, serum calcium, magnesium, zinc and iron in the pregnant women were as follow: in the 1st trimester 8.3, 1.9, 74.9 and 74.4 µg/dl respectively; in the 2nd trimester 8.5, 1.9, 73.1 and 79.3 µg/dl, respectively; in the 3rd trimester 8.6, 1.9, 68.4, and 82.2 µg/dl, respectively. In the umbilical cord blood, the mean serum calcium, magnesium, zinc and iron were 8.5, 1.9, 84.1, and 89.8 µg/dl, respectively. The mean serum calcium and magnesium during the three trimesters of pregnancy were not significantly different from that in the umbilical cord blood, while the mean serum zinc and iron in the umbilical cord blood were significantly different (p<0.05) in the three trimester of pregnancy. The mean birth weight of neonates was 3.1 kg and 12% of neonates showed low birth weight. Our findings showed that, except magnesium, the profile of other biochemical variables, namely, calcium, zinc and iron in the umbilical cord blood of the neonates with normal birth weight (NBW) were significantly higher than in the umbilical cord blood of neonates with low birth weight (LBW).
Conclusion:
The results suggest that maternal serum zinc, iron and calcium concentration influenced the birth weight of neonates as outcome of pregnancy, and however, there is need for proper, adequate and balanced micronutrient during pregnancy to affect neonates as healthy outcome.
Keywords: Trace elements, umbilical cord blood, pregnancy outcome
1. INTRODUCTION
Pregnancy is associated with increased demand of all the nutrients. The importance of mineral balance during pregnancy is still, underestimated, though diligent research demonstrates that trace elements and minerals are critical for the development of fetus (1). Many minerals are transferred to the fetus for fetal stores in the latter part of the pregnancy, although they may play important developmental role throughout pregnancy. Magnesium is known to be part of many different enzyme systems and is involved in controlling various metabolic functions. Zinc is a necessary part of hormone systems, and a deficiency of this vital trace element can lead to impaired growth, sexual problems, even diabetes. It has been shown that various trace elements such as Ca, P, Mg, Zn, Cu, iron etc are metabolically interrelated and there is alteration in their concentration during pregnancy. Iron deficiency results in anemia, which may increase the risk of death from hemorrhage during delivery, however its effects on fetal development and birth outcomes still needs further elucidation (2). Pregnancy is also associated with increased demand of all the nutrients and deficiency of any of these could affect pregnancy, delivery and outcome of pregnancy. The main objective of current survey was to study the levels of trace elements namely zinc, iron, magnesium and calcium in maternal and umbilical cord blood and their association with neonates as outcome of pregnancy.
2. MATERIALS & METHODS
Sixty pregnant women were selected based on
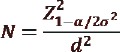
ơ=0.18 (2), CI=95% and d=5%.
Selected pregnant women studied at the clinic of Gynecology and Obstetrics of Imam Ali Hospital in Zabol. They were in age group 20- 35 years with confirmed pregnancy of 15 to 20 days post-conception. All subjects were explained about the purpose of the study and if they agreed to participate, a written consent to participate in the study was obtained from each subject.
Anthropometric measurements of neonates (weight, height, head and chest circumferences) were taken within 24 hours after birth, using standard procedure. Beam balance with an accuracy of 50 g was employed for weighing the infants. Infants were weighed, with minimum clothing, when the child was restful. Infantometers were used for measuring the recumbent length of the newborn infant. A lightweight fibre glass infantometer was used to measure length up to 100 cm. Infants were laid on the board of the infantometer, which was kept on a flat table. The crown of the head was in contact with the top end of the device. The knee was extended so that the feet were at right angles to the leg. The mobile device was then brought in contact with the feet of the neonate and was allowed to be in contact with the device at the bottom end of the board. The distance between the two right angle devices was measured. The reading was recorded in centimeters with accuracy of 0.1 cm. The infant’s head was steadied and the greatest circumference measured, by placing the fibre glass tape firmly round the frontal bones, just superior to the supra-orbital ridges, passing it round the head at the same level, on each side, and laying it over the maximum occipital prominence at the back. The infant’s chest circumference measurement was made at the nipple line, when the child was calm and breathing normally. The fibre glass tape was used for measuring the chest circumference.
Biochemical parameters analyzed with help of the biochemical laboratory. For analysis of Iron, Zinc, Calcium and Magnesium in serum, blood samples were allowed to clot at room temperature and were centrifuged at 3500 rpm for 30 minutes. Serum aliquots were stored at -40ºC until analysis. The serum Iron, Zinc, Calcium and Magnesium were determined by the atomic absorption instrument. A SpectrAA-40 atomic absorption spectrometer, PSC-56 programmable sample changer, Epson LX-80 printer, and Zn, Fe, Ca, Mg, hollow cathode lamps from Varian were used in the procedure. Umbilical cord blood was collected and the serum minerals listed above were analyzed.
Data were analyzed by SPSS Version 16. Mean along with Standard Deviation (Mean± SD) and percentages were calculated where ever necessary and suitable tables and graphs were prepared. The statistical differences among the groups were analyzed by Student’s t-test, and one-way ANOVA followed by post hoc test.
3. RESULTS
The profile of selected biochemical parameters, namely, calcium, magnesium zinc and iron in the serum of the pregnant women during the three trimesters of pregnancy is given in Table 1. Our finding showed mean biochemical profile such, serum calcium, magnesium, zinc and iron in the pregnant women were as follow: in the 1st trimester 8.3, 1.9, 74.9 and 74.4 µg/dl, respectively; in the 2nd trimester 8.5, 1.9, 73.1 and 79.3 µg/dl, respectively; in the 3rd trimester 8.6, 1.9, 68.4, and 82.2 µg/dl, respectively. Our findings showed that there was observable significant difference at 5% level as shown by one way ANOVA post hoc Bonferroni test during the three trimesters of pregnancy in zinc and iron concentration during pregnancy periods (Table 1).
Table 1.
Serum Iron Calcium, Zinc and Magnesium, during the Three Trimesters (n=60). *Significant at 5 percent level; NS: Not Significant. Note: Different superscripts in the same rows indicate significant difference at 5% level as shown by post hoc Bonferroni test §Reference value in non-pregnant women
The mean serum calcium during the three trimesters of pregnancy is presented in Table 1. A comparison between the mean serum calcium during the three trimesters of pregnancy in the current study with the study conducted by Kinght et al. (3) showed that the mean calcium in the 1st, 2nd and the 3rd trimesters of pregnancy was lower than the findings of Kinght et al. (3). The findings of the current study and of Kinght et al. (3) showed a decline in the maternal serum calcium in the 2nd trimester of pregnancy. In a study that was conducted by Sachdeva and Mann (4) on sixty-six young women from India, the subjects were divided into two groups called Experimental (E group) which received Folifer and calcium tablets from the second trimester of pregnancy till delivery along with regular medical supervision and nutrition education about additional nutrient needs, and Control groups (C group). Their findings showed that the mean serum calcium in 1st trimester of pregnancy in E group and C group was the same as mean calcium in the 1st trimester of the current study. The mean serum calcium in the 3rd trimester of pregnancy in E group and C group was slightly higher than in the current study and this may be related to the intake of folifer and calcium as supplement nutrients. The mean serum calcium in normal pregnant women that was reported by Punthumapol and Kittichotpanich (5) from Thailand was the same as seen in the current study. The measurements of serum magnesium during the three trimesters of pregnancy showed a decrease in serum magnesium during the 2nd trimester of pregnancy but the mean serum magnesium during the 1st and 3rd trimester were the same (1.9 mg/dl). In a study that was carried out by Pathak et al., (6) among 283 pregnant women in a rural block of Haryana India, the findings showed that the mean serum magnesium was similar to the current findings, while the mean serum magnesium in normal pregnant women that was reported by Punthumapol and Kittichotpanich (5) from Thailand was higher than was found in the current study. The total amount of zinc retained during pregnancy has been estimated to be 1.5 mmol (100 mg) (7). During the third trimester, the physiological requirement of zinc is approximately twice as high as that in women who are not pregnant (8). In a study conducted in Zahedan city by Salimi et al., (9), during 1st, 2nd, and 3rd trimester of pregnancy 61%, 57%, and 41%, respectively had their serum zinc less than 70 µg/dl. A comparison between the mean serum zinc during the three trimesters of pregnancy in the current study with Knight et al. (3) findings showed that the mean serum zinc in Knight et al. (3) findings was higher than in the current findings. The mean serum zinc during 1st and 3rd trimester of pregnancy in Sachdeva and Mann (4) findings in E group and C group was similar to our findings. A comparison of the mean serum iron during 1st, 2nd and 3rd trimesters showed there was an observable significant difference at 5% level as shown by post hoc Bonforoni with the iron serum of selected subjects during the three trimesters of pregnancy (Table 1). A comparison of the mean serum iron in the current research with the findings of Upadhyaya et al. (2) showed that the mean serum iron was slightly lower than the mean serum iron in non-anaemic pregnant women and higher than the anaemic pregnant women. In Emamghorashi and Heidari (10) findings, the mean serum iron was higher than in the current findings. The mean serum iron in E group and C group that was reported by Sachdeva and Mann (4) in the 1st trimester of pregnancy was lower than in the current study. A similar finding was observed in the mean serum iron of E group and C group vs. findings in the current study.
The results of the present study indicate an increase in the mean serum iron during the pregnancy period; it may be related to the intake of routine supplementation of iron by pregnant women. Interestingly serum zinc levels were significantly (p<0.05) reduced during the pregnancy period. There was no significant difference in the mean serum calcium and magnesium during the three trimesters.
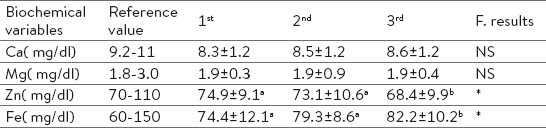
Our findings in the umbilical cord blood, the mean serum calcium, magnesium, zinc and iron were 8.6, 1.9, 84.1, and 89.8µg/dl, respectively. The mean serum calcium and magnesium during the three trimesters of pregnancy were not significantly different from that in the umbilical cord blood, while the mean serum zinc and iron in the umbilical cord blood were significantly different (p<0.05) in the three trimester of pregnancy. As its clear in the Table 1, the mean of serum calcium and magnesium during the three trimesters of pregnancy were not significantly different during pregnancy periods, while the mean serum zinc during pregnancy period showed a significant decrease (p<0.05) during pregnancy periods and an increase observed in the mean of iron of serum. A comparison between the findings about the mean calcium, zinc and iron in cord blood in Sachdeva and Mann (4) report showed that the mean calcium, zinc and iron in the cord blood of E group and C group was higher than that of the current study. A comparison between the mean iron and zinc in the cord blood in the current study (Table 2) with the cord blood in non-anaemic group in Upadhyaya et al. (2) showed that the mean iron and zinc in cord blood of non-anaemic group (normal group) was higher than the findings in the current study. While a comparison of the mean iron in the cord blood in the current study with the anaemic group in Upadhyaya et al. (2) showed that the findings were lower than the findings in the current study Zhou et al. (11), from China; Hess et al. (12), from Switzerland; Okafor et al., (13) from Nigeria; Muslimatun et al. (14) from Indonesia; de-Jong et al. (15) from Philippine; Baron et al. (16) from Spain; Chang et al., (17) from USA reported different percentages of anaemia during pregnancy. The findings of the current research showed (Table 2) mean serum iron in the cord blood was higher than in the pregnant women, which indicate selective uptake of iron by foetus (18). Serum zinc level followed similar trend as iron; cord blood had significantly higher levels of zinc as compared to that in pregnant women. Zinc is passively transferred from mother to foetus across the placenta (2, 19) resulting in an increased level of zinc in cord blood. Zinc is essential for proper growth of foetus and the fall in zinc during pregnancy could also be a physiological response to expanded maternal blood volume (7, 20). Our finding indicated that, mean of serum calcium and magnesium in the serum cord blood and in the serum of pregnant women was similar.
Table 2.
Comparison between Biochemical Parameters in Serum Blood of Pregnant Women and Cord Blood of Neonates (n=60). *Significant at 5% level; NS: Not Significant
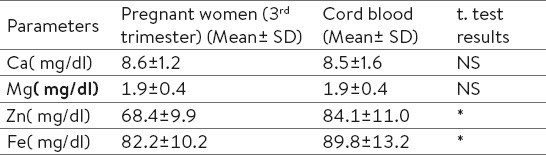
The mean birth weight of neonates was 3.0 kg and 13.5% of neonates showed low birth weight (Table 3). Anthropometric measurements of the neonates, namely, weight, height, head and chest circumferences showed a mean of 3.1 kg, 50.2 cm, 33.3 cm, 32.6 cm respectively (Table 3). A comparison between anthropometric measurements of neonates according to their gender showed a difference between male and female neonates. As it is revealed in Table the male neonates were heavier and taller and their head and chest circumferences were higher than females (Table 3).
Table 3.
Anthropometric Measurements of Neonates (n=60) *Significant at 5% level; NS: Not Significant
Our findings showed that, except magnesium, the profile of other biochemical variables, namely, calcium, zinc and iron in the cord blood of the neonates with normal birth weight (NBW) were significantly higher than in the cord blood of neonates with low birth weight (LBW) (Table 4).
Table 4.
Comparison between Biochemical Parameters in Cord Blood of LBW and NBW Neonates (n=60). *Significant at 5% level; NS: Not Significant
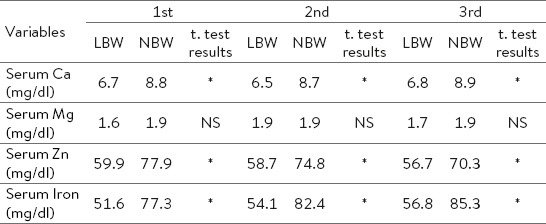
Table 4.
Comparison between Biochemical Parameters in Cord Blood of LBW and NBW Neonates (n=60). *Significant at 5% level; NS: Not Significant
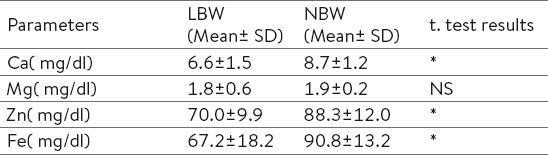
Analysis of data to find out the relationship between the cord blood analysis and the birth weight of neonates was examined. As shown in the Table 4, the LBW babies had significantly lower calcium, zinc and iron level than the NBW babies.
4. CONCLUSION
The results suggest that maternal serum zinc, iron and calcium concentration influenced the birth weight of neonates as outcome of pregnancy, and however, there is need for proper, adequate and balanced micronutrient during pregnancy to affect neonates as healthy outcome.
Footnotes
• Author’s contribution: all authors contributed equally in the preparation of the manuscript.
• Conflict of interest: none declared.
REFERENCES
- 1.Baig S, Hasnain N, Ud-din Q. Studies on Zn, Cu, Mg, Ca and Phosphorous in maternal and cord blood. JPMA. 2003;53(9):417–9. [PubMed] [Google Scholar]
- 2.Upadhyaya C, Mishra S, Ajmera P, Sharma P. Serum iron, and zinc status in Mtaternal and cord blood. Ind J Clin Bio. 2004;19(2):48–52. doi: 10.1007/BF02894257. doi: 10.1007/BF02894257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knight E, Spurlock B, Edward C, Johnson A, Oyemade U, Cole O, et al. Biochemical profile of African American during three trimesters of pregnancy and delivery. J Nutr. 1994;124:943S–53S. doi: 10.1093/jn/124.suppl_6.943S. [DOI] [PubMed] [Google Scholar]
- 4.Sachdeva R, Mann S. Impact of nutrition counseling and supplements on the mineral nutriture of rural pregnant women and their neonates. Indian J Pediatr. 1994;31:643–9. [PubMed] [Google Scholar]
- 5.Punthumapol C, Kittichotpanich B. Serum calcium, magnesium and uric acid in Preeclampsia and normal pregnancy. J Med Assoc Thai. 2008;91(7):968–73. [PubMed] [Google Scholar]
- 6.Pathak P, Kapil U, Kapoor S, Dwivedi S, Singh R. Magnitude of zinc deficiency among nulliparous nonpregnant women in a rural community of Haryana State, India. Food Nutr Bull. 2003;24:368–71. doi: 10.1177/156482650302400407. PMID: 15572822. [DOI] [PubMed] [Google Scholar]
- 7.Swanson C, King J. Reduced serum zinc concentration during pregnancy. Obstet Gynecol. 1983:313–6. doi: 10.1097/00006250-198309000-00010. PMID: 6192374. [DOI] [PubMed] [Google Scholar]
- 8.WHO. Trace elements in human nutrition and health. Geneva: World Health Organization; 1996. World Health Organization. Geneva 1996. [Google Scholar]
- 9.Salimi S, Yaghmaei M, Joshghani H, Mansourian A. Study of zinc deficiency in pregnant women. Iranian J Publ Health. 2004;33(3):15–8. [Google Scholar]
- 10.Emamghorashi F, Heidari T. Iron status of babies born to iron - deficient anaemic mothers in an Iranian hospital. East Mediter Health J. 2004;10(6):808–14. [PubMed] [Google Scholar]
- 11.Zhou L, Yang W, Hua J, Deng C, Tao X, Stoltzfus R. Relation of hemoglobin measured at different times in pregnancy to pre term birth and low birth weight in Shanghai, China. Am J Epidemiol. 1998;148:998–1006. doi: 10.1093/oxfordjournals.aje.a009577. [DOI] [PubMed] [Google Scholar]
- 12.Hess S, Zimmermann M, Brogli S, Hurrell R. A national survey of iron and folate status in pregnant women in Switzerland. Int J Vit Nutr Res. 2001;71(5):269–73. doi: 10.1024/0300-9831.71.5.268. [DOI] [PubMed] [Google Scholar]
- 13.Okafor J, Oloyo R, Addo A. A study of iron status of pregnant women in Yewa south local government area of Ogun State. Ind J Nutr Dietet. 2001;38:394–402. [Google Scholar]
- 14.Muslimatun S, Schmidt M, Schultink W, West C, Hautvast J, Muhilal R. Weekly supplementation with iron and vitamin A during pregnancy increases haemoglobin concentration but decrease serum ferritin concentration in Indonesian pregnant women. J Nutr. 2001;131(1):85–90. doi: 10.1093/jn/131.1.85. [DOI] [PubMed] [Google Scholar]
- 15.de-Jong N, Aurora B, Romano A, RS RG. Zinc and iron status during pregnancy of Filipino women. Asia Paci J Clin Nutr. 2002;11(3):186–97. doi: 10.1046/j.1440-6047.2002.00289.x. [DOI] [PubMed] [Google Scholar]
- 16.Baron M, Solano L, Liovera D, Pena E. Vitamin A status in pregnant adolescent of low socioeconomic income. Arch Latinoam Nutr. 2003;53(4):364–8. [PubMed] [Google Scholar]
- 17.Chang S, O’Brien K, Nathanson M, Mancini J, FR FW. Haemoglobin concentrations influence birth outcomes in pregnant African - American adolescents. J Nutr. 2003;70(4):299–301. doi: 10.1093/jn/133.7.2348. [DOI] [PubMed] [Google Scholar]
- 18.Balai K, Pendse V, Gupta R, Gupta S. Effect of maternal anemia on iron status of the newborn. Indian J Matern Child Health. 1992;3(2):54–6. [PubMed] [Google Scholar]
- 19.Henkin I, Marshall J, Meret S. Materno fetal metabolism of copper and zinc at term. Am J Obstet Gynecol. 1971;110:131–4. doi: 10.1016/0002-9378(71)90234-1. [DOI] [PubMed] [Google Scholar]
- 20.Bro S, Berendtsen H, Norgaard J, Host A, Jorgensen P. Serum zinc and copper concentration in maternal and umbilical cord blood: Relation to course and outcome of pregnancy. Scand J Clin Lab Invest. 1998;48:805–11. doi: 10.3109/00365518809088764. [DOI] [PubMed] [Google Scholar]


