Abstract
Background:
We wanted to systematically review the available evidence to evaluate the drug adherence in elderly with polypharmacy living at home.
Methods:
We performed a literature search using MEDLINE, ISI Web of Science, ProQuest, EMBASE, SCOPUS, Springer Link, Sage Journals and CINAHL. We used the following terms: Medication Adherence, Medication Compliance, Polypharmacy, and Elderly. The search was limited to English-language articles. We included only clinical trials, systematic reviews, meta-analysis and cross-sectional studies.
Results:
A total of seven articles were included in this systematic review after applying the search strategy. Six studies dealt with the prevalence of medication adherence and its correlates in patients aged 65 years or more with polypharmacy. Two studies dealt with the effect of various interventions on medication adherence in patients aged 65 years or more with polypharmacy.
Conclusion:
The available literature on the polypharmacy and drug adherence in elderly living at home is scarce and further studies are needed.
Keywords: Polypharmacy, Medication Adherence, Aged, Systematic Review
1. INTRODUCTION
According to Eurostat, the number of people aged 65 years or more in the EU is expected to grow from around 84 million in 2008 to around 141 million by 2050 and they will account for 28.7% of the EU-28’s population by 2080, compared with 18.5% in 2014 (1). Primary care is the usually entry point into the health care system for all patients health problems and needs. The most important chronic diseases of the elderly population are cardiovascular diseases, mental health problems, cancer, diabetes mellitus, musculoskeletal system diseases and injuries (2). The WONCA definition of family medicine put forward competencies of family medicine which suggest managing patients also from a psychological, social, cultural and existential perspective (3). This means that chronic patients and not diseases should be managed at the primary health care level. Here, also polypharmacy should be taken into account and such patients should be managed according to family medicine competencies (4). Polypharmacy increasingly is a problem in the health care of polymorbid and elderly people, and affects morbidity and mortality. However, when addressing polypharmacy, we should take into account that several chronic conditions frequently require more than one drug in order to be adequately treated (i.e. ‘rational polypharmacy’ resulting from treatment via different mechanisms). Nevertheless, it has been shown that polypharmacy positively correlates with an increased risk for adverse drug reactions (ADRs), as well as drug-drug and drug-disease interactions (5). On the other hand, polypharmacy can increase the risk for medication non-adherence, which consecutively can cause suboptimal therapeutic effectiveness and poor clinical response.
A consequence of several chronic clinical conditions is not only that the older adults tend to use multiple drugs, but as well their long term use. It has been found in the literature that the number of drugs taken among older patients is up to six prescribed medications and up to three non-prescribed medications (2). Medication-taking behavior is extremely complex and individual, requiring numerous multifactorial strategies to improve adherence. Most of the research has resulted in the development of medications with proven efficacy and positive benefit-to-risk profiles with great focus on outcomes. However, it seems to be forgotten that medication adherence lies between the former and the latter (6).
The World Health Organization (WHO) defined medication adherence as the extent to which a person´s behavior - taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider (7). This definition highlights the importance of an active involvement of the patient with the health professionals with a good communication (8).
According to WHO definition, the non-adherence describes the patient who does not or only partially follow the treatment arrangements previously agreed with the doctor (7). Medication adherence (the patients’ use of the right drug in the correct dose at the right interval), which is a key factor associated with the effectiveness of all pharmacological therapies is essential in the treatment of the elderly. Medication taking behavior is complex and involves patient, physician, and process components. Increasing adherence may have a bigger effect on health than improvement in specific medical therapy. Identification of non-adherence is challenging and requires specific skills (6). If not recognized, the non-adherence can lead to a dose augmentation of the initial medication or the addition of a second drug, thereby increasing the risk for ADRs (6), increased emergency visits, hospitalizations, lower quality of life and increased health care costs. Of all medication-related hospitalizations that occur in the United States of America, between one third and two thirds are the results of poor medication adherence (9).
The aim of our systematic review was to analyses the published literature on the polypharmacy and drug adherence in elderly living at home.
2. METHOD
We performed a literature search using MEDLINE (1966-2014), ISI Web of Science (1970-2014), ProQuest (1980-2014), EMBASE (1980-2014), SCOPUS (1960-2014), Springer Link (1980-2014), Sage Journals (1980-2014) and CINAHL (1982-2014). We used the following terms: Medication Adherence, Medication Compliance, Polypharmacy, and Elderly. The search was limited to English-language articles. We included only clinical trials, systematic reviews, meta-analysis and cross-sectional studies. Bibliographies of published reviews were also screened for potentially relevant studies.
The inclusion criteria for articles to be included in this review were patients aged 65 years old or older and patients living at home. The exclusion criteria were community dwelling patients, hospital patients, patients with severe disabilities and patients with cognitive impairment.
Search strategy consisted of five steps. In the first step, we performed a search in the databases according to search terms. In the second step, we reviewed the titles and excluded those appearing not to correspond to our search terms. In the third step, we removed the duplicates. The abstracts of the remaining articles were reviewed in the fourth step. The abstracts that did not meet the inclusion criteria were excluded. We also excluded the articles according to the exclusion criteria. In the fifth step, we reviewed the full text of the remaining articles and excluded those that again did not correspond to the type of the study eligible for our review, inclusion and exclusion criteria (Figure 1).
Figure 1.
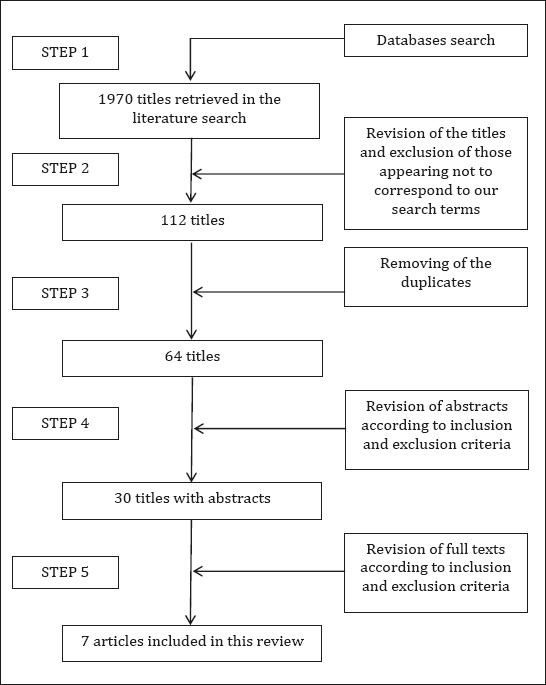
Flow-Chart Summary of Literature Search
3. RESULTS
A total of seven articles were included in this review after applying the search strategy (Figure 1). Six studies dealt with the prevalence of medication adherence and its correlates in patients aged 65 years or more with polypharmacy. Two studies dealt with the effect of various interventions on medication adherence in patients aged 65 years or more with polypharmacy (Table 1).
Table 1.
Summary of studies’ characteristics and their main results
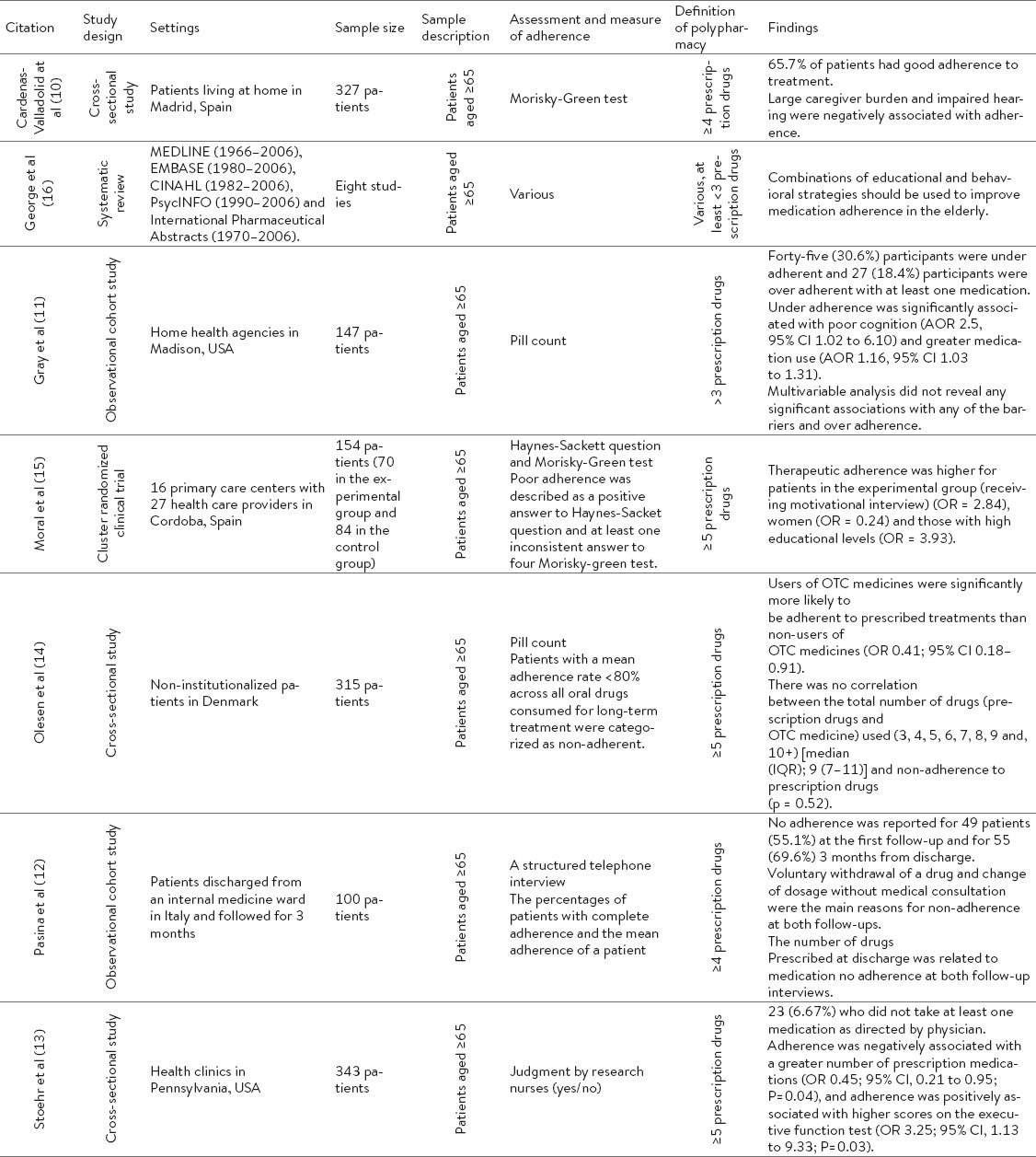
3.1 Prevalence of medication adherence and its correlates
The prevalence of non-adherence in elderly patients receiving polypharmacy ranged from 6 to 55% (10-13). Medication adherence was negatively associated with large caregiver burden (10), impaired hearing (10), poor cognition (11), and greater number of drugs (11-13). The adherence was positively associated with the use of over-the-counter drugs (14), in patients with higher educational level (15), in women (15), and with higher scores on the executive function test (13).
3.2 The effect of various interventions on medication adherence
A systematic review of intervention to improve medication adherence (16) revealed several problems regarding the inconsistent methodology and findings in the studies included in the review. There was not enough evidence to justify the use of different single interventions for enhancing medication adherence in the elderly receiving polypharmacy. The authors suggested that until form evidence is available, combinations of educational and behavioral strategies should be used to improve medication adherence.
Moral et al (15) studied the effect of a face-to-face motivational interviewing in improving medication adherence in elderly receiving polypharmacy. They concluded that a face-to-face motivational approach in primary care helps elderly patients who are being treated by polypharmacy to achieve an improved level of treatment adherence than traditional strategies of providing information and advice.
4. DISCUSSION
Despite the fact that medication adherence is a crucial part in the management of patients with chronic diseases the theme about adherence in elderly living at home is a research topic that is not often presented in available scientific literature. With our systematic review, we could detect only seven articles that matched our inclusion criteria which indicate that this topic is currently not well studied. Our results also showed that this topic is difficult to study as several studies had problems regarding the inconsistent definitions of terms used in that seven article. Most problems were with tools for the assessment of adherence as different studies used different tools such as questionnaires, tests, pill count or judgment by research nurse (10, 13-15). The same variability was in defining polypharmacy, where the researchers used different definitions, for example 3 or more to 5 or more drugs per day by the patients (11, 14). Like the assessment of adherence and polypharmacy definition, the findings in the included research papers were quite spread. They dealt with various topics about polypharmacy and adherence in elderly patients covering mainly the prevalence of medication adherence, its correlates and the effect of various interventions in medication adherence.
The results of the previous studies included in this systematic review reported that the problem of polypharmacy and medication adherence in elderly living at home was common with the prevalence up to 55%. This was somehow expected as chronic diseases and diseases symptoms are common in such populations (17-19). Patients with several chronic diseases can quickly become patients with polypharmacy and problems with medication adherence. Often, the drug which is good for one disease is not good for the other. Usually, the randomized controlled trials for drugs are done on ideal patients with only one disease and no polypharmacy. Hence, the guidelines developed in the basis of such studies do not apply in elderly multimorbid patients. This indicates the need for more studies in such populations. Medication adherence was found to be associated with various patients’ characteristics such as demographic (15), functional (10) and health (11-14). Special emphasis should be given on these subgroups of patients when dealing with medication adherence.
Despite the enormous complexities involved in medical adherence, research on improving adherence has been challenging and generally focused on single disease states. A Cochrane review of 78 randomized trials found no one simple intervention and relatively few complex ones to be effective at improving long term medication adherence and health outcomes, 69 underscoring the difficulty on improving medical adherence (6). For improving medication adherence one of the studies suggested a combination of educational and behavioral strategies (16) and one praised the positive outcome in the patient group receiving motivational interview (15). But overall evidence for the effects of various methods for improving medication adherence is scarce and inconsistent. Through systematic review of the present literature in eight large data sources from 1966 to 2015, we found 1970 titles which corresponded to at least one including key word. This is the strength of our approach to the topic. There are some articles we didn’t include in our study because they were not available online (e.g. master’s or doctoral theses) and others in languages other than English which could present a limitation of our systematic review.
5. CONCLUSION
There is a continuous and growing trend of population aging, growing cost of health care and increasing reports of adverse drug reactions by multimorbid elderly. Therefore, we need innovative approach for effective managing of the new problems in medicine. This approach should be based on the overview of the present situation in the field of polypharmacy and drug adherence in elderly living at home which is scarce and further studies are needed. This is especially important for family physicians that mostly take care for elderly living at home and need appropriate guidelines and evidence.
Acknowledgements
This study was partially supported by a project grant from National Research Agency L3 6805.
Footnotes
• Author’s contribution: Erika Zelko (orcid.org/000-0002-2730-9118): substantial contribution to conception and design, drafting the article, substantial contribution to analysis and interpretation of data. Zalika Klemenc-Ketis: substantial contribution to conception and design, substantial contribution to acquisition of data, substantial contribution to analysis and interpretation of data, critically revising the article for important intellectual content. Ksenija Tusek-Bunc: substantial contribution to conception and design, substantial contribution to analysis and interpretation of data, critically revising the article for important intellectual content.
REFERENCES
- 1.EUROSTAT. Population data - EUROSTAT. 2015. [cited 2015 July 25]. Available from: http://ec.europa.eu/eurostat .
- 2.Stewart RB, Cooper JW. Polypharmacy in the aged. Practical solutions. Drugs Aging. 1994;4(6):449–61. doi: 10.2165/00002512-199404060-00002. [DOI] [PubMed] [Google Scholar]
- 3.Allen J, Gay B, Crebolder H, Heyrman J, Svab I, Ram P. The European definition of general practice/family medicine. In: Evans P, editor. Wonca Europe; 2011. [Google Scholar]
- 4.Allen J, Gay B, Crebolder H, Heyrman J, Svab I, Ram P. The European definitions of the key features of the discipline of general practice: the role of the GP and core competencies. Br J Gen Pract. 2002;52(479):526–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Hajjar ER, Cafiero AC, Hanlon JT. Polypharmacy in elderly patients. Am J Geriatr Pharmacother. 2007;5(4):345–51. doi: 10.1016/j.amjopharm.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 6.Brown MT, Bussell JK. Medication adherence: WHO cares? Mayo Clin Proc. 2011;86(4):304–14. doi: 10.4065/mcp.2010.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sabate E, editor. Adherence to Long-term Therapies: Evidence for Action. Geneva: WHO; 2003. [PubMed] [Google Scholar]
- 8.Cutler DM, Everett W. Thinking outside the pillbox - medication adherence as a priority for health care reform. N Engl J Med. 2010;362(17):1553–5. doi: 10.1056/NEJMp1002305. [DOI] [PubMed] [Google Scholar]
- 9.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 10.Cardenas-Valladolid J, Martin-Madrazo C, Salinero-Fort MA, Carrillo de-Santa Pau E, Abanades-Herranz JC, de Burgos-Lunar C. Prevalence of adherence to treatment in homebound elderly people in primary health care: a descriptive, cross-sectional, multicentre study. Drugs Aging. 2010;27(8):641–51. doi: 10.2165/11537320-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 11.Gray SL, Mahoney JE, Blough DK. Medication adherence in elderly patients receiving home health services following hospital discharge. Ann Pharmacother. 2001;35(5):539–45. doi: 10.1345/aph.10295. [DOI] [PubMed] [Google Scholar]
- 12.Pasina L, Brucato AL, Falcone C, Cucchi E, Bresciani A, Sottocorno M, et al. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging. 2014;31(4):283–9. doi: 10.1007/s40266-014-0163-7. [DOI] [PubMed] [Google Scholar]
- 13.Stoehr GP, Lu SY, Lavery L, Bilt JV, Saxton JA, Chang CC, et al. Factors associated with adherence to medication regimens in older primary care patients: the Steel Valley Seniors Survey. Am J Geriatr Pharmacother. 2008;6(5):255–63. doi: 10.1016/j.amjopharm.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Olesen C, Harbig P, Barat I, Damsgaard EM. Generic substitution does not seem to affect adherence negatively in elderly polypharmacy patients. Pharmacoepidemiol Drug Saf. 2013;22(10):1093–8. doi: 10.1002/pds.3497. [DOI] [PubMed] [Google Scholar]
- 15.Moral RR, Torres LA, Ortega LP, Larumbe MC, Villalobos AR, Garcia JA, et al. Effectiveness of motivational interviewing to improve therapeutic adherence in patients over 65 years old with chronic diseases: A cluster randomized clinical trial in primary care. Patient Educ Couns. 2015;98(8):977–83. doi: 10.1016/j.pec.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 16.George J, Elliott RA, Stewart DC. A systematic review of interventions to improve medication taking in elderly patients prescribed multiple medications. Drugs Aging. 2008;25(4):307–24. doi: 10.2165/00002512-200825040-00004. [DOI] [PubMed] [Google Scholar]
- 17.Softic N, Smogavec M, Klemenc-Ketis Z, Kersnik J. Prevalence of chronic diseases among adult Slovene population. Zdrav Var. 2011;50:185–90. [Google Scholar]
- 18.Pivec N, Serdinsek T, Klemenc-Ketis Z, Kersnik J. Prevalence of disease symptoms in slovenian adult population and factors associated with their prevalence. Zdrav Var. 2014;53:262–9. [Google Scholar]
- 19.Poplas-Susic T, Svab I, Kersnik J. The project of model practices in family medicine in Slovenia. Zdrav Vestn. 2013;82(10):635–47. [Google Scholar]


