Abstract
OBJECTIVE
The purpose of the current study was to examine the indirect effect of youth screen time (e.g., television, computers, smartphones, video games, and tablets) on behavioral health problems (i.e., internalizing, externalizing, and peer problems) through sleep duration and disturbances.
METHODS
We assessed a community sample of parents with a child in one of three developmental stages: young childhood (3 – 7 yrs.; N = 209), middle childhood (8 – 12 yrs.; N = 202), and adolescence (13 – 17 yrs.; N = 210). Path analysis was employed to test the hypothesized indirect effect model.
RESULTS
Findings indicated that, regardless of the developmental stage of the youth, higher levels of youth screen time were associated with more sleep disturbances, which, in turn, were linked to higher levels of youth behavioral health problems.
CONCLUSION
Children who have increased screen time are more likely to have poor sleep quality and problem behaviors.
Keywords: screen time, sleep disturbances, sleep duration, behavioral health problems
Introduction
The explosion of digital technology ownership in the last five years1,2 has created a dramatic shift in how youth and families use technology3,4. Further, the increased access to new digital media (e.g., smartphones and tablets) devices has contributed to a rapid rise in average screen time exposure for children4,5. Total daily screen time across devices in children 8- to 18-years old has risen from five to approximately eight hours since 19996, far exceeding the American Academy of Pediatric’s (AAP) recommendation of two hours or less7.
Excessive screen time in childhood is associated with behavioral health problems8–10. However, the process by which screen time increases these problems has not been elucidated. One potential mechanism of this association is youth sleep quality: There are established individual associations between youth screen time and compromised sleep duration and quality11–13 as well as between sleep and a variety of childhood behavioral health outcomes (e.g., internalizing, externalizing, & peer problems)14–16. The mechanisms by which higher levels of screen time cause sleep disturbances have been attributed to environmental, psychosocial, and biological causes.11–13 One of these environmental sources is the use of screen-based activities, which often delays bedtime or truncates total sleep time11. One psychosocial source may be arousal due to the content of the media, interfering with the ability to fall and stay asleep17. And finally, one potential biological mechanism is the effect of screen light on both circadian rhythm and alertness.
Though initial support is promising, only two studies have examined sleep as a link between screen time and youth behavioral health with both finding some support for sleep duration serving in this role18,19. Each study had limitations that dampen the generalizability of results and implications for modern families. These include: Failure to examine sleep quality, which may be a more important marker of sleep than is duration14,20–23; limited assessment of screen time (e.g., during the school day); absence of modern media devices (e.g., tablets, smartphones); limited assessment of behavioral health problems; and narrow age ranges (e.g., middle school children), precluding the examination of differences over the course of child development14.
The purpose of the current study was to address the limitations noted above and provide updated information and recommendations to families. We (1) examine both sleep duration and sleep disturbances, a proxy for sleep quality24,25; (2) assess screen time after school for all the primary types of devices children use today (e.g., smartphones, tablets, video games, laptops); (3) assess internalizing, externalizing, and peer relationship problems; and (4) use a sample of families with a child in one of three developmental stages: young childhood (3 – 7 yrs.), middle childhood (8 – 12 yrs.), and adolescence (13 – 17 yrs.). These age groups were chosen a priori based typical age divisions of prevention and intervention programs that involve parenting as a primary component (e.g., young children26; middle childhood27; adolescence28) in order to more directly inform the development of programs to help parents manage their children’s screen time at different developmental stages. Of importance, research has long indicated that children have different cognitive skill development and play different roles in the family during these stages of development29. We hypothesized that higher levels of screen time would be indirectly related to higher levels of youth behavioral health problems (i.e., internalizing, externalizing, and peer problems) through lower sleep duration and higher levels of sleep disturbance. We hypothesize that these indirect effects would be significant across the three developmental stages.
Methods
Participants and Recruitment
Parents of 3 to 7 (N = 209), 8 – 12 (N = 202), and 13 – 17 (N = 210) year old children were recruited online through Amazon’s Mechanical Turk (MTurk), the dominant crowdsourcing application in the social sciences. On MTurk, workers browse Human Intelligence Tasks (HITs) by title, keyword, reward, availability, and so on, and complete HITs of interest. Participants are compensated by requesters upon successful completion of tasks (for an introduction to using MTurk30). Participation requirements were being a U.S. resident and having at least a 95% task approval rate on MTurk.
Online data collection about screen time has been used successfully, previously31. Furthermore, there are several advantages for the use of crowdsourcing methods in clinical and developmental research. First, relatively large samples sizes can be collected quickly32 for a minimal cost allowing researchers to address unanswered questions, particularly about mechanisms that statistically require large sample sizes. Second, a diverse range of participants (e.g., race, SES, household composition) can be recruited from across the United States32–34. Third, prior research has convincingly demonstrated that data obtained via crowdsourcing methods are as reliable as those obtained via more traditional data collection methods32,33. Fourth, previous work has also shown that participation and data quality are unaffected by compensation rate or task length35. Fifth, as demonstrated by the current study, crowdsourcing methods afford an opportunity to recruit mothers and fathers, the latter being long underrepresented in clinical research36,37. Sixth, crowdsourcing methods use identification numbers, which protects respondent anonymity and prevent any individual worker from participating in a single HIT more than once.
Procedure
All study procedures were approved by the BLIND Institutional Review Board. Parents were initially consented online and, after completing surveys, compensated $4.00. For families with multiple children in the target age range, one child was randomly selected through a computer algorithm. Ten attention check items, placed throughout the survey, asked participants to enter a specific response that changed throughout the survey and appeared randomly. To ensure that responses were not random or automated, participants (N = 2) were excluded from the study if they had more than one incorrect response.
Measures
Youth weekly screen time
Parents were asked two questions regarding their child’s screen time: “Now thinking about [target child]’s typical activities, on a typical weekday (“weekend” in second question) how much time does [target child] spend doing each of the following at home?” Parents responded with the number of hours and/or minutes their child engaged in each of the following activities: (1) Watching TV or DVDs; (2) using the computer; (3) playing video games on a console game player (such as: Xbox, Playstation, Wii); (4) playing on a handheld game console like a Gameboy, PSP, or DS; (5) using a tablet computer (such as iPad); and (6) using a smart phone for playing games, watching videos, or surfing the Internet (not including time spent talking on the phone). A daily use (averaged across the weekend and weekday) was calculated by device and then summed across all devices. Due to outliers two standard deviations above the mean that were beyond possible daily totals, such values were winsorized and assigned the highest value at two standard deviations. The method employed in the current study to measure child screen time was similar to those used by major industry reports and peer-reviewed research38,39.
Sleep disturbances and duration
An abbreviated version of the Children’s Sleep Habit Questionnaire (CSHQ) was used to measure youth sleep disturbances and duration. The CSHQ is a widely used parent-report questionnaire to screen for childhood sleep problems and has been shown to be highly correlated with objective measures sleep functioning such as actigraphy. Parents rated the frequency of sleep behavior for the most recent “typical” week on a four-point Likert scale, with the response options usually (five to seven times per week), sometimes (two to four times per week), rarely (zero to one time per week), and never (less than once a week). A higher score indicates more sleep disturbances. Seven items were chosen to measure sleep disturbances across several domains: daytime sleepiness (“falls asleep while involved in activities”), daytime fatigue (“seems tired during the day”), sleep efficiency (“wakes up during the night”), continuity of sleep (“is restless and moves a lot during sleep”), consistency of sleep (“sleeps about the same amount each day” and “goes to bed at the same time at night”), and sleep latency (“falls asleep within 20 minutes after going to bed”). Items were scored such that higher scores represented more sleep disturbances (current α = .72). To measure sleep duration, parents reported what time their child typically goes to sleep on weeknights and weekend nights separately, and what time they typically wake up on weekdays and weekend days. From these, the amount of sleep was calculated by multiplying the weekday totals by 5 (days), adding it to the weekend totals multiplied by 2, and dividing the total by 7 to indicate average daily sleep duration.
Youth internalizing and externalizing problems
The parent form of the 19-item Brief Problem Monitor (BPM)40 measured two indices of youth behavioral health problems: internalizing and externalizing problems. BPM items were selected from the Child Behavior Checklist (CBCL) and Youth Self Report (YSR)41 using item response theory and factor analysis42. The internal consistency, test–retest reliability, and validity of the BPM are excellent40,42. Each item is rated on a 0 to 2 scale (0 = not true, 1 = somewhat true, or 2 = very true). Higher scores indicate more internalizing (current α = .72) or externalizing (current α = .72) problems.
Peer problems
For the third indicator of behavioral health problems, the peer problem subscale of the Strengths and Difficulties Questionnaire43 was used. Responses to each of the five peer problem items (e.g., playing alone; being bullied and generally not liked by other children) were rated on a 3-point Likert scale (0 = not true, 1 = somewhat true, or 2 = certainly true). Psychometric properties are well established44–46. Higher scores indicate more peer problems (current α = .72).
Data Analytic Plan
Evaluation of the structural model
Path analysis to test the hypothesized structural model was conducted with Mplus 6.0 software47. Because previous research recommends examining sleep duration and problems separately20,23, models were run individually with sleep disturbances and then sleep duration as the link between screen time and behavioral health problems. The following fit statistics were employed to evaluate model fit: Chi-square (χ2: p > .05 excellent), Comparative Fit Index (CFI; > .90 acceptable, > .95 excellent), Root Mean Square Error of Approximation (RMSEA; < .08 acceptable, < .05 excellent) and the Standardized Root Mean Square Residual (SRMR; < .08 acceptable, < .05 excellent)48,49. As missing data were less than 1% overall for all core variables, full information maximum likelihood estimation techniques were used for inclusion of all available data. The Model Indirect command in Mplus was utilized to calculate a standardized indirect effect parameter and biased-corrected bootstrap confidence intervals. Additionally, the ratio of the indirect effect to the total effect (ab/c)50 for each significant indirect effect test was calculated.
Covariates
Although not included in the proposed conceptual model, the effects youth gender, parent marital status (one parent family vs. two-parent), and family income on the model were examined by running a multiple-indicator/multiple-cause MIMIC51 model in which all major constructs of the final model were regressed on the covariates separately. If paths in the structural model remained significant with the inclusion of these covariates, it was concluded that the control variables did not influence the relations among variables in the model.
Secondary analyses
In order to facilitate recommendations for families on how many hours of youth screen time is disruptive for sleep (i.e., disturbances and duration), one-way analysis of variance (ANOVA) with six levels of screen time (0– 2 hours as recommended by AAP; 2.1 to 4 hours; 4.1 to 6 hours; 6.1 to 8 hours; 8.1 to 10 hours; and 10.1 hours or more) was conducted with sleep disturbances and duration as the dependent variables.
Results
Primary Analyses
Sample demographics by developmental stage (young childhood, middle childhood, and adolescent samples) are presented in Table 1.
Table 1.
Sample demographic characteristics by developmental stage.
| M (S.D.) or Percentage | |||
|---|---|---|---|
| Young Childhood n = 209 |
Middle Childhood n = 202 |
Adolescence n = 210 |
|
| Parent Age | 31.61 (6.57) | 35.39 (6.45) | 41.78 (7.66) |
| Parent (% Mothers) | 59.8% | 58.4% | 62.4% |
| Parent Race | |||
| White | 76.0% | 77.2% | 78.8% |
| Black | 10.6% | 10.4% | 11.1% |
| Latino/a | 5.8% | 6.9% | 5.8% |
| Asian | 6.7% | 4.0% | 3.4% |
| Other | .9% | 1.5% | .9% |
| Parent Marital Status | |||
| Single | 18.4% | 15.4% | 18.8% |
| Married | 58.7% | 68.2% | 66.3% |
| Cohabitating | 22.8% | 16.4% | 14.9% |
| Parent Education | |||
| Did not complete H.S. | 1.0% | 0.0% | 0.0% |
| H.S. or GED | 12.5% | 12.9% | 11.9% |
| Some College | 30.6% | 25.2% | 35.2% |
| College Degree | 42.5% | 41.1% | 39.5% |
| > College Degree | 13.4% | 20.8% | 13.3% |
| Family Income | |||
| Under $30,000 | 20.5% | 19.8% | 24.8% |
| $30,000 – $49,999 | 32.6% | 29.2% | 26.2% |
| $50,000 – $69,999 | 20.1% | 16.8% | 20.0% |
| $70,000 – $99,999 | 14.8% | 18.8% | 16.6 |
| $100,000 or more | 12.0% | 15.4% | 12.4 |
| Family Neighborhood | |||
| Urban | 27.8% | 26.2% | 25.7% |
| Suburban | 51.7% | 52.0% | 51.0% |
| Rural | 20.6% | 21.8% | 23.3% |
| Number of Children | 1.67 (.85) | 2.05 (1.36) | 1.72 (.93) |
| Youth Age | 4.47 (1.34) | 9.46 (1.38) | 14.70 (1.40) |
| Youth Gender (% Girls) | 44.0% | 46.0% | 44.8% |
| Youth Screen Time (hours) | 4.95 (4.1) | 5.50 (4.3) | 8.80 (5.1) |
| 0 – 2 Hours | 16.8% | 8.0% | 0% |
| 2.1 – 4 Hours | 37.0% | 34.0% | 9.3% |
| 4.1 – 6 Hours | 21.6% | 25.5% | 25.0% |
| 6.1 – 8 Hours | 12.0% | 15.0% | 24.5% |
| 8.1 – 10 Hours | 5.9% | 8.0% | 14.2% |
| > 10 Hours | 6.7% | 9.5% | 27.0% |
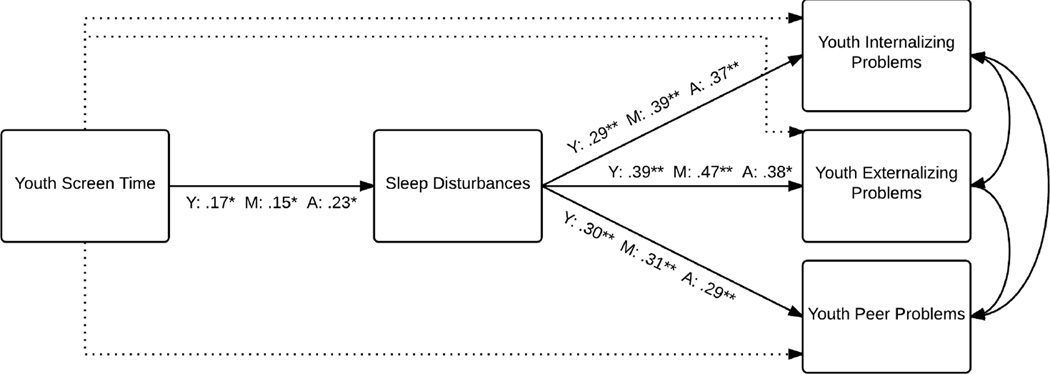
The multiple-group function in Mplus was used to determine model fit across all three developmental stages, but paths in the model were freely estimated by youth developmental stage. When sleep disturbances was included in the model, direct paths from youth screen time to behavioral health problems were non-significant across all developmental stages and thus, these paths were dropped in order to determine model fit. This final model demonstrated excellent fit, χ2 (9, N = 613) = 10.73, p > .15, RMSEA = .03, 95% CI .00 – .088, CFI = 1.0, SRMR = .03, and is displayed by each child developmental stage in Figure 1. The standardized estimates of direct and indirect effects are presented in Table 2 along with bias-corrected bootstrap confidence intervals for all effects for each of the three developmental stages.
Figure 1.
The indirect effect of youth screen time on behavioral health problems through sleep disturbances.
Note: Y = Young Childhood; M = Middle Childhood; A = Adolescence; * = p < .05; ** = p <.01; non-significant paths indicated by dashed line.
Table 2.
Standardized estimates for the final structural model by youth developmental stage.
| Paths in the model | Standardized Estimate [95% CI] | ||
|---|---|---|---|
| Young | Middle | Adolescence | |
| Sleep Disturbances | |||
| Screen Time – Sleep Disturbances | .17 [.04 – .30] | .15 [.02 – .29] | .23 [.10 – .36] |
| Sleep Disturbances – Internalizing Problems | .29 [.16 – .41] | .39 [.28 – .51] | .37 [.25 – .49] |
| Sleep Disturbances – Externalizing Problems | .39 [.27 – .50] | .47 [.37 – .58] | .38 [.26 – .50] |
| Sleep Disturbances – Peer Problems | .30 [.17 – .42] | .31 [.19 – .44] | .29 [.17 – .42] |
| Screen Time IND Internalizing Problems | .05 [.004 – .09] | .06 [.004 – .12] | .08 [.03 – .14] |
| Screen Time IND Externalizing Problems | .07 [.01 – .12] | .07 [.01 – .14] | .09 [.03 – .15] |
| Screen Time IND Peer Problems | .05 [.01 – .09] | .05 [.001 – .10] | .07 [.02 – .12] |
| Internalizing WITH Externalizing | .25 [.12 – .38] | .45 [.34 – .56] | .21 [.08 – .35] |
| Internalizing WITH Peer Problems | .23 [.10 – .35] | .34 [.22 – .47] | .45 [.34 – .56] |
| Externalizing WITH Peer Problems | .03 [−.11 – .16] | .29 [.16 – .41] | .24 [.12 – .37] |
| Sleep Duration | |||
| Screen Time – Sleep Duration | −.29 [−.48 – −.10] | −.53 [−.71 – −.36] | .14 [−.01 – .29] |
| Sleep Duration – Internalizing Problems | −.05 [−.20 – .11] | −.06 [−.21 – .08] | −.01 [−.16 – .14] |
| Sleep Duration – Externalizing Problems | −.10 [−.24 – .04] | −.22 [−.38 – −.06] | −.09 [−.23 – .05] |
| Sleep Duration – Peer Problems | −.06 [−.18 – .06] | −.05 [−.21 – .11] | .15 [−.01 – .31] |
| Internalizing WITH Externalizing | .33 [.17 – .48] | .55 [.43 – .68] | .32 [.18 – .47] |
| Internalizing WITH Peer Problems | .29 [.15 – .43] | .42 [.29 – .55] | .51 [.39 – .64] |
| Externalizing WITH Peer Problems | .13 [−.04 – .30] | .39 [.24 – .53] | .35 [.22 – .47] |
Note: IND = Indirect Effect; CI = Confidence Intervals; CI that do not contain zero can be considered statistically significant
The statistically significant standardized estimates of pathways in the sleep disturbances model (Figure 1) were consistent across all three developmental stages: As predicted, higher levels of youth screen time were associated with higher levels of sleep disturbances which, in turn, were related to higher levels of internalizing, externalizing, and peer problems. Further, the indirect effect of youth screen time on youth internalizing, externalizing, and peer problems through sleep disturbances was significant across all developmental stages (see Table 2). The ratio of the indirect effect to the total effect for youth screen time on problem behaviors for the young, middle, and adolescent children ranged from 33% to 50% for internalizing problems, from 33% to 89% for externalizing problems, and from 44% to 98% for peer problems.
MIMIC models tested the demographic effects of youth gender, parent marital status, and family income on the associations in the model for each age group. All the major constructs of the model were regressed on the control variables separately. All paths in the structural model across all three samples were largely unaffected (i.e., remained significant without large reductions in effect size) by the inclusion of these control variables; thus, it was concluded that the control variables did not influence the original relations among variables in the model.
Next, the model was run with sleep duration in the model instead of disturbances. This model demonstrated excellent fit, χ2 (9, N = 613) = 13.89, p > .10, RMSEA = .05, 95% CI .00 – .10, CFI = .98, SRMR = .04, see Table 2 for standardized estimates and 95% confidence intervals. Youth screen time was related to sleep duration for young and middle childhood, but not for adolescence. Sleep duration was only related to youth externalizing problems in middle childhood; all other paths from sleep duration to behavioral health outcomes were not significant. This model was not considered further (e.g., MIMIC models were not tested).
Secondary analyses
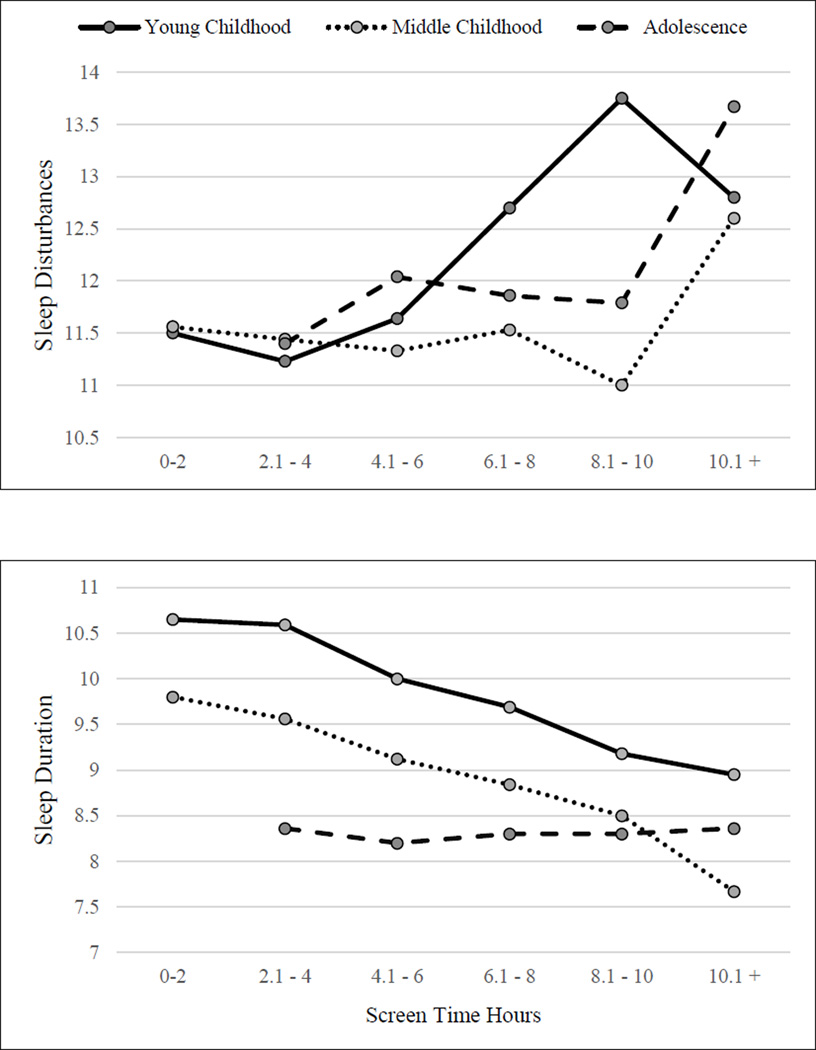
See the bottom of Table 1 for overall mean screen time and percentage of sample in each category. To examine how many hours of screen time is disruptive for sleep, sleep disturbances initially and then duration served as a dependent variable and six levels of youth screen time served as the independent variable in an ANOVA. A significant effect emerged for young childhood (F (5, 203) = 2.43, p < .05) and adolescence (F (4, 199) = 3.74, p < .01), but not for middle childhood (F (5, 194) = .60, p > .10); however, the pattern of means for middle childhood are consistent with the adolescent sample. Contrasts were performed in order examine the significant differences between screen time categories (see Figure 2 for estimated sleep disturbance means by screen time category). For middle childhood and adolescence, though only significant in adolescence (p < .01), 10 plus hours of screen time is associated with higher levels of sleep disturbances than all other levels of screen time. In contrast, for young childhood age, a steep increase in sleep disturbances begins after 6 hours of screen time (p < .05) and increases again after 8 hours (p < .01).
Figure 2.
Estimated means for sleep disturbances and duration by youth screen time.
When sleep duration served as the dependent variable, a significant effect emerged for young childhood (F (5, 202) = 2.8, p < .05) and middle childhood (F (5, 194) = 12.05, p < .001), but not for adolescence (F (4, 199) = .19, p > .10) (see Figure 2 for estimated sleep duration means by screen time category). For the middle childhood sample, sleep duration was not different for 0 – 2 and 2.1 – 4 hours of screen time (p > .15), whereas after 4 hours of screen time, sleep duration decreased significantly with each 2-hour increase in screen time (all p < .05). A similar pattern of effects emerged for the young childhood sample; sleep duration was not different for 0 −2, 2.1 – 4, and 4.1 – 6 (all p > .05) but decreased for each 2-hour increase in screen time afterward (all p < .05).
Discussion
This study examined the indirect effect of youth screen time on behavioral health problems through sleep duration and disturbances. Findings indicated that, regardless of the developmental stage of the youth, higher levels of youth screen time were associated with more sleep disturbances, which, in turn, were linked to higher levels of youth internalizing, externalizing, and peer problems. Contrary to expectation, sleep duration only served to link screen time to behavioral health problems for externalizing problems in middle childhood.
The consistency of findings for sleep disturbances across developmental stages ranging in age from 3 to 17 provides substantial support for the roles of youth screen time and sleep disturbances in youth behavioral health problems. Beyond the significant links in the model, the effect size of the indirect effect from youth screen time to all three types of behavioral health problems through sleep disturbances was substantial at each developmental stage. As most research has focused on young children15, the findings for older children and adolescents are particularly important.
Secondary analyses provided additional data in order to facilitate recommendations for families on how many hours of youth screen time is disruptive for sleep. At all three developmental stages, average screen time is substantially above that recommended by AAP7 but comparable to major industry reports6. For young children, sleep disturbances appear to emerge after 6 hours of daily screen time whereas for middle childhood and adolescence, these disturbances increase only at high levels of daily screen time use (10 hours or more). Sleep duration appears to decrease progressively after 4 or 6 hours of daily screen time for preadolescents. As both duration and quality of sleep are important for children and adolescents25, the findings suggest that for preadolescents screen time above 4 to 6 hours daily is disruptive and for adolescents screen time above 10 hours daily is disruptive. Of importance, the findings are limited to sleep; higher levels of screen time may disrupt functioning in other areas (e.g., academic performance).
As sleep hygiene is important in the treatment of behavioral health difficulties52, the present findings suggest practitioners should assess for youth screen time and, if appropriate, include recommendations to reduce children’s screen time. As the adoption of mobile media devices continues to grow, it will be particularly important to provide parents with effective strategies for managing their child’s screen time (e.g., technology-specific parenting strategies).
There are several limitations of the current study. First, the data are cross-sectional, raising questions about the direction of effects and temporal precedence that are better addressed by longitudinal designs. Second, due to the crowdsourcing methodology, all variables in the model were from a single reporter. As this is a potential issue of shared method variance and parent’s reports of adolescent sleep and internalizing may be biased53, the use of multiple reporters and methods (e.g., actigraphy) on constructs of interest could strengthen confidence of findings in future work. Third, we did not separate out weekend from weekday screen time and sleep. These are important topics for families; however, research has not yet addressed weekday vs. weekend measurement of these constructs. Research designs utilizing daily-diary or ecological momentary assessment methodologies will be well suited to examine the roles weekday vs. weekend assessment play. Fourth, our assessment of youth screen time did not account for overlapping use of multiple devices. Though our average screen time hours were in line with major industry reports6, future research should take into account potential device overlap and examine if simultaneous use of multiple devices further increases risk for behavioral health problems. Furthermore, screen time outside the home (e.g., friend’s home) was not considered in our assessment. Fifth, the current study did not include self-reported medical or behavioral health issues (e.g., ADHD). This is an important potential confounder and future research should include this information as potential covariates. Additionally, our assessment of sleep disturbances and youth problem behavior used measures not yet validated for children under six.
Sixth, the online nature of participant recruiting in the present study precludes the examination of parents who may not use the internet, possibly as a result of their perceptions of technology. Given that approximately 15% of adults in the United States do not use the internet54, it will be important in future research to include these families. Seventh, the present study’s focus on negative effects of screen time precluded the examination of potential positive effects of screen time. For example, the importance of technology for a child’s academic success provides a source of unique tension for parents as they attempt to balance the positive and negative effects of screen time. Future research should incorporate positive effects of screen time, such as academic success, as an additional potential outcome associated with child screen time. Eighth, our measure of sleep disturbances was an abbreviated version of the full CSHQ. Though most items and subscales from this measure were not of interest to the current investigation, further research on the validity of the brief version is needed. Ninth, future research will benefit from utilizing objective methods of assessing sleep duration and quality25.
An additional limitation of the current investigation is the simplification of the process by which high levels of screen time influence sleep and problem behaviors. Though necessary for initial stages of inquiry into this growing topic of research, future research should seek to examine the mechanisms involved for each pathway in the current model and do so with the child’s developmental stage as a central context. For example, it is plausible that the mechanisms by which high levels of screen time is related to sleep disturbance, which in turn is related to behavioral health, would differ depending on the child’s developmental stage. For example, adolescents may engage in screen time rather than sleeping whereas young children may be overstimulated by the games and, therefore, have a more difficult time settling in when it is time to sleep. Further, a developmentally-informed approach to identifying mechanisms of influence will greatly enhance both the breadth and confidence in findings as well as the broad scale generalizability of findings to families and children.
Conclusions
The use of mobile media devices continues to increase in childhood. The current findings suggest that excessive screen time is associated with reduced sleep duration in the preadolescent years and sleep disturbances in three age groups ranging from 3 to 17 years. In turn, sleep disturbances, and to a lesser extent duration, are associated with behavioral health problems. Effective interventions to decrease screen time need to be developed and tested for their effects on these negative outcomes. Once mechanisms have been identified within and across children at different developmental stages, interventions targeting these mechanisms can be designed and implemented. Potential targets for intervention may include psychoeducation for both parent and child regarding the consequences of excessive screen time, as well as targeting screen time indirectly through interventions aimed at improving parental efficacy when managing this behavior.
Acknowledgments
Funding Source: This research was supported by the Child and Adolescent Psychology Training and Research, Inc (CAPTR). The first author is supported by NICHD F31HD082858. The funding organizations had no input into design and conduct of the study, collection, management, analysis, and interpretation of the data, or preparation, review, or approval of the manuscript nor in the decision to submit the manuscript for publication.
Footnotes
Data analysis: The first author has full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Rainie L, Smith A. Tablet and E-reader ownership update. [Accessed March 25, 2015];Pew Res Cent Internet Am Life Proj. 2013 http://www.pewinternet.org/2013/10/18/tablet-and-e-reader-ownership-update/ [Google Scholar]
- 2.Smith A. Smartphone ownership 2013. [Accessed March 25, 2015];Pew Res Cent Internet Am Life Proj. 2013 http://www.pewinternet.org/2013/06/05/smartphone-ownership-2013/ [Google Scholar]
- 3.Madden M, Lenhart A, Duggen M, et al. Teens and Technology 2013. [Accessed March 25, 2015];Pew Res Cent Internet Am Life Proj. 2013 http://www.pewinternet.org/2013/03/13/teens-and-technology-2013/ [Google Scholar]
- 4.Wartella E, Rideout V, Lauricella A, Connell S. Parenting in the Age of Digital Technology. [Accessed March 25, 2015];2013 http://cmhd.northwestern.edu/parenting-in-the-age-of-digital-technology/ [Google Scholar]
- 5.Pea R, Nass C, Meheula L, et al. Media use, face-to-face communication, media multitasking, and social well-being among 8- to 12-year-old girls. Dev Psychol. 2012;48(2):327–336. doi: 10.1037/a0027030. [DOI] [PubMed] [Google Scholar]
- 6.Rideout VJ, Foehr UG, Roberts DF. Generation M2: Media in the Lives of 8- to 18-Year-Olds. Henry J; 2010. [Accessed March 25, 2015]. http://eric.ed.gov/?id=ED527859. [Google Scholar]
- 7.Strasburger VC, Hogan MJ, Mulligan DA, et al. Children, adolescents, and the media. Pediatrics. 2013;132(5):958–961. doi: 10.1542/peds.2013-2656. [DOI] [PubMed] [Google Scholar]
- 8.Anderson CA. An update on the effects of playing violent video games. J Adolesc. 2004;27(1):113–122. doi: 10.1016/j.adolescence.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Kremer P, Elshaug C, Leslie E, et al. Physical activity, leisure-time screen use and depression among children and young adolescents. J Sci Med Sport. 2014;17(2):183–187. doi: 10.1016/j.jsams.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Page AS, Cooper AR, Griew P, et al. Children’s screen viewing is related to psychological difficulties irrespective of physical activity. Pediatrics. 2010 Oct; doi: 10.1542/peds.2010-1154. peds.2010-1154. [DOI] [PubMed] [Google Scholar]
- 11.Cain N, Gradisar M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010;11(8):735–742. doi: 10.1016/j.sleep.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Gradisar M, Short MA. The Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. New York, N.Y: Oxford University Press; 2013. Sleep hygiene and environment: Role of technology; pp. 113–126. [Google Scholar]
- 13.Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Med Rev. (0) doi: 10.1016/j.smrv.2014.07.007. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bagley E, El-Sheikh M. The Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. New York, N.Y: Oxford University Press; 2013. Children’s sleep and internalizing and externalizing symptoms; pp. 381–396. [Google Scholar]
- 15.El-Sheikh M, Sadeh AI. Sleep and development: Introduction to the monograph. Monogr Soc Res Child Dev. 2015;80(1):1–14. doi: 10.1111/mono.12141. [DOI] [PubMed] [Google Scholar]
- 16.Smedje H, Broman JE, Hetta J. Associations between disturbed sleep and behavioural difficulties in 635 children aged six to eight years: a study based on parents’ perceptions. Eur Child Adolesc Psychiatry. 2001;10(1):1–9. doi: 10.1007/s007870170041. [DOI] [PubMed] [Google Scholar]
- 17.Higuchi S, Motohashi Y, Liu Y, Maeda A. Effects of playing a computer game using a bright display on presleep physiological variables, sleep latency, slow wave sleep and REM sleep. J Sleep Res. 2005;14(3):267–273. doi: 10.1111/j.1365-2869.2005.00463.x. [DOI] [PubMed] [Google Scholar]
- 18.Barlett ND, Gentile DA, Barlett CP, et al. Sleep as a mediator of screen time effects on US children’s health outcomes. J Child Media. 2012;6(1):37–50. [Google Scholar]
- 19.Nuutinen T, Roos E, Ray C, et al. Computer use, sleep duration and health symptoms: a cross-sectional study of 15-year olds in three countries. Int J Public Health. 2014;59(4):619–628. doi: 10.1007/s00038-014-0561-y. [DOI] [PubMed] [Google Scholar]
- 20.Dewald JF, Meijer AM, Oort FJ, et al. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med Rev. 2010;14(3):179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Kelly RJ, Marks BT, El-Sheikh M. Longitudinal relations between parent-child conflict and children’s adjustment: the role of children’s sleep. J Abnorm Child Psychol. 2014;42(7):1175–1185. doi: 10.1007/s10802-014-9863-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michels N, Clays E, De Buyzere M, et al. Children’s sleep and autonomic function: Low sleep quality has an impact on heart rate variability. Sleep. 2013;36(12):1939–1946. doi: 10.5665/sleep.3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: Relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997;42(6):583–596. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- 24.Owens JA, Spirito A, McGuinn M. The Children’s Sleep Habits Questionnaire (CSHQ): Psychometric properties of a survey instrument for school-aged children. Sleep. 2000;23(8):1043–1051. [PubMed] [Google Scholar]
- 25.Sadeh A., Iii Sleep assessment methods. Monogr Soc Res Child Dev. 2015;80(1):33–48. doi: 10.1111/mono.12143. [DOI] [PubMed] [Google Scholar]
- 26.McMahon RJ, Forehand RL. Helping the Noncompliant Child: Family-Based Treatment for Oppositional Behavior. 2nd. New York, NY, US: Guilford Press; 2003. [Google Scholar]
- 27.Kazdin AE. Parent Management Training : Treatment for Oppositional, Aggressive, and Antisocial Behavior in Children and Adolescents: Treatment for Oppositional, Aggressive, and Antisocial Behavior in Children and Adolescents. USA: Oxford University Press; 2005. [Google Scholar]
- 28.Patterson GR, Forgatch MS. Parents and Adolescents Living Together: Family Problem Solving. Research Press; 2005. [Google Scholar]
- 29.Forehand R, Wierson M. The role of developmental factors in planning behavioral interventions for children: Disruptive behavior as an example. Behav Ther. 1993;24(1):117–141. [Google Scholar]
- 30.Mason W, Suri S. Conducting behavioral research on Amazon’s Mechanical Turk. Behav Res Methods. 2012;44(1):1–23. doi: 10.3758/s13428-011-0124-6. [DOI] [PubMed] [Google Scholar]
- 31.Nielsen Reports. Reports and Insights | Global Online Consumers and Multi-Screen Media: Today and Tomorrow | Nielsen. [Accessed December 15, 2015];2012 http://www.nielsen.com/us/en/insights/reports/2012/global-online-consumers-and-multi-screen-media-today-and-tomorr.html. [Google Scholar]
- 32.Buhrmester M, Kwang T, Gosling SD. Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspect Psychol Sci. 2011;6(1):3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 33.Casler K, Bickel L, Hackett E. Separate but equal? A comparison of participants and data gathered via Amazon’s MTurk, social media, and face-to-face behavioral testing. Comput Hum Behav. 2013;29(6):2156–2160. [Google Scholar]
- 34.Paolacci G, Chandler J, Ipeirotis P. Running experiments on Amazon Mechanical Turk. Judgm Decis Mak. 2010;5(5):411–419. [Google Scholar]
- 35.Shapiro DN, Chandler J, Mueller PA. Using Mechanical Turk to study clinical populations. Clin Psychol Sci. 2013 Jan; 2167702612469015. [Google Scholar]
- 36.Phares V. Where’s poppa? The relative lack of attention to the role of fathers in child and adolescent psychopathology. Am Psychol. 1992;47(5):656–664. doi: 10.1037//0003-066x.47.5.656. [DOI] [PubMed] [Google Scholar]
- 37.Phares V, Fields S, Kamboukos D, Lopez E. Still looking for Poppa. Am Psychol. 2005;60(7):735–736. doi: 10.1037/0003-066X.60.7.735. [DOI] [PubMed] [Google Scholar]
- 38.Gingold JA, Simon AE, Schoendorf KC. Excess Screen Time in US Children Association With Family Rules and Alternative Activities. Clin Pediatr (Phila) 2014;53(1):41–50. doi: 10.1177/0009922813498152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sanders W, Parent J, Forehand R, et al. The roles of general and technology-specific parenting in managing youth screen time. J Fam Psychol. 2016 doi: 10.1037/fam0000175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Achenbach TM, McConaughy SH, Ivanova MY, et al. Manual for the ASEBA Brief Problem Monitor (BPM) Burlington, VT: ASEBA; 2011. [Google Scholar]
- 41.Achenbach TM, Rescorla L. ASEBA School-Age Forms & Profiles. Aseba Burlington; 2001. [Accessed December 19, 2014]. http://aseba.com/ordering/ASEBA%20Reliability%20and%20Validity-School%20Age.pdf. [Google Scholar]
- 42.Chorpita BF, Reise S, Weisz JR, et al. Evaluation of the Brief Problem Checklist: Child and caregiver interviews to measure clinical progress. J Consult Clin Psychol. 2010;78(4):526–536. doi: 10.1037/a0019602. [DOI] [PubMed] [Google Scholar]
- 43.Goodman R. The Strengths and Difficulties Questionnaire: A research note. J Child Psychol Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- 44.Björnsdotter A, Enebrink P, Ghaderi A. Psychometric properties of online administered parental strengths and difficulties questionnaire (SDQ), and normative data based on combined online and paper-and-pencil administration. Child Adolesc Psychiatry Ment Health. 2013;7:40. doi: 10.1186/1753-2000-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bourdon KH, Goodman R, Rae DS, et al. The strengths and difficulties questionnaire: U.S. normative data and psychometric properties. J Am Acad Child Adolesc Psychiatry. 2005;44(6):557–564. doi: 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- 46.Goodman R, Ford T, Simmons H, et al. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. Br J Psychiatry. 2000;177(6):534–539. doi: 10.1192/bjp.177.6.534. [DOI] [PubMed] [Google Scholar]
- 47.Muthen LK, Muthen BO. Mplus User’s Guide. 6th. Los Angeles, CA: Muthen & Muthen; 2010. [Google Scholar]
- 48.Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociol Methods Res. 1992;21(2):230–258. [Google Scholar]
- 49.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model Multidiscip J. 1999;6(1):1–55. [Google Scholar]
- 50.Preacher KJ, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16(2):93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- 51.Muthén BO. Latent variable modeling in heterogeneous populations. Psychometrika. 1989;54(4):557–585. [Google Scholar]
- 52.Wolfson AR, Montgomery-Downs HE. The Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. Oxford University Press; 2013. [Google Scholar]
- 53.Short MA, Gradisar M, Lack LC, et al. Estimating adolescent sleep patterns: parent reports versus adolescent self-report surveys, sleep diaries, and actigraphy. Nat Sci Sleep. 2013;5:23–26. doi: 10.2147/NSS.S38369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zickuhr K. Tablet Ownership 2013 Tablet Computers. Washington, D.C: 2013. [Google Scholar]