Lean management is an organizational philosophy and accompanying set of tools that originate from a study of business processes employed by the Toyota Motor Company in the 1980s. More recently, a similar approach, termed Lean Healthcare, has been employed by an increasing number of health-care systems (1). The goal of lean in health care is to improve value from the patient's perspective (2). Value stream mapping is a key tool used in lean to help define steps in a process that bring the organization or unit closer to this goal. In the next sections, we will review value stream mapping in the context of lean, provide an example of a value stream map (VSM) for a gastroenterology clinic, and suggest practical steps a practice can take to employ this approach in everyday work.
A VSM is a visual representation of the flow of people, material, and information in a complex system (3,4). By including material and information, the VSM differs from a traditional process flow map; in fact, this method was originally called “Material and Information Flow Mapping” at Toyota (5). The goal of creating such a detailed map is to facilitate a common understanding of this flow, shared by all stakeholders, to enable process improvement through the elimination of non-value added steps. There are several key features of a VSM that deserve mention. First, the VSM must be created by a multidisciplinary team that includes front-line workers. One of the core tenets of lean is that empowerment of front-line workers to lead improvement efforts creates a cultural transformation in an organization toward one of continuous improvement. Furthermore, front-line workers understand a particular process with a level of intimacy not available to more senior managers. Second, a VSM must be detailed enough to allow identification of all non-value added steps, no matter how small. The cumulative improvement from many small changes is what makes lean so impactful. Third, for each step in the VSM, the team must consider whether the step brings value to the patient and whether a safer, more efficient, or more effective option exists. If the answer to any of these questions is “yes”, then there is an opportunity for improvement. Fourth, the creation of a VSM is an iterative process. As interventions are undertaken to eliminate waste, the VSM changes and must be revaluated in comparison with an “ideal” state. As such, it represents the continuous nature of lean.
Several examples of VSM in gastroenterology are available in the literature (6–8). In each of these examples, a detailed VSM created by a multidisciplinary team is utilized to identify waste in a process and guide successful quality improvement interventions. The complexity of each of these VSM differs, however, reflecting the process being modeled and the resources available to assist in the improvement effort. Indeed, the assistance of experts in lean can be invaluable in the early stages of a lean journey to model best practices.
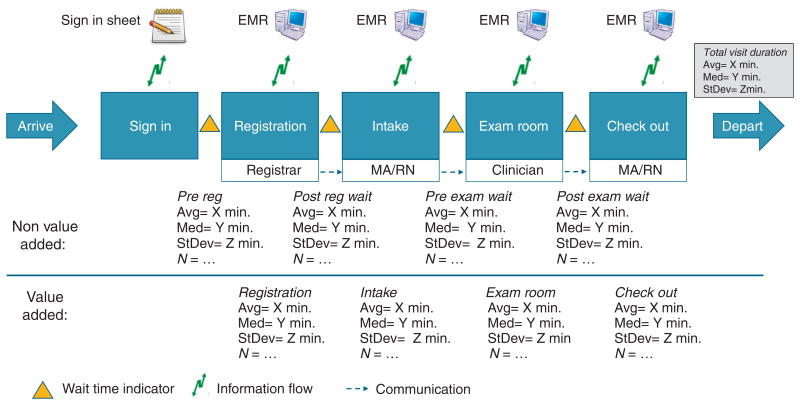
As an example, Figure 1 shows a template for a simple VSM of an outpatient clinic. Patients arrive, sign in, register, undergo intake, an exam, and are discharged. Between each of these events is a waiting time for the next operation to proceed. For each event in the process, the value added time of the patient interaction may be calculated, as well as the non-value added time of the wait between each event. Non-value added time may be broken up into both “necessary non-value added time” and “waste”. Necessary non-value added time may be, for example, insurance verification that must, for regulatory reasons, be processed by fax rather than phone or electronically, resulting in delays that are beyond the control of the system. Figure 1 shows both the process flow of the patient through the clinical environment, and the necessary communication at each step with the electronic medical record and between members of the medical team. This represents both the flow of material (people) and information. Using this tool, it is possible to identify and isolate the effects of process interventions to specific sub-stages, thereby revealing the inherent value of potential operation improvements.
Figure 1. Template for the value stream map of an outpatient clinic.
Value stream mapping is but one tool in the set of tools and principles of Lean Healthcare. Although a detailed instruction manual is beyond the scope of this commentary, practices are encouraged to use the principles highlighted above and the references provided to explore the benefits that value stream mapping can bring to their practice.
Acknowledgments
The authors thank Anna Frye, BS, of The Children's Hospital of Philadelphia for assistance with the figure.
Financial support: Gellad's effort is funded by Veterans Affairs Health Services Research and Development Career Development Award (CDA 14-158).
Footnotes
Guarantor of the article: Ziad F. Gellad, MD, MPH.
Specific author contributions: Ziad F. Gellad and Theodore Eugene Day contributed to manuscript design, manuscript drafting, critical revision, and approval of the final draft.
Potential competing interests: None.
References
- 1.Gabow PA, Goodman PL. The lean prescription: powerful medicine for our ailing healthcare system. CRC Press; Boca Raton, FL: 2015. [Google Scholar]
- 2.Toussaint JS, Berry LL. The promise of lean in health care. Mayo Clin Proc. 2013;88:74–82. doi: 10.1016/j.mayocp.2012.07.025. [DOI] [PubMed] [Google Scholar]
- 3.Lee E, Grooms R, Mamidala S, et al. Six easy steps on how to create a lean sigma value stream map for a multidisciplinary clinical operation. J Am Coll Radiol. 2014;11:1144–9. doi: 10.1016/j.jacr.2014.08.031. [DOI] [PubMed] [Google Scholar]
- 4.Simon RW, Canacari EG. A practiceal guide to applying lean tools and management principles to health care improvement projects. AORN J. 2012;95:85–100. doi: 10.1016/j.aorn.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Rother M, Shook J. Learning to see: value-stream mapping to create value and eliminate muda Lean Enterprise Institute: Cambridge. MA. 1999 [Google Scholar]
- 6.Sugianto JZ, Stewart B, Ambruzs JM, et al. Applying the principles of lean production to gastrointestinal biopsy handling: from the factory floor to the anatomic pathology laboratory. Lab Med. 2015;46:259–64. doi: 10.1309/LMJCUFUN0LT8C6DB. [DOI] [PubMed] [Google Scholar]
- 7.Patel KK, Cummings S, Sellin J, et al. Applying lean design principles to a gastrointestinal endoscopy program for uninsured patients improves health care utilization. Clin Gastroenterol Hepatol. 2015;13:1556–1559. doi: 10.1016/j.cgh.2015.07.003. e4. [DOI] [PubMed] [Google Scholar]
- 8.Damle A, Andrew N, Kaur S, et al. Elimination of waste: creation of a successful lean colonoscopy program at an academic medical center. Surg Endosc. 2015:1–6. doi: 10.1007/s00464-015-4599-6. [DOI] [PubMed] [Google Scholar]