Abstract
INTRODUCTION
Dietary quality has been linked to obesity in children. Obesity among children of farmworker families exceeds that of other US Hispanic children. Knowledge of their dietary quality is needed to understand the origins and prevention of this obesity.
METHODS
Mothers (n=237) of 3-year old children in farmworker families completed 3 24-hour recalls with trained interviewers using the Nutrition Data System for Research (NDS-R). Output was used to calculate total and component scores of the Revised Children’s Diet Quality Index (RC-DQI).
RESULTS
Mean total score was 62 (range 36–86) of an optimal score of 90. Scores for total fat, total grains, excess juice and iron were >80% of the optimum, but scores for added sugar, whole grains, fruits, and vegetables were considerably lower.
DISCUSSION
Children in farmworker families have low overall dietary quality. Intervention targeted to specific food issues may be an efficient way to addressing the problem.
Keywords: Obesity, Prevention, Minority, Nutrition
INTRODUCTION
Among US children aged 2 to 5, almost one in four were overweight or obese in 2011–12 (1). Proportions of obesity and overweight consistently vary along lines of race and ethnicity: while 17.4% and 3.5% of non-Hispanic white children were overweight and obese in 2011–12, rates were 13.1% and 16.7% among Hispanic children. These disparities may set the stage for observed disparities in adults, as chronic diseases and risk factors such as obesity and hypertension are higher among Hispanics, particularly in association with acculturation (2, 3).
Several aspects of child diet have been associated with weight status. Consumption of sugared beverages in childhood has been associated with development of overweight and obesity (4, 5). Greater consumption of whole grains, fruits, and vegetables has been associated with normal weight status in adults (6). This suggests that a diet high in whole foods and low in added sugars is a high quality diet for young children, which can promote healthy weight. Such a diet consumed from an early age may also help children gain familiarity with a variety of foods and form positive food habits (7, 8). Using both positive and negative food consumption findings, several measures of diet quality have been constructed and found associated with both precedent factors (e.g., parental feeding styles, socio-economic status (9, 10)) and weight-related outcomes (9, 11, 12).
Among the immigrant Hispanic population in the US, farmworkers constitute a medically under-served population with high rates of chronic disease. Farmworkers are employed as needed during the agricultural season to do hand labor in crop production. Some are migrants, moving and establishing temporary residences to work during the agricultural season, while others are seasonal workers, residing in one area year round and working seasonally in agricultural. The US farmworker population is estimated at 900,000 workers plus their dependents (13). The number of children is unknown, but previous estimates have put the number at over 800,000 (14). Because farm work is often the entry point through which immigrant families enter the US, farmworker families are important beyond their numbers for efforts to understand and prevent the development of childhood obesity in the Hispanic population.
Children of migrant and seasonal farmworkers are at risk for poor diet quality due to economic constraints, ineligibility for some food safety net benefits, migratory lifestyle, and housing with inadequate cooking facilities (15–19). Few studies exist of weight status in children of farmworkers, but all indicate these children have overweight and obesity rates exceeding other Mexican American children (19–23). Development of obesity prevention strategies requires understanding the diet of these children, as well as environmental, social, and cultural constraints on achieving a high quality diet.
This study is based on data from a sample of mothers and young children in farmworker families in North Carolina. North Carolina has the sixth largest farmworker population of states in the US. This paper describes: 1) the diet quality of preschool-age children of migrant and seasonal farmworkers in North Carolina, and 2) examines the association of diet quality with demographic factors. These findings are discussed in terms of environmental and social constraints on child diet in farmworker families.
METHODS
The data for this study are from the Niños Sanos study, a 2-year prospective cohort study of 248 young Latino children living in farmworker families in North Carolina designed to understand the role of diet and physical activity in the development of obesity. This analysis is based on data collected at the baseline assessment and is restricted to 237 for whom complete data exist. The Wake Forest School of Medicine Institutional Review Board approved all research procedures. Mothers provided signed informed consent. A Certificate of Confidentiality was obtained from the National Institutes of Health to protect the anonymity of study participants.
Sampling
The goal was to create a sample representative of farmworker families with young children in North Carolina. Because no sampling frame of Latino farmworker families existed and because the narrow child-age range would require contacting a substantial fraction of the eligible population, a site-based sampling plan (24–26) was developed to provide as large a contact base as possible. Such a plan is appropriate for hard-to-reach populations and has been used by the research team over the last 19 years in studies focused on the health of immigrant Latinos and their families (27–29). “Sites” are organizations or locations with which members of the target community are associated. Logically, all families should be associated with a site and most with multiple sites. In this study, site categories (and number of sites targeted within categories) were: Migrant and regular Head Start Programs-7; Migrant Education Programs-15; Community Health Centers-4; WIC-1; community partner non-profit organizations serving Latino immigrants-2; and stores, churches, and events serving predominantly farmworkers-7. In addition, door-to-door recruitment was undertaken in Latino neighborhoods and farmworker camps; and families from current or recently completed Latino farmworker studies and from personal networks were contacted.
Recruitment
For institutions, such as Head Start, subject to privacy regulations, a staff member contacted the family, introduced the study, and obtained authorization to release contact information. In other cases, a trained data collector, who was a native Spanish-speaker, attempted contact with individuals for whom contact information was available. Once contact was made, the data collector introduced and explained the study, including its requirements and incentives and screened for inclusion criterion, which were: 1) a woman who self-identified as Latino, 2) a child 2.5 to 3.5 years of age, and 3) at least one member of the household that worked in farm work during the past year. Women were excluded if the focal child had a special health care need limiting normal physical activity. Eligible women were invited to participate in the study, and an appointment was scheduled for baseline data collection. In most cases, baseline data were collected at the time of recruitment.
Data Collection
Interviews were collected from 4/19/11 through 4/20/12, by 9 trained interviewers. The maternal questionnaire collected demographic, family, and household characteristics. Interviewer-administered questionnaires were completed in Spanish in participants’ homes or another location determined by the participant. Mothers received $10 for completing the interview.
Dietary data were collected using three 24-hour recalls during a seven day period, including one weekend day and two weekdays. The first recall was conducted face-to-face in the context of the interview; subsequent interviews were conducted by telephone. Participants were given an incentive of $10 per completed recall. Mothers who lacked a telephone were loaned a cell phone programmed only for study use. At the time of the diet recall, mothers were asked to report the amount of time the child spent watching television during the recall day.
During the in-home interview, each participant was instructed on use of a printed serving size guide; the interviewer measured the size of child’s usual bowl, plate and cup to facilitate calculation of serving sizes. Data were reported by mothers, who sought input from caregivers, particularly for away-from-home food consumption. For children enrolled in formal preschools or daycares, food intake data were obtained (with mothers’ permission) directly from the caregivers.
Dietary data were collected by bilingual staff members with the Nutrition Data System for Research (NDS-R) software (Nutrition Coordinating Center, University of Minnesota, Minneapolis, MN) developed by the Nutrition Coordinating Center at the University of Minnesota, which uses the multiple-pass method (30). This method asks the respondent to give a general chronological overview of the food consumption (e.g., meals, snacks, primary foods) before food consumption events are probed in detail to elicit serving sizes, preparation methods, brand names, and condiments. NDS-R contains over 18,000 foods, 8000 brand-name products, and many Hispanic and Latino foods. The software provides values for 139 nutrients, nutrient ratios, food-group serving counts, and other food components. The NDS-R computer interface was in English; all queries to the mothers were presented in Spanish. Because some mothers needed to obtain intake data from caregivers, the random day procedure usually used for repeated recalls was modified. The initial recall was unannounced, because it was part of the interview. Subsequent interviews were negotiated at that time to fit the mother’s availability, although the weekday/weekend distribution of days was maintained. Interviewer training and quality assurance review of randomly selected recalls was provided by the Diet, Physical Activity and Body Composition Core of the UNC-CH Nutrition Obesity Research Center, Anna Maria Siega-Riz, PhD, director.
Measures
Dietary intake was output as nutrients and as food group servings per day and averaged for the three days. Dietary quality was calculated using specifications of the Revised Children’s Diet Quality Index (RC-DQI), which are described in detail elsewhere (12, 31). This index has a total score of 90 points, and includes 13 components: added sugar, total fat, linoleic and linolenic fatty acids, docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA), total grains, whole grains, vegetables, fruits, excess fruit juice, dairy, and iron intake, as well as a component representing a proxy for energy balance (time spent watching television adjusted for total daily energy intake). Calculation of scores is based on both over- and under-consumption.
Mothers reported their own age, level of educational attainment, birth country, and employment arrangement (i.e., not working, working outside of farm work, working in farm work), the child’s gender, and child’s birth country. Family migrant status was based on maternal characterizations of her or another household member’s involvement in farm work: if she classified herself or another as a “migrant worker who moves from place to place to do farm work,” the family was classified as a migrant. Otherwise, the family was classified as being seasonal. For child care arrangements, children whose mothers reported their child being involved in Migrant Head Start, Head Start, or Smart Start were classified as having government child care; other options were private daycare center, in-home child care, and no child care.
Analyses
Descriptive statistics summarized the sample characteristics. RC-DQI total scores were grouped into four quartiles. Mean (SD) component scores are presented for the full sample and lowest and highest RC-DQI total score quartiles. Means (SD) for component foods and selected nutrients are presented for all four RC- DQI total score quartiles. For each nutrient, a one-way ANOVA with a linear contrast was performed to test for differences across RC-DQI quartiles. Multivariate linear models tested for relationships between child and family characteristics and diet quality components. A 5% significance level was used for all analyses. All analyses were performed using SAS v. 9.4.
RESULTS
Of the 248 mother-child dyads enrolled in the Niños Sanos study, 8 failed to complete any diet recalls; and 3 provided incomplete dietary data. Therefore, these analyses are based on 237 dyads. Mothers ranged in age from 18 to 45, with most between the ages of 26 to 35 years (Table 1). Most had less than a high school education; 43.5% had six or fewer years of education. Over 85% were born in Mexico. About half the children (52.3%) were two years of age; the remainder (47.7%) were three. There were slightly more girls than boys. Almost all children (98.7%) were born in the US. About 40% were in some form of child care.
Table 1.
Selected Demographic Characteristics of Participating Mothers and Children in Latino Farmworker Families (N = 237)
| N | (%) | |
|---|---|---|
| Mothers | ||
| Age (yr) | ||
| 18–25 | 69 | (29.1) |
| 26–35 | 131 | (55.3) |
| 36–45 | 37 | (15.6) |
| Education (yr) | ||
| 0–6 | 103 | (43.5) |
| 7–9 | 73 | (30.8) |
| 10+ | 61 | (25.7) |
| Place of birth | ||
| US | 11 | (4.6) |
| Mexico | 203 | (85.7) |
| Other | 23 | (9.7) |
| Family status | ||
| Migrant | 63 | (26.6) |
| Seasonal | 174 | (73.4) |
| Children | ||
| Age (yr) | ||
| 2 | 124 | (52.3) |
| 3 | 113 | (47.7) |
| Gender | ||
| Boy | 115 | (48.5) |
| Girl | 122 | (51.5) |
| Place of birth | ||
| US | 234 | (98.7) |
| Other | 3 | (1.3) |
| Child care arrangements1 | ||
| Government (e.g., Migrant Head Start) | 53 | (22.6) |
| Private day care center | 16 | (6.8) |
| In-home child care | 32 | (13.6) |
| No child care | 134 | (57.0) |
Missing data for two cases.
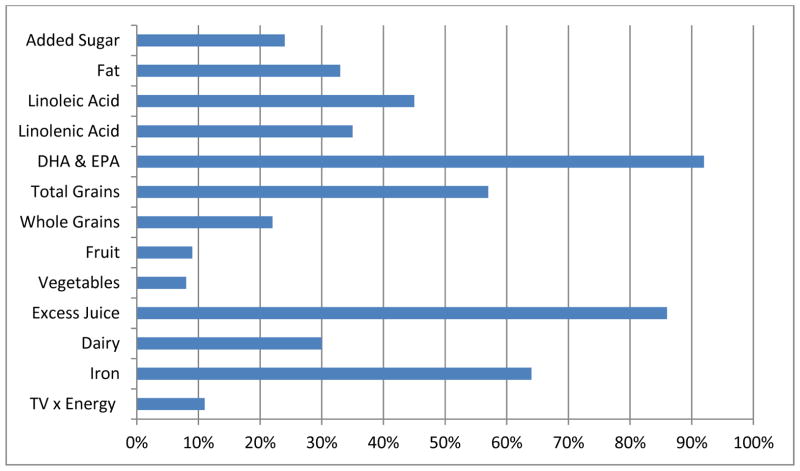
The mean (SD) total RC-DQI score was 61.8 (9.8). Scores ranged from 36.1 to 86.2, none reaching the optimum score of 90. Examination of individual component scores showed that total fat, fatty acids, total grains, excess juice, and iron all exceeded 80% of the maximum diet quality score and had narrow distributions (Table 2). Mean scores for added sugar, whole grains, fruit, and vegetable components are considerably lower (60% or less) than the maximum score with wide distributions. Comparing component scores from the lowest and highest quartile of total RC-DQI scores, component scores track with the total score, except for total fat, which has almost no variation. The components with the highest percentage of children reaching the optimum scores were DHA and EPA, excess juice, and iron (Figure 1). A third or less achieved optimums for added sugar, fat, whole grains, fruits, vegetables, dairy, and energy.
Table 2.
Comparison of RC-DQI component scores in the highest and lowest quartile of total RC-DQI score.
| Component | Maximum Score | Mean (SD) | RC-DQI Total Score Quartile
|
|
|---|---|---|---|---|
| Lowest | Highest | |||
| Added Sugar | 10 | 5.1 (4.0) | 2.7 (3.6) | 8.4 (2.4) |
| Total Fat | 2.5 | 2.2 (0.3) | 2.2 (0.3) | 2.2 (0.3) |
| Linoleic Acid | 2.5 | 2.1 (0.4) | 2.1 (0.4) | 2.2 (0.4) |
| Linolenic Acid | 2.5 | 2.1 (0.5) | 2.0 (0.4) | 2.2 (0.4) |
| DHA + EPA | 2.5 | 2.4 (0.4) | 2.4 (0.5) | 2.5 (0.1) |
| Total Grains | 5 | 4.4 (1.0) | 3.7 (1.3) | 4.7 (0.6) |
| Whole Grains | 5 | 2.9 (1.7) | 1.9 (1.4) | 3.7 (1.5) |
| Fruit | 10 | 4.5 (2.9) | 3.1 (2.3) | 6.3 (3.0) |
| Vegetables | 10 | 4.3 (2.9) | 2.8 (2.4) | 6.4 (3.0) |
| Excess Juice | 10 | 9.1 (2.4) | 9.0 (2.6) | 9.6 (1.6) |
| Dairy | 10 | 7.5 (2.5) | 5.8 (2.7) | 8.7 (1.8) |
| Iron | 10 | 8.1 (2.6) | 6.0 (2.6) | 9.3 (1.7) |
| Television x Energy | 10 | 7.0 (2.4) | 6.0 (2.5) | 8.2 (1.6) |
Figure 1.
Percentage of children reaching optimal score for Revised Children’s Diet Quality Index total score and component scores.
Comparisons of food and nutrient intakes across quartiles of total RC-DQI show that most intakes vary as expected, with significant changes across quartiles (Table 3). For example, percent of calories from added sugar drops from 20.1 (± 6.9) to 10.3 (± 3.7) from lowest to highest quartile. Intakes of grain, whole grain, vegetables, fruits, dairy, iron, protein, fiber, and vitamin C all increase across quartiles. Total fat, as well as specific fatty acids, and the excess juice component show little difference across total RC-DQI quartiles. Reported television viewing time decreases from lowest to highest quartile.
Table 3.
Mean (± standard deviation) of foods and selected nutrients by total RC-DQI score quartiles
| Component | RC-DQI Total Score Quartiles
|
F | P value | |||
|---|---|---|---|---|---|---|
| Quartile 1 (36.1–55.0) | Quartile 2 (55.1–62.2) | Quartile 3 (62.3–68.7) | Quartile 4 (69.3–86.2) | |||
| Added sugar (% kcal) | 20.1 (6.9) | 17.6 (5.8) | 12.6 (5.6) | 10.3 (3.7) | 110.55 | <.0001 |
| Total fat (% kcal) | 27.4 (5.5) | 27.3 (5.4) | 29.0 (5.8) | 27.9 (5.5) | 0.96 | 0.3278 |
| Linoleic acid (% kcal) | 5.1 (2.1) | 4.6 (1.6) | 5.3 (1.8) | 5.1 (1.9) | 0.36 | 0.5493 |
| Linolenic acid (% kcal) | 0.6 (0.3) | 0.5 (0.2) | 0.6 (0.2) | 0.6 (0.2) | 1.84 | 0.1759 |
| DHA + EPA (% kcal) | 4.8 (4.7) | 4.9 (4.3) | 4.4 (4.1) | 3.7 (2.8) | 2.52 | 0.1139 |
| Grain (oz) | 2.6 (1.4) | 3.3 (1.5) | 3.9 (1.5) | 3.9 (1.6) | 27.17 | <.0001 |
| Whole grains (oz) | 0.6 (0.5) | 0.9 (0.6) | 1.3 (1.1) | 1.4 (0.9) | 39.10 | <.0001 |
| Vegetable (c) | 0.3 (0.3) | 0.4 (0.3) | 0.5 (0.4) | 0.7 (0.5) | 44.19 | <.0001 |
| Fruit (c) | 0.5 (0.4) | 0.6 (0.4) | 0.8 (0.5) | 1.1 (0.6) | 51.88 | <.0001 |
| Dairy (c) | 1.4 (1.0) | 1.9 (0.9) | 2.0 (1.0) | 2.1 (0.7) | 16.82 | <.0001 |
| Excess Juice (c) | 0.1 (0.2) | 0.1 (0.2) | 0.1 (0.3) | 0.0 (0.2) | 0.71 | 0.4018 |
| Iron (g) | 6.1 (2.9) | 9.5 (4.7) | 11.5 (6.6) | 11.0 (4.1) | 35.98 | <.0001 |
| Television (hr) | 1.8 (1.2) | 1.5 (1.0) | 1.2 (0.9) | 0.8 (0.6) | 35.30 | <.0001 |
| Energy (kcal) | 1043.2 (371.0) | 1194.2 (345.9) | 1258.6 (382.2) | 1244.4 (344.4) | 10.16 | 0.0016 |
| Carbohydrates (g) | 153.6 (54.5) | 174.8 (50.9) | 176.6 (58.2) | 177.7 (50.1) | 5.67 | 0.0181 |
| Saturated fat (g) | 11.9 (6.4) | 14.9 (6.5) | 15.1 (5.4) | 15.3 (6.2) | 8.29 | 0.0044 |
| Protein (g) | 36.1 (14.4) | 43.3 (15.3) | 48.1 (16.1) | 48.3 (13.7) | 23.11 | <.0001 |
| Fiber (g) | 6.5 (2.6) | 8.7 (2.8) | 10.6 (4.4) | 12.6 (4.7) | 84.58 | <.0001 |
| Calcium (mg) | 587.8 (302.9) | 804.6 (257.4) | 853.6 (325.2) | 881.6 (245.8) | 31.73 | <.0001 |
| Vitamin A (IU) | 1916.2 (1028.9) | 2562.6 (1194.9) | 2677.9 (1349.9) | 3887.6 (2927.5) | 33.65 | <.0001 |
| Vitamin C (mg) | 57.1 (45.3) | 67.6 (38.4) | 77.8 (49.4) | 84.4 (47.3) | 12.28 | 0.0005 |
Total RC-DQI scores did not vary by farmworker status of the family, gender or age of the child, and type of child care arrangements used by the family (data not shown). When component scores were compared by these same characteristics, only three significant associations were found. The dairy component score was associated with age; for each month of age, the dairy component was an average of 0.072 lower (p=.011). The whole grains component was also associated with age, with the component score 0.045 higher, on average, for each month of age (p=0.018). The total grains component was associated with gender; girls had a component score 0.29 points lower, on average, than boys (p=0.030).
DISCUSSION
These findings show that young children in farmworker families have relatively poor diet quality. On average, they score almost 40% lower than optimal for the summary score. Looking at individual components, they have particularly low diet quality in four areas: added sugar, whole grains, fruits, and vegetables. Diet quality appears to be relatively high for total grains, fats, and excess juice. The added sugar component in the RC-DQI score sums sugars in prepared and processed foods such as cereals, cookies, and cakes, which are typically sources of refined grains, as well as fruit “drinks” that are not 100% juice. This suggests that this group is likely consuming a diet that is high in refined grains, with little whole fruit or vegetables.
The RC-DQI has been used to assess diet quality of children in several national data sets, including the Continuing Survey of Food Intakes by Individuals (CSFII) for 1994–1998 (31) and the National Health and Nutrition Examination Survey (NHANES) for 2003–2006 (32). Compared to the CSFII, the present study found lower median diet quality scores and a more constrained range of values for most components. While the present study found better scores for whole grains, the scores for fruits and vegetables were considerably worse than children in the CSFII sample. Compared to NHANES, children in the present study had higher values for whole grains, similar values for dairy and total grains, and much lower values for fruits and vegetables. Children from farmworker families may score better than US children in general for whole grains because of consuming foods such as tortillas made with corn meal, but they still have scores less than 60% of the optimal score.
Excess juice is a concern because it can be a source of excess calories leading to obesity and metabolic syndrome (33, 34). Recommendations have been made to limit or even eliminate 100% fruit juice in children’s diets (35, 36). In the present study, children’s scores for excess juice were high, indicating they were not exceeding the American Academy of Pediatrics’ recommended 6 ounces per day (37). This may, however, conceal the fact that mothers were giving children less expensive fruit “drinks”, which have added sugar and are not included in the excess juice calculation.
One of the strengths of this study is its use of the RC-DQI. Several measures have been developed to provide an assessment of diet quality. The Health Eating Index (HEI) and Diet Quality Index (DQI), for example, were developed to measure compliance with federal recommendations (38, 39), and have been revised over time to reflect changes in these recommendations (40, 41). Because neither the HEI nor the DQI were designed to address the specific needs of young children, the Children’s Diet Quality Index (C-DQI) (31) was developed for children under 6 and revised to the RC-DQI (12) to take account of changes in dietary intake guidance. All of these measures have specific components reflecting food categories and include a total score. The RC-DQI incorporates gender- and age-specific recommendations, and adjusts its component scores for intakes below and above recommended levels. It goes beyond other indices’ focus primarily on Dietary Guidelines for Americans in incorporating recommendations from the American Academy of Pediatrics, as well as the Dietary Reference Intakes for macronutrients and iron, and the American Dietetic Association recommendations for total energy and television viewing time (12, 31). The use of the RC-DQI allows identification of both excessive and deficient intakes, and therefore can serve as the basis for efforts to improve diet.
This study’s results should be interpreted in light of its limitations. Data were collected from farmworker families in one region, and results might differ in other areas. The RC-DQI method relies on maternal reports; mothers might have adjusted their reports to provide more socially desirable answers or they might have forgotten foods. Some children were in child care on recall days. This required the usual procedures of unannounced random days for data collection to be modified so that mothers could obtain diet information from caregivers. Nevertheless, the dietary data were collected using a rigorous multi-pass method (30) and used three 24-hr recalls, rather than the single recall used in some studies, so captured both weekday and weekend intakes.
Farmworkers constitute a vulnerable population with several characteristics that put them at risk for poor dietary quality: low income, food insecurity, rural isolation, poor housing, and lack of access to the social safety net programs, including those related to food (15–17, 42, 43). Beyond such structural factors, parental behaviors such as indulgent feeding styles may also underlie poor dietary quality (34). The present study confirms that, for children in farmworker families, dietary quality is poor. Because of the connections of diet quality to obesity and the negative health outcomes of obesity, interventions to improve dietary quality are needed for farmworker families.
Acknowledgments
This research was supported by a grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD059855). Dietary data analysis was supported by a grant to University of North Carolina Chapel Hill from the National Institute of Diabetes and Digestive and Kidney Diseases (P30 DK56350).
Footnotes
A preliminary version of this paper was presented at the American Public Health Association annual meeting, November 2012.
REFERENCES CITED
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daviglus ML, Talavera GA, Avilés-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775–1784. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Ruyter JC, Olthof MR, Seidell JC, Katan MB. A trial of sugar-free or sugar-sweetened beverages and body weight in children. N Engl J Med. 2012;367(15):1397–406. doi: 10.1056/NEJMoa1203034. [DOI] [PubMed] [Google Scholar]
- 5.Zheng M, Rangan A, Olsen NJ, Andersen LB, Wedderkopp N, Kristensen P, Grøntved A, Ried-Larsen M, Lempert SM, Allman-Farinelli M, Heitmann BL. Substituting sugar-sweetened beverages with water or milk is inversely associated with body fatness development from childhood to adolescence. Nutrition. 2015;31:38–44. doi: 10.1016/j.nut.2014.04.017. [DOI] [PubMed] [Google Scholar]
- 6.Newby PK, Peterson KE, Berkey CS, Leppert J, Willett WC, Colditz GA. Dietary composition and weight change among low-income preschool children. Arch Pediatr Adolesc Med. 2003;157:759–64. doi: 10.1001/archpedi.157.8.759. [DOI] [PubMed] [Google Scholar]
- 7.Ventura AK, Birch LL. Does parenting affect children’s eating and weight status? Int J Behav Nutr Phys Act. 2008;5:15. doi: 10.1186/1479-5868-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Birch LL. Child feeding practices and the etiology of obesity. Obesity (Silver Spring) 2006;14(3):343–4. doi: 10.1038/oby.2006.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Couch SC, Glanz K, Zhou C, Sallis JF, Saelens BE. Home food environment in relation to children’s diet quality and weight status. J Acad Nutr Diet. 2014;114(10):1569–1579. doi: 10.1016/j.jand.2014.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang DD, Leung CW, Li Y, Ding EL, Chiuve SE, Hu FB, Willett WC. Trends in dietary quality among adults in the United States, 1999 through 2010. JAMA Intern Med. 2014;174:1587–95. doi: 10.1001/jamainternmed.2014.3422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lioret S, McNaughton SA, Cameron AJ, Crawford D, Campbell KJ, Cleland VJ, Ball K. Three-year change in diet quality and associated changes in BMI among schoolchildren living in socio-economically disadvantaged neighbourhoods. Br J Nutr. 2014;112:260–268. doi: 10.1017/S0007114514000749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kranz S, Findeis JL, Shrestha SS. Use of the Revised Children’s Diet Quality Index to assess preschooler’s diet quality, its sociodemographic predictors, and its association with body weight status. J Pediatr (Rio J) 2008 Jan-Feb;84(1):26–34. doi: 10.2223/JPED.1745. [DOI] [PubMed] [Google Scholar]
- 13.USDA. Farm Labor (December 2013) National Agricultural Statistics Service, USDA; 2013. [Accessed 3-6-14]. http://usda01.library.cornell.edu/usda/current/FarmLabo/FarmLabo-12-05-2013_revision.pdf. [Google Scholar]
- 14.Mines R. Children in immigrant and nonimmigrant farmworker families. In: Hernandez DJ, editor. Children of immigrants: Health, Adjustment and Public Assistance. Washington, DC: National Academy Press; 1999. pp. 620–658. [PubMed] [Google Scholar]
- 15.Quandt SA, Shoaf JI, Tapia J, Hernandez-Pelletier M, Clark HM, Arcury TA. Experiences of Latino immigrant families in North Carolina help explain elevated levels of food insecurity and hunger. J Nutr. 2006;136:2638–2644. doi: 10.1093/jn/136.10.2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Quandt SA, Summers P, Bischoff WE, Chen H, Wiggins MF, Spears CR, Arcury TA. Cooking and eating facilities in migrant farmworker housing in North Carolina. Am J Public Health. 2013;103:e78–84. doi: 10.2105/AJPH.2012.300831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quandt SA, Grzywacz JG, Trejo G, Arcury TA. Nutritional strategies of Latino farmworker families with preschool children: Identifying leverage points for obesity prevention. Soc Sci Med. 2014;123C:72–81. doi: 10.1016/j.socscimed.2014.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kilanowski JF. Patterns and correlates of nutrition among migrant farm-worker children. West J Nurs Res. 2012;34:396–416. doi: 10.1177/0193945910381597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaiser LL, Melgar-Quiñonez HR, Lamp CL, Johns MC, Sutherlin JM, Harwood JO. Food security and nutritional outcomes of preschool-age Mexican-American children. J Am Diet Assoc. 2002;102:924–929. doi: 10.1016/s0002-8223(02)90210-5. [DOI] [PubMed] [Google Scholar]
- 20.Borre K, Ertle L, Graff M. Working to eat: vulnerability, food insecurity, and obesity among migrant and seasonal farmworker families. Am J Ind Med. 2010;53:443–462. doi: 10.1002/ajim.20836. [DOI] [PubMed] [Google Scholar]
- 21.Kilanowski JF, Ryan-Wenger NA. Health status in an invisible population: carnival and migrant worker children. West J Nurs Res. 2007;29:100–120. doi: 10.1177/0193945906295484. [DOI] [PubMed] [Google Scholar]
- 22.Markowitz DL, Cosminsky S. Overweight and stunting in migrant Hispanic children in the USA. Economics & Human Biology. 2005;3:215–240. doi: 10.1016/j.ehb.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 23.Rosado JI, Johnson SB, McGinnity KA, Cuevas JP. Obesity among Latino children within a migrant farmworker community. Am J Prev Med. 2013;44(3 Suppl 3):S274–S281. doi: 10.1016/j.amepre.2012.11.019. [DOI] [PubMed] [Google Scholar]
- 24.Arcury TA, Quandt SA. Participant recruitment for qualitative research: a site-based approach to community research in complex societies. Hum Organ. 1999;58:128–133. [Google Scholar]
- 25.Faugier J, Sargeant M. Sampling hard to reach populations. J Adv Nurs. 1997;26(4):790–797. doi: 10.1046/j.1365-2648.1997.00371.x. [DOI] [PubMed] [Google Scholar]
- 26.Muhib FB, Lin LS, Stueve A, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(Suppl 1):216–222. doi: 10.1093/phr/116.S1.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Arcury TA, Grzywacz JG, Talton JW, et al. Repeated pesticide exposure among North Carolina migrant and seasonal farmworkers. Am J Ind Med. 2010;53(8):802–813. doi: 10.1002/ajim.20856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grzywacz JG, Quandt SA, Chen H, et al. Depressive symptoms among Latino farmworkers across the agricultural season: Structural and situational influences. Cultur Divers Ethnic Minor Psychol. 2010;16:335–343. doi: 10.1037/a0019722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quandt SA, Chen H, Grzywacz JG, Vallejos QM, Galvan L, Arcury TA. Cholinesterase depression and its association with pesticide exposure across the agricultural season among Latino farmworkers in North Carolina. Environ Health Perspect. 2010;118:635–639. doi: 10.1289/ehp.0901492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johnson RK. Dietary intake: How do we measure what people are really eating? Obesity Res. 2002;10(Suppl 1):63S–68S. doi: 10.1038/oby.2002.192. [DOI] [PubMed] [Google Scholar]
- 31.Kranz S, Hartman T, Siega-Riz AM, Herring AH. A diet quality index for American preschoolers based on current dietary intake recommendations and an indicator of energy balance. J Am Dietet Assoc. 2006;106:1594–1604. doi: 10.1016/j.jada.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 32.Kranz S, McCabe GP. Examination of the five comparable component scores of the diet quality indexes HEI-2005 and RC-DQI using a nationally representative sample of 2–18 year old children: NHANES 2003–2006. J Obes. 2013;2013:376314. doi: 10.1155/2013/376314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shefferly A, Scharf RJ, DeBoer MD. Longitudinal evaluation of 100% fruit juice consumption on BMI status in 2-5-year-old children. Pediatr Obes. 2015 Jun 25; doi: 10.1111/ijpo.12048. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chaidez V, McNiven S, Vosti SA, Kaiser LL. Sweetened food purchases and indulgent feeding are associated with increased toddler anthropometry. J Nutr Educ Behav. 2014;46:293–298. doi: 10.1016/j.jneb.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 35.Rader RK, Mullen KB, Sterkel R, Strunk RC, Garbutt JM. Opportunities to reduce children’s excessive consumption of calories from beverages. Clin Pediatr (Phila) 2014;53:1047–1054. doi: 10.1177/0009922814540989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wojcicki JM, Heyman MB. Reducing childhood obesity by eliminating 100% fruit juice. Am J Public Health. 2012;102:1630–1633. doi: 10.2105/AJPH.2012.300719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.American Academy of Pediatrics Committee on Nutrition. The use and misuse of fruit juice in pediatrics. Pediatrics. 2001;107:1210–1213. doi: 10.1542/peds.107.5.1210. [DOI] [PubMed] [Google Scholar]
- 38.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Dietet Assoc. 1995;95:1103–1108. doi: 10.1016/S0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- 39.Patterson EE, Haines PS, Popkin BM. Diet Quality Index: capturing a multidimensional behavior. J Am Dietet Assoc. 1994;94:57–64. doi: 10.1016/0002-8223(94)92042-7. [DOI] [PubMed] [Google Scholar]
- 40.Guenther PM, Reedy J, Krebs-Smith SM. Development of the Healthy Eating Index-2005. J Am Dietet Assoc. 2008;108:1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 41.Haines PS, Siega-Riz AM, Popkin BM. The diet quality index revised: a measurement instrument for populations. J Am Dietet Assoc. 1999;99:697–704. doi: 10.1016/S0002-8223(99)00168-6. [DOI] [PubMed] [Google Scholar]
- 42.Padilla YC, Scott JL, Lopez O. Economic insecurity and access to the social safety net among Latino farmworker families. Soc Work. 2014;59:157–165. doi: 10.1093/sw/swu013. [DOI] [PubMed] [Google Scholar]
- 43.Kilanowski JF, Moore LC. Food security and dietary intake in Midwest migrant farmworker children. J Pediatr Nurs. 2010;25:360–366. doi: 10.1016/j.pedn.2009.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]