Abstract
Despite considerable advances in the research and treatment, the precise relationship between inflammation and cardiovascular (CV) disease remains incompletely understood. Therefore, understanding the immunoinflammatory processes underlying the initiation, progression, and exacerbation of many cardiovascular diseases is of prime importance. The innate immune system has an ancient origin and is well conserved across species. Its activation occurs in response to pathogens or tissue injury. Recent studies suggest that altered ionic balance, and production of noxious gaseous mediators link to immune and inflammatory responses with altered ion channel expression and function. Among plausible candidates for this are transient receptor potential (TRP) channels that function as polymodal sensors and scaffolding proteins involved in many physiological and pathological processes. In this review, we will first focus on the relevance of TRP channel to both exogenous and endogenous factors related to innate immune response and transcription factors related to sustained inflammatory status. The emerging role of inflammasome to regulate innate immunity and its possible connection to TRP channels will also be discussed. Secondly, we will discuss about the linkage of TRP channels to inflammatory CV diseases, from a viewpoint of inflammation in a general sense which is not restricted to the innate immunity. These knowledge may serve to provide new insights into the pathogenesis of various inflammatory CV diseases and their novel therapeutic strategies.
Keywords: TRP, Inflammation, Innate immune system, Inflammasome, Cardiovascular, Disease
Introduction
In the past two decades, growing attention has been directed to the pivotal roles of immunoinflammatory processes in the initiation, progression, and exacerbation of many cardiovascular diseases including atherosclerosis, post-injury vascular stenosis, myocardial infarction, heart failure, myocarditis, vasculitis, and allograft vasculopathy [1–4]. This view originates from a remarkable paradigm shift made by Ross in 1990s who first described that “excessive inflammatory-fibroproliferative response to various forms of insult to the endothelium and smooth muscle of the artery wall” is essential for the pathogenesis of atherosclerosis [5]. There is now paramount evidence that both innate and adaptive immune reactions avidly contribute to many pathological changes in the cardiovascular system, which not only involve the remodeling of the major cellular components of cardiovascular tissues but also activated immune cells migrating and accumulating therein [6]. Of particular note, solid evidence is now rapidly accumulating for the central significance of “inflammasome,” which serves as a platform mediating many innate immune reactions. The inflammasome is composed of pattern recognition receptors, apoptosis-associated speck-like protein containing a CARD (ASC) [7], and caspase-1, which by cleaving their inactive precursors generate major inflammatory cytokines interleukin (IL)-β1 and IL-18. Because of its interesting connections to both pathogen- and non-pathogen-derived cell-toxic signals such as infection, tissue damage, metabolic disorders, and other dysfunctional states of cells (see below), the activation of inflammasome is thought to be a key process leading to chronic inflammatory and autoinflammatory diseases [8]. Yet, the mechanism(s) of the activation still remains poorly understood. There are however intriguing suggestions that activation of inflammasome may depend crucially on altered ionic balance (Ca2+, K+, Cl−) and production of noxious gaseous mediators and its downstream mediators (ROS, NO) [9–11]. At a first glance, besides other types of channels transporting K+, Cl−, and Ca2+, these properties are strongly reminiscent of transient receptor potential (TRP) channels.
This review paper aims to promote our understanding about this rapidly developing field, i.e., the emerging significance of TRP channels for immunoinflammatory mechanisms in the cardiovascular (CV) system, with particular interest in innate immunity. To this end, in the first parts, we will focus on both exogenous and endogenous factors related to innate immunity and its sustained status, i.e., chronic inflammation, which possibly connect to TRP channel activities. The emerging role of autophagy to regulate innate immunity and its possible connection to TRP channels will also be discussed. In the last part, we will discuss about the linkage of TRP channels to CV inflammatory diseases, but rather from a viewpoint of inflammation in a general sense which is not restricted to the innate immunity, because the available information in this field is still greatly limited. Readers interested in another important topic, the connection of adaptive immunopathophysiology to various Ca2+-mobilizing mechanisms, are advised to consult with a few excellent reviews published elsewhere [12].
Connection between TRP channels and innate immunity
The innate immune system has an ancient origin and is well conserved across species (plants, invertebrates, and vertebrates). This system defends on the frontline against microbial infection and tissue damage, consisting of environmental sensors, cellular signaling cascades, and production of antimicrobial peptides [13–16]. The recognition of pathogen-associated molecular patterns (PAMPs) or non-pathogen-associated (or danger- or damage-associated) molecular patterns (DAMPs) is the first step of activating the innate immune response, which is fulfilled via their specific receptors called the pattern recognition receptors (PRRs). The PRR family is comprised of membrane-bound Toll-like receptors (TLRs), C-type lectin receptors, retinoid acid-inducible gene (RIG)-1-like receptors, and nucleotide-binding oligomerization domain (NOD) receptor-like receptors (NLRs). TLRs have been shown to be expressed ubiquitously in cells constituting or residing in the CV system such as cardiomyocytes (TLR5), endothelial cells (TLR2/4), and macropharges/monocytes and dendritic cells (TLR1/2/4/5/8 and TLR1/2/3/7/9, respectively) [17]. Activation of PRRs by PAMPs or DAMPs is known to subsequently activate inflammasomes, whereby to promote the production of highly proinflammatory cytokines such as IL-1β and IL-18 [18]. A variety of inflammatory factors are suggested to activate the inflammasome. These include both direct and indirect signal recognition factors such as virus, bacterial toxins, particle matters, autoantibodies, and other products released from cells in dysfunction. Although there is no biochemical or morphological evidence for the coexpression with these PPRs, recent studies have suggested that TRP channels may functionally act as a cofactor PAMP/DAMP-mediated signaling for a multitude of ligands of both endogenous and exogenous origins [19]. Available evidence suggests that the connection of TLRs to TRP channels occurs through directly by LPS (TRPA1; [20]); diacylglycerol (DAG) (TRPC6; [21]); ROS (TRPM4 and TRPM7; [22], [23]); and PKC (TRPV1; [24]).
TRP channels are a family of non-selective cation channels that function as polymodal signal detectors [25, 26] and involved in a variety of body functions and diseases [27]. TRP channels are membrane proteins with six putative transmembrane segments (S1–S6) and a pore region between S5 and S6. About 30 different mammalian TRP channels have been identified and classified into six subfamilies on the basis of sequence homology: canonical or classical (TRPC; TRPC1–7), vanilloid (TRPV; TRPV1–6), melastatin (TRPM; TRPM1–8), polycystin (TRPP; TRPP2, TRPP3, TRPP5), mucolipin (TRPML; TRPML1–3), and ankyrin (TRPA; TRPA1) [28]. Different TRP channels show distinct cation selectivities and gating mechanisms and can be activated by a wide array of physical and chemical stimuli [26, 28, 29]. The regulation of TRP channels occurs at transcriptional, translational, and post-translational levels, which frequently depends on the ionic balance, microbial ligands, cytokines, or reactive oxygen species (ROS). Indeed, inflammatory transcription factors such as nuclear factor-kappa B (NF-κB), signal transducer and activator of transcription 3 (STAT3), and hypoxia-inducible factor (HIF)-1 are linked to ROS and elevated intracellular Ca2+ concentration. These features render TRP channels potentially effective to modulate inflammations.
In the following, we will discuss about how TRP channels are connected to respective factors and mechanisms that can activate/modulate inflammation through innate immunity.
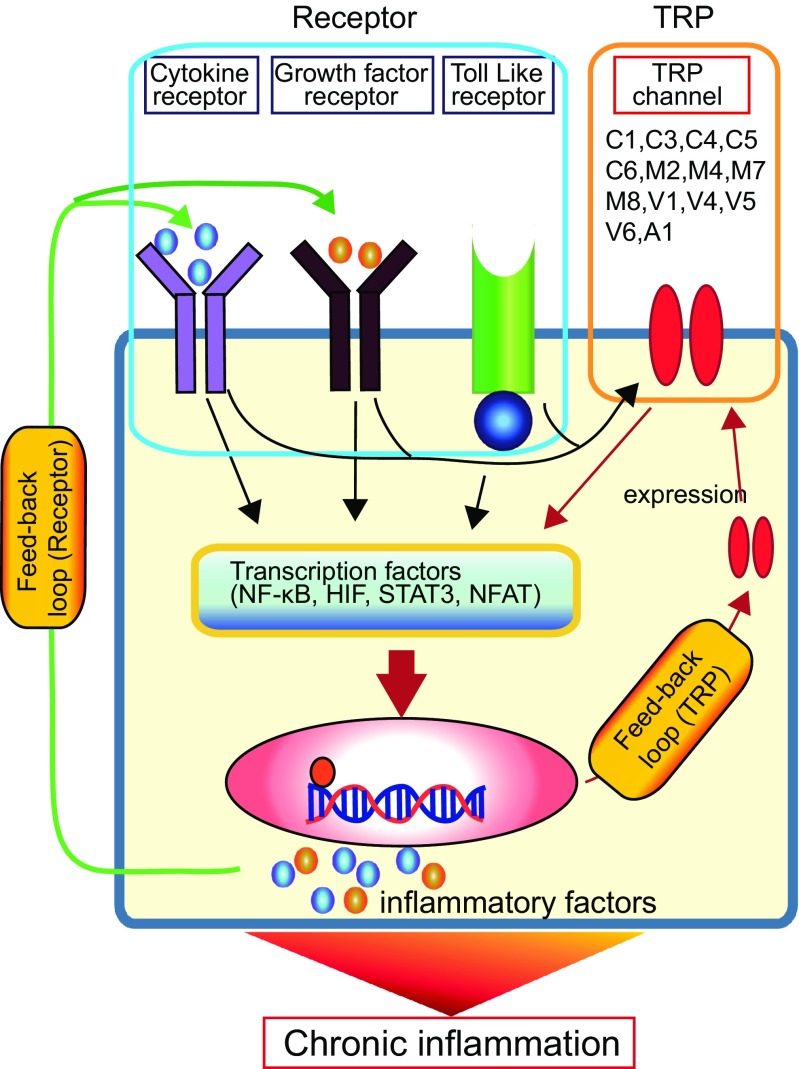
Factors that affect innate immune response via TRP channels (see Fig. 1)
Fig. 1.
Factors affecting innate immune response via TRP channels. An incoming microorganism or virus infection can induce inflammasome activation by stimulating innate immune receptors, such as Toll-like receptors (TLRs). Alternatively, TRP channel can be activated by the constituents of microorganism (e.g., LPS) directly or indirectly through TLR activation. TRP channel is also activated by potentially toxic/harmful environmental factors, such as MSU, silica, Alum, Aβ, and PM. In addition, an essential nutrient and a cellular constituent cholesterol can modulate TRP channel activity. Abnormal TRP channel activity causes Ca2+ influx and thereby produces ROS. The resultant intracellular Ca2+ elevation and ROS may induce inflammasome activity. Moreover, dysfunction of TRP channel in mitochondria or lysosome can also activate inflammasome. It should be noted that appropriate operation of autophagy is essential to suppress the caspase-1 activity, which would prevent the production of inflammatory cytokine (IL-1β and IL-18). How TRP channel-mediated Ca2+ influx regulates the inflammasome activation is not fully understood; but quite conceivably, it would play a key role in innate immune response. Question marks denote the hypothetical pathways that will require further proof
Viral and bacterial infections
Viral and bacterial infections are logical candidates for environmental triggers of immune reactions associated with TRP channel-dependent signaling and inflammasome activation. Upon recognition of microbial pathogens, TLRs serve as germline-encoded PRRs that play a central role in host cell recognition and responses. However, how TLR-dependent signaling links to TRP channel was unclear until very recently.
Several studies in the past few years revealed intriguing connections of TLRs to TRP channels. One study reported that hemolytic streptococcal infection affects the expression levels of at least seven TRP members, i.e., TRPC4, TRPM6, TRPM7, TRPM8, TRPV1, TRPV4, and TRPA1 [30, 31]. Another study showed that TRPC1 plays a functional role in host defense against gram-negative bacteria. Upon infection, TRPC1 (−/−) mice exhibited decreased survival, severe lung injury, and systemic bacterial dissemination. Furthermore, siRNA silencing of TRPC1 resulted in decreased Ca2+ entry, reduced proinflammatory cytokine production, and lowered bacterial clearance. Importantly, bacterium-mediated activation of TRPC1 was coupled with a cascade of TLR4 signaling; TLR4-dependent, TRPC1-mediated Ca2+ entry triggers PKCα activity to facilitate NF-κB/c-Jun N-terminal kinase (JNK) activation and augment the proinflammatory response, leading to tissue damage and eventually mortality. These findings favor the view that activation of TRPC1 is required for the host defense against bacterial infections through the TLR4-TRPC1-PKCα signaling pathway, but its excessive activity may lead to exacerbation of inflammation [32]. A similar but in-opposite-direction involvement of TRPC1-mediated Ca2+ entry in TLR-mediated inflammation has been demonstrated in microglia and macrophages from mice intracranially inoculated with a helminth Mesocestoides corti [33, 34]; it has been known that humans infected with a related helminth cestode Taenia solium have immunosuppressive rather than inflammatory responses in the asymptomatic phase after the infection. Experiments using soluble parasite factors from Mesocestoides-infected mice showed that suppression of TRPC1-mediated store-operated Ca2+ entry by these factors and consequent inhibition of NF-κB, JNK, and MAPK pathways are likely responsible for the immunosuppression. This novel immunosuppressive mechanism appears therapeutically useful to prevent the initiation of TLR-dependent inflammatory response via suppression of TRPC1 activity. In cultured macrophages, however, degradation of TRPC1 by caspase-11, an inducible caspase which is activated by NLRP3 inflammasome activator lipopolysaccharide (LPS), was found to increase the secretion of IL-1β. This negative regulation by TRPC1 occurred independently of caspase-1 cleavage or cell death [35] and thus likely reflects a distinctive mechanism from those described above. Consistently, a higher IL-1β secretion was observed in the sepsis model of TRPC1-deficient mice made by intraperitoneal LPS injection [35]. Although there is always a caveat to the relevance of knockout studies such as compensatory expression of homologous or other types of molecules which might affect downstream signaling (similar arguments may also hold for other TRP knockout models; see below), these results collectively imply the presence of multiple signaling pathways involving TRPC1 that regulate TLR-mediated inflammation. Further detailed analyses will be necessary to understand how manipulation of TRPC1 activity could be utilized for immune-modulatory interventions of inflammation.
In addition, there is evidence linking other TRP members to TLR-mediated signaling. In airway smooth muscle (ASM) cells, exposure to a proinflammatory cytokine TNF alpha (TNFα) or a mixture of allergens (ovalbumin, house dust mite, Alternaria, and Aspergillus extracts) causes both acute and chronic inflammations. These inflammatory responses involve at least in part increased secretion of brain-derived neurotrophic factor (BDNF) in a manner dependent on TRPC3-mediated Ca2+ entry [36]. In endothelial cells (ECs), endotoxin (LPS) induces pathological vascular leakage. This occurs through the interaction between TLR4 signaling and TRPC6-mediated Ca2+ entry, which causes increased endothelial permeability via activation of non-muscle myosin light chain kinase (MYLK) and NF-κB. Genetic deletion of TRPC6 rendered mice resistant to endotoxin-induced barrier dysfunction and inflammation and protected against sepsis-induced lethality [21].
TRPM4 is causally related to LPS-induced endothelial cell death via intracellular Na+ overloading. Pharmacological inhibition of TRPM4 activity with 9-phenathrol or glibenclamide was found to attenuate this consequence, suggesting a therapeutic potential of TRPM4 for endotoxin shock [22]. TRPM7-mediated intracellular concentration of Ca2+ ([Ca2+]i) elevation serves as a key regulator for endotoxin-induced endothelial fibrosis through endothelial to mesenchymal transition [23]. This channel is also implicated in LPS-induced endothelial cell migration via TLR4/NF-κB pathway [37]. TRPM2-deficient mice shows compromised innate immunity against Listeria monocytogenes infection which allows uncontrolled replication of the bacteria with significantly reduced production of IL-12 and interferon-γ [38]. Consistent with this finding, in a cecal ligation and puncture (CLP)-induced mouse sepsis model, genetic disruption of TRPM2 was found to cause impaired host defense, leading to increased mortality associated with increased bacterial burden, organ injury, and systemic inflammation. Interestingly, this finding appears to reflect failed upregulation of heme oxgenase (HO)-1 in macrophages which is normally induced by TRPM2-mediated Ca2+ influx and essential for bacterial clearance [39].
In recent years, the potential benefits of TRPV1 activation have been recognized for the abatement of inflammatory response. For example, in Helicobacter pylori-positive patients, the genetic polymorphism of TRPV1 945G>C has been suggested to be one of the pathophysiological factors of functional dyspepsia [40]. In murine sepsis models, genetic or pharmacologic disruption of TRPV1 can affect mortality, blood bacteria clearance, and cytokine response, in such a pattern that may vary according to the sepsis-inducing events and the methods of TRPV1 disruption [41, 42]. In salivary glands, polyinosinic-polycytidylic acid or LPS activates, via TLR4 activation, NF-κB by IκB-α degradation and phosphorylation to release highly proinflammatory cytokines TNFα and IL-6. Capsaicin inhibits this process by interacting with the NF-κB pathway whereby to potentially alleviate inflammation of salivary glands [43]. Indeed, in healthy human subjects as well as patients, capsaicin has been suggested to have a therapeutic potential alone or in combination with other non-steroidal anti-inflammatory drugs [44], and in a mouse CLP model, capsaicin is shown to relieve the damaging impact of sepsis through TRPV1 activation [44, 45]
MSU, cholesterol, amyloid-β, and ambient particle matter
MSU
A uric acid crystal, monosodium urate (MSU), has emerged as an important factor for both gouty arthritis and immune regulation. This simple crystalline structure appears to activate innate host defense mechanisms in multiple ways and trigger robust inflammation and immune reactions. When MSU enters the cell, MSU further triggers NLRP3 inflammasome activation, but the activation mechanism responsible is still elusive. A number of reports suggested that sensory TRP channels such as TRPV1 and TRPA1 may contribute to this activation process [46, 47]. However, this interesting hypothetical link relies on the intracellular Ca2+ measurements, and whether MSU crystals can directly activate TRPV1 [46] or TRPA1 [47] has not been shown. Considering that MSU crystal acts as an oxidative stress to facilitate ROS production, it may activate TRPA1 and TRPV1 via ROS production. Nevertheless, the fact that TRPV1 and TRPA1 mediate MSU crystal-induced inflammation and pain in experimental models strongly supports their undoubted roles as inflammatory mediators [46–50].
Cholesterol
A high serum level cholesterol (hypercholesterolemia), a risk factor for CV disease, promotes inflammatory responses including TLR signaling, inflammasome activation, and the production of monocytes and neutrophils in bone marrow and spleen [51]. Cholesterol was also shown to have a significant impact on several different types of TRP channel activities [52]. Cellular cholesterol affects arterial reactivity to endothelin-1 (ET-1). In endothelium-denuded caudal artery, cholesterol depletion by methyl-β-cyclodextrin (mβcd) treatment attenuated vasoconstriction to ET-1, with paralleled reduction of store-operated Ca2+ entry via TRPC1 [53]. Similarly, cholesterol-mediated activation was observed for other TRP channels. In TRPC3 expressing HEK cells, application of cholesterol enhanced TRPC3 activity [54]. In prostate cancer cells which endogenously express TRPM7, cholesterol-mediated activation of TRPM7 is important for initiation and/or progression of the cancer [55]
In vascular smooth muscle cells (VSMCs), TRPM3 expression was detected at both mRNA and protein levels. In freshly isolated aorta, constitutively active TRPM3 channel positively modulated the contractile responses independently of L-type calcium channels; elevation of cholesterol suppressed TRPM3 channel activity [56].
These results collectively suggest that an appropriate level of cholesterol may be requisite for normal contractility of arteries, and its excess level may lead to CV diseases as well as makeup of microenvironments propensitive for cancer development.
Amyloid-β
The fibrillar peptide amyloid-β (Aβ) is a main pathogenic factor of Alzheimer’s disease (AD). It has been reported that activation of TRPM2 contributes to Aβ- and oxidative stress-induced striatal cell death in rat striatum [57]. The activation of TRPM2 is thought to occur through direct and indirect pathways. Accumulation of Aβ which increases vascular oxidative stress via mitochondrial dysfunction results in sequential occurrences of DNA damages, poly-ADP-ribose polymerase activation, and ADP-ribose production in ECs, which leads to their dysfunction via TRPM2-mediated intracellular Ca2+ overload [58]. The resultant cerebrovascular dysfunction may accelerate the AD pathogenesis by reducing the cerebral blood and glucose supply, increasing susceptibility to vascular insufficiency, and further promoting Aβ accumulation [59]. The other oxidative stress-sensitive TRP channels such as TRPV1, TRPV4, and TRPC1 are also implicated in Aβ-induced damages of other cell types including glia [60–63], smooth muscle cells [64], and ECs [65].
Ambient particle matter
Exposure to ambient particulate matters (PMs) is a significant risk factor to increase respiratory and cardiopulmonary morbidity and mortality, but the mechanism underlying remains largely unknown. In addition to the implications of sensory nerve TRPV1 and TRPA1 in airway hypersensitivity and inflammation which involve environmental noxious stimuli [66], there is evidence that PM acts as a proinflammatory agent to the endothelium and increases vascular permeability in vitro and in vivo via ROS generation. This suggests the possibility that oxidative stress-sensitive TRP channels may be involved in PM-mediated pathophysiology. Indeed, TRPM2, TRPV1, TRPV4, and TRPA1 have been implicated in cellular and tissue damages caused by PM-mediated oxidative stresses associated with diesel exhaust, wood smoke, and other concentrated ambient particles [67–75].
Autophagy and lysosomal function
Autophagy is a highly evolutionarily conserved catabolic process to degrade and recycle cytoplasmic contents via a lysosomal route for reuse in downstream metabolism. It becomes increasingly clear that insufficiency of autophagy is an important pathogenic mechanism for inflammatory diseases [76]. Recently, a possible link between autophagy deficiency and increased inflammasome activation was suggested. The mechanism proposed includes the following causal sequence of cellular events: inefficient mitophagy, accumulation of damaged mitochondria, increased ROS production, and ROS-mediated inflammasome activation which occurs either directly or indirectly via DNA damage and secondary inflammatory signaling(s). Autophagy deficiency also reduces the efficiency of lysosomal degradation and thereby facilitates the accumulation of intra-lysosomal lipids and cholesterol crystals. This then leads to lysosomal membrane destabilization, lysosomal leakage, and inflammasome activation [77]. A similar consequence of autophagy deficiency can be expected for inefficient lysosomal degradation of damaged organelles and proteins. Therefore, normal function of the autophagy system is indispensable for keeping the cell healthy.
TRPML1 is an important player in endosomal sorting and transporting processes at the late endocytotic phase, specifically the formation of late endosome-lysosome hybrid vesicles [78–81]. In other words, the role of this channel is to control the delivery of cellular materials to lysosomes, an essential process of autophagy [82–84]. Altered activity of TRPML1 has been implicated in lysosomal dysfunction and impaired autophagy associated with AD-linked presenilin-1 mutations. In this pathological state, disrupted lysosomal acidification due to defective vesicular ATPase activity are thought to be primarily responsible for lysosomal and autophagy deficits, but concurrently, abnormal cytosolic Ca2+ elevation occurs via facilitated Ca2+ efflux through TRPML1 channel. However, correcting this abnormal Ca2+ homeostasis alone is not sufficient to restore normal lysosomal proteolytic and autophagic activities, thus suggesting that TRPML1 may play a permissive role in this process [85]. In this regard, it may deserve to mention that in humans, mutations in the gene encoding TRPML1 channel (MCOLN1) are the cause of the neurodegenerative disorder mucolipidosis type IV (MLIV) [86].
TRPML3 is a novel Ca2+ channel that plays a crucial role in the regulation of cargo trafficking along the endosomal [87, 88] and autophagosomal maturation [89] pathways. In infected bladder epithelial cells (BECs), TRPML3 triggers a non-lytic expulsion of bacteria (which is a powerful cell-autonomous defense strategy) to rapidly reduce infectious burden. This lysosomal channel is capable of sensing uropathogenic Escherichia coli-mediated lysosome neutralization and, in turn, releasing Ca2+, thereby triggering lysosomal exocytosis to expel the bacteria.[90]
The full-length form of TRPM2 channel (TRPM2-L) has a short splice variant consisting of only the N terminus and the first two transmembrane segments and lacking a pore domain (TRPM2-S). In expression system, coexpression of TRPM2-S suppressed oxidant-induced Ca2+ entry through TRPM2-L and subsequent cell death, presumably through a negative physical interaction [91]. Although its pathophysiological significance had been unclear, a recent study has revealed an interesting connection of this short variant (TRPM2-S) to autophagy. Mitochondrial homeostasis is dynamically regulated by the processes of autophagy/mitophagy and mitochondrial biogenesis. As compared with tumor cells expressing TRPM2-L isoform abundantly, those expressing TRPM2-S showed the accumulation of damaged mitochondrial DNAs with increased levels of unremoved heat shock protein 60 (Hsp60) and a mitochondrial protein translocase of outer membrane 20 (Tom20) in mitochondria. These results are interpreted to suggest that oxidant-induced Ca2+ entry mediated by TRPM2 may be crucial to maintain normal autophagy/mitophagy activity [92].
Oxidative stress induces pleiotropic responses ranging from cell survival to death. A recent study has given an interesting explanation about these differential cell fates, i.e., involvement of distinct poly(ADP-ribose) polymerase (PARP) isoforms (PARP1, PARP2) and distinctive cellular localization of TRPM2 channel. PARPs are enzymes producing poly(ADP-ribose) and, in conjunction with poly(ADP-ribose) glyocohydorase, capable of activating TRPM2 channel via immediate conversion of poly(ADP-ribose) into monomeric ADP-ribose. Under moderate oxidative stress conditions (5 mM H2O2), plasma membrane TRPM2 is under the control of PARP1, activation of which leads to the phosphorylation of p38, SAPK/JNK, and cAMP response element-binding protein (CREB)/ATF-1. This ultimately induces autophagy, thereby allowing cell survival. In contrast, high oxidative stress (10 mM H2O2) triggers late autophagy steps and PARP2 activation, leading to cell death with the activation of lysosomal TRPM2 channel [93].
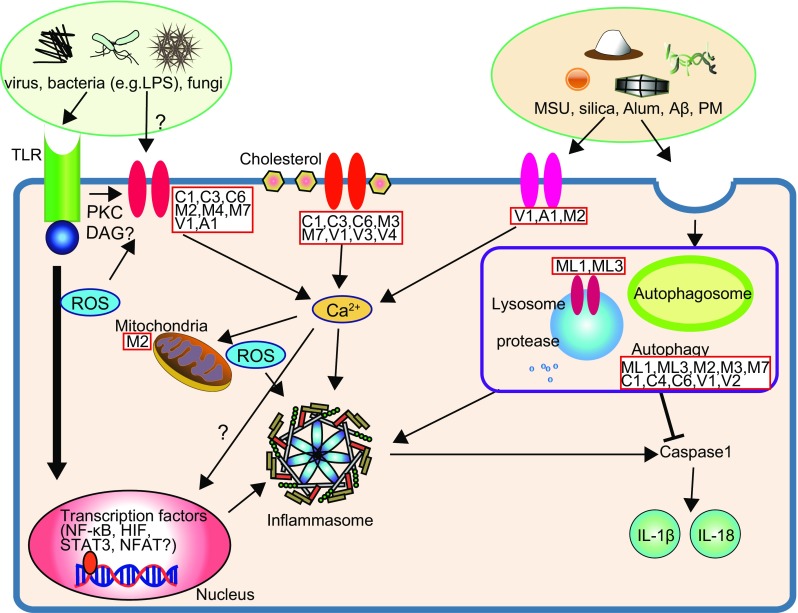
TRP channels may link to persistent activation of inflammasome (see Fig. 2)
Fig. 2.
Possible link of TRP channels to persistent inflammasome activation. Inflammation are mediated by signal transduction from both inflammation-related receptors and stress-sensing TRP channels to transcription factors. The “Receptor” pathway is activated via alteration of internal or external environmental factors in affected cells, including abnormal upregulation or persistent activation of receptors (e.g., cytokine receptors, growth factor receptors, Toll-like receptors) with increased kinase activity, excessive ROS production, and intracellular Ca2+ perturbation. The “TRP” pathway can also be activated by alteration of internal or external environmental factors and is susceptible to the regulations at functional and expression levels. Importantly, both pathways may intersect to modulate each other, since many of the environmental factors associated with inflammation are physical and chemical cell-stressing stimuli. Besides being involved in proliferation, survival, migration, and differentiation, transcription factors can induce the expression of many proinflammatory cytokines and other inflammatory mediators. Importantly, the receptors for many of these cytokines, chemokines, and mediators can further activate the inflammatory transcription factors, thereby forming autocrine and paracrine feedback loops. This would then result in the continuous amplification and promotion of inflammatory reactions leading to chronic inflammation
The early inflammatory response is absolutely essential for the elimination of pathogens, but the termination of the process is equally an important step. Failure to control inflammation leads to immunopathology, including CV diseases and organ dysfunctions. Over time, this leads to fibrotic or cancerous transformation or chronic inflammation.
There are three aspects in the progression of inflammation with respect to inflammasome activity. The first is the “priming” signal that enhances the gene expression of inflammasome components. The second is the “activation” signal that promotes the assembly of inflammasome components. And the last is the “amplification” signal that drives a feedback signal amplification loop. The NLRP3 inflammasome activates caspase-1, which then promotes maturation and secretion of two potent inflammatory cytokines: IL-1β and IL-18. The NLRP3 inflammasome responds not only to pathogens but also to a variety of “danger signals” released in inflamed tissues including cytokines, tissue degradation products, etc. This leads to the formation of a dangerous positive feedback loop which continuously exacerbates the NLRP3 inflammasome response. Under these pathological conditions, the activation of transcription factors, e.g., NF-κB, nuclear factor of activated T cell (NFAT), STAT3, and HIF-1, by inflammatory cytokines appears crucial for the amplification loop of inflammasomes [94–97]. Therefore, the suppression of this amplification loop is of key importance to effectively eliminate infection by stopping acute inflammation and/or restoring homeostatic regulation.
Concentrations of both extracellular and intracellular Ca2+ can increase at the sites of infection, inflammation, or immune cell activation. It has been shown that increased extracellular calcium could act as a danger signal and an amplifier of inflammation via activation of the G protein-coupled calcium sensing receptor—phosphatidylinositol/Ca2+—NLRP3 inflammasome signaling pathway [98]. Therefore, Ca2+ influx may serve as an important control point for inflammasome activity that needs to be tightly regulated by the host in order to avoid an excessive production of cytokines or overt cell death. Moreover, proinflammatory transcription factors, in particular, Ca2+-dependent ones, may play central roles in this control. In this section, we attempt to summarize the connection between inflammatory transcription factors and TRP channels.
NF-κB
NF-κB consists of a family of transcription factors that play critical roles in inflammation, immunity, cell proliferation, differentiation, and survival [99]. One of the factors known to activate NF-κB is an elevation in [Ca2+]i [100, 101]. There are several papers linking Ca2+-permeable TRP channels to NF-κB-mediated inflammatory reactions; suppression of TRPC1-mediated Ca2+ entry inhibited NF-κB activation, which is associated with immunosuppressive mechanism in helminth infections [34]; pharmacological inhibition of TRPM7 channel suggested its involvement in LPS-induced EC migration via the TLR-NF-κB signaling [37]; endotoxin-induced lung injury involves TLR4-mediated NF-κB activation in a manner dependent on TRPC6-mediated Ca2+ entry [21].
Therapeutic potential of targeting NF-κB has been validated by its decoy treatments in a number of inflammatory CV diseases, including myocarditis, post-stenting coronary restenosis, and coronary hypertophic proliferation [102–104].
STAT3
The STAT3 has a dual role: both transducing signals through the cytoplasm and functioning as a transcription factor in the nucleus. STAT3 can be activated by extrinsic pathways, i.e., environmental factors, such as ultraviolet (UV) radiation, chemical carcinogens, infection, stress, and cigarette smoke, through growth factor, cytokine, Toll-like, adrenergic, and nicotinic receptors, respectively [95]. Persistently activated STAT3 mediates cell proliferation, survival, and invasion during inflammasome activation. Several studies suggest that TRP channels may regulate STAT3 activity.
Receptor-induced phosphorylation of cellular Janus kinase 2 (JAK2) or c-Jun and STAT3 are regulated by TRPC1- and TRPC6-mediated Ca2+ influxes [105–108]. This could cause persistent inflammation, resulting in chronic inflammation with global tissue changes and injury. The Ca2+ transporting activity of TRPM7 is closely associated with the activation of the JAK2/STAT3 and/or Notch signaling pathways, which, in turn, induces ischemic neuronal cell death, metastatic transformation of breast cancer cells or proliferation, migration and invasion of glioma stem cells, and the fingerprints of sustained or chronic inflammation [109–111]. Albeit little evidence, it is tempting to speculate that constitutive Ca2+ permeating activity TRPM7 channel might effectively drive, via Ca2+-dependent activation of STAT3, a feedback cycle of persistent activation of inflammasome toward chronic inflammation. A different line of evidence suggests that TRPV1 activates the STAT3 and NF-κB signaling pathways and thereby facilitates the expression of anti-inflammatory neuropeptides [112]. This hints a unique protective role of TRPV1 against inflammation, which is rarely seen for the other types of TRP channels.
HIF-1
HIFs are transcription factors that respond to changes in available oxygen in the cellular environment. However, a recent research suggests that, in certain pathological settings, HIF induction in normoxia likely causes serious consequences encompassing chronic inflammatory components. Chronic inflammation can be a self-perpetuating process so that it may continuously distort cellular microenvironments as the result of aberrantly active transcription factors. Consequent alterations in growth factors, chemokines, cytokines, and redox balance occur within the cellular milieu that, in turn, provide the axis of growth and survival needed for de novo development of cancer and metastasis [113]. In addition, a recent study suggested that cAMP/PKA/CREB/HIF-1α pathway is important for sustained inflammasome activity [114]. Considering that TRP channels serve as important Ca2+ entry routes associated with cellular stresses, it is possible that abnormal TRP channel activity would damage the intracellular microorganelles and disturb the redox balance. In fact, there are many reports found for the linkage between HIF-1 and TRP channels (e.g., TRPC1 [115–117], TRPC3 [118], TRPC5 [119], TRPC6 [120, 121], TRPM2 [92, 122], and TRPM7 [123]).
NFAT
The calcineurin-NFAT signaling plays a pivotal role in the transcription of cytokine genes and other genes critical for the T cell-mediated adaptive immune responses [124]. However, later studies identified its more ubiquitous roles in other organ systems [125]. For example, an established role of NFAT in the CV system is a hub mediator of hypertrophic signaling. In the heart, both mechanical and neurohormonal stresses activate the calcineurin-NFAT signaling to induce prominent pathological hypertrophy. The members of TRPC subfamily have been implicated in the activation step of this signaling as the stress-sensing Ca2+-permeating channels [126–128]. In blood vessels, therapeutic benefits of an immunosuppressant cyclosporin A is known for transplant vasculopathy, part of which is causally related to the inhibition of calcineurin-NFAT signaling in ECs [129]. In diabetic mice, pharmacological inhibition of NFAT (by A-285222) reduced atherosclerotic lesion by inhibiting cytokine release and adhesion molecule expression [130]. Albeit scanty information, involvement of TRPC members has been suggested for inflammatory responses in renal podocyte injury and structural and functional remodeling after myocardial infarction via activation of the calcineurin-NFAT signaling [131, 132]. There is however little evidence yet obtained that directly links TRP channels to chronic inflammatory diseases (e.g., atherosclerosis) through this signaling pathway.
TRP inflammation relationship in CV diseases
Many CV diseases are tightly associated with inflammatory/immune responses in their pathogenesis. This include a wide range of vascular diseases (endotoxin shock, acute vasculitis, atherosclerosis, post-operative stenosis, allograft vasculopathy), cardiac diseases (cardiac hypertrophy, dilated cardiomyopathy, myocardial infarction or ischemia/reperfusion injury, and myocarditis) [133–142], and several autoimmune diseases in the CV system [8]. In the final section of this review, we will briefly overview what is presently known about some of these CV diseases in terms of TRP channel physiology and pathophysiology (see also Table 1).
Table 1.
Therapeutic potential of TRP channel in cardiovascular disease
| Disease | TRP | The potential benefit for disease (+): positive regulation is good, (−): negative regulation is good |
Ref. |
|---|---|---|---|
| Atherosclerosis | C1 | C1(+): Vascular contractility in cholesterol depletion C1(−): Coronary artery disease in metabolic syndrome |
[53, 143, 144] |
| C3 | C3(−): The size of atherosclerotic lesions | [145, 146] | |
| C3(−): Adhesion of monocyte in coronary artery ECs | |||
| C6 | C6(−): Migration and apoptosis of EC in atherosclerotic arteries (by microRNA-26a) | [147, 148] | |
| C6, V1 | C6(−): V1(−): Lysophosphatidylcholine-induced infiltration of monocyte | [149] | |
| V1 | V1(+): Evodiamine-induced angiogenesis and atherosclerosis V1(+): ox-LDL-induced foam cell formation by inducing autophagy in vascular SMC V1(+): ox-LDL-induced lipid accumulation and TNFα-induced inflammation in macrophages V1(+): Adhesion monocyte and EC |
[150–153] | |
| Neointimal hyperplasia | C1 | C1(−): Remodeling of SM | [154] |
| M2 | M2(−): Remodeling of SM | [155] | |
| Hemorrhagic Shock | C1/C4 | C1/C4(−): Development of vasospasm after subarachnoid hemorrhage | [156] |
| V1 | V1(−): Survival rates in hemorrhagic shock model | [157] | |
| Cardiovasculitis | ND | ||
| Cardiac hypertrophy, dilated cardiomyopathy | C1 | C1(−): Related to cardiac fibrosis in Duchenne muscular dystrophy model mice C1(−): Increasing endothelin-1 vasoconstrictor reactivity through Ca2+/ROS/NFATc3 C1(−): Maladaptive cardiac hypertrophy and failure thorough Ca2+/calcineurin/NFAT pathway C1(−): Development of cardiac hypertrophy through Ca2+/calcineurin/NFAT pathway in hypertension in sleep apnea |
[158–161] |
| C3 | C3(−): Ca2+-dependent production of CaMK II and ROS in dilated cardiomyopathy C3(−): Cardiac hypertrophy via GATA4 and TRPC3 (antagonist: miR-26b) C3(−): Cardiac hypertrophy via a positive feedback mechanism through Ca2+/calcineurin/NFAT signaling |
[162–164] | |
| C3/C6 | C3/C6(−): Hypoxia-induced HIF1α, leading to expression, enhanced Ca2+/calcineurin signals C3/C6(−): Ang II-induced cardiac hypertrophy through Ca2+/calcineurin/NFAT signaling |
[118, 165] | |
| C6 | C6(−): Ca2+/calcineurin/NFAT regulatory loop that drives pathologic cardiac remodeling C6(−): Ang II-induced cardiac hypertrophy C6(−): Development of cardiac hypertrophy through GATA4 and NFATc4 |
[166–168] | |
| V1 | V1(+): Long-term high-salt diet-induced cardiac hypertrophy and fibrosis V1(+): Pressure overload-induced cardiac hypertrophy and fibrosis |
[169, 170] | |
| V2 | V2(−): Ventricular dilation and fibrosis through CaMK II and ROS in DCM patients and three DCM model mice | [171] | |
| M4 | M4(+): Hyperplasia in the cardiac hypertrophy M4(+): Ang II-induced cardiac hypertrophy through Ca2+/calcineurin/NFAT pathway |
[172, 173] | |
| Allograft | ND | ||
| Coronary, myocardial infarction | C3/C4/C6 | C3/C4/C6(−): After MI induce Ca2+/calcineurin/NFAT pathway pathway, activate cardiac hypertrophy, reduces contractility reserve C3/C6(+): MI-induced injury and cardiomyocyte apoptosis are alleviated by BDNF/TrkB axis |
[132, 174] |
| M4 | M4(−): MI cause cell death and decrease β-adrenergic cardiac reserve | [175] | |
| V1 V1 |
V1(+): Post-MI enhances fibrosis and impairs myocardial contractile performance V1(+): Acute myocardial ischemia augments the Bezold–Jarisch reflex |
[176, 177] | |
| V2 | V2(+): M1 macrophage infiltration after MI | [178] | |
| Ischemia reperfusion | V1 | V1(+): Myocardial I/R injury can be protected by 12-lipoxygenase-derived eicosanoids V1(+): PAR2-induced cardiac protection against I/R injury V1(+): Cardiac performance in I/R-injured diabetic heart V1(+): Acute MI |
[179–182] |
| M2 | M2(−): Myocardial I/R injury in neutrophil M2(−): I/R induce TNFα, caspase-8 activation, ROS production, PARP-1 activation, ADP-ribose production, that contribute to cardiomyocyte cell death |
[183, 184] | |
| M4 | M4(−): I/R injury | [185] | |
| Stenosis, systemic lupus erythematosus | C5/C6 | C5/C6(−): Linkage analysis data for infantile hypertrophic pyloric stenosis | [186] |
| Autoimmune, autoantibody | ND | ||
| Hypertension, diabetes | ND |
EC endothelial cell, SMC smooth muscle cell, ox-LDL oxidized low-density lipoprotein, TNFα tumor necrosis factor, I/R ischemia reperfusion, ND no data, Ang II angiotensin II, miR microRNA, ADP adenosine diphosphate, PARP-1 poly[ADP-ribose] polymerase-1, DCM dilated cardiomyopathy, ROS reactive oxygen species, MI myocardial infarction, BDNF brain-derived neurotrophic factor, TrkB tropomyosin receptor kinase B, PAR2 protease-activated receptor-2, NFAT nuclear factor of activated T cells
Atherosclerosis
Atherosclerosis is a progressive inflammatory disease that disintegrates the structure and function of blood vessels through lipid deposition and activation of innate/adaptive immune reactions. There are good evidence to suggest that TRP channels are involved in the respective stages of atherosclerosis. This will be described below, in a stage-by-stage manner.
The main initiation factor for atherosclerosis is the oxidized low-density lipoprotein (ox-LDL), which affects the endothelial surface and thereby induces EC dysfunction. But, other inflammatory components/elements (virus, bacteria, toxins, toxic nutrients and metabolites, ambient particles, autoantibody, heat shock protein [187]; see also above) also promote atherosclerosis. Among TRP channels expressed in the CVS, two reports suggest proatherogenic potential of TRPC6 channel. It is reported that a cardiovascular risk factor, lysophosphatidylcholine (LPC), facilitates TRPC6 translocation to cell membrane causing a rapid Ca2+ influx in EC. This, in turn, induces the externalization of TRPC5, thereby allowing sustained Ca2+ influx through TRPC6/TRPC5 complex. This cascaded TRPC6/TRPC5 activation causes the inhibition of EC migration which is essential for the healing of atherosclerotic arteries [147]. Endothelial expression of microRNA miR-26a is reduced in the aortic intima of atherogenic ApoE (−/−) mice and ox-LDL-treated human ECs, whereas overexpression of miR-26a induces EC apoptosis. miR-26a acts as a negative regulator of TRPC6, activation of which allows Ca2+ influx activating the mitochondrial apoptotic pathway associated with atherosclerosis. Thus, abnormal TRPC6 activity can induce apoptotic EC death, and application of miR-26a may be able to reduce the atherosclerotic lesion [148]. These results provide, albeit indirect, evidence to support non-trivial roles of TRPC6 in the progression of atherosclerosis.
At the site of injury, ECs allow the entry of monocytes and lymphocytes into the vessel wall. In the early stage of this process, the adhesion of monocytes to the endothelial surface is supported by increased intracellular Ca2+ concentration in ECs. When the monocyte contacts EC, Ca2+ influx into EC is activated, which further strengthens the adherence of monocytes. Pharmacological inhibition of TRPV1 reduces the number of adherent monocytes, so that activation of TRPV1-mediated Ca2+ influx likely enables strong adhesion of monocytes to EC. In a similar context, TRPC3-mediated Ca2+ influx has been implicated in ATP-induced expression of vascular cell adhesion molecule-1 (VCAM-1) which is critical to recruit monocytes to EC [145, 150].
After injury, monocytes transmigrate across the damaged endothelium and enter the intimal layer of the vessel wall. Thus, reducing monocyte infiltration is thought to be one of the powerful strategies to attenuate the progression of atherosclerosis. A major atherogenic agent LPC can induce a strong chemotaxis of monocytes which appears to require Ca2+ influx. Pharmacological characterization of LPC-activated Ca2+-permeable currents strongly suggested that activation of both TRPC and TRPV1 is necessary for the optimal chemotaxic activity [149]. In this regard, these two TRP channels could be good molecular targets for anti-atherosclerotic therapy.
The monocytes that have migrated into the intima differentiate into macrophages and uptake ox-LDL. These lipid-laden macrophages are known as foam cells. Although the main foam cells are derived from macrophages, VSMCs can also transform to foam cells. Interestingly, activation of TRPV1 by capsaicin impedes the transformation of ox-LDL-treated VSMCs to foam cells by rescuing otherwise impaired autophagy by ox-LDL [151]. Moreover, TRPV1 activation protected macrophages from ox-LDL-induced lipid accumulation and TNFα-induced inflammation. These results indicate that activation of TRPV1 by capsaicin is another effective strategy to inhibit atherosclerosis.
After transformation, foam cells start to produce inflammatory cytokines. The released inflammatory cytokines trigger further transformation of VSMCs which gain the ability to migrate from the medial to intimal layer. These inflammatory responses make atherosclerotic plaques through necrosis and apoptosis, completing the clinical picture of atherosclerosis. In cultured RAW264 macrophages, LPS-induced production of cytokines (TNFα, IL-6) was shown to depend on TRPV2-mediated Ca2+ influx. Thus, in this late stage of atherosclerosis, targeting TRPV2 may be another novel strategy to suppress inflammatory cytokine production and thus formation of atherosclerotic lesions [188].
Vascular stenosis after bypass surgery and angioplasty
Bypass surgery and angioplasty with stenting often causes the vascular injury. Injured VSMCs then undergo transformation from quiescent and contractile to invasive and proliferative states. Such phenotype switching is an important process to recover vascular contractility but can also be part of the cause of occlusive vascular diseases including atherosclerosis and adverse responses accompanying neointimal hyperplasia. Several lines of evidence suggest that excessive (constitutively active) TRPC1 and (ROS-induced) TRPM2 activities in VSMCs are involved in the neointimal hyperplasia induced after vascular cuff injury in rat and mouse models, respectively. These changes were accompanied by enhanced cell cycle activity and inhibited by specific antibodies raised against the third extracellular loop of TRPC1 or TRPM2 channel (E3 antibodies). Similar increased expression of TRPC1 was also observed in the intimal layer of human vein graft samples. Thus, these channels may be novel therapeutic targets for occlusive vascular diseases [154, 155].
Cardiac hypertrophy, dilated cardiomyopathy
In cardiomyocytes, Ca2+ transients convey information to both contraction and gene transcription. Changes of cytoplasmic Ca2+ in cardiomyocytes are controlled by a variety of ion channels, the Na+/Ca2+ exchanger, Ca2+ pumps, and Ca2+-binding proteins. Several recent studies using animal models have implicated TRP channels in the development of hypertrophy. It has been shown that hypertrophic agonists upregulate the expression of TRPC1, TRPC3, and TRPC6 channels in cardiac myocytes, leading to activation of the Ca2+-(and ROS)–calmodulin–calcineurin-NFAT pathway which eventually results in cardiac hypertrophy. These hypertrophic changes are a pathological process basically involving inflammatory reactions [136, 189] and ultimately reduce the cardiac function increasing the mortality of experimental animals [118, 158–168].
More recent studies have added a new connection of TRP channels (TRPV2 and TRPM4) to cardiomyopathy. In the patients of cardiomyopathy as well as in its genetic and chemically induced animal models which typically show ventricular dilation, fibrosis, and severely compromised heart function, the expression of TRPV2 was found to be concentrated on the ventricular sarcolemma. Specific abrogation of TRPV2 activity by either overexpression of the amino-terminal domain of TRPV2 (amino acids 1–387) or treatment with chemical inhibitors ameliorated these pathological changes and the contractile function of the heart and improved the survival of the affected animals [171]. Since the excessive activity of TRPV2 was associated with increased production of ROS and phosphorylation of Ca2+/calmodulin-dependent protein kinase II (CaMK II), participation of inflammatory process is strongly suggested for these pathological changes. Thus, targeting TRPV2 may become a new clinical option to treat cardiomyopathy-associated heart failure.
In addition, a recent gene invalidation study showed that the activity of TRPM4 may be a prerequisite to preventing the development of eccentric ventricular hypertrophy of the heart. Indeed, TRPM4 has been shown to negatively regulate angiotensin II-induced cardiac hypertrophy owing its membrane depolarizing ability whereby the magnitude of store-operated Ca2+ entry which activates the calcineurin-NFAT hypertrophic pathway is negatively controlled [172, 173]. The correlation of these findings with inflammation is however unclear, since immunohistological examination revealed no obvious sign of fibrosis or hypertrophy but rather hyperplasia of smaller sized cardiomyocytes compared with normal ones.
Myocardial infarction (MI)
In infarcted myocardium, necrotic cardiomyocytes release danger signals, activating an intense inflammatory response, by which complex cellular processes associated with injury, repair, and remodeling of the infarcted regions are activated [141]. In the MI period of animal models and human patients, the plasma level of brain-derived neurotrophic factor (BDNF) was found elevated along with tropomyosin-related kinase B (TrkB) and its downstream effector TRPC3 and TRPC6 channels. After BDNF treatment, the infarct size was markedly reduced and cardiac contractility was significantly restored, which seemed to be associated with decreased apoptotic response of cardiomyocytes. Since these beneficial effects of BDNF were reversed by pharmacological or functional inhibition of TRPC3/TRPC6 channels, these channels likely play a protective role against detrimental cardiac remodeling after MI [132, 174]. In a puzzling contrast, however, adenovirus-mediated overexpression of TRPC3/TRPC4/TRPC6 was reported to induce a hypertrophic response via the NFAT-mediated signaling in adult feline cardiomyocytes and accompany reduction of the contractility and catecholamine response due to increased spontaneous Ca2+ leak from the SR. In the same study, mice treated with MI procedures showed similarly enhanced TRPC1, TRPC3, TRPC4, and TRPC6 expression and Ca2+ channel activity along with induction of hypertrophic genes. These two lines of evidence have been interpreted to indicate the benefits of blocking the TRPC channels that improve post-MI structural remodeling and dysfunction. It is a matter of further investigation of what differences in experimental settings would make such disparate consequences of TRPC channel activation in the post-MI recovery.
In sharp contrast with a protective role of TRPM4 against dilated cardiomyopathy (see above), the deletion of the trpm4 gene in mice rather improved survival and β-adrenergic cardiac reserve after experimentally induced ischemic heart failure [175, 185]. In addition, several lines of evidence support the ameliorative role of TRPV1 in myocardial infarction as found in atherosclerosis [176, 177, 179–182].
Ischemia/reperfusion injury
Reperfusion of the ischemic myocardium is essential for rescuing it from the death. However, reperfusion itself causes additional myocardial injury termed “ischemia/reperfusion (I/R) injury” [190]. I/R injury in the heart occurs through innate immune responses involving TLR (TLR2, TLR4) and the Myd88- and Trif-dependent NF-κB-interferon-3 pathway, activation of which induces the release of proinflammatory and immunomodulatory cytokines [142]. Moreover, oxidative stress-induced acute inflammatory response is implicated in the development of I/R injury [191].
There are two conflicting reports linking TRPM2 channel to I/R injury. One study suggested that activation of neutrophil TRPM2 channel by ROS exacerbated myocardial I/R injury by upregulating the expression of endothelial adhesion molecules MAC-1 and LFA-1. This then resulted in a stronger adhesion of neutrophils on the coronary EC surface. Neutrophil accumulation in the myocardium is a key process that induces myocardial injury [191]. Thus, specific inhibition of neutrophil TRPM2 activity may serve as an effective means to mitigate the exacerbation of myocardial infarction. However, in a striking contrast to this view, an independent study proposed an opposing and more complex hypothesis. According to the findings of this study, genetic deletion of TRPM2 exacerbated the extent of myocardial dysfunction after I/R injury via increased generation (upregulation of NADPH oxidase) and decreased scavenging capacity (downregulation of superoxide anion disulmutases) of ROS. As pointed out by the authors themselves, the discrepancies between the above two studies may reflect small but essential differences in experimental designs, as well as the use of global knockout mice with different exon-targeting invalidation strategies [122]. In any case, it is almost undoubted that TRPM2 channel is among central players in immunoinflammatory reactions in the cardiovascular disease and thus a promising therapeutic target.
Concluding remarks and perspectives
In this review, we summarized the current knowledge linking inflammation and TRP channels and attempted to provide new insights into the pathogenesis of various inflammatory CV diseases (refer to Table 1). In addition, we described the evidence that dysregulation or altered expression of TRP channels are in close association with inflammasome activation and the pathogenesis of CV diseases. Our major but tentative conclusions drawn from this review writing are as follows: TRPC1, TRPC3, TRPC6, and TRPM7 may be the most promising therapeutic targets in the subacute or chronic stages of some CV diseases (i.e., remodeling, proliferation), presumably via inhibition of persistent inflammasome activation as well as aberrant regulation of cytokine production and transcription factor activity. In case of ischemia/reperfusion, the molecules’ sensing/transducing oxidative stress appears contributory to the initiation of inflammation, wherein TRPM2 channel is the most plausible candidate (although roles of other oxidative stress-sensitive channels TRPV1, TRPM7, TRPA1, TRPC1, TRPC3, and TRPC6 should not be underestimated). Finally, dietary capsaicin, which appears to act as both sensory nerve (e.g., CLP sepsis model) and VSMC (e.g., atherosclerosis), TRPV1 activators, may have broad relevance to improving CV disorders through its anti-inflammatory actions.
The current research on the immunopathophysiology of TRP channels is still in its infant stage. It is thus strongly anticipated that further extensive investigations will greatly improve our yet premature understanding about it, which will pave a way to developing new effective therapies for inflammatory CV diseases.
Acknowledgments
This work has been in part supported by grants-in-aid from the Ministry of Science, Education, and Culture, Japan, to T.N. (No. 15K08197) and R.I. (No. 22136008; for Scientific Research on Innovative Areas).
Conflict of interest
None.
Footnotes
This submission is related to Role of TRP Ion Channels in Physiology and Pathology - Dr. Armen Akopian
Contributor Information
Tomohiro Numata, Phone: 81-92-801-1011, Email: numata@fukuoka-u.ac.jp.
Ryuji Inoue, Phone: 81-92-801-1011, Email: inouery@fukuoka-u.ac.jp.
References
- 1.Tousoulis D, Psarros C, Demosthenous M, Patel R, Antoniades C, Stefanadis C. Innate and adaptive inflammation as a therapeutic target in vascular disease: the emerging role of statins. J Am Coll Cardiol. 2014;63(23):2491–2502. doi: 10.1016/j.jacc.2014.01.054. [DOI] [PubMed] [Google Scholar]
- 2.Virdis A, Schiffrin EL. Vascular inflammation: a role in vascular disease in hypertension? Curr Opin Nephrol Hypertens. 2003;12(2):181–187. doi: 10.1097/00041552-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Golia E, Limongelli G, Natale F, Fimiani F, Maddaloni V, Pariggiano I, Bianchi R, Crisci M, D’Acierno L, Giordano R, Di Palma G, Conte M, Golino P, Russo MG, Calabro R, Calabro P. Inflammation and cardiovascular disease: from pathogenesis to therapeutic target. Curr Atheroscler Rep. 2014;16(9):435. doi: 10.1007/s11883-014-0435-z. [DOI] [PubMed] [Google Scholar]
- 4.Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 1999;340(2):115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 5.Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993;362(6423):801–809. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- 6.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 7.Masumoto J, Taniguchi S, Ayukawa K, Sarvotham H, Kishino T, Niikawa N, Hidaka E, Katsuyama T, Higuchi T, Sagara J. ASC, a novel 22-kDa protein, aggregates during apoptosis of human promyelocytic leukemia HL-60 cells. J biol Chem. 1999;274(48):33835–33838. doi: 10.1074/jbc.274.48.33835. [DOI] [PubMed] [Google Scholar]
- 8.Broderick L, De Nardo D, Franklin BS, Hoffman HM, Latz E. The inflammasomes and autoinflammatory syndromes. Annu Rev Pathol. 2015;10:395–424. doi: 10.1146/annurev-pathol-012414-040431. [DOI] [PubMed] [Google Scholar]
- 9.Yin Y, Pastrana JL, Li X, Huang X, Mallilankaraman K, Choi ET, Madesh M, Wang H, Yang XF. Inflammasomes: sensors of metabolic stresses for vascular inflammation. Front Biosci (Landmark edition) 2013;18:638–649. doi: 10.2741/4127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abais JM, Xia M, Zhang Y, Boini KM, Li PL. Redox regulation of NLRP3 inflammasomes: ROS as trigger or effector? Antioxid Redox Signal. 2015;22(13):1111–1129. doi: 10.1089/ars.2014.5994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Latz E, Xiao TS, Stutz A. Activation and regulation of the inflammasomes. Nat Rev Immunol. 2013;13(6):397–411. doi: 10.1038/nri3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feske S. Calcium signalling in lymphocyte activation and disease. Nat Rev Immunol. 2007;7(9):690–702. doi: 10.1038/nri2152. [DOI] [PubMed] [Google Scholar]
- 13.Jones JD, Dangl JL. The plant immune system. Nature. 2006;444(7117):323–329. doi: 10.1038/nature05286. [DOI] [PubMed] [Google Scholar]
- 14.Janeway CA, Jr, Medzhitov R. Innate immune recognition. Annu Rev Immunol. 2002;20:197–216. doi: 10.1146/annurev.immunol.20.083001.084359. [DOI] [PubMed] [Google Scholar]
- 15.Seong SY, Matzinger P. Hydrophobicity: an ancient damage-associated molecular pattern that initiates innate immune responses. Nat Rev Immunol. 2004;4(6):469–478. doi: 10.1038/nri1372. [DOI] [PubMed] [Google Scholar]
- 16.Ong PY, Ohtake T, Brandt C, Strickland I, Boguniewicz M, Ganz T, Gallo RL, Leung DY. Endogenous antimicrobial peptides and skin infections in atopic dermatitis. N Engl J Med. 2002;347(15):1151–1160. doi: 10.1056/NEJMoa021481. [DOI] [PubMed] [Google Scholar]
- 17.de Kleijn D, Pasterkamp G. Toll-like receptors in cardiovascular diseases. Cardiovasc Res. 2003;60(1):58–67. doi: 10.1016/s0008-6363(03)00348-1. [DOI] [PubMed] [Google Scholar]
- 18.Strowig T, Henao-Mejia J, Elinav E, Flavell R. Inflammasomes in health and disease. Nature. 2012;481(7381):278–286. doi: 10.1038/nature10759. [DOI] [PubMed] [Google Scholar]
- 19.Santoni G, Cardinali C, Morelli MB, Santoni M, Nabissi M, Amantini C. Danger- and pathogen-associated molecular patterns recognition by pattern-recognition receptors and ion channels of the transient receptor potential family triggers the inflammasome activation in immune cells and sensory neurons. J Neuroinflammation. 2015;12:21. doi: 10.1186/s12974-015-0239-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meseguer V, Alpizar YA, Luis E, Tajada S, Denlinger B, Fajardo O, Manenschijn JA, Fernandez-Pena C, Talavera A, Kichko T, Navia B, Sanchez A, Senaris R, Reeh P, Perez-Garcia MT, Lopez-Lopez JR, Voets T, Belmonte C, Talavera K, Viana F. TRPA1 channels mediate acute neurogenic inflammation and pain produced by bacterial endotoxins. Nat Commun. 2014;5:3125. doi: 10.1038/ncomms4125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tauseef M, Knezevic N, Chava KR, Smith M, Sukriti S, Gianaris N, Obukhov AG, Vogel SM, Schraufnagel DE, Dietrich A, Birnbaumer L, Malik AB, Mehta D. TLR4 activation of TRPC6-dependent calcium signaling mediates endotoxin-induced lung vascular permeability and inflammation. J Exp Med. 2012;209(11):1953–1968. doi: 10.1084/jem.20111355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Becerra A, Echeverria C, Varela D, Sarmiento D, Armisen R, Nunez-Villena F, Montecinos M, Simon F. Transient receptor potential melastatin 4 inhibition prevents lipopolysaccharide-induced endothelial cell death. Cardiovasc Res. 2011;91(4):677–684. doi: 10.1093/cvr/cvr135. [DOI] [PubMed] [Google Scholar]
- 23.Echeverria C, Montorfano I, Hermosilla T, Armisen R, Velasquez LA, Cabello-Verrugio C, Varela D, Simon F. Endotoxin induces fibrosis in vascular endothelial cells through a mechanism dependent on transient receptor protein melastatin 7 activity. PLoS One. 2014;9(4) doi: 10.1371/journal.pone.0094146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Assas BM, Miyan JA, Pennock JL. Cross-talk between neural and immune receptors provides a potential mechanism of homeostatic regulation in the gut mucosa. Mucosal Immunol. 2014;7(6):1283–1289. doi: 10.1038/mi.2014.80. [DOI] [PubMed] [Google Scholar]
- 25.Numata T, Kiyonaka S, Kato K, Takahashi N, Mori Y (2011) Activation of TRP Channels in Mammalian Systems. In: Zhu MX (ed) TRP Channels. CRC Press LLc., Boca Raton (FL) [PubMed]
- 26.Ramsey IS, Delling M, Clapham DE. An introduction to TRP channels. Annu Rev Physiol. 2006;68:619–647. doi: 10.1146/annurev.physiol.68.040204.100431. [DOI] [PubMed] [Google Scholar]
- 27.Nilius B, Owsianik G, Voets T, Peters JA. Transient receptor potential cation channels in disease. Physiol Rev. 2007;87(1):165–217. doi: 10.1152/physrev.00021.2006. [DOI] [PubMed] [Google Scholar]
- 28.Clapham DE, Montell C, Schultz G, Julius D. International Union of Pharmacology. XLIII. Compendium of voltage-gated ion channels: transient receptor potential channels. Pharmacol Rev. 2003;55(4):591–596. doi: 10.1124/pr.55.4.6. [DOI] [PubMed] [Google Scholar]
- 29.Owsianik G, Talavera K, Voets T, Nilius B. Permeation and selectivity of TRP channels. Annu Rev Physiol. 2006;68:685–717. doi: 10.1146/annurev.physiol.68.040204.101406. [DOI] [PubMed] [Google Scholar]
- 30.Ulasli M, Gurses SA, Bayraktar R, Yumrutas O, Oztuzcu S, Igci M, Igci YZ, Cakmak EA, Arslan A. The effects of Nigella sativa (Ns), Anthemis hyalina (Ah) and Citrus sinensis (Cs) extracts on the replication of coronavirus and the expression of TRP genes family. Mol Biol Rep. 2014;41(3):1703–1711. doi: 10.1007/s11033-014-3019-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abdullah H, Heaney LG, Cosby SL, McGarvey LP. Rhinovirus upregulates transient receptor potential channels in a human neuronal cell line: implications for respiratory virus-induced cough reflex sensitivity. Thorax. 2014;69(1):46–54. doi: 10.1136/thoraxjnl-2013-203894. [DOI] [PubMed] [Google Scholar]
- 32.Zhou X, Ye Y, Sun Y, Li X, Wang W, Privratsky B, Tan S, Zhou Z, Huang C, Wei YQ, Birnbaumer L, Singh BB, Wu M. Transient Receptor Potential Channel 1 Deficiency Impairs Host Defense and Proinflammatory Responses to Bacterial Infection by Regulating Protein Kinase Calpha Signaling. Mol Cell Biol. 2015;35(16):2729–2739. doi: 10.1128/MCB.00256-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sun CK, Zhen YY, Lu HI, Sung PH, Chang LT, Tsai TH, Sheu JJ, Chen YL, Chua S, Chang HW, Chen YL, Lee FY, Yip HK. Reducing TRPC1 Expression through Liposome-Mediated siRNA Delivery Markedly Attenuates Hypoxia-Induced Pulmonary Arterial Hypertension in a Murine Model. Stem Cells Int. 2014;2014:316214. doi: 10.1155/2014/316214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chauhan A, Sun Y, Pani B, Quenumzangbe F, Sharma J, Singh BB, Mishra BB. Helminth induced suppression of macrophage activation is correlated with inhibition of calcium channel activity. PLoS One. 2014;9(7) doi: 10.1371/journal.pone.0101023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Py BF, Jin M, Desai BN, Penumaka A, Zhu H, Kober M, Dietrich A, Lipinski MM, Henry T, Clapham DE, Yuan J. Caspase-11 controls interleukin-1beta release through degradation of TRPC1. Cell Rep. 2014;6(6):1122–1128. doi: 10.1016/j.celrep.2014.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vohra PK, Thompson MA, Sathish V, Kiel A, Jerde C, Pabelick CM, Singh BB, Prakash YS. TRPC3 regulates release of brain-derived neurotrophic factor from human airway smooth muscle. Biochim Biophys Acta. 2013;1833(12):2953–2960. doi: 10.1016/j.bbamcr.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sarmiento D, Montorfano I, Caceres M, Echeverria C, Fernandez R, Cabello-Verrugio C, Cerda O, Tapia P, Simon F. Endotoxin-induced vascular endothelial cell migration is dependent on TLR4/NF-kappaB pathway, NAD(P)H oxidase activation, and transient receptor potential melastatin 7 calcium channel activity. Int J Biochem Cell Biol. 2014;55:11–23. doi: 10.1016/j.biocel.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 38.Knowles H, Heizer JW, Li Y, Chapman K, Ogden CA, Andreasen K, Shapland E, Kucera G, Mogan J, Humann J, Lenz LL, Morrison AD, Perraud AL. Transient Receptor Potential Melastatin 2 (TRPM2) ion channel is required for innate immunity against Listeria monocytogenes. Proc Natl Acad Sci U S A. 2011;108(28):11578–11583. doi: 10.1073/pnas.1010678108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Qian X, Numata T, Zhang K, Li C, Hou J, Mori Y, Fang X. Transient receptor potential melastatin 2 protects mice against polymicrobial sepsis by enhancing bacterial clearance. Anesthesiology. 2014;121(2):336–351. doi: 10.1097/ALN.0000000000000275. [DOI] [PubMed] [Google Scholar]
- 40.Hwang SW, Kim N, Jung HK, Park JH, Choi YJ, Kim H, Kim J, Kim JS, Jung HC. Association of SLC6A4 5-HTTLPR and TRPV1 945G>C with functional dyspepsia in Korea. J Gastroenterol Hepatol. 2014;29(10):1770–1777. doi: 10.1111/jgh.12596. [DOI] [PubMed] [Google Scholar]
- 41.Guptill V, Cui X, Khaibullina A, Keller JM, Spornick N, Mannes A, Iadarola M, Quezado ZM. Disruption of the transient receptor potential vanilloid 1 can affect survival, bacterial clearance, and cytokine gene expression during murine sepsis. Anesthesiology. 2011;114(5):1190–1199. doi: 10.1097/ALN.0b013e318212515b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wanner SP, Garami A, Pakai E, Oliveira DL, Gavva NR, Coimbra CC, Romanovsky AA. Aging reverses the role of the transient receptor potential vanilloid-1 channel in systemic inflammation from anti-inflammatory to proinflammatory. Cell Cycle (Georgetown, Tex) 2012;11(2):343–349. doi: 10.4161/cc.11.2.18772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shin YH, Namkoong E, Choi S, Bae JS, Jin M, Hwang SM, Arote R, Choi SY, Park K. Capsaicin regulates the NF-kappaB pathway in salivary gland inflammation. J Dent Res. 2013;92(6):547–552. doi: 10.1177/0022034513487376. [DOI] [PubMed] [Google Scholar]
- 44.Mozsik G. Capsaicin as new orally applicable gastroprotective and therapeutic drug alone or in combination with nonsteroidal anti-inflammatory drugs in healthy human subjects and in patients. Prog Drug Res Fortschr Der Arzneimittelforschung Prog Des Rech Pharm. 2014;68:209–258. doi: 10.1007/978-3-0348-0828-6_9. [DOI] [PubMed] [Google Scholar]
- 45.Fernandes ES, Liang L, Smillie SJ, Kaiser F, Purcell R, Rivett DW, Alam S, Howat S, Collins H, Thompson SJ, Keeble JE, Riffo-Vasquez Y, Bruce KD, Brain SD. TRPV1 deletion enhances local inflammation and accelerates the onset of systemic inflammatory response syndrome. J Immunol. 2012;188(11):5741–5751. doi: 10.4049/jimmunol.1102147. [DOI] [PubMed] [Google Scholar]
- 46.Hoffmeister C, Trevisan G, Rossato MF, de Oliveira SM, Gomez MV, Ferreira J. Role of TRPV1 in nociception and edema induced by monosodium urate crystals in rats. Pain. 2011;152(8):1777–1788. doi: 10.1016/j.pain.2011.03.025. [DOI] [PubMed] [Google Scholar]
- 47.Moilanen LJ, Hamalainen M, Lehtimaki L, Nieminen RM, Moilanen E. Urate crystal induced inflammation and joint pain are reduced in transient receptor potential ankyrin 1 deficient mice--potential role for transient receptor potential ankyrin 1 in gout. PLoS One. 2015;10(2) doi: 10.1371/journal.pone.0117770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Trevisan G, Hoffmeister C, Rossato MF, Oliveira SM, Silva MA, Ineu RP, Guerra GP, Materazzi S, Fusi C, Nassini R, Geppetti P, Ferreira J. Transient receptor potential ankyrin 1 receptor stimulation by hydrogen peroxide is critical to trigger pain during monosodium urate-induced inflammation in rodents. Arthritis Rheum. 2013;65(11):2984–2995. doi: 10.1002/art.38112. [DOI] [PubMed] [Google Scholar]
- 49.Trevisan G, Hoffmeister C, Rossato MF, Oliveira SM, Silva MA, Silva CR, Fusi C, Tonello R, Minocci D, Guerra GP, Materazzi S, Nassini R, Geppetti P, Ferreira J. TRPA1 receptor stimulation by hydrogen peroxide is critical to trigger hyperalgesia and inflammation in a model of acute gout. Free Radic Biol Med. 2014;72:200–209. doi: 10.1016/j.freeradbiomed.2014.04.021. [DOI] [PubMed] [Google Scholar]
- 50.Hoffmeister C, Silva MA, Rossato MF, Trevisan G, Oliveira SM, Guerra GP, Silva CR, Ferreira J. Participation of the TRPV1 receptor in the development of acute gout attacks. Rheumatol (Oxford, England) 2014;53(2):240–249. doi: 10.1093/rheumatology/ket352. [DOI] [PubMed] [Google Scholar]
- 51.Tall AR, Yvan-Charvet L. Cholesterol, inflammation and innate immunity. Nat Rev Immunol. 2015;15(2):104–116. doi: 10.1038/nri3793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosenhouse-Dantsker A, Mehta D, Levitan I. Regulation of ion channels by membrane lipids. Compr Physiol. 2012;2(1):31–68. doi: 10.1002/cphy.c110001. [DOI] [PubMed] [Google Scholar]
- 53.Bergdahl A, Gomez MF, Dreja K, Xu SZ, Adner M, Beech DJ, Broman J, Hellstrand P, Sward K. Cholesterol depletion impairs vascular reactivity to endothelin-1 by reducing store-operated Ca2+ entry dependent on TRPC1. Circ Res. 2003;93(9):839–847. doi: 10.1161/01.RES.0000100367.45446.A3. [DOI] [PubMed] [Google Scholar]
- 54.Graziani A, Rosker C, Kohlwein SD, Zhu MX, Romanin C, Sattler W, Groschner K, Poteser M. Cellular cholesterol controls TRPC3 function: evidence from a novel dominant-negative knockdown strategy. Biochem J. 2006;396(1):147–155. doi: 10.1042/BJ20051246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun Y, Sukumaran P, Varma A, Derry S, Sahmoun AE, Singh BB. Cholesterol-induced activation of TRPM7 regulates cell proliferation, migration, and viability of human prostate cells. Biochim Biophys Acta. 2014;1843(9):1839–1850. doi: 10.1016/j.bbamcr.2014.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Naylor J, Li J, Milligan CJ, Zeng F, Sukumar P, Hou B, Sedo A, Yuldasheva N, Majeed Y, Beri D, Jiang S, Seymour VA, McKeown L, Kumar B, Harteneck C, O’Regan D, Wheatcroft SB, Kearney MT, Jones C, Porter KE, Beech DJ. Pregnenolone sulphate- and cholesterol-regulated TRPM3 channels coupled to vascular smooth muscle secretion and contraction. Circ Res. 2010;106(9):1507–1515. doi: 10.1161/CIRCRESAHA.110.219329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fonfria E, Marshall IC, Boyfield I, Skaper SD, Hughes JP, Owen DE, Zhang W, Miller BA, Benham CD, McNulty S. Amyloid beta-peptide(1–42) and hydrogen peroxide-induced toxicity are mediated by TRPM2 in rat primary striatal cultures. J Neurochem. 2005;95(3):715–723. doi: 10.1111/j.1471-4159.2005.03396.x. [DOI] [PubMed] [Google Scholar]
- 58.Park L, Wang G, Moore J, Girouard H, Zhou P, Anrather J, Iadecola C. The key role of transient receptor potential melastatin-2 channels in amyloid-beta-induced neurovascular dysfunction. Nat Commun. 2014;5:5318. doi: 10.1038/ncomms6318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Koizumi K, Wang G, Park L. Endothelial Dysfunction and Amyloid-beta-Induced Neurovascular Alterations. Cell Mol Neurobiol. 2015 doi: 10.1007/s10571-015-0256-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schilling T, Eder C. Amyloid-beta-induced reactive oxygen species production and priming are differentially regulated by ion channels in microglia. J Cell Physiol. 2011;226(12):3295–3302. doi: 10.1002/jcp.22675. [DOI] [PubMed] [Google Scholar]
- 61.Ronco V, Grolla AA, Glasnov TN, Canonico PL, Verkhratsky A, Genazzani AA, Lim D. Differential deregulation of astrocytic calcium signalling by amyloid-beta, TNFalpha, IL-1beta and LPS. Cell Calcium. 2014;55(4):219–229. doi: 10.1016/j.ceca.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 62.Bai JZ, Lipski J. Involvement of TRPV4 channels in Abeta(40)-induced hippocampal cell death and astrocytic Ca(2+) signalling. Neurotoxicology. 2014;41:64–72. doi: 10.1016/j.neuro.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 63.Linde CI, Baryshnikov SG, Mazzocco-Spezzia A, Golovina VA. Dysregulation of Ca2+ signaling in astrocytes from mice lacking amyloid precursor protein. Am J Physiol Cell Physiol. 2011;300(6):C1502–1512. doi: 10.1152/ajpcell.00379.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hamel E. Cerebral circulation: function and dysfunction in Alzheimer’s disease. J Cardiovasc Pharmacol. 2015;65(4):317–324. doi: 10.1097/FJC.0000000000000177. [DOI] [PubMed] [Google Scholar]
- 65.Zhang L, Papadopoulos P, Hamel E. Endothelial TRPV4 channels mediate dilation of cerebral arteries: impairment and recovery in cerebrovascular pathologies related to Alzheimer’s disease. Br J Pharmacol. 2013;170(3):661–670. doi: 10.1111/bph.12315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Bessac BF, Jordt SE. Breathtaking TRP channels: TRPA1 and TRPV1 in airway chemosensation and reflex control. Physiol (Bethesda, Md) 2008;23:360–370. doi: 10.1152/physiol.00026.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang T, Wang L, Moreno-Vinasco L, Lang GD, Siegler JH, Mathew B, Usatyuk PV, Samet JM, Geyh AS, Breysse PN, Natarajan V, Garcia JG. Particulate matter air pollution disrupts endothelial cell barrier via calpain-mediated tight junction protein degradation. Part Fibre Toxicol. 2012;9:35. doi: 10.1186/1743-8977-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Robertson S, Thomson AL, Carter R, Stott HR, Shaw CA, Hadoke PW, Newby DE, Miller MR, Gray GA. Pulmonary diesel particulate increases susceptibility to myocardial ischemia/reperfusion injury via activation of sensory TRPV1 and beta1 adrenoreceptors. Part Fibre Toxicol. 2014;11:12. doi: 10.1186/1743-8977-11-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Deering-Rice CE, Johansen ME, Roberts JK, Thomas KC, Romero EG, Lee J, Yost GS, Veranth JM, Reilly CA. Transient receptor potential vanilloid-1 (TRPV1) is a mediator of lung toxicity for coal fly ash particulate material. Mol Pharmacol. 2012;81(3):411–419. doi: 10.1124/mol.111.076067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ghelfi E, Rhoden CR, Wellenius GA, Lawrence J, Gonzalez-Flecha B. Cardiac oxidative stress and electrophysiological changes in rats exposed to concentrated ambient particles are mediated by TRP-dependent pulmonary reflexes. Toxicol Scie Off J Soc Toxicol. 2008;102(2):328–336. doi: 10.1093/toxsci/kfn005. [DOI] [PubMed] [Google Scholar]
- 71.Agopyan N, Head J, Yu S, Simon SA. TRPV1 receptors mediate particulate matter-induced apoptosis. Am J Physiol Lung Cell Mol Physiol. 2004;286(3):L563–572. doi: 10.1152/ajplung.00299.2003. [DOI] [PubMed] [Google Scholar]
- 72.Agopyan N, Bhatti T, Yu S, Simon SA. Vanilloid receptor activation by 2- and 10-microm particles induces responses leading to apoptosis in human airway epithelial cells. Toxicol Appl Pharmacol. 2003;192(1):21–35. doi: 10.1016/s0041-008x(03)00259-x. [DOI] [PubMed] [Google Scholar]
- 73.Shapiro D, Deering-Rice CE, Romero EG, Hughen RW, Light AR, Veranth JM, Reilly CA. Activation of transient receptor potential ankyrin-1 (TRPA1) in lung cells by wood smoke particulate material. Chem Res Toxicol. 2013;26(5):750–758. doi: 10.1021/tx400024h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Deering-Rice CE, Romero EG, Shapiro D, Hughen RW, Light AR, Yost GS, Veranth JM, Reilly CA. Electrophilic components of diesel exhaust particles (DEP) activate transient receptor potential ankyrin-1 (TRPA1): a probable mechanism of acute pulmonary toxicity for DEP. Chem Res Toxicol. 2011;24(6):950–959. doi: 10.1021/tx200123z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li J, Kanju P, Patterson M, Chew WL, Cho SH, Gilmour I, Oliver T, Yasuda R, Ghio A, Simon SA, Liedtke W. TRPV4-mediated calcium influx into human bronchial epithelia upon exposure to diesel exhaust particles. Environ Health Perspect. 2011;119(6):784–793. doi: 10.1289/ehp.1002807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Deretic V, Saitoh T, Akira S. Autophagy in infection, inflammation and immunity. Nat Rev Immunol. 2013;13(10):722–737. doi: 10.1038/nri3532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sergin I, Razani B. Self-eating in the plaque: what macrophage autophagy reveals about atherosclerosis. Trends Endocrinol Metab: TEM. 2014;25(5):225–234. doi: 10.1016/j.tem.2014.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang W, Gao Q, Yang M, Zhang X, Yu L, Lawas M, Li X, Bryant-Genevier M, Southall NT, Marugan J, Ferrer M, Xu H. Up-regulation of lysosomal TRPML1 channels is essential for lysosomal adaptation to nutrient starvation. Proc Natl Acad Sci U S A. 2015;112(11):E1373–1381. doi: 10.1073/pnas.1419669112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Onyenwoke RU, Sexton JZ, Yan F, Diaz MC, Forsberg LJ, Major MB, Brenman JE. The mucolipidosis IV Ca2+ channel TRPML1 (MCOLN1) is regulated by the TOR kinase. Biochemical J. 2015;470(3):331–342. doi: 10.1042/BJ20150219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sun T, Wang X, Lu Q, Ren H, Zhang H. CUP-5, the C. elegans ortholog of the mammalian lysosomal channel protein MLN1/TRPML1, is required for proteolytic degradation in autolysosomes. Autophagy. 2011;7(11):1308–1315. doi: 10.4161/auto.7.11.17759. [DOI] [PubMed] [Google Scholar]
- 81.Medina DL, Di Paola S, Peluso I, Armani A, De Stefani D, Venditti R, Montefusco S, Scotto-Rosato A, Prezioso C, Forrester A, Settembre C, Wang W, Gao Q, Xu H, Sandri M, Rizzuto R, De Matteis MA, Ballabio A. Lysosomal calcium signalling regulates autophagy through calcineurin and TFEB. Nat Cell Biol. 2015;17(3):288–299. doi: 10.1038/ncb3114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Curcio-Morelli C, Charles FA, Micsenyi MC, Cao Y, Venugopal B, Browning MF, Dobrenis K, Cotman SL, Walkley SU, Slaugenhaupt SA. Macroautophagy is defective in mucolipin-1-deficient mouse neurons. Neurobiol Dis. 2010;40(2):370–377. doi: 10.1016/j.nbd.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Venugopal B, Mesires NT, Kennedy JC, Curcio-Morelli C, Laplante JM, Dice JF, Slaugenhaupt SA. Chaperone-mediated autophagy is defective in mucolipidosis type IV. J Cell Physiol. 2009;219(2):344–353. doi: 10.1002/jcp.21676. [DOI] [PubMed] [Google Scholar]
- 84.Zeevi DA, Lev S, Frumkin A, Minke B, Bach G. Heteromultimeric TRPML channel assemblies play a crucial role in the regulation of cell viability models and starvation-induced autophagy. J Cell Sci. 2010;123(Pt 18):3112–3124. doi: 10.1242/jcs.067330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee JH, McBrayer MK, Wolfe DM, Haslett LJ, Kumar A, Sato Y, Lie PP, Mohan P, Coffey EE, Kompella U, Mitchell CH, Lloyd-Evans E, Nixon RA. Presenilin 1 Maintains Lysosomal Ca(2+) Homeostasis via TRPML1 by Regulating vATPase-Mediated Lysosome Acidification. Cell reports. 2015;12(9):1430–1444. doi: 10.1016/j.celrep.2015.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Venkatachalam K, Long AA, Elsaesser R, Nikolaeva D, Broadie K, Montell C. Motor deficit in a Drosophila model of mucolipidosis type IV due to defective clearance of apoptotic cells. Cell. 2008;135(5):838–851. doi: 10.1016/j.cell.2008.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Martina JA, Lelouvier B, Puertollano R. The calcium channel mucolipin-3 is a novel regulator of trafficking along the endosomal pathway. Traffic (Copenhagen, Denmark) 2009;10(8):1143–1156. doi: 10.1111/j.1600-0854.2009.00935.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Kim HJ, Soyombo AA, Tjon-Kon-Sang S, So I, Muallem S. The Ca(2+) channel TRPML3 regulates membrane trafficking and autophagy. Traffic (Copenhagen, Denmark) 2009;10(8):1157–1167. doi: 10.1111/j.1600-0854.2009.00924.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Choi S, Kim HJ. The Ca2+ channel TRPML3 specifically interacts with the mammalian ATG8 homologue GATE16 to regulate autophagy. Biochem Biophys Res Commun. 2014;443(1):56–61. doi: 10.1016/j.bbrc.2013.11.044. [DOI] [PubMed] [Google Scholar]
- 90.Miao Y, Li G, Zhang X, Xu H, Abraham SN. A TRP Channel Senses Lysosome Neutralization by Pathogens to Trigger Their Expulsion. Cell. 2015;161(6):1306–1319. doi: 10.1016/j.cell.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhang W, Chu X, Tong Q, Cheung JY, Conrad K, Masker K, Miller BA. A novel TRPM2 isoform inhibits calcium influx and susceptibility to cell death. J Biol Chem. 2003;278(18):16222–16229. doi: 10.1074/jbc.M300298200. [DOI] [PubMed] [Google Scholar]
- 92.Chen SJ, Hoffman NE, Shanmughapriya S, Bao L, Keefer K, Conrad K, Merali S, Takahashi Y, Abraham T, Hirschler-Laszkiewicz I, Wang J, Zhang XQ, Song J, Barrero C, Shi Y, Kawasawa YI, Bayerl M, Sun T, Barbour M, Wang HG, Madesh M, Cheung JY, Miller BA. A splice variant of the human ion channel TRPM2 modulates neuroblastoma tumor growth through hypoxia-inducible factor (HIF)-1/2alpha. J Biol Chem. 2014;289(52):36284–36302. doi: 10.1074/jbc.M114.620922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wyrsch P, Blenn C, Bader J, Althaus FR. Cell death and autophagy under oxidative stress: roles of poly(ADP-Ribose) polymerases and Ca(2+) Mol Cell Biol. 2012;32(17):3541–3553. doi: 10.1128/MCB.00437-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Atsumi T, Singh R, Sabharwal L, Bando H, Meng J, Arima Y, Yamada M, Harada M, Jiang JJ, Kamimura D, Ogura H, Hirano T, Murakami M. Inflammation amplifier, a new paradigm in cancer biology. Cancer Res. 2014;74(1):8–14. doi: 10.1158/0008-5472.CAN-13-2322. [DOI] [PubMed] [Google Scholar]
- 95.Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer. 2009;9(11):798–809. doi: 10.1038/nrc2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mishra BB, Rathinam VA, Martens GW, Martinot AJ, Kornfeld H, Fitzgerald KA, Sassetti CM. Nitric oxide controls the immunopathology of tuberculosis by inhibiting NLRP3 inflammasome-dependent processing of IL-1beta. Nat Immunol. 2013;14(1):52–60. doi: 10.1038/ni.2474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Fric J, Zelante T, Ricciardi-Castagnoli P. Phagocytosis of Particulate Antigens - All Roads Lead to Calcineurin/NFAT Signaling Pathway. Front Immunol. 2014;4:513. doi: 10.3389/fimmu.2013.00513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Rossol M, Pierer M, Raulien N, Quandt D, Meusch U, Rothe K, Schubert K, Schoneberg T, Schaefer M, Krugel U, Smajilovic S, Brauner-Osborne H, Baerwald C, Wagner U. Extracellular Ca2+ is a danger signal activating the NLRP3 inflammasome through G protein-coupled calcium sensing receptors. Nat Commun. 2012;3:1329. doi: 10.1038/ncomms2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Oeckinghaus A, Ghosh S. The NF-kappaB family of transcription factors and its regulation. Cold Spring Harbor Perspect Biol. 2009;1(4):a000034. doi: 10.1101/cshperspect.a000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tabary O, Boncoeur E, de Martin R, Pepperkok R, Clement A, Schultz C, Jacquot J. Calcium-dependent regulation of NF-(kappa)B activation in cystic fibrosis airway epithelial cells. Cell Signal. 2006;18(5):652–660. doi: 10.1016/j.cellsig.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 101.Zhu L, Song S, Pi Y, Yu Y, She W, Ye H, Su Y, Hu Q. Cumulated Ca2(+) spike duration underlies Ca2(+) oscillation frequency-regulated NFkappaB transcriptional activity. J Cell Sci. 2011;124(Pt 15):2591–2601. doi: 10.1242/jcs.082727. [DOI] [PubMed] [Google Scholar]
- 102.Yokoseki O, Suzuki J, Kitabayashi H, Watanabe N, Wada Y, Aoki M, Morishita R, Kaneda Y, Ogihara T, Futamatsu H, Kobayashi Y, Isobe M. cis Element decoy against nuclear factor-kappaB attenuates development of experimental autoimmune myocarditis in rats. Circ Res. 2001;89(10):899–906. doi: 10.1161/hh2201.099373. [DOI] [PubMed] [Google Scholar]
- 103.Suzuki H, Maehara K, Yaoita H, Maruyama Y. Altered effects of angiotensin ii type 1 and type 2 receptor blockers on cardiac norepinephrine release and inotropic responses during cardiac sympathetic nerve stimulation in aorto-caval shunt rats. Circ J : Off J Jpn Circ Soc. 2004;68(7):683–690. doi: 10.1253/circj.68.683. [DOI] [PubMed] [Google Scholar]
- 104.Takahashi Y, Watanabe H, Murakami M, Ohba T, Radovanovic M, Ono K, Iijima T, Ito H. Involvement of transient receptor potential canonical 1 (TRPC1) in angiotensin II-induced vascular smooth muscle cell hypertrophy. Atherosclerosis. 2007;195(2):287–296. doi: 10.1016/j.atherosclerosis.2006.12.033. [DOI] [PubMed] [Google Scholar]
- 105.Yang K, Lu W, Jia J, Zhang J, Zhao M, Wang S, Jiang H, Xu L, Wang J. Noggin inhibits hypoxia-induced proliferation by targeting store-operated calcium entry and transient receptor potential cation channels. Am J Physiol Cell Physiol. 2015;308(11):C869–878. doi: 10.1152/ajpcell.00349.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yu Y, Sweeney M, Zhang S, Platoshyn O, Landsberg J, Rothman A, Yuan JX. PDGF stimulates pulmonary vascular smooth muscle cell proliferation by upregulating TRPC6 expression. Am J Physiol Cell Physiol. 2003;284(2):C316–330. doi: 10.1152/ajpcell.00125.2002. [DOI] [PubMed] [Google Scholar]
- 107.Abkhezr M, Kim EY, Roshanravan H, Nikolos F, Thomas C, Hagmann H, Benzing T, Dryer SE. Pleiotropic signaling evoked by tumor necrosis factor in podocytes. Am J Physiol Renal Physiol. 2015;309(2):F98–f108. doi: 10.1152/ajprenal.00146.2015. [DOI] [PubMed] [Google Scholar]
- 108.Abkhezr M, Dryer SE. Angiotensin II and canonical transient receptor potential-6 activation stimulate release of a signal transducer and activator of transcription 3-activating factor from mouse podocytes. Mol Pharmacol. 2014;86(2):150–158. doi: 10.1124/mol.114.092536. [DOI] [PubMed] [Google Scholar]
- 109.Liu M, Inoue K, Leng T, Guo S, Xiong ZG. TRPM7 channels regulate glioma stem cell through STAT3 and Notch signaling pathways. Cell Signal. 2014;26(12):2773–2781. doi: 10.1016/j.cellsig.2014.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Davis FM, Azimi I, Faville RA, Peters AA, Jalink K, Putney JW, Jr, Goodhill GJ, Thompson EW, Roberts-Thomson SJ, Monteith GR. Induction of epithelial-mesenchymal transition (EMT) in breast cancer cells is calcium signal dependent. Oncogene. 2014;33(18):2307–2316. doi: 10.1038/onc.2013.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Agrawal M, Kumar V, Singh AK, Kashyap MP, Khanna VK, Siddiqui MA, Pant AB. trans-Resveratrol protects ischemic PC12 Cells by inhibiting the hypoxia associated transcription factors and increasing the levels of antioxidant defense enzymes. ACS Chem Neurosci. 2013;4(2):285–294. doi: 10.1021/cn300143m. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Vinuesa AG, Sancho R, Garcia-Limones C, Behrens A, ten Dijke P, Calzado MA, Munoz E. Vanilloid receptor-1 regulates neurogenic inflammation in colon and protects mice from colon cancer. Cancer Res. 2012;72(7):1705–1716. doi: 10.1158/0008-5472.CAN-11-3693. [DOI] [PubMed] [Google Scholar]
- 113.Hussain SP, Harris CC. Inflammation and cancer: an ancient link with novel potentials. Int J Cancer J Int Du Cancer. 2007;121(11):2373–2380. doi: 10.1002/ijc.23173. [DOI] [PubMed] [Google Scholar]
- 114.Ouyang X, Ghani A, Malik A, Wilder T, Colegio OR, Flavell RA, Cronstein BN, Mehal WZ. Adenosine is required for sustained inflammasome activation via the A(2)A receptor and the HIF-1alpha pathway. Nat Commun. 2013;4:2909. doi: 10.1038/ncomms3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wang Y, Lu W, Yang K, Wang Y, Zhang J, Jia J, Yun X, Tian L, Chen Y, Jiang Q, Zhang B, Chen X, Wang J. Peroxisome proliferator-activated receptor gamma inhibits pulmonary hypertension targeting store-operated calcium entry. J Mol Med (Berlin, Germany) 2015;93(3):327–342. doi: 10.1007/s00109-014-1216-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Asghar MY, Magnusson M, Kemppainen K, Sukumaran P, Lof C, Pulli I, Kalhori V, Tornquist K. Transient Receptor Potential Canonical 1 (TRPC1) Channels as Regulators of Sphingolipid and VEGF Receptor Expression: IMPLICATIONS FOR THYROID CANCER CELL MIGRATION AND PROLIFERATION. J Biol Chem. 2015;290(26):16116–16131. doi: 10.1074/jbc.M115.643668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang J, Wang N, Xie J, Walton SC, McKown RL, Raab RW, Ma P, Beck SL, Coffman GL, Hussaini IM, Laurie GW. Restricted epithelial proliferation by lacritin via PKCalpha-dependent NFAT and mTOR pathways. J Cell Biol. 2006;174(5):689–700. doi: 10.1083/jcb.200605140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chu W, Wan L, Zhao D, Qu X, Cai F, Huo R, Wang N, Zhu J, Zhang C, Zheng F, Cai R, Dong D, Lu Y, Yang B. Mild hypoxia-induced cardiomyocyte hypertrophy via up-regulation of HIF-1alpha-mediated TRPC signalling. J Cell Mol Med. 2012;16(9):2022–2034. doi: 10.1111/j.1582-4934.2011.01497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zhu Y, Pan Q, Meng H, Jiang Y, Mao A, Wang T, Hua D, Yao X, Jin J, Ma X. Enhancement of vascular endothelial growth factor release in long-term drug-treated breast cancer via transient receptor potential channel 5-Ca(2+)-hypoxia-inducible factor 1alpha pathway. Pharmacol Res. 2015;93:36–42. doi: 10.1016/j.phrs.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 120.Li S, Wang J, Wei Y, Liu Y, Ding X, Dong B, Xu Y, Wang Y. Crucial role of TRPC6 in maintaining the stability of HIF-1alpha in glioma cells under hypoxia. J Cell Sci. 2015;128(17):3317–3329. doi: 10.1242/jcs.173161. [DOI] [PubMed] [Google Scholar]
- 121.Iyer SC, Kannan A, Gopal A, Devaraj N, Halagowder D. Receptor channel TRPC6 orchestrate the activation of human hepatic stellate cell under hypoxia condition. Exp Cell Res. 2015;336(1):66–75. doi: 10.1016/j.yexcr.2015.03.023. [DOI] [PubMed] [Google Scholar]
- 122.Miller BA, Wang J, Hirschler-Laszkiewicz I, Gao E, Song J, Zhang XQ, Koch WJ, Madesh M, Mallilankaraman K, Gu T, Chen SJ, Keefer K, Conrad K, Feldman AM, Cheung JY. The second member of transient receptor potential-melastatin channel family protects hearts from ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol. 2013;304(7):H1010–1022. doi: 10.1152/ajpheart.00906.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Schoolmeesters A, Brown DD, Fedorov Y. Kinome-wide functional genomics screen reveals a novel mechanism of TNFalpha-induced nuclear accumulation of the HIF-1alpha transcription factor in cancer cells. PLoS One. 2012;7(2) doi: 10.1371/journal.pone.0031270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Rao A, Luo C, Hogan PG. Transcription factors of the NFAT family: regulation and function. Annu Rev Immunol. 1997;15:707–747. doi: 10.1146/annurev.immunol.15.1.707. [DOI] [PubMed] [Google Scholar]
- 125.Vandewalle A, Tourneur E, Bens M, Chassin C, Werts C. Calcineurin/NFAT signaling and innate host defence: a role for NOD1-mediated phagocytic functions. Cell Commun Signal : CCS. 2014;12:8. doi: 10.1186/1478-811X-12-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Inoue R, Jensen LJ, Shi J, Morita H, Nishida M, Honda A, Ito Y. Transient receptor potential channels in cardiovascular function and disease. Circ Res. 2006;99(2):119–131. doi: 10.1161/01.RES.0000233356.10630.8a. [DOI] [PubMed] [Google Scholar]
- 127.Nishida M, Kurose H. Roles of TRP channels in the development of cardiac hypertrophy. Naunyn Schmiedeberg’s Arch Pharmacol. 2008;378(4):395–406. doi: 10.1007/s00210-008-0321-8. [DOI] [PubMed] [Google Scholar]
- 128.Eder P, Molkentin JD. TRPC channels as effectors of cardiac hypertrophy. Circ Res. 2011;108(2):265–272. doi: 10.1161/CIRCRESAHA.110.225888. [DOI] [PubMed] [Google Scholar]
- 129.Kockx M, Jessup W, Kritharides L. Cyclosporin A and atherosclerosis--cellular pathways in atherogenesis. Pharmacol Ther. 2010;128(1):106–118. doi: 10.1016/j.pharmthera.2010.06.001. [DOI] [PubMed] [Google Scholar]
- 130.Zetterqvist AV, Berglund LM, Blanco F, Garcia-Vaz E, Wigren M, Duner P, Andersson AM, To F, Spegel P, Nilsson J, Bengtsson E, Gomez MF. Inhibition of nuclear factor of activated T-cells (NFAT) suppresses accelerated atherosclerosis in diabetic mice. PLoS One. 2014;8(6) doi: 10.1371/journal.pone.0065020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Abkhezr M, Kim EY, Roshanravan H, Nikolos F, Thomas C, Hagmann H, Benzing T, Dryer SE. Pleiotropic signaling evoked by tumor necrosis factor in podocytes. Am J Physiol Renal Physiol. 2015;309(2):F98–108. doi: 10.1152/ajprenal.00146.2015. [DOI] [PubMed] [Google Scholar]
- 132.Makarewich CA, Zhang H, Davis J, Correll RN, Trappanese DM, Hoffman NE, Troupes CD, Berretta RM, Kubo H, Madesh M, Chen X, Gao E, Molkentin JD, Houser SR. Transient receptor potential channels contribute to pathological structural and functional remodeling after myocardial infarction. Circ Res. 2014;115(6):567–580. doi: 10.1161/CIRCRESAHA.115.303831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32(9):2045–2051. doi: 10.1161/ATVBAHA.108.179705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Vassalli G, Gallino A, Weis M, von Scheidt W, Kappenberger L, von Segesser LK, Goy JJ. Alloimmunity and nonimmunologic risk factors in cardiac allograft vasculopathy. Eur Heart J. 2003;24(13):1180–1188. doi: 10.1016/s0195-668x(03)00237-9. [DOI] [PubMed] [Google Scholar]
- 135.Perez-Ruiz F, Becker MA. Inflammation: a possible mechanism for a causative role of hyperuricemia/gout in cardiovascular disease. Curr Med Res Opin. 2015;31(Suppl 2):9–14. doi: 10.1185/03007995.2015.1087980. [DOI] [PubMed] [Google Scholar]
- 136.Frieler RA, Mortensen RM. Immune cell and other noncardiomyocyte regulation of cardiac hypertrophy and remodeling. Circulation. 2015;131(11):1019–1030. doi: 10.1161/CIRCULATIONAHA.114.008788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Yamashita T, Sasaki N, Kasahara K, Hirata K. Anti-inflammatory and immune-modulatory therapies for preventing atherosclerotic cardiovascular disease. J Cardiol. 2015;66(1):1–8. doi: 10.1016/j.jjcc.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 138.Nguyen MU, Wallace MJ, Pepe S, Menheniott TR, Moss TJ. Burgner D (2015) Perinatal inflammation: a common factor in the early origins of cardiovascular disease? Clinical science (London. England : 1979;129(8):769–784. doi: 10.1042/CS20150045. [DOI] [PubMed] [Google Scholar]
- 139.Hollan I, Dessein PH, Ronda N, Wasko MC, Svenungsson E, Agewall S, Cohen-Tervaert JW, Maki-Petaja K, Grundtvig M, Karpouzas GA, Meroni PL. Prevention of cardiovascular disease in rheumatoid arthritis. Autoimmun Rev. 2015;14(10):952–969. doi: 10.1016/j.autrev.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 140.Qiu Z, Hu J, Van den Steen PE, Opdenakker G. Targeting matrix metalloproteinases in acute inflammatory shock syndromes. Comb Chem High Throughput Screen. 2012;15(7):555–570. doi: 10.2174/138620712801619159. [DOI] [PubMed] [Google Scholar]
- 141.Saxena A, Russo I, Frangogiannis NG. Inflammation as a therapeutic target in myocardial infarction: learning from past failures to meet future challenges. Transl Res J Lab Clin Med. 2015 doi: 10.1016/j.trsl.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Vilahur G, Badimon L. Ischemia/reperfusion activates myocardial innate immune response: the key role of the toll-like receptor. Front Physiol. 2014;5:496. doi: 10.3389/fphys.2014.00496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bergdahl A, Gomez MF, Wihlborg AK, Erlinge D, Eyjolfson A, Xu SZ, Beech DJ, Dreja K, Hellstrand P. Plasticity of TRPC expression in arterial smooth muscle: correlation with store-operated Ca2+ entry. Am J Physiol Cell Physiol. 2005;288(4):C872–880. doi: 10.1152/ajpcell.00334.2004. [DOI] [PubMed] [Google Scholar]
- 144.Edwards JM, Neeb ZP, Alloosh MA, Long X, Bratz IN, Peller CR, Byrd JP, Kumar S, Obukhov AG, Sturek M. Exercise training decreases store-operated Ca2+entry associated with metabolic syndrome and coronary atherosclerosis. Cardiovasc Res. 2010;85(3):631–640. doi: 10.1093/cvr/cvp308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Smedlund K, Vazquez G. Involvement of native TRPC3 proteins in ATP-dependent expression of VCAM-1 and monocyte adherence in coronary artery endothelial cells. Arterioscler Thromb Vasc Biol. 2008;28(11):2049–2055. doi: 10.1161/ATVBAHA.108.175356. [DOI] [PubMed] [Google Scholar]
- 146.Smedlund KB, Birnbaumer L, Vazquez G. Increased size and cellularity of advanced atherosclerotic lesions in mice with endothelial overexpression of the human TRPC3 channel. Proc Natl Acad Sci U S A. 2015;112(17):E2201–2206. doi: 10.1073/pnas.1505410112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Chaudhuri P, Colles SM, Bhat M, Van Wagoner DR, Birnbaumer L, Graham LM. Elucidation of a TRPC6-TRPC5 channel cascade that restricts endothelial cell movement. Mol Biol Cell. 2008;19(8):3203–3211. doi: 10.1091/mbc.E07-08-0765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhang Y, Qin W, Zhang L, Wu X, Du N, Hu Y, Li X, Shen N, Xiao D, Zhang H, Li Z, Zhang Y, Yang H, Gao F, Du Z, Xu C, Yang B. MicroRNA-26a prevents endothelial cell apoptosis by directly targeting TRPC6 in the setting of atherosclerosis. Scientific reports. 2015;5:9401. doi: 10.1038/srep09401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Schilling T, Eder C. Non-selective cation channel activity is required for lysophosphatidylcholine-induced monocyte migration. J Cell Physiol. 2009;221(2):325–334. doi: 10.1002/jcp.21857. [DOI] [PubMed] [Google Scholar]
- 150.Himi N, Hamaguchi A, Hashimoto K, Koga T, Narita K, Miyamoto O. Calcium influx through the TRPV1 channel of endothelial cells (ECs) correlates with a stronger adhesion between monocytes and ECs. Adv Med Sci. 2012;57(2):224–229. doi: 10.2478/v10039-012-0044-4. [DOI] [PubMed] [Google Scholar]
- 151.Li BH, Yin YW, Liu Y, Pi Y, Guo L, Cao XJ, Gao CY, Zhang LL, Li JC. TRPV1 activation impedes foam cell formation by inducing autophagy in oxLDL-treated vascular smooth muscle cells. Cell Death Dis. 2014;5 doi: 10.1038/cddis.2014.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ching LC, Kou YR, Shyue SK, Su KH, Wei J, Cheng LC, Yu YB, Pan CC, Lee TS. Molecular mechanisms of activation of endothelial nitric oxide synthase mediated by transient receptor potential vanilloid type 1. Cardiovasc Res. 2011;91(3):492–501. doi: 10.1093/cvr/cvr104. [DOI] [PubMed] [Google Scholar]
- 153.Zhao JF, Ching LC, Kou YR, Lin SJ, Wei J, Shyue SK, Lee TS. Activation of TRPV1 prevents OxLDL-induced lipid accumulation and TNF-alpha-induced inflammation in macrophages: role of liver X receptor alpha. Mediat Inflamm. 2013;2013:925171. doi: 10.1155/2013/925171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kumar B, Dreja K, Shah SS, Cheong A, Xu SZ, Sukumar P, Naylor J, Forte A, Cipollaro M, McHugh D, Kingston PA, Heagerty AM, Munsch CM, Bergdahl A, Hultgardh-Nilsson A, Gomez MF, Porter KE, Hellstrand P, Beech DJ. Upregulated TRPC1 channel in vascular injury in vivo and its role in human neointimal hyperplasia. Circ Res. 2006;98(4):557–563. doi: 10.1161/01.RES.0000204724.29685.db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ru X, Zheng C, Zhao Q, Lan HY, Huang Y, Wan S, Mori Y, Yao X. Transient receptor potential channel M2 contributes to neointimal hyperplasia in vascular walls. Biochim Biophys Acta. 2015;1852(7):1360–1371. doi: 10.1016/j.bbadis.2015.03.014. [DOI] [PubMed] [Google Scholar]
- 156.Xie A, Aihara Y, Bouryi VA, Nikitina E, Jahromi BS, Zhang ZD, Takahashi M, Macdonald RL. Novel mechanism of endothelin-1-induced vasospasm after subarachnoid hemorrhage. J Cereb Blood Flow Metab : Off J Int Soc Cereb Blood Flow Metab. 2007;27(10):1692–1701. doi: 10.1038/sj.jcbfm.9600471. [DOI] [PubMed] [Google Scholar]
- 157.Akabori H, Yamamoto H, Tsuchihashi H, Mori T, Fujino K, Shimizu T, Endo Y, Tani T. Transient receptor potential vanilloid 1 antagonist, capsazepine, improves survival in a rat hemorrhagic shock model. Ann Surg. 2007;245(6):964–970. doi: 10.1097/01.sla.0000255577.80800.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Williams IA, Allen DG. Intracellular calcium handling in ventricular myocytes from mdx mice. Am J Physiol Heart Circ Physiol. 2007;292(2):H846–855. doi: 10.1152/ajpheart.00688.2006. [DOI] [PubMed] [Google Scholar]
- 159.Friedman JK, Nitta CH, Henderson KM, Codianni SJ, Sanchez L, Ramiro-Diaz JM, Howard TA, Giermakowska W, Kanagy NL, Gonzalez Bosc LV. Intermittent hypoxia-induced increases in reactive oxygen species activate NFATc3 increasing endothelin-1 vasoconstrictor reactivity. Vasc Pharmacol. 2014;60(1):17–24. doi: 10.1016/j.vph.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Seth M, Zhang ZS, Mao L, Graham V, Burch J, Stiber J, Tsiokas L, Winn M, Abramowitz J, Rockman HA, Birnbaumer L, Rosenberg P. TRPC1 channels are critical for hypertrophic signaling in the heart. Circ Res. 2009;105(10):1023–1030. doi: 10.1161/CIRCRESAHA.109.206581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Vindis C, D’Angelo R, Mucher E, Negre-Salvayre A, Parini A, Mialet-Perez J. Essential role of TRPC1 channels in cardiomyoblasts hypertrophy mediated by 5-HT2A serotonin receptors. Biochem Biophys Res Commun. 2010;391(1):979–983. doi: 10.1016/j.bbrc.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 162.Kitajima N, Watanabe K, Morimoto S, Sato Y, Kiyonaka S, Hoshijima M, Ikeda Y, Nakaya M, Ide T, Mori Y, Kurose H, Nishida M. TRPC3-mediated Ca2+ influx contributes to Rac1-mediated production of reactive oxygen species in MLP-deficient mouse hearts. Biochem Biophys Res Commun. 2011;409(1):108–113. doi: 10.1016/j.bbrc.2011.04.124. [DOI] [PubMed] [Google Scholar]
- 163.Sowa N, Horie T, Kuwabara Y, Baba O, Watanabe S, Nishi H, Kinoshita M, Takanabe-Mori R, Wada H, Shimatsu A, Hasegawa K, Kimura T, Ono K. MicroRNA 26b encoded by the intron of small CTD phosphatase (SCP) 1 has an antagonistic effect on its host gene. J Cell Biochem. 2012;113(11):3455–3465. doi: 10.1002/jcb.24222. [DOI] [PubMed] [Google Scholar]
- 164.Bush EW, Hood DB, Papst PJ, Chapo JA, Minobe W, Bristow MR, Olson EN, McKinsey TA. Canonical transient receptor potential channels promote cardiomyocyte hypertrophy through activation of calcineurin signaling. J Bio Chem. 2006;281(44):33487–33496. doi: 10.1074/jbc.M605536200. [DOI] [PubMed] [Google Scholar]
- 165.Onohara N, Nishida M, Inoue R, Kobayashi H, Sumimoto H, Sato Y, Mori Y, Nagao T, Kurose H. TRPC3 and TRPC6 are essential for angiotensin II-induced cardiac hypertrophy. EMBO J. 2006;25(22):5305–5316. doi: 10.1038/sj.emboj.7601417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Kuwahara K, Wang Y, McAnally J, Richardson JA, Bassel-Duby R, Hill JA, Olson EN. TRPC6 fulfills a calcineurin signaling circuit during pathologic cardiac remodeling. J Clin Invest. 2006;116(12):3114–3126. doi: 10.1172/JCI27702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kinoshita H, Kuwahara K, Nishida M, Jian Z, Rong X, Kiyonaka S, Kuwabara Y, Kurose H, Inoue R, Mori Y, Li Y, Nakagawa Y, Usami S, Fujiwara M, Yamada Y, Minami T, Ueshima K, Nakao K. Inhibition of TRPC6 channel activity contributes to the antihypertrophic effects of natriuretic peptides-guanylyl cyclase-A signaling in the heart. Circ Res. 2010;106(12):1849–1860. doi: 10.1161/CIRCRESAHA.109.208314. [DOI] [PubMed] [Google Scholar]
- 168.Kunert-Keil C, Landsberger M, Jantzen F, Niessner F, Kroemer HK, Felix SB, Brinkmeier H, Peters J. Molecular changes in the early phase of renin-dependent cardiac hypertrophy in hypertensive cyp1a1ren-2 transgenic rats. J Renin-Angiotensin-Aldosterone Syst : JRAAS. 2013;14(1):41–50. doi: 10.1177/1470320312460070. [DOI] [PubMed] [Google Scholar]
- 169.Gao F, Liang Y, Wang X, Lu Z, Li L, Zhu S, Liu D, Yan Z, Zhu Z. TRPV1 Activation Attenuates High-Salt Diet-Induced Cardiac Hypertrophy and Fibrosis through PPAR-delta Upregulation. PPAR Res. 2014;2014:491963. doi: 10.1155/2014/491963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Wang Q, Ma S, Li D, Zhang Y, Tang B, Qiu C, Yang Y, Yang D. Dietary capsaicin ameliorates pressure overload-induced cardiac hypertrophy and fibrosis through the transient receptor potential vanilloid type 1. Am J Hypertens. 2014;27(12):1521–1529. doi: 10.1093/ajh/hpu068. [DOI] [PubMed] [Google Scholar]
- 171.Iwata Y, Ohtake H, Suzuki O, Matsuda J, Komamura K, Wakabayashi S. Blockade of sarcolemmal TRPV2 accumulation inhibits progression of dilated cardiomyopathy. Cardiovasc Res. 2013;99(4):760–768. doi: 10.1093/cvr/cvt163. [DOI] [PubMed] [Google Scholar]
- 172.Demion M, Thireau J, Gueffier M, Finan A, Khoueiry Z, Cassan C, Serafini N, Aimond F, Granier M, Pasquie JL, Launay P, Richard S. Trpm4 gene invalidation leads to cardiac hypertrophy and electrophysiological alterations. PLoS One. 2014;9(12) doi: 10.1371/journal.pone.0115256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Kecskes M, Jacobs G, Kerselaers S, Syam N, Menigoz A, Vangheluwe P, Freichel M, Flockerzi V, Voets T, Vennekens R. The Ca(2+)-activated cation channel TRPM4 is a negative regulator of angiotensin II-induced cardiac hypertrophy. Basic Res Cardiol. 2015;110(4):43. doi: 10.1007/s00395-015-0501-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Hang P, Zhao J, Cai B, Tian S, Huang W, Guo J, Sun C, Li Y, Du Z. Brain-derived neurotrophic factor regulates TRPC3/6 channels and protects against myocardial infarction in rodents. Int J Biol Sci. 2015;11(5):536–545. doi: 10.7150/ijbs.10754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Jacobs G, Oosterlinck W, Dresselaers T, Geenens R, Kerselaers S, Himmelreich U, Herijgers P, Vennekens R. Enhanced beta-adrenergic cardiac reserve in Trpm4(−)/(−) mice with ischaemic heart failure. Cardiovasc Res. 2015;105(3):330–339. doi: 10.1093/cvr/cvv009. [DOI] [PubMed] [Google Scholar]
- 176.Huang W, Rubinstein J, Prieto AR, Wang DH. Enhanced postmyocardial infarction fibrosis via stimulation of the transforming growth factor-beta-Smad2 signaling pathway: role of transient receptor potential vanilloid type 1 channels. J Hypertens. 2010;28(2):367–376. doi: 10.1097/HJH.0b013e328333af48. [DOI] [PubMed] [Google Scholar]
- 177.Lupinski SL, Schlicker E, Pedzinska-Betiuk A, Malinowska B. Acute myocardial ischemia enhances the vanilloid TRPV1 and serotonin 5-HT3 receptor-mediated Bezold-Jarisch reflex in rats. Pharmacol Rep : PR. 2011;63(6):1450–1459. doi: 10.1016/s1734-1140(11)70709-5. [DOI] [PubMed] [Google Scholar]
- 178.Entin-Meer M, Levy R, Goryainov P, Landa N, Barshack I, Avivi C, Semo J, Keren G. The transient receptor potential vanilloid 2 cation channel is abundant in macrophages accumulating at the peri-infarct zone and may enhance their migration capacity towards injured cardiomyocytes following myocardial infarction. PLoS One. 2014;9(8) doi: 10.1371/journal.pone.0105055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Sexton A, McDonald M, Cayla C, Thiemermann C, Ahluwalia A. 12-Lipoxygenase-derived eicosanoids protect against myocardial ischemia/reperfusion injury via activation of neuronal TRPV1. FASEB J : Off Publ Fed Am Soc Exp Biol. 2007;21(11):2695–2703. doi: 10.1096/fj.06-7828com. [DOI] [PubMed] [Google Scholar]
- 180.Zhong B, Wang DH. Protease-activated receptor 2-mediated protection of myocardial ischemia-reperfusion injury: role of transient receptor potential vanilloid receptors. Am J Physiol Regul, Integ Comp Physiol. 2009;297(6):R1681–1690. doi: 10.1152/ajpregu.90746.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Zheng LR, Zhang YY, Han J, Sun ZW, Zhou SX, Zhao WT, Wang LH. Nerve growth factor rescues diabetic mice heart after ischemia/reperfusion injury via up-regulation of the TRPV1 receptor. J Diabetes Complicat. 2015;29(3):323–328. doi: 10.1016/j.jdiacomp.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 182.Gao Y, Song J, Chen H, Cao C, Lee C. TRPV1 activation is involved in the cardioprotection of remote limb ischemic postconditioning in ischemia-reperfusion injury rats. Biochem Biophys Res Commun. 2015;463(4):1034–1039. doi: 10.1016/j.bbrc.2015.06.054. [DOI] [PubMed] [Google Scholar]
- 183.Hiroi T, Wajima T, Negoro T, Ishii M, Nakano Y, Kiuchi Y, Mori Y, Shimizu S. Neutrophil TRPM2 channels are implicated in the exacerbation of myocardial ischaemia/reperfusion injury. Cardiovasc Res. 2013;97(2):271–281. doi: 10.1093/cvr/cvs332. [DOI] [PubMed] [Google Scholar]
- 184.Roberge S, Roussel J, Andersson DC, Meli AC, Vidal B, Blandel F, Lanner JT, Le Guennec JY, Katz A, Westerblad H, Lacampagne A, Fauconnier J. TNF-alpha-mediated caspase-8 activation induces ROS production and TRPM2 activation in adult ventricular myocytes. Cardiovasc Res. 2014;103(1):90–99. doi: 10.1093/cvr/cvu112. [DOI] [PubMed] [Google Scholar]
- 185.Piao H, Takahashi K, Yamaguchi Y, Wang C, Liu K, Naruse K. Transient receptor potential melastatin-4 is involved in hypoxia-reoxygenation injury in the cardiomyocytes. PLoS One. 2015;10(4) doi: 10.1371/journal.pone.0121703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Everett KV, Chioza BA, Georgoula C, Reece A, Capon F, Parker KA, Cord-Udy C, McKeigue P, Mitton S, Pierro A, Puri P, Mitchison HM, Chung EM, Gardiner RM. Genome-wide high-density SNP-based linkage analysis of infantile hypertrophic pyloric stenosis identifies loci on chromosomes 11q14-q22 and Xq23. Am J Hum Genet. 2008;82(3):756–762. doi: 10.1016/j.ajhg.2007.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wick G, Knoflach M, Kind M, Henderson B, Bernhard D. Heat shock proteins and stress in atherosclerosis. Autoimmun Rev. 2004;3(Suppl 1):S30–31. [PubMed] [Google Scholar]
- 188.Yamashiro K, Sasano T, Tojo K, Namekata I, Kurokawa J, Sawada N, Suganami T, Kamei Y, Tanaka H, Tajima N, Utsunomiya K, Ogawa Y, Furukawa T. Role of transient receptor potential vanilloid 2 in LPS-induced cytokine production in macrophages. Biochem Biophys Res Commun. 2010;398(2):284–289. doi: 10.1016/j.bbrc.2010.06.082. [DOI] [PubMed] [Google Scholar]
- 189.Kamo T, Akazawa H, Komuro I. Cardiac nonmyocytes in the hub of cardiac hypertrophy. Circ Res. 2015;117(1):89–98. doi: 10.1161/CIRCRESAHA.117.305349. [DOI] [PubMed] [Google Scholar]
- 190.Levitsky S. Protecting the myocardial cell during coronary revascularization. The William W. L Glenn Lec Circ. 2006;114(1 Suppl):I339–343. doi: 10.1161/CIRCULATIONAHA.105.001685. [DOI] [PubMed] [Google Scholar]
- 191.Kaminski KA, Bonda TA, Korecki J, Musial WJ. Oxidative stress and neutrophil activation--the two keystones of ischemia/reperfusion injury. Int J Cardiol. 2002;86(1):41–59. doi: 10.1016/s0167-5273(02)00189-4. [DOI] [PubMed] [Google Scholar]