Abstract
Background
We investigated social inequalities in walking speed in early old age.
Methods
Walking speed was measured by 8 ft (2.44 m) timed test in 6345 individuals, mean (SD) age 61.1 (6.0) years. Current or last known Civil Service employment grade defined socioeconomic position.
Results
Mean (SD) walking speed was 1.36 (0.29) m/s in men and 1.21 (0.30) in women. Average age- and ethnicity-adjusted walking speed was approximately 13% higher in the highest employment grade compared to the lowest. Based on the relative index of inequality (RII), the difference in walking speed across the social hierarchy was 0.15 m/s (95% CI 0.12–0.18) in men and 0.17 (0.12–0.22) in women, corresponding to an age-related difference of 18.7 (13.6–23.8) years in men and 14.9 (9.9–19.9) years in women. The RII for slow walking speed (logistic model for lowest sex-specific quartile versus others) adjusted for age, sex and ethnicity was 3.40 (2.64–4.36). Explanatory factors for the social gradient in walking speed included SF-36 physical functioning, labor market status, financial insecurity, height and BMI. Demographic, psychosocial, behavioral, biological and health factors in combination accounted for 40% of social inequality in walking speed.
Conclusions
Social inequality in walking speed is substantial in early old age, and reflects many factors beyond the direct effects of physical health.
Keywords: Age Factors, Aged, Male, Middle Aged, Sex Factors, Social Class, Body Mass Index, Cohort Studies, Cross-Sectional Studies, Employment, Female, Gait, Health Behavior, Health Status, Humans, London
Life expectancy has increased dramatically in recent decades, but the extent of this health gain is dependent on socioeconomic position. 1 Disability-free life expectancy appears not to be increasing as fast as life-expectancy in rich countries, with the prospect that large segments of such populations will experience a considerable period of functional limitation in their later decades. 2–4 In the USA, there is a steep inverse social gradient in self-reported functional limitation above age 55 across the full range of income. 5 In the UK, occupational status is strongly predictive of reported disability and severe limitation in physical functioning after retirement age.6
Walking speed is a simple performance-based measure of physical functioning. Low walking speed predicts mortality in older persons.7 In a battery of three tests – standing balance, chair rises and walking speed over eight feet – the walking speed test was most closely related to future disability in previously non-disabled older people.8
We measured walking speed in the Whitehall II study of British civil servants for the first time when participants were aged 50 to 74 years. Between these ages, inequalities in self-reported physical health became wider in the cohort.9 Our cross-sectional analysis has the following objectives. First, to describe age, sex and social differences in walking speed. Second, to identify psychosocial, behavioral, biological and health correlates of walking speed and third, to investigate the extent to which such correlates account for the observed social inequalities in walking speed.
Methods
Participants
The Whitehall II study is a longitudinal study of 10,308 male and female civil servants (initially aged 35–55) based in London and set up in 1985. The response rate was 73%.10 We analyzed the seventh phase (2002–4, n=6914) of the study, when 6483 participants attended the research clinic (n=5742) or were visited at home by a nurse (n=741). The analysis is based on 6345 individuals who completed the walking speed test (97.9% of the eligible sample). The participation rate was 64.9%, taking account of 537 deaths by the mid-point of the clinic phase. Attrition between phases 1 and 7 was higher in lower employment grades (high grades 26.3%, intermediate grades 32.2%, low grades 53.1%). Small proportions of the sample defined themselves of South Asian (n=291, 4.6%), Afro-Caribbean (n=166, 2.6%) or other non-European ethnicity (n=93, 1.5%), with the rest of the cohort being of European origin.
Walking speed
Walking speed was measured by a trained nurse over a clearly marked eight foot walking course using a standardized protocol.11 Participants wore either low-heeled close-fitting footwear or walked barefoot. Prior to the test, participants were shown the walking course and asked to “walk to the other end of the course at your usual walking pace, just as if you were walking down the street to go the shops. Walk all the way past the other end of the tape before you stop”. The starting position was standing with both feet together at the start of the course. Participants were asked to begin walking when properly positioned. The stopwatch was started as the participant’s foot hit the floor across the starting line. Nurses walked behind and to the side of the participant and stopped timing when the participant’s foot hit the floor after the end of the walking course.
Three tests were conducted and the fastest walk was used in the analysis. Pairwise correlations between measurements were between 0.92 and 0.95. The difference between the fastest walk speed and the mean of the two other measurements (mean (SD) men 0.119 (0.096), women 0.117 (0.092) m/s) was unrelated to employment grade in men and weakly related in women (mean age-adjusted difference 0.017 m/s (0.18xSD) smaller in low versus high grade).
Employment grade
Socioeconomic position was measured as current or last known employment grade. Self-reported grade title was classified into six levels, defining a clear hierarchy of salary and pension entitlement.10
Health status and other covariates
Prevalent coronary heart disease (non-fatal myocardial infarction or angina pectoris: CHD) was identified by self-report or electrocardiogram with confirmation from medical records. Prevalent diabetes was defined by self-report (doctor diagnosis and/or diabetic medication) or research clinic oral glucose tolerance test (1999 WHO classification). Longstanding illnesses were identified by self-report and coded to ICD-10. Musculoskeletal disorders were defined as diseases of the musculoskeletal system and connective tissue including arthropathies, osteoporosis with and without fracture, and fibromyalgia (M00–M99) plus complications of internal orthopedic prosthetic devices (T84) and falls (W00–W19). Chronic respiratory illness included bronchitis, emphysema, chronic obstructive pulmonary disease, bronchiectasis and asthma (J40 –J47). Self-reported peripheral arterial disease (I73) was rare (men n=9, women n=4) and not included in the analysis. The physical function scale is one of eight component scales derived from the UK version of the SF-36 questionnaire. 12 Height, weight and waist circumference were measured in standardized fashion with participants dressed in a cloth gown and underclothes. 13 Lung function was measured by portable flow spirometry. The highest of three measurements was used to define forced expiratory volume in one second (FEV1) and forced vital capacity (FVC).
Labor market status was derived from responses to questions on employment, retirement and disability. Social network score was based on number and frequency of contacts with relatives and friends. Quality of the nominated closest relationship was defined in three components: practical, confiding and negative aspects of support received. Time urgency/impatience score was based on three items from the Framingham type A questionnaire (upset waiting, agitated or irritated by slow people, agitated or irritated when queuing). These items loaded uniquely onto a single factor in principal components analysis with orthogonal rotation. Financial insecurity (none/minor/major) was computed from items about difficulties paying bills and affording food or clothing for the family. Physical activity measurement was based on recording activities in the past four weeks in four categories (sport, gardening, home improvements and housework) which were assigned standard energy expenditure levels.14 Exercise intensity was categorized into three groups: light, <3 cal/kg/h; moderate, 3–6 cal/kg/h; vigorous, >6 cal/kg/h. All measures were administered at phase 7 except time urgency/impatience (phase 1).
Statistical methods
Participants were assigned to one of five age-groups (50–54, 55–59, 60–64, 65–69, 70–73 years) and one of four BMI groups (15.1–20, 20.1–25, 25.1–30, 30.1–57.1 kg/m2). A two-level indicator (50–59, 60–73 years) was used to examine differences between younger and older participants. A small, quadratic, deviation from a linear association between age in years and walking speed was observed in women. ANOVA was used to test group differences and trends in mean walking speed for the selected covariates. Mean walking speed by employment grade (Figure 1B) was estimated by linear regression using dummy variables for each sex-grade combination with adjustment for age (linear and quadratic terms), ethnicity and test location (clinic or home), together with sex interaction terms for age and ethnicity.
Figure 1.
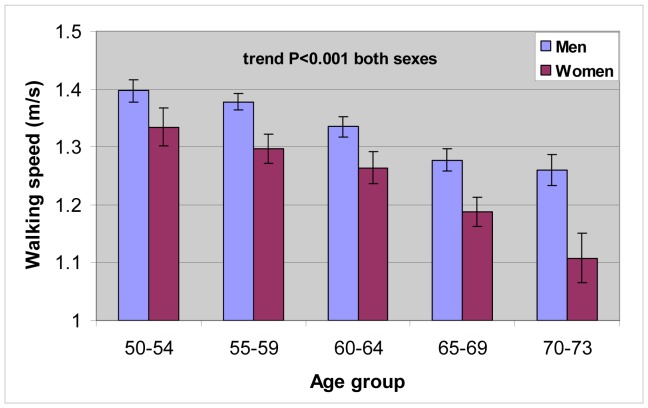
Figure 1A Mean Walking Speed With 95% Confidence Interval by Age and Sex. Adjusted for Employment Grade and Ethnicity.
Interaction between sex and age (p=0.03)
Regression model controls for test location (clinic or home).
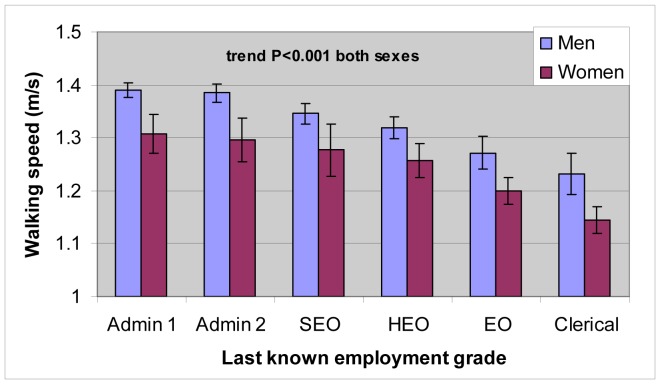
Figure 1B Mean Walking Speed With 95% Confidence Interval by Employment Grade and Sex. Adjusted for Age and Ethnicity.
No interaction between sex and grade (p=0.76).
The sample size in each group, highest to lowest grade, was for men: 1377, 1079, 801, 675, 374, 183; and for women: 235, 188, 174, 301, 435, 523
Walking speed adjusted to age 61. Model controls for test location (clinic or home).
Admin 1, high-ranking administrative personnel; Admin 2, adminstrative personnel; SEO, senior executive officer; HEO, higher executive officer; EO, executive officer
Quartiles of sex-specific walking speed were used to create binary indicators for the fastest and slowest 25% of walkers, versus the remainder of the sample. Fast walking may be subject to motivational influence while slow walking is relevant to loss of function. The relative index of inequality for grade (RII) was computed based on six levels of employment grade. 15 The RII method uses all observations to summarize inequality and takes account of differing distributions of men and women across grades. Each participant was assigned a grade score between zero (highest socioeconomic position) and one (lowest position), based on the proportion of the sample in each grade category. The score was used in a linear or logistic regression model to estimate the RII: the mean difference in walking speed or the odds ratio of being a slow walker between the extremes of the grade hierarchy (bottom versus top). The base model included the grade score and terms for sex, age (linear and quadratic), ethnicity and test location together with the sex interaction terms for age and ethnicity. The difference in mean walking speed according to socioeconomic position, expressed in years of age, was calculated as the ratio of regression coefficients for grade score (RII) and age, controlling for ethnicity and test location. The variance of the ratio of regression coefficients was calculated from their respective regression coefficients and variances using a standard formula.
For both the linear and logistic regression models, the effect on the RII of including risk factors of interest, singly or in groups, into the base model was assessed by calculating the attenuation (percentage reduction) in the mean difference in walking speed (linear model) or log odds ratio for slow walking (logistic model). This analysis included 5701 participants (89.9% of the sample) with complete data. Due to missing spirometry data, models including lung function were run separately in a smaller complete cases analysis (n=4266, 67.2% of the sample).
Results
The mean (SD) age of the sample was 61.1 (6.0) years. Under one third of participants were female (n=1856, 29.3%). Mean body mass index was in the overweight category (26.7 kg/m2). There were few current smokers (n=725, 12.1%) and less than half of participants reported they engaged in any vigorous physical activity (n=2487, 40.0%). Around one tenth of participants had diagnosed or screen-detected CHD (n=703, 11.1%) or diabetes (n=535, 8.4%). The mean (SD) SF-36 physical function scale score (range 0–100) was 84.5 (18.3). Musculoskeletal disorders and chronic respiratory illnesses were reported by 18.2% (n=1146) and 4.6% (n=290) of participants respectively.
Mean (SD) walking speed was higher in men (1.36 (0.29) m/s) than women (1.21 (0.30) m/s, difference P<0.001) (3.04 (0.64), 2.71 (0.67) mile/h respectively). Adjusting for grade, ethnicity and test location, mean walking speed declined with age, the difference being more marked in women (figure 1A). Mean walking speed was directly related to employment grade, with a similar relative difference in men and women of some 13% between highest and lowest grade (figure 1B). A similar grade effect was obtained if the mean of the two slower walking speed measurements was used instead of the fastest.
The social difference in walking speed, based on the RII was equivalent to 18.7 (95% CI: 13.6–23.8) years of age in men, and 14.9 (9.9–19.9) years in women with adjustment for ethnicity and test location. Controlling additionally for height, the respective social differences were 18.5 (13.1–24.0) and 14.4 (8.9–19.8). The age equivalent social difference among European participants only was similar in men (18.8 years) and slightly less in women (13.7 years). Social inequalities in mean speed, and odds of fast or slow walking did not differ between younger and older participants (all interactions P>0.3). Among men, the odds ratio for fast walking using the RII tended to be greater in magnitude in older versus younger participants (odds ratio (95% CI) 0.38 (0.24–0.58) versus 0.47 (0.32–0.69)). The RII for slow walking, based on a logistic model adjusted for age, sex and ethnicity was 3.40 (2.64–4.36).
Mean walking speed according to demographic and psychosocial factors, health and physical functioning, height and adiposity, and behavioral factors is reported in table 1. Care should be taken in interpreting the test statistics for trend and heterogeneity in consideration of multiple comparisons. Mean walking speed varied according to ethnicity. Adjustment for height reduced ethnic differences by about 5%. There were few ethnic minority participants in higher employment grades and no further analysis of ethnic differences was conducted. Higher mean walking speed was associated with married/cohabiting versus single status, working versus retired labor market status, financial security versus insecurity, high level of practical support (women only) and low level of negative aspects of support from closest person (men only). Mean walking speed was lower in those with CHD and diabetes, self-reports of musculoskeletal disorders and chronic respiratory illness (women only). Mean walking speed was directly related to lung function and SF-36 physical function. Self-reported musculoskeletal conditions were strongly associated with SF36 physical functioning. Mean SF-36 physical function quartile scores (range 0–3) for presence versus absence of self-report were 1.18 v. 2.08 in men and 0.88 v. 1.83 in women (both sexes, difference P<0.001). Higher mean walking speed was associated with height, low BMI, never smoking, levels of moderate and vigorous exercise in both sexes, and light exercise in women only. Time urgency/impatience was associated with faster walking and inversely associated with slower walking in women only (sex*impatience interaction P=0.11 for fastest quartile, P=0.008 for slowest quartile)(data not shown).
Table 1.
Mean Walking Speed (m/s) According to Selected Characteristics of the Sample
| MEN (N=4489) | WOMEN (N=1856) | |||||||
|---|---|---|---|---|---|---|---|---|
| N | mean | SD | Test P | N | mean | SD | Test P | |
|
|
|
|||||||
| Demographic and psychosocial | ||||||||
| Ethnicity | ||||||||
| White | 4201 | 1.37 | 0.28 | 1594 | 1.23 | 0.30 | ||
| South Asian | 178 | 1.14 | 0.31 | 113 | 1.04 | 0.25 | ||
| Black | 58 | 1.24 | 0.29 | 108 | 1.05 | 0.26 | ||
| Other | 52 | 1.22 | 0.32 | <0.001 | 41 | 1.10 | 0.26 | <0.001 |
| Marital status | ||||||||
| Married/cohabiting | 3706 | 1.37 | 0.28 | 1057 | 1.22 | 0.29 | ||
| Single/divorced/widowed | 757 | 1.33 | 0.29 | 0.003 | 779 | 1.19 | 0.31 | 0.017 |
| Labor market status | ||||||||
| working | 2394 | 1.40 | 0.27 | 781 | 1.30 | 0.28 | ||
| retired | 1864 | 1.31 | 0.28 | 924 | 1.14 | 0.29 | ||
| unemployed | 155 | 1.34 | 0.34 | 101 | 1.24 | 0.29 | ||
| long term sick/not working | 58 | 1.10 | 0.36 | <0.001 | 41 | 0.96 | 0.34 | <0.001 |
| Financial insecurity | ||||||||
| never/rarely | 3159 | 1.38 | 0.28 | 1150 | 1.24 | 0.29 | ||
| seldom | 806 | 1.32 | 0.29 | 384 | 1.17 | 0.28 | ||
| sometimes/always | 452 | 1.30 | 0.30 | <0.001* | 279 | 1.16 | 0.33 | <0.001* |
| Social network scale | ||||||||
| tertile 1 | 1072 | 1.35 | 0.29 | 425 | 1.22 | 0.31 | ||
| tertile 2 | 1479 | 1.36 | 0.28 | 671 | 1.23 | 0.30 | ||
| tertile 3 | 1766 | 1.37 | 0.28 | 0.14* | 652 | 1.20 | 0.29 | 0.11* |
| Practical support (closest person) | ||||||||
| tertile 1 | 849 | 1.35 | 0.28 | 583 | 1.23 | 0.30 | ||
| tertile 2 | 1247 | 1.37 | 0.28 | 455 | 1.22 | 0.29 | ||
| tertile 3 | 2256 | 1.36 | 0.29 | 0.85* | 729 | 1.20 | 0.30 | 0.015* |
| Confiding support (closest person) | ||||||||
| tertile 1 | 1386 | 1.35 | 0.27 | 581 | 1.21 | 0.29 | ||
| tertile 2 | 1119 | 1.38 | 0.29 | 512 | 1.21 | 0.29 | ||
| tertile 3 | 1845 | 1.36 | 0.29 | 0.56* | 673 | 1.22 | 0.31 | 0.50* |
| Negative support (closest person) | ||||||||
| tertile 1 | 716 | 1.37 | 0.29 | 305 | 1.20 | 0.32 | ||
| tertile 2 | 2104 | 1.38 | 0.28 | 791 | 1.22 | 0.28 | ||
| tertile 3 | 1526 | 1.34 | 0.29 | <0.001* | 668 | 1.21 | 0.30 | 0.86* |
| Health and physical functioning | ||||||||
| Angina or MI | ||||||||
| no | 3969 | 1.37 | 0.28 | 1673 | 1.22 | 0.30 | ||
| yes | 520 | 1.28 | 0.31 | <0.001 | 183 | 1.09 | 0.29 | <0.001 |
| Diabetes | ||||||||
| no | 4134 | 1.37 | 0.28 | 1676 | 1.22 | 0.30 | ||
| yes | 355 | 1.28 | 0.31 | <0.001 | 180 | 1.09 | 0.30 | <0.001 |
| FEV1 | ||||||||
| low | 819 | 1.30 | 0.29 | 367 | 1.10 | 0.27 | ||
| 2nd quartile | 822 | 1.37 | 0.27 | 381 | 1.18 | 0.27 | ||
| 3rd quartile | 827 | 1.41 | 0.28 | 373 | 1.26 | 0.28 | ||
| high | 852 | 1.42 | 0.27 | <0.001* | 379 | 1.36 | 0.29 | <0.001* |
| SF36 physical functioning | ||||||||
| low | 988 | 1.22 | 0.30 | 381 | 0.96 | 0.28 | ||
| 2nd quartile | 464 | 1.34 | 0.25 | 445 | 1.21 | 0.25 | ||
| 3rd quartile | 767 | 1.39 | 0.27 | 481 | 1.28 | 0.26 | ||
| high | 2201 | 1.42 | 0.27 | <0.001* | 512 | 1.34 | 0.27 | <0.001* |
| Musculoskeletal disorders | ||||||||
| no | 3761 | 1.37 | 0.28 | 1402 | 1.24 | 0.28 | ||
| yes | 703 | 1.31 | 0.31 | <0.001 | 443 | 1.11 | 0.32 | <0.001 |
| Chronic respiratory illness | ||||||||
| no | 4279 | 1.36 | 0.29 | 1740 | 1.21 | 0.30 | ||
| yes | 185 | 1.34 | 0.28 | 0.42 | 105 | 1.13 | 0.32 | 0.005 |
| Height and adiposity | ||||||||
| Height (m) | ||||||||
| quartile 1 | 1112 | 1.29 | 0.29 | 463 | 1.13 | 0.28 | ||
| quartile 2 | 1069 | 1.36 | 0.27 | 438 | 1.19 | 0.30 | ||
| quartile 3 | 1167 | 1.38 | 0.27 | 487 | 1.22 | 0.27 | ||
| quartile 4 | 1137 | 1.41 | 0.30 | <0.001* | 462 | 1.29 | 0.32 | <0.001* |
| Body mass index (kg/m2) | ||||||||
| 15.1–20 | 103 | 1.40 | 0.28 | 93 | 1.28 | 0.30 | ||
| 20.1–25 | 1517 | 1.39 | 0.30 | 637 | 1.29 | 0.29 | ||
| 25.1–30 | 2153 | 1.36 | 0.27 | 658 | 1.19 | 0.28 | ||
| 30.1–57.1 | 704 | 1.29 | 0.30 | <0.001* | 460 | 1.11 | 0.29 | <0.001* |
| Health behaviors | ||||||||
| Smoking status | ||||||||
| never smoker | 1926 | 1.39 | 0.29 | 917 | 1.23 | 0.30 | ||
| ex-smoker | 1835 | 1.34 | 0.27 | 575 | 1.21 | 0.30 | ||
| current smoker | 542 | 1.31 | 0.28 | <0.001 | 183 | 1.19 | 0.29 | 0.27 |
| Light exercise | ||||||||
| quartile 1 | 1041 | 1.35 | 0.30 | 445 | 1.17 | 0.32 | ||
| quartile 2 | 1140 | 1.37 | 0.28 | 438 | 1.21 | 0.30 | ||
| quartile 3 | 1082 | 1.37 | 0.29 | 462 | 1.24 | 0.28 | ||
| quartile 4 | 1154 | 1.36 | 0.28 | 0.53* | 459 | 1.23 | 0.30 | 0.002* |
| Moderate exercise | ||||||||
| quartile 1 | 1089 | 1.33 | 0.30 | 436 | 1.13 | 0.31 | ||
| quartile 2 | 1123 | 1.36 | 0.27 | 462 | 1.21 | 0.28 | ||
| quartile 3 | 1126 | 1.38 | 0.29 | 460 | 1.23 | 0.29 | ||
| quartile 4 | 1101 | 1.37 | 0.28 | <0.001* | 458 | 1.28 | 0.29 | <0.001* |
| Vigorous exercise | ||||||||
| None | 2537 | 1.34 | 0.29 | 1197 | 1.17 | 0.29 | ||
| tertile 1 | 630 | 1.39 | 0.27 | 201 | 1.30 | 0.30 | ||
| tertile 2 | 606 | 1.41 | 0.29 | 191 | 1.24 | 0.28 | ||
| tertile 3 | 644 | 1.39 | 0.27 | <0.001* | 215 | 1.35 | 0.29 | <0.001* |
Test P value for trend if marked with asterisk, otherwise for difference or heterogeneity
Financial insecurity, difficulties paying bills or affording food/clothes (sometimes/often)
Angina or MI, confirmed angina pectoris or non-fatal myocardial infarction
Self-report or screen detected (75g oral glucose tolerance test) diabetes
FEV1, forced expiratory volume in 1 s
SF-36, Short Form 36 physical function scale score (range 0–100)
Amount of exercise in MET-h at 3 exercise intensity levels: light, <3 cal/kg/h; moderate, 3–6 cal/kg/h; vigorous, >6 cal/kg/h
dds of being a slow walker were three fold higher at the bottom of the social hierarchy compared to the top (table 2). Individual demographic and psychosocial factors accounted for <10% of the social gradient and together they explained 16%. Time urgency/impatience, allowing for the sex interaction, did not contribute to the gradient and was omitted. Prevalent CHD, diabetes, musculoskeletal and respiratory conditions, and differences in SF36 physical functioning accounted for one fifth of the gradient in mean walking speed. Differences in height and degree of obesity, and health behaviors each explained small proportions of the social gradient. Over half the social gradient remained unexplained when all covariates were included in the model. SF36 physical functioning was the largest single contributor to the gradients in both mean walking speed and slow walking. The independent contribution of physical functioning was modest when estimated by omitting the term from the full model (for mean speed 7.4% attenuation, for slow walking 4.0%). Models (n=4362) with terms for lung function (FEV1, FVC) only, obtained an attenuation of the RII of 13.4% and 10.7% compared to the base model for mean speed and slow walking respectively. The estimated independent contribution of lung function to the gradient was 3.7% and 2.4% for mean speed and slow walking respectively compared to the full models with lung function terms (40.9% and 27.2% attenuation respectively).
Table 2.
Relative Index of Inequality (95% CI) for Mean Walking Speed and Slow Walking (Lowest Sex-Specific Quartile) and Explanatory Models. Complete cases analysis, N=5701
| Mean walking speed | Slow walking | |||||
|---|---|---|---|---|---|---|
| RII | 95%CI | % attenuation | RII | 95%CI | % attenuation | |
|
|
|
|||||
| Base model | 0.145 | (0.12–0.17) | REF | 3.11 | (2.4–4.1) | REF |
| Demographic and psychosocial | ||||||
| + Marital/cohabitation status | 0.141 | (0.11–0.17) | 2.7% | 2.92 | (2.2–3.8) | 5.6% |
| + Labor market status | 0.133 | (0.11–0.16) | 8.1% | 2.88 | (2.2–3.8) | 6.8% |
| + Financial insecurity | 0.131 | (0.10–0.16) | 9.5% | 2.84 | (2.2–3.7) | 7.8% |
| + Closest person support | 0.146 | (0.11–0.17) | −1.0% | 3.12 | (2.4–4.1) | −0.3% |
| + All above | 0.121 | (0.09–0.15) | 16.4% | 2.58 | (2.0–3.4) | 16.3% |
| Health and physical functioning | ||||||
| + Myocardial Infarct/angina | 0.144 | (0.12–0.17) | 0.7% | 3.09 | (2.4–4.0) | 0.4% |
| + Type 2 diabetes | 0.142 | (0.11–0.17) | 2.0% | 3.04 | (2.3–4.0) | 1.8% |
| + SF-36 physical function | 0.116 | (0.09–0.14) | 20.2% | 2.65 | (2.0–3.5) | 14.1% |
| + Musculoskeletal disorders | 0.147 | (0.19–0.17) | −1.1% | 3.19 | (2.4–4.2) | −2.2% |
| + Chronic respiratory illness | 0.146 | (0.12–0.17) | −0.4% | 3.12 | (2.4–4.1) | −0.5% |
| + All above | 0.114 | (0.09–0.14) | 21.5% | 2.63 | (2.0–3.5) | 14.7% |
| Height and adiposity | ||||||
| + height | 0.132 | (0.10–0.16) | 9.3% | 2.84 | (2.2–3.7) | 8.1% |
| + BMI | 0.135 | (0.10–0.16) | 7.0% | 2.96 | (2.3–3.9) | 4.3% |
| + both | 0.124 | (0.10–0.15) | 14.7% | 2.74 | (2.1–3.6) | 11.0% |
| Health behaviors | ||||||
| + Smoking status | 0.138 | (0.11–0.17) | 5.0% | 2.98 | (2.3–3.9) | 3.7% |
| + Physical activity | 0.142 | (0.11–0.17) | 2.3% | 2.99 | (2.3–3.9) | 3.5% |
| + both | 0.135 | (0.11–0.16) | 6.9% | 2.87 | (2.2–3.8) | 6.9% |
| ALL | 0.087 | (0.06–0.12) | 39.8% | 2.18 | (1.6–2.9) | 31.4% |
Mean walking speed: the linear regression model estimates the relative index of inequality (RII) in m/s, i.e. the difference in mean speed across the grade hierarchy. Coefficients are shown as positive values, with lowest socioeconomic position as reference.
Slow walking speed: the logistic regression model estimates the RII as an odds ratio for occupying the slowest sex-specific quartile, across the grade hierarchy with highest socioeconomic position as reference
Base models control for sex, age (linear and quadratic effects), ethnicity and test location and allow age and ethnicity effects to differ by sex
Closest person support, practical, confiding, negative support from closest person
BMI, body mass index (weight in kilograms divided by height in meters squared)
Physical activity, light moderate and vigorous activity (MET-h)
Discussion
Walking speed in early old age is highly sensitive to socioeconomic position and to demographic, psychosocial, health, anthropometric and behavioral factors. This cross-sectional study revealed a steep and stepwise social gradient in mean walking speed in men and women, equivalent to approximately 17 years of age-related difference. More than half of the large inequality in slow walking remained unexplained after simultaneous adjustment for several important determinants of physical functioning in older people.16
Previous studies of socioeconomic position and physical performance involved participants in later old age, typically above 70 years. 17–19 We have studied a younger, high functioning group within the civil service hierarchy. The employment grade classification identifies strong gradients in educational attainment and income. 10;20 Consistent with theoretical perspectives on the health effects of these correlated dimensions of socioeconomic status, we found evidence for a diverse set of influences on physical performance, indexed by walking speed.21 Among these, financial insecurity accounted for a substantial proportion of the social difference in mean walking speed. This finding adds to parallel observations of the effects of financial insecurity on self-rated health and longstanding illness.22
Social integration and support are important psychosocial influences on quality of life and health in older people. 23;24 Here, the effect of social network size was not evident, while quality of the nominated closest relationship was modestly related to walking speed. Neither of these factors helped to explain social inequality in walking speed. Psychosocial factors may play a role in the observed attenuating effect of marriage/cohabitation on the social gradient in slow walking. A high level of social ties has been shown to be protective of future physical function in older people.25 In our cross-sectional study we were unable to identify this effect or the alternative, the impact of prior functional status on social integration.
Social inequality in walking speed around age 60 has social and biological origins earlier in life. Adult height, reflecting childhood nutrition and other early circumstances, is associated with higher employment grade and it accounted for almost one tenth of social inequalities in slow walking. The influence of long-term behavioral patterns is evident in the explanatory effects of smoking and BMI for the gradient. Social patterning of health behaviors, for example differential rates of quitting smoking, can be traced to childhood circumstances.26 Disparities in incidence of chronic disease are among the important consequences of the long-term social gradient in risk profile.13;27 In this young healthy group prevalent CHD and diabetes account for small proportions of the slow walking gradient. Peripheral arterial disease may emerge as an additional explanatory factor but clinical disease at this phase was rare.28 Lung function was strongly linked to walking speed in our sample. It contributed to the gradient in slow walking above the adjustments for physical functioning, self-reported respiratory illness, smoking status and physical activity (10.3%, data not shown).
Musculoskeletal conditions and other lower limb disorders are reflected in the SF-36 physical functioning score, which was strongly correlated with walking speed. This variable accounted for the largest proportion of social inequality in mean walking speed and in slow walking. Physical performance is the final common pathway of many cumulative processes, including sedentary lifestyle, physiologic impairments and disease, all of which are related to low socioeconomic position. However, prevalent chronic disease, lung function and physical functioning together explained a modest proportion of the gradient, emphasizing that social inequality in walking speed only partially reflects direct influences of physical health. Similarly, in the first Whitehall study, the socioeconomic gradient in reported severe limitation in physical functioning after retirement age was largely unexplained by the presence of chronic disease.6
Social inequality in mean walking speed was calculated as the equivalent in years of age-related decline. This best-available estimate assumes the cross-sectional relation between age and walking speed is a valid estimate of the decline in walking speed in the aging cohort, and will be tested when longitudinal data become available. Further, this cross-sectional study does not shed light on changes in social inequality in walking speed with age. We found that absolute social differences in mean walking speed were similar in younger and older participants, although the RII for fast walking tended to be larger among older men. This may herald widening relative inequality in physical functioning with age, as we show with self-report 9, or may reflect a cohort effect. Our findings are based on a sample of current or former office workers. The completion rate of the walking speed test among those who participated at phase 7 was high. Overall, the phase 7 participation rate was acceptable (65%), however loss to follow up was related to social position. This selective loss may result in an underestimate of the walking speed gradient, since non-participants are less healthy than participants.29 The magnitude of this underestimation cannot be estimated with any certainty. Generalizing to the whole population including manual workers, it is likely that greater social inequality in walking speed would be observed. A history of manual work is associated with poor physical functioning in old age 18 and the social distribution of chronic disease tends to increase the social gradient in physical functioning among older people.30
In conclusion, we conducted a large study of social inequality in walking speed using a timed 8 foot test in early old age. We anticipated that traits of time urgency and impatience might contribute to the relation between socioeconomic position and walking speed. This was not the case. However, the impact of financial insecurity is consistent with a motivational influence on the ‘objective’ walking speed measure and its social gradient. The striking inverse association between socioeconomic position and walking speed is established by the sixth decade, equivalent to 17 years of age-related difference. Contemporaneously measured demographic, psychosocial, biological, behavioral and health factors, reflecting socially patterned exposures over the life course, accounted for approximately one third of the observed social inequality in walking speed. Further studies will take account of additional factors relevant to physical functioning and its age-related decline, particularly cardiovascular risk factors and cognitive function. 31;32
Reference List
- 1.Office for National Statistics. National Statistics website. 2007. Trends in Life Expectancy by social class 1972–2005. [Google Scholar]
- 2.Schoeni RF, Martin LG, Andreski PM, Freedman VA. Persistent and growing socioeconomic disparities in disability among the elderly: 1982–2002. Am J Public Health. 2005;95(11):2065–2070. doi: 10.2105/AJPH.2004.048744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huisman M, Kunst AE, Mackenbach JP. Socioeconomic inequalities in morbidity among the elderly; a European overview. soc sci med. 2003;57(5):861–873. doi: 10.1016/s0277-9536(02)00454-9. [DOI] [PubMed] [Google Scholar]
- 4.Ferrucci L, Giallauria F, Guralnik JM. Epidemiology of aging. Radiol Clin North Am. 2008;46(4):643–52. doi: 10.1016/j.rcl.2008.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med. 2006;355(7):695–703. doi: 10.1056/NEJMsa044316. [DOI] [PubMed] [Google Scholar]
- 6.Breeze E, Fletcher AE, Leon DA, Marmot MG, Clarke RJ, Shipley MJ. Do socioeconomic disadvantages persist into old age? Self-reported morbidity in a 29-year follow-up of the Whitehall Study. Am J Public Health. 2001;91(2):277–283. doi: 10.2105/ajph.91.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melzer D, Lan TY, Guralnik JM. The predictive validity for mortality of the index of mobility-related limitation--results from the EPESE study. Age Ageing. 2003;32(6):619–625. doi: 10.1093/ageing/afg107. [DOI] [PubMed] [Google Scholar]
- 8.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55(4):M221–M231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 9.Chandola T, Ferrie JE, Sacker A, Marmot M. Social inequalities in self reported health in early old age: follow-up of prospective cohort study. Br Med J. 2007;334(7601):990–994. doi: 10.1136/bmj.39167.439792.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marmot MG, Brunner EJ. Cohort Profile: The Whitehall II study. Int J Epidemiol. 2005;34(2):251–256. doi: 10.1093/ije/dyh372. [DOI] [PubMed] [Google Scholar]
- 11.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol Med Sci. 1994;49:M85–M94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 12.Hemingway H, Nicholson A, Stafford M, Roberts R, Marmot M. The impact of socioeconomic status on health functioning as assessed by the SF-36 questionnaire: the Whitehall II study (see comments) Am J Public Health. 1997;87:1484–1490. doi: 10.2105/ajph.87.9.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brunner EJ, Marmot MG, Nanchahal K, Shipley MJ, Stansfeld SA, Juneja M, et al. Social inequality in coronary risk: central obesity and the metabolic syndrome. Evidence from the Whitehall II study. Diabetologia. 1997;40(11):1341–1349. doi: 10.1007/s001250050830. [DOI] [PubMed] [Google Scholar]
- 14.Rennie KL, Hemingway H, Kumari M, Brunner E, Malik M, Marmot M. Effects of moderate and vigorous physical activity on heart rate variability in a British study of civil servants. Am J Epidemiol. 2003;158(2):135–143. doi: 10.1093/aje/kwg120. [DOI] [PubMed] [Google Scholar]
- 15.Kunst AE, Mackenbach JP. The size of mortality differences associated with educational level in nine industrialized countries. Am J Public Health. 1994;84:932–937. doi: 10.2105/ajph.84.6.932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci & Med. 1999;48:445–469. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 17.Coppin AK, Ferrucci L, Lauretani F, Phillips C, Chang M, Bandinelli S, et al. Low socioeconomic status and disability in old age: evidence from the InChianti study for the mediating role of physiological impairments. J Gerontol A Biol Sci Med Sci. 2006;61(1):86–91. doi: 10.1093/gerona/61.1.86. [DOI] [PubMed] [Google Scholar]
- 18.Russo A, Onder G, Cesari M, Zamboni V, Barillaro C, Capoluongo E, et al. Lifetime occupation and physical function: a prospective cohort study on persons aged 80 years and older living in a community. Occup Environ Med. 2006;63(7):438–442. doi: 10.1136/oem.2005.023549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rautio N, Heikkinen E, Ebrahim S. Socio-economic position and its relationship to physical capacity among elderly people living in Jyvaskyla, Finland: five- and ten-year follow-up studies. Soc Sci Med. 2005;60(11):2405–2416. doi: 10.1016/j.socscimed.2004.11.029. [DOI] [PubMed] [Google Scholar]
- 20.Roberts R, Brunner EJ, White I, Marmot MG. Gender differences in occupational mobility and structure of employment in the British civil service. Social Science & Medicine. 1993;37:1415–1425. doi: 10.1016/0277-9536(93)90175-4. [DOI] [PubMed] [Google Scholar]
- 21.Zimmer Z, House JS. Education, income, and functional limitation transitions among American adults: contrasting onset and progression. Int J Epidemiol. 2003;32(6):1089–1097. doi: 10.1093/ije/dyg254. [DOI] [PubMed] [Google Scholar]
- 22.Ferrie JE, Shipley M, Davey-Smith G, Stansfeld S, Marmot MG. Future uncertainty and socioeconomic inequalities in health: the Whitehall II study. Soc Sci Med. 2003;57:637–646. doi: 10.1016/s0277-9536(02)00406-9. [DOI] [PubMed] [Google Scholar]
- 23.Berkman LF, Glass T, Brissette I, Seeman TE. From social integration to health: Durkheim in the new millennium. Soc Sci Med. 2000;51:843–857. doi: 10.1016/s0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 24.House JS. Understanding social factors and inequalities in health: 20th century progress and 21st century prospects. J Health Soc Behav. 2002;43(2):125–142. [PubMed] [Google Scholar]
- 25.Unger JB, McAvay G, Bruce ML, Berkman L, Seeman T. Variation in the impact of social network characteristics on physical functioning in elderly persons: MacArthur Studies of Successful Aging. J Gerontol B Psychol Sci Soc Sci. 1999;54(5):S245–S251. doi: 10.1093/geronb/54b.5.s245. [DOI] [PubMed] [Google Scholar]
- 26.Brunner EJ, Shipley MJ, Blane D, Davey Smith G, Marmot MG. When does cardiovascular risk start? Past and present socioeconomic circumstances and risk factors in adulthood. J Epidemiol Community Health. 1999;53(12):757–764. doi: 10.1136/jech.53.12.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kumari M, Head J, Marmot M. Prospective study of social and other risk factors for incidence of type 2 diabetes in the Whitehall II study. Arch Intern Med. 2004;164(17):1873–1880. doi: 10.1001/archinte.164.17.1873. [DOI] [PubMed] [Google Scholar]
- 28.Garg PK, Liu K, Tian L, Guralnik JM, Ferrucci L, Criqui MH, et al. Physical Activity During Daily Life and Functional Decline in Peripheral Arterial Disease. Circulation. 2008 doi: 10.1161/CIRCULATIONAHA.108.791491. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ferrie JE, Kivimaki M, Singh-Manoux A, Shortt A, Martikainen P, Head J, et al. Non-response to baseline, non-response to follow-up and mortality in the Whitehall II cohort. Int J Epidemiol. 2009 doi: 10.1093/ije/dyp153. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sacker A, Head J, Bartley M. Impact of coronary heart disease on health functioning in an aging population: are there differences according to socioeconomic position? Psychosom Med. 2008;70(2):133–140. doi: 10.1097/PSY.0b013e3181642ef5. [DOI] [PubMed] [Google Scholar]
- 31.Volpato S, Ble A, Metter EJ, Lauretani F, Bandinelli S, Zuliani G, et al. High-density lipoprotein cholesterol and objective measures of lower extremity performance in older nondisabled persons: the InChianti study. J Am Geriatr Soc. 2008;56(4):621–629. doi: 10.1111/j.1532-5415.2007.01608.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kuh D, Cooper R, Hardy R, Guralnik J, Richards M. Lifetime Cognitive Performance is Associated With Midlife Physical Performance in a Prospective National Birth Cohort Study. Psychosom Med. 2009 doi: 10.1097/PSY.0b013e31818a1620. epub. [DOI] [PMC free article] [PubMed] [Google Scholar]