Abstract
Objectives:
To assess the epidemiological characteristics of prematurity and survival rate in preterm infants diagnosed at a university hospital in the Eastern province of Saudi Arabia.
Methods:
A retrospective study was carried out of 476 preterm infants who were admitted with the diagnosis of prematurity to King Fahd Hospital of the University, Al-Khobar, Saudi Arabia, between June 2008 and 2013. Demographics, birth weight, and neonatal survival rate were analyzed.
Results:
Four hundred and seventy-six preterm infants were admitted with a total prevalence of 7.5%. Descriptive analysis revealed 55% were males. Extremely preterm infants (<28 weeks’ gestation) comprised 9% and very preterm infants (28 to <32 weeks’ gestation) comprised 20%. Extremely low-birth-weight (ELBW) infants (<1000 g) comprised 11%. One hundred and fifty-seven (32%) infants were small for gestational age. Out of the total number of ELBW infants, 58% of them were discharged. The overall mortality was 7.6%. The mortality rate of male infants was 53%. The survival to discharge according to gestational age ranged from 30-97.6%.
Conclusion:
The estimated prevalence of preterm births in a university hospital in eastern province of Saudi Arabia, is consistent with various studies from different parts of the world.
Prematurity has been, and still is, one of the major causes of neonatal morbidity and mortality in intensive care units (ICUs) worldwide. It is considered the second leading cause of neonatal mortality after congenital anomalies, and a major determinant of neonatal and infant morbidity.1 Preterm birth affects almost 11.1% of all pregnancies worldwide.2 Preterm infants are at higher risk for acquiring complications that result from either anatomic or functional immaturity. A common finding on mortality and morbidity for very low birth weight infants is that the risk of developing complications decreases with increasing gestational age and birth weight.3 The survival of very low birth weight infants has improved significantly with the development of antenatal and neonatal intensive care during the last 2 decades. Among all early neonatal deaths (deaths within the first 7 days of life) that are not related to congenital malformations, 28% are due to preterm birth.4 Prematurity accounts for most admissions to ICUs in the immediate newborn period. As ICU costs are high, quantifying the prevalence and short-term complications of prematurity is crucially important to allow for rational planning, allocation of most frequent etiologies, and proper management. In 2005, a study5 estimated that the costs to the USA alone in terms of medical and educational expenditure and lost productivity associated with preterm birth were more than US$ 26.2 billion.
Although there are international published studies targeting this entity, current available studies on the incidence of prematurity from Saudi Arabia are scant. Almost all published studies from this region have not been recent and have been plagued with problems of small sample size or the lack of distinct focus on preterm infants.6-12 The few reliable quantitative figures of prematurity in Saudi Arabia emphasize the importance of such study. The aim of this study is to determine the prevalence of prematurity, retrospectively in the preterm infants who were admitted in the Eastern Province of Saudi Arabia.
Methods
The medical records of preterm infants admitted to the Neonatal Intensive Care Unit (NICU) with a diagnosis of prematurity at the King Fahd Hospital of the University, Al-Khobar, Kingdom of Saudi Arabia between June 2008 and June 2013 were reviewed retrospectively. The following variables were reviewed from their files: gestational age, gender, nationality, birth weight, mortality, and length of neonatal stay in the NICU.
The study followed the World Health Organization (WHO) definition of preterm birth as its only inclusion criteria, which is defined by any birth before 37 completed weeks of gestation, or fewer than 259 days since the first day of the woman’s last menstrual period (LMP).13 Gestational age (GA) was determined upon the first day of LMP. Preterm infants born at gestational age of 23 weeks or less, or infants with birth weight less than 400g were excluded from the study (n=8).
After obtaining ethical approval from the Institutional Review Board (IRB) of the University of Dammam, data for the study were obtained from the hospital records and exported to MS Excel for data manipulation and cleaning. The final data was exported using the Statistical Packages for Social Sciences (IBM Corp., Armonk, NY, USA) for analysis.
A search strategy was used to find prior related studies. A systematic literature search was applied to PubMed (from 2010 to present). We used a combination of controlled vocabulary and key words; prematurity, preterm births, and prematurity in Saudi Arabia. The results of the search were then reviewed by the research team. References from included studies were hand-searched to identify any additional relevant studies.
For the purpose of this study, prematurity was subdivided on the basis of gestational age into: extremely preterm (<28 weeks), very preterm (28 to <32 weeks), and moderate or late preterm (32 to <37 completed weeks of gestation).13 This is in line with best practice guidelines on the subject. Birthweight classification was based on the classification defined by the Centers for Disease Control14 as extremely low-birth-weight (ELBW) with birth weight <1000g, very low-birth-weight (VLBW) with birth weight ranging between 1000-1499g, low-birth-weight (LBW) with birth weight ranging between 1500-2499g, normal birth weight (NBW) with birth weight ranging between 2500-3999g, and high birth weight (HBW) with birth weight equals to or more than 4000g. Mortality was defined by death as a result of prematurity and/or at least one of its short-term complications during the hospitalization period. Small for gestational age was defined as birth weight below the 10th percentile for age.15
For statistical analysis, a simple descriptive analysis was used to measure the study variables. Bar charts and tables were used to summarize the study figures and results. Comparison was made between the characteristics of preterm infants based on both gestational age and birth weight. Livebirth numbers were included to determine the study’s rate of preterm births. For continuous variables, distributions were compared graphically and statistically.
Results
Over the study period, the number of live births delivered at the hospital was 6455. Based on the retrospective review of the medical reports, a total of 484 preterm infants were admitted to the NICU during this period. Eight patients were excluded from the study due to either being born at a gestational age of 23 weeks or less, or with birth weight less than 400 g. After these exclusions, the number of patients selected for the study was 476. Thirty-one infants (6.5%) were referred to our hospital from other regional hospitals. The total prevalence of preterm births was 7.5%, with 6455 live births. The distribution and rate of preterm births per year are shown in Figure 1. The preterm infants’ demographic data descriptive analysis revealed that 263 of them were males (55%), and 213 of them were females (45%). The prematurity and birth weight classifications of the study population are shown in Table 1.
Figure 1.
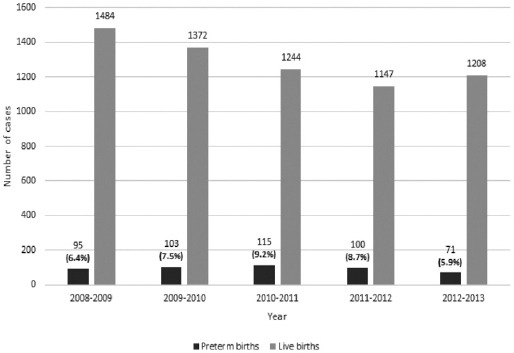
The distribution of prematurity case per year admitted to the Neonatal Intensive Care Unit (NICU) with diagnosis of prematurity at the King Fahd Hospital of the University, Al-Khobar, Kingdom of Saudi Arabia.
Table 1.
Classification of the study population according to gestational age and birth weight.
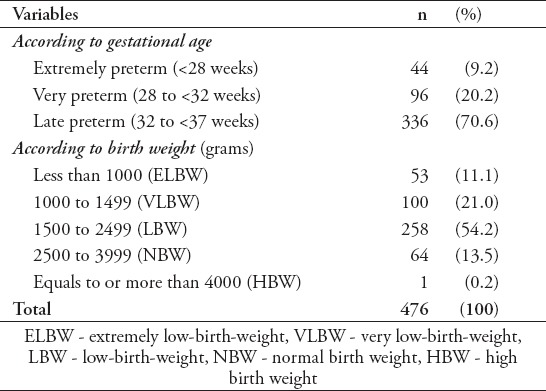
One hundred and fifty seven (32%) of our study population were small for gestational age (SGA), whereas 5 (10.9%) extreme preterm infants were SGA. The mean gestational age was 32 weeks and 4 days, whereas mean gestational age of ELBW infants was 26 weeks and 3 days with a range of 24-31 weeks. The mean birth weight of the total study population of preterm infants was 1827.6g, whereas the mean birth weight of ELBW infants was 727.83g with a range of 430g to 980g. Out of the total number of ELBW infants, 58.5% (n=31) of them were discharged from the NICU with a mean length of stay of 85.25 days and a range between 57-188 days. Out of the discharged ELBW, 45.2% (n=14) were males. The lowest birth weight of the discharged ELBW preterm infants was 580g. The overall mortality was 7.6%. The mortality rate of male preterm infants was 53%, compared with 47.2% females.
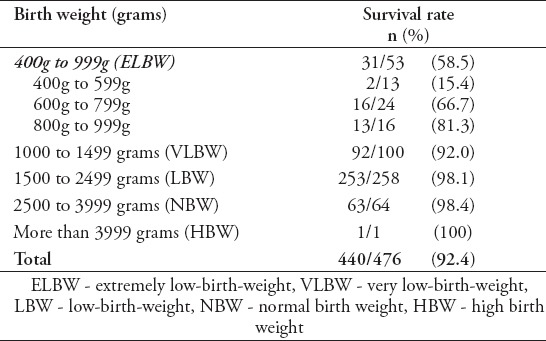
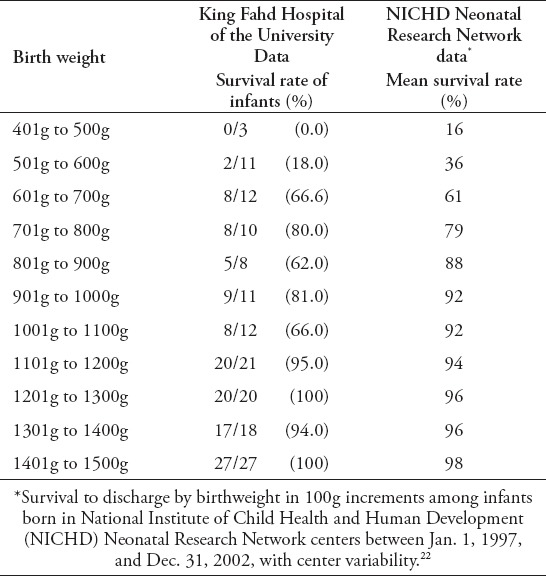
Infants with birth weights <1000g, the mortality rate was 41.5%, whereas 3.3% of infants with birth weights >1000g died prior to discharge. Furthermore, 52.7% of the mortalities occurred in infants with birth weights <800g. The survival rate per birth weight is shown in Table 2.
Table 2.
Survival by birth weight classification, with scaled survival rates among ELBW infants with 200 g increments.
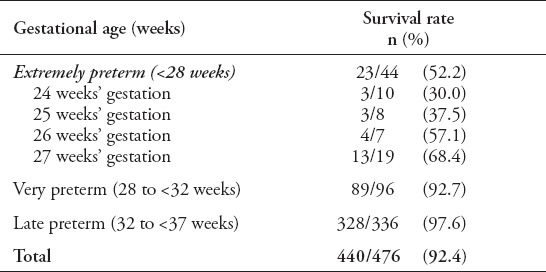
In regard to the gestational age, the survival rate per gestational age is shown in Table 3. The survival to discharge according to gestational age was ranging from 30-97.6%.
Table 3.
Survival by gestational age, with scaled survival rates among extremely preterm infants.
Discussion
More than one in 10 of babies born in 2010 were premature, making an estimated 14.9 million preterm infants (11.1%) of all pregnancies worldwide, of which more than 1 million died as a result of their prematurity. Most preterm births (84%, 12.5 million) occur after 32 completed weeks of gestation.2 This data represents a fundamental challenge for over-financed health, training, and social service sectors globally. Prematurity is now the second-leading cause of death in children under 5 years, and the single most important cause of death in the critical first month of life.16 As an indicator in the area of maternal and perinatal health, preterm births reflects the distinct discrepancies between different nations with regard to perinatal health, neonatal mortality rates, and survival rates.
In our study, 55.25% of the preterm infants were males, which is consistent with most other studies,17 and the cause of male predominance is not yet completely explained, but it could be related to the fetal sex hormone effects that influences the labor-inducing deliveries.18 As our study is focusing on the descriptive data of overall prematurity and LBW infants, there is no local studies to compare our finding with. We found the estimated prevalence of prematurity in this study was approximately 7.5% during the study period between 2009 and 2013. However, when comparing our data of preterm births to the data of the 10 countries with the highest numbers of preterm births according to worldwide estimates of preterm birth rates in the year 2010 for some selected countries, we found that our estimate of preterm births rate in 2010 (7.5%) is far lower than the high rates of the preterm births of those countries except for China (7.1%), which is listed as the second based on the number of preterm births, and that is due to the high number of livebirths as compared with our study.2
Our study trend of distribution of preterm infants by gestational age is higher than the international scale; with extremely preterm infants of 9.2% versus 5.2%, very preterm infants of 20.1% versus 10.4%.2 This could be explained by the fact that our hospital is a referral center for high risk cases and pregnancies, with 6.5% of our study population being outside referrals after delivery, and out of which most were below 32 weeks’ gestation. In addition, there is a good percentage of antenatal high risk pregnancies referrals as well.
One hundred and fifty seven (32%) of our study population were SGA, this finding was higher than the international trends of preterm-SGA for the top 10 low-income and middle-income countries with the highest numbers of SGA infants born in 2010 as found by Lee et al19 (ranging between 22.3% and 16%), and this difference can be explained as a result of being a referral hospital for high-risk pregnancies with 7.6% of our preterm-SGA being referred cases. In one study, Al-Alaiyan et al20 stated that Saudi VLBW infants are more likely to be born as small for gestational age (SGA), which might represent a genetic factor, poor maternal nutrition, or suboptimal antenatal care and follow-up. In comparison with our findings, among the total number of preterm-SGA, 26.7% were VLBW infants, whereas in another local study concerning exclusively VLBW preterm infants it was 30.2%.21 At an international level, based on perinatal information for VLBW infants born in the National Institute of Child Health and Human Development (NICHD) Neonatal Research Network between January 1997 and December 2002, the prevalence of preterm-SGA was 21%.22
Our results revealed that 92.4% of our population survived to discharge during the study period. Of the total number of ELBW infants, 58.5% of them were discharged from the NICU with a mean length of stay of 85.25 days, and 45% were male infants. With reference to gender, we found that the mortality rate was 52.7% in male preterm infants compared with 47.2% in female preterm infants. This finding of female predominance in countering the survival to discharge estimates in ELBW infants are supporting the well-established consensus adopted by Neonatal Research Network (NRN) of The Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD).23 Also, we found that the lowest birth weight of the discharged ELBW preterm infants was 580 g. In infants with birth weights below 1000 g, mortality was 41.5%, whereas 3.3% of infants with birth weights more than 1000 g died prior to discharge. Furthermore, 52.7% of the mortalities occurred in infants with birth weights below 800g.
One of the strengths of this study is that we emphasized the survival rate of our population by 2 methods based on gestational age and birth weight. Based on birth weights, preterm infants <1000 g were divided into 3 groups; those weighing 400-599g had a survival rate of 15.3%, those weighing 600-799g had a survival rate 66.6% and finally preterm infants weighing 800-999g had a survival rate of 81%, almost 4 times improvement in chance of survival compared to those less than 600g.
National Institute of Child Health and Human Development Neonatal Research Network study that was undertaken to document the mortality and morbidity of infants weighing from 501-1500 g at birth, according to gestational age, birth weight, and gender, during 2 periods (1995-1996 and 1997-2002), we compared our results with those of the NICHD and found an almost similar survival rate of preterm infants by birthweight except at birthweight of 401-500 g,22 and this is might be due to the difference between the 2 study population sizes. This comparison is shown in Table 4.
Table 4.
Survival to discharge by birthweight in 100 grams increments.
We found a continuous increasing trend of survival among preterm infants as shown in Table 2, and this is due to the marked development of antenatal and neonatal intensive care concepts regarding the implementation of strict policies and procedures, infection control measures, and evolution of applied medical practices during the last 2 decades. Also, the survival rate by gestational age varies among different groups of the population. The survival rate of preterm infants with gestational age of 24 weeks was 30%, with a major difference equalling 38% when compared to the survival rate of preterm infants with gestational age of 27 weeks (68%). A significant improvement in survival rate by gestational age was seen in preterm infants of 28 weeks’ gestation with a survival rate of 90%. The survival to discharge ranged from 30-98.4% based on gestational age. When we compared our findings of survival per gestational age to those of 3 regional hospitals in the Kingdom, we found them comparable with their results.20
The limitations of our study include the relative small number of infants enrolled. Secondly, being a referral center for high-risk cases may demonstrate slightly exaggerated figures in regards to our rates of prematurity and preterm-SGA, though we tried to emphasize our results for both groups in a separable manner. Finally, this study represents data of a single center; thus our results cannot be generalized to all preterm infants in Saudi Arabia.
In conclusion, findings of this study have estimated the prevalence of preterm births in a university hospital in the eastern province of Saudi Arabia, and compare the epidemiological characteristics of prematurity with various international studies from different parts of the world. Wide retrospective and prospective studies at a national level are needed to determine the accurate prevalence and survival rates of prematurity in Saudi Arabia.
Acknowledgment
The authors would like to acknowledge the following medical students and interns with regard to their efforts in the process of data collection (in alphabetical order): Dr. Abdulaziz Alzughaibi, Dr. Ahmed Abutalib, Dr. Ahmed Alkhalifah, Dr. Amr Alalwani, Dr. Anas Alhindi, Dr. Badriah Alomari, Dr. Danya Alkabbani, Dr. Fadi Busaleh, Dr. Latifah Almoaibed, Dr. Muhannad Almarhoon, Dr. Norah Alwakeel, Dr. Saleh Alsaeed, Dr. Sarah Bawazir, and Dr. Shaikhah Alhajre.
Footnotes
Statistics.
Excerpts from the Uniform Requirements for Manuscripts Submitted to Biomedical Journals updated November 2003.
Available from www.icmje.org
Describe statistical methods with enough detail to enable a knowledgeable reader with access to the original data to verify the reported results. When possible, quantify findings and present them with appropriate indicators of measurement error or uncertainty (such as confidence intervals). Avoid relying solely on statistical hypothesis testing, such as the use of P values, which fails to convey important information about effect size. References for the design of the study and statistical methods should be to standard works when possible (with pages stated). Define statistical terms, abbreviations, and most symbols. Specify the computer software used.
References
- 1.Heron M, Sutton P, Xu J, Ventura S, Strobino D, Guyer B. Annual Summary of Vital Statistics 2007. Pediatrics. 2010;125:4–15. doi: 10.1542/peds.2009-2416. [DOI] [PubMed] [Google Scholar]
- 2.Blencowe H, Cousens S, Oestergaard MZ, Chou D, Moller AB, Narwal R, et al. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 3.Horbar JD, Badger GJ, Carpenter JH, Fanaroff AA, Kilpatrick S, LaCorte M, et al. Trends in mortality and morbidity for Very Low Birth Weight Infants 1991-1999. Pediatrics. 2002;110(1 Pt 1):143–1451. doi: 10.1542/peds.110.1.143. [DOI] [PubMed] [Google Scholar]
- 4.Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000. Int J Epidemiol. 2006;35:706–718. doi: 10.1093/ije/dyl043. [DOI] [PubMed] [Google Scholar]
- 5.March of Dimes. PeriStats. [[Updated 2016; Accessed 2016 January]]. Available from: http://www.marchofdimes.com/peristats/
- 6.Dawodu AH, Al Umran K, Al Faraidy A. Neonatal vital statistics: A 5-year review in Saudi Arabia. Ann Trop Paediatr. 1988;8:187–192. doi: 10.1080/02724936.1988.11748567. [DOI] [PubMed] [Google Scholar]
- 7.Bassuni W, Abbag F, Asindi A, Al Barki A, Al Binali AM. Neonatal deaths in the Asir Region of Saudi Arabia: Experience in a referral neonatal intensive care unit. Ann Saudi Med. 1997;17:522–526. doi: 10.5144/0256-4947.1997.522. [DOI] [PubMed] [Google Scholar]
- 8.Nabi G, Karim MA. Predictors of neonatal mortality in the intensive care unit in Abha, Kingdom of Saudi Arabia. Saudi Med J. 2004;25:1306. [PubMed] [Google Scholar]
- 9.Arafa MA, Al Shehri MA. Predictors of neonatal mortality in the intensive care unit in Abha, Saudi Arabia. Saudi Med J. 2003;24:1374–1376. [PubMed] [Google Scholar]
- 10.Abdelmoneim I. A study of determinants of low birth weight in Abha, Saudi Arabia. Afr J Med Med Sci. 2004;33:145–148. [PubMed] [Google Scholar]
- 11.Khashoggi TY. Outcome of pregnancies with preterm premature rupture of membranes. Saudi Med J. 2004;25:1957–1961. [PubMed] [Google Scholar]
- 12.Abu-Heija AT. Maternal and neonatal outcome of high order gestation. Arch Gynecol Obstet. 2003;268:15–18. doi: 10.1007/s00404-002-0322-7. [DOI] [PubMed] [Google Scholar]
- 13.WHO: recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet Gynecol Scand. 1977;56:247–253. [PubMed] [Google Scholar]
- 14.Martin JA, Hamilton BE, Ventura SJ, Osterman MJ, Kirmeyer S, Mathews TJ, et al. Births: final data for 2009. Natl Vital Stat Rep. 2011;60:1–70. [PubMed] [Google Scholar]
- 15.Mikolajczyk RT, Zhang J, Betran AP, Souza JP, Mori R, Gülmezoglu AM, et al. A global reference for fetal-weight and birthweight percentiles. Lancet. 2011;377:1855–1861. doi: 10.1016/S0140-6736(11)60364-4. [DOI] [PubMed] [Google Scholar]
- 16.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 17.Zeitlin J, Saurel-Cubizolles MJ, De Mouzon J, Rivera L, Ancel PY, Blondel B, et al. Fetal sex and preterm birth: are males at greater risk? Hum Reprod. 2002;17:2762–2728. doi: 10.1093/humrep/17.10.2762. [DOI] [PubMed] [Google Scholar]
- 18.Cooperstock M, Campbell J. Excess males in preterm birth: interactions with gestational age, race, and multiple birth. Obstet Gynecol. 1996;88:189–193. doi: 10.1016/0029-7844(96)00106-8. [DOI] [PubMed] [Google Scholar]
- 19.Lee AC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1:e26–e36. doi: 10.1016/S2214-109X(13)70006-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Alaiyan S, Al-Abdi S, Alallah J, Al-Hazzani F, AlFaleh K. Pre-viable Newborns in Saudi Arabia: Where are We Now and What the Future May Hold? Current Pediatric Reviews. 2013;9:4–8. [Google Scholar]
- 21.Al Hazzani F, Al-Alaiyan S, Hassanein J, Khadawardi E. Short-term outcome of very low-birth-weight infants in a tertiary care hospital in Saudi Arabia. Ann Saudi Med. 2011;31:581–585. doi: 10.4103/0256-4947.87093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196:147.e1–147.e8. doi: 10.1016/j.ajog.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 23.Tyson JE, Parikh NA, Langer J, Green C, Higgins RD. Intensive care for extreme prematurity: Moving beyond gestational age. N Engl J Med. 2008;358:1672–1681. doi: 10.1056/NEJMoa073059. [DOI] [PMC free article] [PubMed] [Google Scholar]


