Abstract
Background:
Evaluating the landmarks for rotation of the distal femur is a challenge for orthopedic surgeons. Although the posterior femoral condyle axis is a good landmark for surgeons, the surgical transepicondylar axis may be a better option with the help of preoperative CT scanning. The purpose of this study was to ascertain relationships among the axes’ guiding distal femur rotational alignment in preoperative CT scans of Iranian patients who were candidates for total knee arthroplasty and the effects of age, gender, and knee alignment on these relationships.
Methods:
One hundred and eight cases who were admitted to two university hospitals for total knee arthroplasty were included in this study. The rotation of the distal femur was evaluated using single axial CT images through the femoral epicondyle. Four lines were drawn digitally in this view: anatomical and surgical transepicondylar axes, posterior condylar axis and the Whiteside anteroposterior line. The alignment of the extremity was evaluated in the standing alignment view. Then the angles were measured along these lines and their relationship was evaluated.
Results:
The mean angle between the anatomical transepicondylar axis and posterior condylar axis and between the surgical transepicondylar axis and posterior condylar axis were 5.9 ± 1.6 degrees and 1.6±1.7 degrees respectively. The mean angle between the Whiteside’s anteroposterior line and the line perpendicular to the posterior condylar axis was 3.7±2.1 degrees. Significant differences existed between the two genders in these relationships. No significant correlation between the age of patients and angles of the distal femur was detected. The anatomical surgical transepicondylar axis was in 4.3 degrees external rotation in relation to the surgical transepicondylar axis.
Conclusion:
Preoperative CT scanning can help accurately determine rotational landmarks of the distal femur. If one of the reference axes cannot be determined, other reference axes can be used because of the good correlation between these landmarks.
Keywords: Distal femur, Rotational alignment, Transepicondylar axis, Whiteside line
Introduction
The geometry of the distal femur may influence the biomechanics of the tibiofemoral and patellofemoral joint. In total knee arthroplasty, positioning of the implants in the axial plane is referred to as rotational alignment (1). Correct rotational positioning of femoral components is critical in total knee arthroplasty (TKA), because the consequences of malrotation may produce patellofemoral problems, flexion instability, stiffness, and abnormal gait patterns (2, 3). Despite the current high success rate of TKA, patellofemoral complications are a common cause of revision surgeries, and proper positioning of TKA components is vital for the functional outcome of the procedure. Although the desired positions and guiding landmarks for placement of the femoral and tibial components in the coronal and sagittal planes have been well defined, rotational positioning of the components are still a challenge (3, 4).
Femoral component malrotation especially in internal rotation is a common mistake in TKA. If the femoral component is inserted inappropriately, malrotation induces patellofemoral maltracking and flexion gap mismatch. Patellar maltracking eventually results in patella dislocation or severe limited range of motion, and flexion gap mismatch causes knee instability. These complications reduce the life span of the prosthesis and disturb the postoperative clinical outcome and patient satisfaction. Multiple researches have confirmed the relation between malrotation of the femoral component and early failure of TKA (5, 6).
An essential point is the exact rotational alignment of the distal femur during surgery. There are several reference lines to assess the rotation of the distal femur that help to make the best cut from the posterior aspect of the femoral condyles, but there is still incongruity over the lines’ significance and angular relationship (1, 7). Distal femoral references include the posterior femoral condyle axis (PCA), the surgical and anatomical transepicondylar axes (A-TEA), and the trochlear anteroposterior (Whiteside) line. The most imperious and ultimate reference for the rotation of the distal femur is the surgical transepicondylar axis (S-TEA): the line connecting the tip of the lateral epicondyle to the medial epicondylar sulcus as defined according to Berger et al. (8). It is a valid reference for both the femur and tibia, probably because it approximates the flexion-extension axis of the knee and the origin of the femoral collateral ligament, but sometimes it is difficult to identify the femoral epicondyle and medial sulcus during surgery (2). Consequently, most orthopedic surgeons prefer to use the more accessible posterior femoral condyle axis (PCA) and cut the posterior part of the femoral condyle at 3 degrees of external rotation, relative to the PCA. Although many factors such as gender, condylar hypoplasia, and coronal alignment of the extremity can disturb the rotation of the distal femur and change the angle between the PCA and transepicondylar axis from 5 degree internal rotation to 10 degree external rotation (3, 9).
Evaluation and determination of bony landmarks of the distal femur during surgery in patients with severe knee osteoarthritis is challenging; especially, if the surgeon lacks adequate skill to dissect the soft tissue around the epicondyles without collateral ligament injury. That is why preoperative CT scanning approaches have been recommended by some academics (2, 10, 11). By preoperative CT scanning, the surgeon can precisely evaluate the angles between the transepicondylar axis and anteroposterior line with the PCA; decreasing the possibility of femur malpositioning during surgery. Occasionally, determining the medial sulcus in CT scans is problematic. Even if the surgeon is patience and careful in choosing the best CT slices for sulcus identification, usually 30 mm from the joint line, the sulcus is detected in just 80% of patients, and in 20% it is impossible to find the medial sulcus and the surgeon has to use other landmarks (2, 5, 11). The more severe the arthritis, the more difficult it is to locate the sulcus (1). Therefore, assessing other axes and determining the angles between the A-TEA, S-TEA, Whiteside line, and PCA helps us to use one axis as an alternative.
The purpose of this study was to determine the relationship between the described axes guiding distal femur rotational alignment of patients with severe arthritis who were also candidates for total knee arthroplasty determined by preoperative CT scanning, and to determine if there were any effects due to age, gender and alignment of the extremity on these relationships.
Material and Methods
One hundred ten patients between 44 and 81-years-old who were candidates for total knee arthroplasty from two university hospitals during November 2012 to April 2015 were included in this case series study and their knees were assessed by spiral CT scans in these centers.
Before recruitment of the subjects, the local ethics committee of the university approved the study. The study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki. All patients signed their informed consent prior to recruitment into the study.
Patients with a history of fracture or surgery of the knee and a history of rheumatoid arthritis and other rheumatologic diseases were excluded. The standard standing long leg alignment view was obtained for all patients. The following angles were then measured: the angle between the mechanical and anatomical femoral axes (IM angle), the angle between mechanical tibial and femoral axes, lateral distal femoral angle (LDFA), medial proximal tibial angle (MTPA), and joint line convergence angle (JLCA).
We used a Siemens Somatom spirit dual CT scanner (Siemens Medical Solutions USA, Malvern, PA) for all scans in both centers. Each patient was placed in the supine position on the scanning table with the affected knee in extension, and a leg holder was used during imaging to reduce leg movement. We evaluated the rotation alignment according to Berger’s CT scanning protocol (8). A scout view was obtained, and multislice CT scans of the knees with a 1.5-mm slice thickness were obtained from the femoral distal metaphysis perpendicular to mechanical axes of the femur. Two knee surgeons individually analyzed all the scans. The rotation of the distal femur was evaluated using single axial CT images through the femoral epicondyles. This cut is 28-32 mm above the joint line where the medial sulcus is usually seen. Also, small holes related to the nutrient vessels are occasionally observed in the medial sulcus. Four lines were drawn digitally in this view on the monitor:
-
1)
Anatomical transepicondylar axis (A-TEA), which connects the lateral and medial epicondylar prominence [Figure 1],
-
2)
Surgical transepicondylar axis (S-TEA), which connects the lateral epicondylar prominence and the medial sulcus in the posterior aspect of the medial epicondyle [Figure 2],
-
3)
Posterior condylar axis (PCA), which was drawn tangent to the posterior aspect of the two epicondyles of the femur, and
-
4)
The Whiteside trochlear anteroposterior line (WAP), which connects the deepest point of the trochlear groove to the top of the femoral notch.
Figure 1.
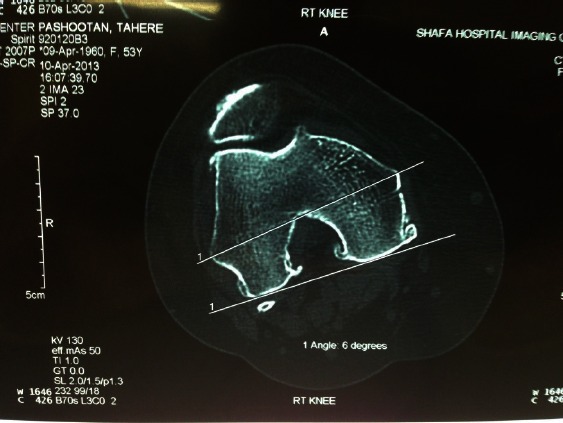
The anatomical transepicondylar axis is in 6 degrees externally rotation related to PCA in a 53-year-old female. The medial sulcus with a nutrient hole was observed posterior to the medial epicondyle (Courtesy of the archive unit of Shafa Orthopedic Hospital).
Figure 2.
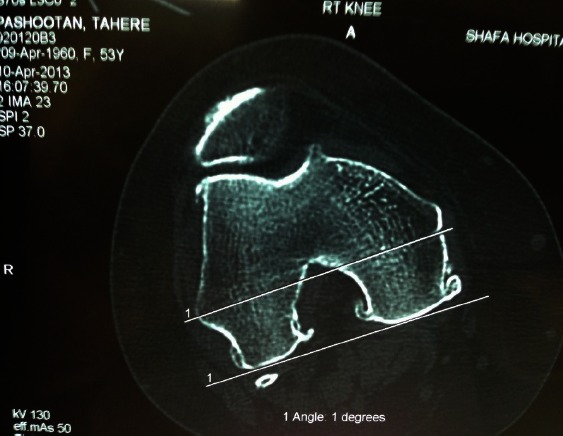
The angle between the surgical transepicondylar axis and PCA in the same case. Surgical transepicondylar axis in 1 degree external rotation related to PCA (Courtesy of the archive unit of Shafa Orthopedic Hospital).
Then we measured the angles along these lines digitally on the monitor. The posterior condylar angle was formed by the posterior condylar line and the surgical transepicondylar axis, and the condylar twist angle was formed by the posterior condylar line and the anatomical transepicondylar axis. This angle is used when the sulcus is absent on the medial side (2). We also measured the angle between the Whiteside’s line and the line perpendicular to the PCA and labeled it: WAP/PCA. Lastly, we analyzed the data and evaluated the relationship among these references line with each other and with age, sex and knee alignment.
Data were analyzed using the SPSS version 16 software, and P-value ≤ 0.05 was considered statistically significant. The mean of the angles was recorded, and the correlation between alignment and CT scan angles and among the angles, sex, and age were evaluated.
Results
Two patients were excluded from the study due to a suspicious history of rheumatologic disease. Data of 108 cases with osteoarthritis who were candidates for total knee arthroplasty were analyzed. The patients mean age was 65.15± 8.17 years old (from 44 to 81) and of these 43 patients were male and 65 were female. Right side involvement was noted in 66 cases (61.1%) and left side involvement in 42 cases (38.8%). In 82 cases (76%) only the medial compartment of the knee was severely involved and in 26 cases (24%) involvement was bilateral.
All patients had varus knee, and the measurements were recorded as such: the mean angle between the femoral and tibial axes was 16.1±7.1 degrees (varus); and the mean varus angle in male patients was 16.5±5.5 degrees and in females it was 15.9± 7.2 degrees without significant deference between the two genders (P=0.3).
The mean of other angles in the alignment view was also recorded: The mean of the LDFA was 91.4±2.8 degrees (92.1±0.5 degrees in male patients and 90.9±2.8 degrees in females). The mean of the MTPA was 81.7±3.9 degrees (81.2±4.9 degrees in male patients and 82.1±3.9 degrees in females). The mean of the JLCA was 6.4±3.8 degrees (5.6±2.1 degrees in male patients and 7.1±3.9 degrees in females). The mean of the IM angle was 6.2±0.9 degrees (6.4±0.6 degrees in males and 6.1±0.9 degrees in females). There was no significant difference between males and females in these parameters of extremity alignment.
While evaluating CT scans, we could not find the medial sulcus in 23 patients (21.3%), because of large osteophytes and severe deformation. These results were obtained from the analysis of the patients’ CT scans:
The mean condylar twist angle, means the angle between A-TEA and PCA was 5.9±1.6 degrees. The mean condylar twist angle in male patients was 7.2±1.1 degrees and in females it was 5.1±1.5 degrees with a significant difference between the two genders (P<0.001).
The mean posterior condylar angle, means the angle between the S-TEA and PCA was 1.6±1.7 degrees. The mean posterior condylar angle in male patients was 2.9±1.2 degrees and in females it was 0.7±1.5 degrees, and there was a significant difference between the two genders (P<0.001).
The mean angle between the WAP line and PCA was 3.7±2.1 degrees. The mean WAP/PCA angles in male patients was 4.4±1.5 degrees and in females it was 3.2±1.5 degrees, and there was a significant difference between males and females (P<0.001).
No significant correlation between patients’ age and findings in the alignment view and CT imaging was detected, except in posterior condylar angle and condylar twist angle. There was a significant correlation between patients’ age and the PCA (P=0.02, r=0.287), and between patients’ age and the condylar twist angle (P=0.003, r=0.383). Also, there was no significant correlation between findings in the alignment view and findings in the ST scan. In varus cases, there was not any correlation between severity of the varus and rotation of the distal femur.
There was a significant correlation between posterior condylar angle and condylar twist angle (r=0.866, P=0.001). The difference between the mean posterior condylar angle and condylar twist angle was 4.3 degrees, so the A-TEA was in 4.3 degrees external rotation related to the S-TEA in all cases (4.3±1.3 degrees in males and 4.4±1.5 degrees in females). Significant correlation existed between posterior condylar angle and WAP/PCA A (r=0.831, P<0.001), showing that the axis perpendicular to the WAP was in approximately 2.1 degree external rotation relative to the S-TEA in all cases (1.5 degrees in males and 2.5 degrees in females).
Discussion
Several studies have cited the importance of proper rotational alignment of the femoral component in TKA (1, 5, 9). Femoral component rotation determines the position of the patellar groove and flexion gap stability (12). Rotational malalignment still accounts for an unacceptable number of failures in total knee arthroplasty (1, 5). Sometimes intraoperative determination of the bony landmarks of the distal femur and identification of the secondary reference axis is difficult for surgeons (13, 14).
Berger was the first to use CT scans to evaluate the rotational alignment of the components. In 1993, he defined the surgical transepicondylar axis of the distal femur and posterior condylar angle as a reproducible secondary anatomic axis, useful to determine the rotational orientation of the femoral component of TKA. Their measurements showed a mean angle between the S-TEA and PCA was 3.5+1.2 degrees for males and 0.3 degrees for females. Compared with the A- TEA, the angles were 5.2 degrees and 4.7 degrees respectively. They showed that rotational alignment of the femoral component could be accurately estimated using the posterior condylar angle, referenced from the S-TEA (8). In a cadaveric study, Victor et al. evaluated bony landmarks of the distal femur in CT scans. They found that the horizontal plane projections of the posterior condylar line and the surgical and anatomical transepicondylar axis can be determined accurately on a CT scan with low intra- and inter-observer variability (9). Yoshioka et al. observed 32 cadaveric femoral bones and reported a small gender-based difference. They found a condylar twist angle of 5 degrees in males and 6 degrees in females (15). In another CT scan-based study, Nagamine et al. evaluated the reliability of the A-TEA and WAP line versus the PCA in normal knees and knees with osteoarthritis. They found the A-TEA to be 6+2.4 degrees externally rotated relative to the PCA. This angle was 5.8+2.7 degrees and 6.2+1.9 degrees in normal knees and involved knees, respectively (16).
We previously evaluated the rotational landmarks of the distal femur in a healthy Iranian population (17). In this study the mean angle between the S-TEA and PCA was 1.58±1.69 degrees (mean: 2.6±1.67 for males and 1±1.55 for females) (17). In the present study, the mean angle between the S-TEA and PCA in the group candidate for TKA was 1.6±1.7 degrees (mean: 2.9±1.2 degrees for males and 0.7±1.52 degrees for females). When performing the rotational adjustment, the surgeon should take into consideration the amount of worn posterior cartilage not included in the CT imaging measurements (2).
Some investigations have tried to show a correlation between the distal femur rotation and frontal alignment of the knee (18). In 2008, Aglietti et al. studied preoperative knee CT scans of 100 patients with primary osteoarthritis undergoing TKA. The researchers identified a linear relationship (P<0.001) between the posterior condylar angle and mechanical axis of the extremity. Also, the two genders had similar posterior condylar angles (mean: 2.8±1.7 degrees for females and 2.1± 1.6 degrees for men). They suggested preoperative CT scans as a helpful, simple, and relatively low cost procedure to identify relevant anatomy and to adjust rotational positioning, but not as a routine plan. They also developed a simplified formula for the relation between distal femur rotation and frontal alignment of the knee that increases the posterior condylar angle by 1 degree per 10 degrees of coronal deformity increments from the varus to the valgus (2).
We could not find any correlation between the distal femoral rotation and alignment finding. It may be because all the cases in our study were varus knee. Aglietti et al.’s study was based on osteoarthritis patients with a spectrum of frontal malalignment. Other authors have described a larger posterior condylar angle in valgus knees than in the varus (18). This reflects the lateral femoral condyle hypoplasia, which is present in valgus knees, whereas varus knee distal femur anatomy does not differ from the normal (19).
Based on Aglietti et al.’s understanding, with patience and by choosing the best CT slices for sulcus identification - usually 30 mm from the joint line - they could detect the sulcus in 80% of the patients. If the sulcus was absent on the medial side, the condylar twist angle was used instead of the posterior condylar angle (2). Yoshino et al. studied the relationship between surgical and anatomical TEA in CT scans of 48 patients with osteoarthritis. The medial sulcus could only be determined in 30% of the knees because the arthritis was more severe in the study’s patients (20).
Although CT scans shows the bony anatomy of the distal femur, its evaluation of the cartilage of the distal femur is limited (2). If it has been performed on arthritic knees, this could influence the results attributable particularly to cartilage erosion, particularly in cases with relatively good lateral knee compartment. In our study, it was not possible to find the medial sulcus in 23 CT scans (21.3%). To evaluate the distal femoral rotation in these cases, we need the size of the angle between the surgical and anatomical transepicondylar axis. Based on our findings, this angle in Iranian patients with severe osteoarthritis is approximately 4.3 degrees.
The trochlear AP axis was described by Arima and Whiteside as a reliable rotational landmark in 1995. The mean angle with a posterior condylar axis was 3.8 degrees of external rotation, but with a high range from 0.5 to 7 degrees. They reported less patellar complications when the trochlear AP axis was used as a reference than when the PCA was used (21). In Nagamine’s study, the A-TEA was 1.4+3.3 degrees externally rotated relative to the line perpendicular to the WAP axis (16).
In the current study, the mean angle between the line perpendicular to the Whiteside’s AP axis and PCA was 3.7±2.1 degrees (mean: 4.4±1.5 degrees for males and 3.2±1.5 degrees for females). The results are similar to other researches (1, 16, 18). The line perpendicular to the WAP axis was approximately 2.1 degrees externally rotated relative to the S-TEA and 2.2 degrees internally rotated relative to the A-TEA.
In 2009, Victor presented a systematic review of previously published articles about rotational alignment of the distal femur and different techniques in obtaining correct rotational alignment of the femoral component. Based on the published principles, the posterior condylar line was on average 3 degrees internally rotated relative to the S-TEA, 5 degrees relative to the A-TEA and 4 degrees relative to the perpendicular to the Whiteside line. He suggested using preoperative CT scans because of the large ranges and standard deviations of all reference axes during surgery, especially the important variability in the surgical location of the TEA (1). In a CT-scan-based study using cadavers, Victor et al. evaluated the variability of distal femur axes. Inter- and intra-observer variability in the three-dimensional CT reconstructions revealed slight angular errors ranging from 0.16 degrees to 1.15 degrees for all axes, except for the trochlear AP axis that had an inter-observer error of 2 degrees (22). In another cadaver study, they revealed slight inter and intra-observer variability in marking the transepicondylar axis on CT scans (9).
In our study, the S-TEA, A-TEA, and the line perpendicular to the Whiteside line were on average 1.6, 5.9, and 3.7 degrees externally rotated relative to the PCA respectively. These results are close to the findings of Victor et al, but unlike their study, we evaluated the effect of gender in the rotational reference axes and found significant differences between the two genders. The mean posterior condylar angle, condylar twist angle, and WAP/PCA angle are significantly higher in males than females.
Our study limitations are its small sample size and so to have accurate findings, we recommend performing investigations on larger populations. Second, the patient sampling was limited to only patients with varus knee because it is a common finding among patients who were candidate for TKA.
This study showed that in Iranian patients, inserting the femoral component of the TKA only at 3 degrees external rotation relative to the posterior condylar line may cause a mistake in rotational alignment, especially in females. Preoperative CT scanning can help determine rotational landmarks of the distal femur accurately. If one of the reference axes could not be determined in the preoperative evaluation by CT scanning or during surgery, other reference axes can be used because of a high correlation between these landmarks.
References
- 1.Victor J. Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res. 2009;95(5):365–72. doi: 10.1016/j.otsr.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 2.Aglietti P, Sensi L, Cuomo P, Ciardullo A. Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res. 2008;466(11):2751–5. doi: 10.1007/s11999-008-0452-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossi R, Bruzzone M, Bonasia DE, Marmotti A, Castoldi F. Evaluation of tibial rotational alignment in total knee arthroplasty: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2010;18(7):889–93. doi: 10.1007/s00167-009-1023-6. [DOI] [PubMed] [Google Scholar]
- 4.Zhang XL, Zhang W, Shao JJ. Rotational alignment in total knee arthroplasty: nonimage-based navigation system versus conventional technique. Chin Med J (Engl) 2012;125(2):236–43. [PubMed] [Google Scholar]
- 5.Sun T, Lv H, Hong N. Rotational landmarks and total knee arthroplasty in osteoarthritic knees. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2007;21(3):226–30. [PubMed] [Google Scholar]
- 6.Uehara K, Kadoya Y, Kobayashi A, Ohashi H, Yamano Y. Bone anatomy and rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2002;402:196–201. doi: 10.1097/00003086-200209000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Berhouet J, Beaufils P, Boisrenoult P, Frasca D, Pujol N. Rotational positioning of the tibial tray in total knee arthroplasty: a CT evaluation. Orthop Traumatol Surg Res. 2011;97(7):699–704. doi: 10.1016/j.otsr.2011.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Berger RA, Rubash HE, Seel MJ, Thompson WH, Crossett LS. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res. 1993;286:40–7. [PubMed] [Google Scholar]
- 9.Victor J, Van Doninck D, Labey L, Innocenti B, Parizel PM, Bellemans J. How precise can bony landmarks be determined on a CT scan of the knee. Knee. 2009;16(5):358–65. doi: 10.1016/j.knee.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Vaidya SV, Gadhiya RM, Bagaria V, Ranawat AS, Ranawat CS. Computed tomographic evaluation of femoral component rotation in total knee arthroplasty. Indian J Orthop. 2013;47(1):40–4. doi: 10.4103/0019-5413.106898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stiehl JB, Abbott BD. Morphology of the transepicondylar axis and its application in primary and revision total knee arthroplasty. J Arthroplasty. 1995;10(6):785–9. doi: 10.1016/s0883-5403(05)80075-0. [DOI] [PubMed] [Google Scholar]
- 12.Stiehl JB, Cherveny PM. Femoral rotational alignment using the tibial shaft axis in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:47–55. doi: 10.1097/00003086-199610000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Galaud B, Beaufils P, Michaut M, Abadie P, Fallet L, Boisrenoult P. Distal femoral torsion: comparison of CT scan and intra operative navigation measurements during total knee arthroplasty. A report of 70 cases. Rev Chir Orthop Reparatrice Appar mot. 2008;94(6):573–9. doi: 10.1016/j.rco.2008.03.039. [DOI] [PubMed] [Google Scholar]
- 14.Jenny JY, Boeri C. Low reproducibility of then intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand. 2004;75(1):74–7. doi: 10.1080/00016470410001708150. [DOI] [PubMed] [Google Scholar]
- 15.Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am. 1987;69(6):873–80. [PubMed] [Google Scholar]
- 16.Nagamine R, Miura H, Inoue Y, Urabe K, Matsuda S, Okamoto Y, et al. Reliability of the anteroposterior axis and the posterior condylar axis for determining rotational alignment of the femoral component in total knee arthroplasty. J Orthop Sci. 1998;3(4):194–8. doi: 10.1007/s007760050041. [DOI] [PubMed] [Google Scholar]
- 17.Jabalameli M, Rahbar M, Bagherifard A, Hadi HA, Moradi A, Mokhtari T. Evaluation of distal femoral rotational alignment according to transepicondylar axis and Whiteside line (A study in Iranian population) SOJ. 2013;1(3):22–28. [Google Scholar]
- 18.Griffin FM, Insall JN, Scuderi GR. The posterior condylar angle in osteoarthritic knees. J Arthroplasty. 1998;13(7):812–5. doi: 10.1016/s0883-5403(98)90036-5. [DOI] [PubMed] [Google Scholar]
- 19.Matsuda S, Miura H, Nagamine R, Mawatari T, Tokunaga M, Nabeyama R, et al. Anatomical analysis of the femoral condyle in normal and osteoarthritic knees. J Orthop Res. 2004;22(1):104–9. doi: 10.1016/S0736-0266(03)00134-7. [DOI] [PubMed] [Google Scholar]
- 20.Yosnhino N, Takai S, Ohtsuki Y, Hirasawa Y. Computed tomography measurement of the surgical and clinical transepicondylar axis of the distal femur in osteoarthritic knees. J Arthroplasty. 2001;16(4):493–7. doi: 10.1054/arth.2001.23621. [DOI] [PubMed] [Google Scholar]
- 21.Arima J, Whiteside LA, McCarthy DS, White SE. Femoral rotational alignment, based on the anteroposterior axis, in total knee arthroplasty in a valgus knee. A technical note. J Bone joint Surg Am. 1995;77(9):1331–4. doi: 10.2106/00004623-199509000-00006. [DOI] [PubMed] [Google Scholar]
- 22.Victor J, Van Doninck D, Labey L, Van Glabbeek F, Parizel P, Bellemans J. A common reference frame for describing rotation of the distal femur: a ct-based kinematic study using cadavers. J Bone Joint Surg Br. 2009;91(5):683–90. doi: 10.1302/0301-620X.91B5.21827. [DOI] [PubMed] [Google Scholar]


