Abstract
Objective
High levels of weight suppression have been associated with greater binge eating and weight gain as well as poorer treatment outcome in bulimia nervosa. This study examined the relationship between weight suppression and bulimia nervosa symptoms and explored how weight suppression might interact with body mass index (BMI) in accounting for level of symptomatology at presentation for treatment.
Method
Participants were 64 women with threshold or sub-threshold bulimia nervosa. A clinical interview assessed binge eating and purging.
Results
Weight suppression and the interaction between BMI and weight suppression predicted frequency of binge eating such that participants with low BMI and high weight suppression engaged in the most binge eating. High levels of weight suppression also predicted more frequent purging.
Discussion
Additional research is warranted to examine mediators of these relationships.
Weight suppression, which is the discrepancy between a patient’s highest weight and current weight, may be an important factor in the course and outcome of bulimia nervosa (BN). Individuals who are weight suppressed weigh less than they once did. Because patients with BN usually present for treatment at a normal weight, the fact that many were once overweight or obese is often overlooked (1). The average weight suppression for BN patients is high, with those in outpatient or residential treatment having average levels of 9.6 kg and 12.0 kg, respectively (2,3). Healthy college students, by comparison, have a mean weight suppression of 2.7 kg (4).
The perpetual dieting and/or compensatory behaviors that are needed to maintain a suppressed weight could maintain binge eating and purging. This large reduction in weight also could make patients with BN more susceptible to weight gain (possibly due to reduced metabolic rate, increased overeating, or both), leading to even greater dietary restriction, which maintains the binge/purge cycle (2, 5). Two studies have found that weight suppression predicted weight gain in patients with BN (β = .21, p = .03, 4.7% of variability in weight gain (3); B = 0.100, SE = 0.04, p =.01, Exp (B) = 1.11, R2= 0.06 (6)). This weight gain could cause increased body image dissatisfaction and lead to higher rates of disordered eating in an effort to avoid future weight gain or to lose the undesired weight. Additionally, since many individuals with BN were previously overweight, they may have an even greater fear of weight gain because they have previously seen those fears realized. This fear of weight gain could also contribute to greater levels of dieting and compensatory behaviors. Research has shown that patients who are high in weight suppression, compared to their peers with lower weight suppression, have a higher frequency of objective binge eating ((β = .319, p< .05), a higher probability of maintaining a bulimic syndrome over 10 years (7), a higher risk of dropping out of treatment (B = −0.37, SE = 0.07, p =.01, Exp(B) = 0.69) (2), and a lower chance of abstaining from binge eating and purging by treatment completion (2, 6, 8).
Weight suppression is calculated by two factors: current weight and highest weight. Research has examined whether either factor is predictive above and beyond weight suppression. To date, highest weight has not been predictive of BN symptoms or treatment outcome (2, 8). However, current weight is independently predictive of BN symptoms and outcome, with those who have lower weights demonstrating higher rates of BN pathology (9) and higher risk of treatment dropout (10).
Despite research suggesting that both current relative weight and weight suppression are predictive of bulimic pathology, no study has investigated the potential interaction between current weight and weight suppression. Individuals who have high weight suppression and low current weight might have the greatest motivation to stay thin, and may engage most in unhealthy eating behaviors. Individuals who are high in weight suppression and have a relatively high weight or those who are thin but not weight suppressed may have less severe symptoms, possibly because these individuals are not as afraid of weight gain or experience less biological pressures toward weight gain. In addition, the combination of high weight suppression and low weight could engage defensive biological mechanisms that could induce more binge eating and metabolic efficiency and therefore predispose these individuals towards weight gain. To test this hypothesis, the current study examined weight suppression, body mass index (BMI), and the interaction between weight suppression and BMI as predictors of bulimic symptoms upon admission to treatment. It was hypothesized that weight suppression and BMI would be independent predictors of bulimic symptoms, and that the interaction would be significant, with patients who have high weight suppression and low BMI demonstrating the most bulimic symptoms.
Method
Participants
Participants were 64 women beginning intensive outpatient treatment at a private eating disorders treatment facility. To be eligible for the study, participants needed to be 14 years of age or older and have no history of a psychotic disorder. The Structured Clinical Interview for DSM-IV (11) was used to determine eating disorder diagnoses. Participants had to meet full or sub-threshold criteria for BN. Many patients seeking treatment at eating disorder facilities are diagnosed with sub-threshold eating disorders, suggesting that including these participants in research samples provides maximal clinical generalizability (12, 13). The level of subjective distress and functional impairment in threshold and sub-threshold cases does not appear to differ significantly, providing further support for including sub-threshold cases in research (14). Other recent eating disorder studies have included sub-threshold patients, providing a precedent for doing so (e.g., 15, 16). Participants in this study were diagnosed with sub-threshold BN if their weight was above 85% of ideal body weight and they met all criteria for BN except that binge eating or compensatory behaviors were present but occurred less than twice per week. In this study, 10% of included participants received a sub-threshold diagnosis. Participants were excluded if they met diagnostic criteria for binge eating disorder.
Approximately 50% of patients who were admitted to treatment during the study period enrolled in this study. Because of limited resources, research staff members were able to approach only 60–70% of patients about the opportunity to participate. The majority of patients who were approached provided informed consent and enrolled. The research was reviewed and approved by an institutional review board.
Assessment
Weight and height were measured with a digital scale and a stadiometer and were used to calculate BMI. BMI was used as the key independent variable, rather than weight, because BMI provides a height-adjusted proxy for body mass. Weight suppression was calculated as the difference between previous highest weight and measured weight at admission to treatment. Participants’ previous highest and lowest weights at current height, not due to pregnancy or illness, were gathered by self-report. The validity of recalled past weights in young women has been documented (12). Also, Swenne (17) examined measured weights in females before they developed an eating disorder and found, in line with the data on highest previous weights reported here, that premorbid weights were higher than those of age-matched females in the general population.
The Eating Disorder Examination (EDE; 18), a semistructured clinical interview, was conducted at pretreatment. The EDE provides frequency ratings for objective binge eating episodes and purging episodes over the previous 28 days. (In this sample, the correlation between binge eating and purging episodes was r = .66.) The EDE has four subscales: Restraint (i.e., attempts to restrict food intake to influence shape and weight), Shape Concern, Weight Concern, and Eating Concern (i.e., preoccupation with food and losing control over eating). The EDE has demonstrated good inter-rater reliability and convergent and discriminant validity (19, 20, 21). The EDE interviewers in this study demonstrated high reliability (ICC ratings: Global score = .97; Restraint =.97; Eating Concern = .96; Weight Concern = .91; Shape Concerns = .99).
Statistical Analysis Plan
Multivariate linear regressions were conducted to determine if weight suppression, BMI, or their interaction were significant predictors of binge eating or purging frequency. The interaction variable was created by centering and then multiplying weight suppression and BMI. Subsequent regression equations were created in which additional variables were entered in the equation as covariates.
Results
Descriptive Statistics
On average, participants were 21.9 years of age (SD = 5.6). As shown in Table 1, participants had a mean weight suppression of 10.4 kg (SD = 13.8) and a mean BMI of 22.7 kg/m2 (SD = 3.9). Half of the participants were previously overweight or obese: 37.9% reported highest previous weights that were in the overweight range (i.e., BMI 25.0–29.9 kg/m2) and 13.6% reported weights that were obese (i.e., BMI ≥30.0 kg/m2).
Table 1.
Descriptive Statistics for Variables at Baseline
| Variable | Mean | Standard Deviation |
|---|---|---|
| Weight Suppression (kg) | 10.4 | 13.8 |
| Baseline BMI | 22.7 | 3.9 |
| BMI at highest weight | 26.7 | 6.0 |
| BMI at lowest weight | 18.8 | 3.2 |
| Current weight minus lowest weight (kg) | 9.6 | 8.6 |
| Length of illness (years) | 5.1 | 5.4 |
| Current age (years) | 21.9 | 5.6 |
| Eating Disorder Examination (EDE) Restraint | 2.9 | 1.5 |
| EDE Eating Concern | 4.0 | 1.5 |
| EDE Weight Concern | 3.0 | 1.4 |
| EDE Shape Concern | 3.7 | 1.5 |
| EDE binge eating episodes in last 28 days | 22.4 | 27.6 |
| EDE purging episodes in last 28 days | 30.9 | 41.9 |
Relationships between Weight Suppression, BMI, and Symptomatology
Bivariate correlations between weight suppression, BMI, and other variables of interest are shown in Table 2. Weight suppression and BMI were not significantly related. Weight suppression was positively correlated with highest previous BMI. Participants with greater weight suppression and higher baseline BMIs reported a longer time since the onset of their eating disorder and older age. Those with higher weight suppression reported more frequent binge eating and purging episodes.
Table 2.
Bivariate Correlations Between Weight Suppression, BMI, and Other Variables
| Weight Suppression | Baseline BMI | |||
|---|---|---|---|---|
|
| ||||
| r | p | r | p | |
| Baseline BMI | −.05 | .71 | – | – |
| BMI at highest weight | .77 | .01 | .04 | .77 |
| BMI at lowest weight | .18 | .14 | −.15 | .21 |
| Current weight minus lowest weight | −.11 | .44 | −.05 | .71 |
| Highest weight minus lowest weight | .78 | .01 | .34 | .01 |
| Length of illness | .33 | .01 | .30 | .02 |
| Current age | .32 | .01 | .21 | .09 |
| EDE Restraint | .01 | .95 | −.08 | .52 |
| EDE Eating Concern | .08 | .52 | .20 | .12 |
| EDE Weight Concern | −.02 | .90 | .11 | .37 |
| EDE Shape Concern | .00 | .98 | .24 | .05 |
| EDE binge eating episodes | .27 | .03 | −.08 | .54 |
| EDE Purging | .24 | .05 | .05 | .72 |
Note: correlations that are significant at p < .05 are shown in bold type.
Linear regressions were conducted to examine if weight suppression, BMI, and their interaction were related to frequency of binge eating. There was a main effect for weight suppression (β = .35, p = .01) but not BMI (β = −.17, p = .16). The interaction between weight suppression and BMI was significant (β = −.41, p = .01). Weight suppression, BMI, and their interaction accounted for 22.5% of the variance in binge eating frequency. The linear regression was repeated controlling for length of illness, age, and EDE Restraint, Shape Concerns, Eating Concerns, and Weight Concerns subscales. Weight suppression (β = .37, p = .01) and the interaction between weight suppression and BMI (β = −.28, p = .04) remained significant predictors of binge eating frequency. To further explore this interaction, participants were first divided into low- and high-BMI groups using a BMI of 21.5 kg/m2 as the cutoff for dichotomozing BMI. This BMI level was chosen because it is the midpoint of the healthy range of BMIs (i.e., 18–25 kg/m2). Because no such objective criterion for dichotomizing weight suppression is available, the median level of weight suppression in this sample, 6.7 kg, was used as the split point. Participants were categorized into four groups: low BMI (i.e., below 21.5 kg/m2) and low weight suppression (i.e., weight suppression of 6.7 kg or less) (n = 11); low BMI and high weight suppression (i.e, greater than 6.7 kg) (n = 18); high BMI (i.e., 21.5 kg/m2 or higher) and low weight suppression (n = 21); and high BMI and high weight suppression (n = 14). Post-hoc ANOVA analyses indicated that patients with low BMI and high weight suppression had binge eating rates more than twice as high as those in the other three groups (all p-values < .05; see Figure 1).
Figure 1.
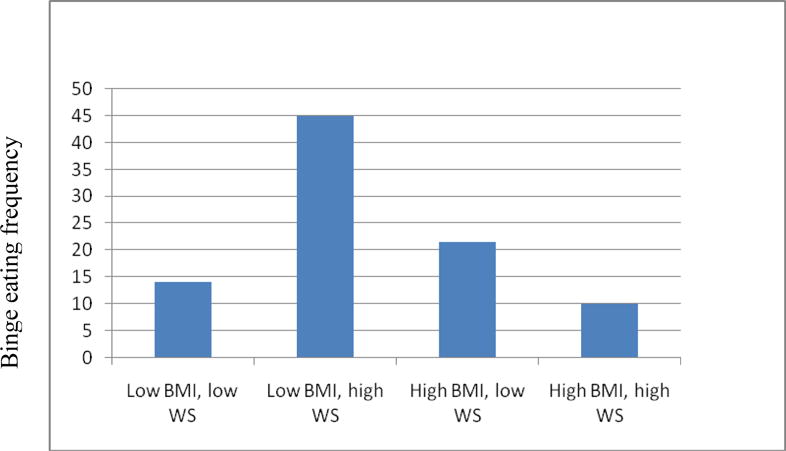
Figure 1 shows how frequency of binge eating in the previous month varies according to participants’ BMI and level of weight suppression. Participants with low BMI and high weight suppression had binge eating rates more than twice as high as those in the other three groups (all p-values < .05).
Linear regressions also were conducted to examine if weight suppression, BMI, and their interaction were related to purging frequency. There was a main effect for weight suppression (β = .27, p = .03) but not BMI (β = −.12, p = .35) or the interaction between weight suppression and BMI (β = −.20, p = .13). These three variables accounted for 9.3% of the variance in purging frequency. The linear regression was repeated controlling for length of illness, age, and EDE Restraint, Shape Concerns, Eating Concerns, and Weight Concerns subscales. Weight suppression (β = .40, p = .01) remained a significant predictors of purging frequency, such that participants with greater weight suppression engaged in more frequent purging episodes.
Weight Suppression versus Weight Fluctuation
One alternative explanation for these results is that weight suppression is simply a proxy of weight fluctuation (i.e., that the discrepancy between highest historical and current weights is predictive only because it is a marker of individuals who have frequently gained and lost large amounts of weight). To address this possibility, four variables were examined: 1) lowest previous BMI (at current height), 2) highest previous BMI (which could be considered a marker of weight gain proneness), 3) the difference between lowest weight (at current height) and current weight, and 4) the difference between highest weight and lowest weight at current height. As shown in Table 3, none of these variables was related to binge eating or purging frequency.
Table 3.
Bivariate correlations between measures of weight fluctuation and binge eating and purging frequency
| Binge eating frequency | Purging frequency | |||
|---|---|---|---|---|
| r | p | r | p | |
| BMI at highest weight | −.17 | .12 | .12 | .26 |
| BMI at lowest weight | −.16 | .15 | −.07 | .52 |
| Current weight minus lowest weight | .19 | .21 | .15 | .26 |
| Highest weight minus lowest weight | .19 | .09 | .01 | .89 |
Finally, the regression equations that tested the primary hypotheses for this study were re-run, replacing the weight suppression variable with the variable that may be the best measure of weight fluctuation: the difference between highest and lowest weights. In the prediction of binge eating frequency, there was a main effect for difference between highest and lowest weights (β = .27, p = .047) but not BMI (β = −.06, p = .68) or the interaction between difference between highest and lowest weights and BMI (β = −.18, p = .24). These three variables accounted for 7.9% of the variance in binge eating frequency. In the prediction of purging frequency, there was no main effect for difference between highest and lowest past weights (β = .12, p = .36) or BMI (β = .07, p = .62) but the interaction between these variables was significant (β = −.35, p = .02). These three variables accounted for 9.1% of the variance in purging frequency. When these linear regressions were repeated with the covariates used in the original models, difference between highest and lowest weights remained a significant predictor of binge eating frequency (β = .39, p = .02) but not purging frequency (β = .16, p = .34).
Discussion
As hypothesized, weight suppression was related to frequency of binge eating and purging and interacted with BMI such that those who were high in weight suppression and low in BMI exhibited more than twice as much binge eating than groups representing other combinations of weight suppression and BMI status. Those higher in weight suppression also exhibited more purging, but neither BMI nor the interaction of BMI and weight suppression were related to purging. This is the first time that a low BMI has been shown to combine synergistically with high weight suppression to predict a substantially elevated frequency of binge eating. The prediction of binge eating by weight suppression also replicates the findings reported by Lowe et al. (8). Neither this study, nor any other study that has been conducted to date, can determine if weight suppression has a causal influence on BN symptomatology. However, additional research on causal mechanisms is clearly warranted, given that the weight suppression effect has not yet been accounted for by other possibly relevant variables (e.g., highest previous weight or the constructs measured by the EDE subscales).
Past research has found that a low BMI predicts greater bulimic pathology in patients with anorexia nervosa (AN) at the end of treatment (9) and greater drop out from treatment amongst a sample with either AN or BN (10). The combination of past and current findings on low BMI and on weight suppression suggests that both influences could exacerbate symptoms and undermine treatment. The body weight regulatory system of individuals with BN may be sensitive to both weight suppression and absolute body mass (i.e., a reduction in BMI below a homeostatically-defended level that engages starvation-induced compensatory reactions – e.g., in women, a slowing of fat oxidation to protect fat stores and preserve regular menstruation).
Of note, when weight fluctuation was operationalized as the difference between highest and lowest weights, this variable was a significant predictor of binge eating frequency (controlling for BMI), but it accounted for a smaller amount of variance than weight suppression. Weight fluctuation alone did not predict purging frequency, but the interaction between weight fluctuation and current BMI was a significant predictor (the amount of variance accounted for by this model was equal to that of the weight suppression model). The correlation between weight suppression and weight fluctuation is very high. Many individuals with eating disorders have identical levels of weight suppression and weight fluctuation (i.e., if their current weight is the lowest weight they have reached at their current height). For other individuals these values are different, in which case it is possible that weight suppression provides more clinically meaningful information, because it takes current weight status into account. Future research should continue to examine the relative importance of each of these variables.
The interactive effects of weight suppression and BMI on binge eating were evident even after relevant psychological constructs such as weight and shape concerns – which are thought to represent the “core psychopathology” of BN (21) – were controlled. These cognitive concerns did not account for significant variance in binge eating or purging, but the behavioral enactment of these concerns – that is, weight loss – still predicted binge eating and purging frequency. Weight suppression, but not BMI or the interaction between these two variables, predicted purging frequency. Because individuals with BN usually purge after each episode of binge eating, the frequency of binge eating and purging is usually correlated. Nonetheless, most individuals with BN engage in some purging that is not preceded by a binge and this might explain why the variables studied did not predict purging frequency as robustly as binge frequency.
Additional research is warranted to determine what variables mediate the relationship between weight suppression and BN symptomatology and to understand why BMI moderates this relationship. Low BMI and high weight suppression could have biological and behavioral effects that increase food intake, feelings of loss of control over eating, or both. Previous research has shown that large weight losses in normal weight individuals can result in binge eating-like behavior (22). Substantial weight loss also produces decreases in anorexigenic hormones such as leptin and orexigenic hormones like ghrelin (23). These hormonal changes could fuel overeating or binge eating, which could partially explain why individuals with BN who are high in weight suppression show accelerated weight gain over time (3, 6). Weight loss also produces a reduction in resting metabolic rate that exceeds the loss in metabolically-active lean tissue (24), which would also predispose weight suppressed individuals toward weight regain.
Weight loss was identified as a potentially significant influence on the etiology or maintenance of BN in the first publication identifying the disorder (25), but little attention has been devoted to the possible significance of BMI and weight suppression for the psychopathology (5) and treatment (21) of BN. The present results, along with those from other recent studies (2, 3, 6, 8) suggest that the weight of individuals with BN relative to an estimate of a biologically healthy weight (i.e., the mid-point of the healthy weight range), and relative to the individual’s highest-ever body weight, may have important implications for symptom status, weight change, and treatment outcome. Future research should 1) examine weight suppression as a risk factor in prospective studies of BN onset and as a predictor of outcome in BN treatment, 2) explore possible metabolic, appetitive, psychological, and behavioral mediators of the relationship between weight suppression and symptomatology, and 3) further explore BMI and other possible moderators of the relationship between weight suppression and symptomatology. Experimental research may be informative. Ethical concerns render most experimental designs unfeasible, such as a study in which weight suppression is induced in healthy young women and the consequences that follow are assessed. It would be more feasible to test whether an intervention of weight gain, which would reduce weight suppression, produces clinical improvements in patients with BN.
Strengths of the current study include the use of a community-based treatment sample, the use of the EDE to collect data on symptomatology, and the simultaneous examination of the independent and combined influence of two measures of body weight status on binge eating and purging. Weaknesses include a self-selected sample of approximately 50% of patients who were admitted to treatment during the study period, the cross-sectional design, and the small sample size. Nonetheless the current findings provide further support for the conclusion that the current and past body mass of BN patients is highly relevant to the understanding and treatment of BN.
This study has several clinical implications. Weight suppression is a clinically significant variable that should be assessed by treatment providers. The interaction between weight suppression and BMI indicates that weight suppression should be interpreted in the context of current BMI. Finally, although no treatment studies have tested this hypothesis, it is possible that some weight gain may be beneficial for BN patients who have high levels of weight suppression and relatively low BMI.
Acknowledgments
This research was supported by a grant from the National Institutes of Mental Health (R34MH71691).
Drs. Butryn and Lowe serve as paid research consultants to The Renfrew Center.
References
- 1.Fairburn CG, Cooper Z. Thinking afresh about the classification of eating disorders. International Journal of Eating Disorders Special Issue on Diagnosis and Classification. 2007;40(Supl):S107–S110. doi: 10.1002/eat.20460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butryn M, Lowe M, Safer D, Agras W. Weight suppression is a robust predictor of outcome in the cognitive-behavioral treatment of BN. Journal of Abnormal Psychology. 2006;115:62–67. doi: 10.1037/0021-843X.115.1.62. [DOI] [PubMed] [Google Scholar]
- 3.Lowe M, Davis W, Lucks D, Annunziato R, Butryn M. Weight suppression predicts weight gain during inpatient treatment of BN. Physiology and Behavior. 2006;87:487–492. doi: 10.1016/j.physbeh.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Lowe MR, Annunziato RA, Markowitz JT, Didie E, Bellace DL, Riddell L, Maille C, McKinney S, Stice E. Multiple types of dieting prospectively predict weight gain during the freshman year of college. Appetite. 2006;47(1):83–90. doi: 10.1016/j.appet.2006.03.160. [DOI] [PubMed] [Google Scholar]
- 5.Wilson G, Grilo C, Vitousek K. Psychological treatment of eating disorders. American Psychologist. 2007;62:199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- 6.Carter F, McIntosh V, Joyce P, Bulik C. Weight suppression predicts weight gain over treatment but not treatment completion or outcome in BN. Journal of Abnormal Psychology. 2008;117:936–940. doi: 10.1037/a0013942. [DOI] [PubMed] [Google Scholar]
- 7.Keel P, Heatherton T. Weight suppression predicts maintenance and onset of bulimic syndromes at 10-year follow-up. Journal of Abnormal Psychology. 2010;119:268–275. doi: 10.1037/a0019190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lowe M, Thomas J, Safer D, Butryn M. The relationship of weight suppression and dietary restraint to binge eating in BN. International Journal of Eating Disorders. 2007;40:640–644. doi: 10.1002/eat.20405. [DOI] [PubMed] [Google Scholar]
- 9.Howard W, Evans K, Quintero-Howard C, Bowers W, Andersen A. Predictors of success or failure of transition to day hospital treatment for inpatients with anorexia nervosa. American Journal of Psychiatry. 1999;156:1697–1702. doi: 10.1176/ajp.156.11.1697. [DOI] [PubMed] [Google Scholar]
- 10.Jones A, Bamford B, Ford H, Schreiber-Kounine C. How important are motivation and initial body mass index for outcome in day therapy service for eating disorders. European Eating Disorders Review. 2007;15:283–289. doi: 10.1002/erv.736. [DOI] [PubMed] [Google Scholar]
- 11.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 12.Field AE, Franko DL, Striegel-Moore RH, Schreiber GB, Crawford PB, Daniels SR. Race differences in accuracy of self-reported childhood body size among white and black women. Obesity Research. 2004;12(7):1136–1144. doi: 10.1038/oby.2004.142. [DOI] [PubMed] [Google Scholar]
- 13.Williamson DA, Gleaves DH, Savin SS. Empirical classification of eating disorder not otherwise specified: Support for DSM-IV changes. Journal of Psychopathology and Behavioral Assessment. 1992;14(2):201–216. [Google Scholar]
- 14.Lewinsohn PM, Striegel-Moore RH, Seeley JH. Epidemiology and natural course of eating disorders in young women from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(10):1284–1292. doi: 10.1097/00004583-200010000-00016. [DOI] [PubMed] [Google Scholar]
- 15.Burton E, Stice E. Evaluation of a healthy-weight treatment program for BN: A preliminary randomized trial. Behaviour Research and Therapy. 2006;44(12):1727–1738. doi: 10.1016/j.brat.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghaderi A, Scott B. Pure and guided self-help for full and sub-threshold BN and binge eating disorder. British Journal of Clinical Psychology. 2003;42(3):257–269. doi: 10.1348/01446650360703375. [DOI] [PubMed] [Google Scholar]
- 17.Swenne I. Weight requirements for catch-up growth in girls with eating disorders and onset of weight loss before menarche. International Journal of Eating Disorders. 2005;38:340–345. doi: 10.1002/eat.20182. [DOI] [PubMed] [Google Scholar]
- 18.Fairburn CG, Cooper Z. The eating disorder examination (12th edition) In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. New York: Guilford Press; 1993. pp. 317–331. [Google Scholar]
- 19.Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. British Journal of Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 20.Rosen JC, Vara L, Wendt S, Leitenberg H. Validity studies of the eating disorder examination. International Journal of Eating Disorders. 1990;9:519–528. [Google Scholar]
- 21.Fairburn CG, editor. Cognitive behavior therapy and eating disorders. New York: Guilford Press; 2008. [Google Scholar]
- 22.Keys A, Brozek K, Henschel A, Mickelsen O, Taylor HL. The biology of human starvation. Minneapolis: University of Minnesota Press; 1950. [Google Scholar]
- 23.Beck B, Richy S. Dietary modulation of ghrelin and leptin and gorging behavior after weight loss in the obese Zucker rat. Journal of Endocrinology. 2009;202:29–34. doi: 10.1677/JOE-09-0080. [DOI] [PubMed] [Google Scholar]
- 24.Rosenbaum M, Hirsch J, Gallagher DA, Leibel RL. Long-term persistence of adaptive thermogenesis in subjects who have maintained a reduced body weight. American Journal of Clinical Nutrition. 2008;88:906–912. doi: 10.1093/ajcn/88.4.906. [DOI] [PubMed] [Google Scholar]
- 25.Russell G. BN: An ominous variant of anorexia nervosa. Psychological Medicine. 1979;9:429–448. doi: 10.1017/s0033291700031974. [DOI] [PubMed] [Google Scholar]


