Abstract
Background
We hypothesized that community-based HIV testing with counselor support and point-of-care CD4 count testing would increase uptake of antiretroviral therapy (ART) and male circumcision.
Methods
We conducted a randomized study of linkage strategies following community-based HIV testing in rural South Africa and Uganda. HIV-positive persons were randomized to 1) lay counselor follow-up home visits, lay counselor clinic linkage facilitation, or standard clinic referral; and then to either 2) point-of-care CD4 testing, or referral for CD4. HIV-negative uncircumcised men who could receive secure text messages were randomized to text message reminders, lay counselor visits, or referral. The primary outcomes were viral suppression at 9 months in HIV-positive persons and uptake of male circumcision by HIV-negative, uncircumcised men at 3 months. The study was registered at ClinicalTrials.gov (NCT02038582).
Findings
Between June 2013 and February 2015, 15,332 participants were tested; 1,325 HIV-positive persons and 750 HIV-negative uncircumcised men were randomized to linkage strategies. Among HIV-positive persons, overall clinic linkage was 93% (1,218/1,303) but ART initiation was only 37% (488/1,303). The proportion of persons who were virally suppressed ranged from 47%-52% (214/422 in the clinic referral arm, 219/419 in the clinic facilitation arm, and 202/431 in the lay counselor follow-up arm; p=0.668 and p=0.273, for the clinic facilitation and lay counselor follow-up arms, respectively, compared with clinic referral). There was no difference in viral suppression at 9 months by study arm. In the male circumcision clinic referral (standard of care) arm, 62/224 men (28%) were circumcised, compared to 137/284 (48%) in the text message reminder arm (RR=1.72, 95% CI 1.36-2.17) and 106/226 (47%) in the lay counselor follow-up arm (RR=1.67, 95% CI 1.29-2.14).
Interpretation
All the community-based strategies achieved very high rates of linkage of HIV positive persons to HIV clinics, approximately one-third of whom initiated ART, and approximately half were virally suppressed by 9 months. Clinic barriers to ART initiation must be addressed in future strategies to increase knowledge of HIV serostatus and linkage to HIV care. Uptake of male circumcision was almost two-fold higher among men who received text message reminders or lay counselor visits.
Keywords: Community-based HIV testing and counseling (HTC); home HTC, point-of-care CD4, linkage to care; HIV prevention and care, HIV infectiousness, and community viral load, Africa
Introduction
High coverage of a combination of synergistic, evidenced-based HIV prevention interventions could substantially reduce the number of incident HIV cases in Africa.1,2 Male circumcision decreases HIV acquisition by 60%3-6 and antiretroviral therapy (ART) almost eliminates HIV transmission from HIV-positive persons who are virally suppressed.7,8 However, at the population level, the coverage for male circumcision and ART has lagged substantially behind targets. In African countries with generalized HIV epidemics and low rates of circumcision, an estimated 30% of men have accessed male circumcision services compared to the target of 80% by 2016.9 In addition, only 40% of all HIV-positive persons are virally suppressed due to drop-off at each stage of the testing to treatment cascade,10 which is much lower than the UNAIDS target of 73%.11 Strategies to achieve high coverage of HIV testing and linkage to combination prevention strategies are critical for a population-level impact on HIV incidence.12
Community-based HIV testing and counseling (HTC)13-15 and linkage strategies by lay persons are approaches to increase uptake of ART and male circumcision. Linkage strategies are defined as interventions to link persons to treatment or prevention following testing. Promising linkage to care strategies include point-of-care CD4 count testing to facilitate ART initiation by providing ‘real-time’ ART eligibility and counseling,16,17 lay counselor home visits to encourage linkage to ART or male circumcision, lay counselor facilitation of the HIV clinic visit to support clients’ understanding of ART initiation,18-20 and text messages to support ART adherence.21,22 The relative effectiveness of community-based strategies to link HIV-positive persons to HIV care and HIV negative uncircumcised men to medical male circumcision in Africa have not been assessed.
Here we present the results of The Linkages Study that evaluated the effectiveness of community-based HTC (i.e. home and mobile HTC) and linkage strategies compared to standard referral for linking HIV-positive persons to ART and HIV-negative, uncircumcised men to male circumcision in two rural settings in Africa. The primary objectives were to evaluate the relative effectiveness of enhanced linkage strategies for HIV-positive persons (lay counselor follow-up visits, clinic visit facilitation, and point-of-care CD4 testing) versus standard of care on clinically-relevant outcomes of linkage to an HIV clinic, ART initiation and viral suppression. For HIV-negative men, the primary objective was to evaluate the relative effectiveness of lay counselor home visits and text message reminders on the uptake of male circumcision.
Methods
Study design
We conducted an individually randomized study of community-based HTC and linkage strategies for HIV-positive persons not on ART and HIV-negative uncircumcised men in South Africa and Uganda. HIV-positive persons not on ART were randomized to one of six linkage strategies (lay counselor follow-up visits, lay counselor clinic facilitation, or standard of care, combined with either point-of-care CD4 testing or referral for CD4 testing) in a factorial design. HIV-negative uncircumcised men were randomized to one of three strategies to increase uptake of male circumcision services (text message reminders, home visits, or standard referral). The University of Washington Institutional Review Board, the Ugandan National HIV/AIDS Research Committee, and the Human Sciences Research Council Research Ethics Committee approved this study. The study was registered at ClinicalTrials.gov, number NCT02038582.
Participants
Following community mobilization, participants were recruited through community-based HIV testing.11 Home-based and mobile HIV testing were conducted in research naïve communities, which have public clinics that offer free HIV care and ART; two communities in uMgungundlovu District, KwaZulu-Natal, South Africa and four in the Sheema District, southwest Uganda. Reported population HIV prevalence in KwaZulu-Natal was 28%,12 and in Mbarara, adjacent to the Sheema District was 10%,13 representing high and medium prevalence settings in southern and East Africa, respectively. The communities in KwaZulu-Natal are characterized by high unemployment and low per capita income (below USD $2 per day).
Trained and supervised lay counselors in Uganda and lay counselor and nurse teams in South Africa conducted study activities. Teams were trained in HIV testing and counseling, HIV natural history, benefits of ART, monitoring of medical male circumcision and ART, and expected procedures at the clinic. Study participants provided written informed consent in a confidential setting. Participants completed a standardized questionnaire about demographics, risk, and engagement in HIV testing, treatment and prevention using the mobile phone software Mobenzi Researcher™ (Durban, South Africa). Lay counselors conducted HIV testing with standardized pre- and post-test counseling and couples disclosure counseling.
HIV-positive persons identified during community-based testing were eligible for randomization if they were able to provide informed consent, were 16 years or older, resident in the participating communities, and not taking ART. HIV-negative men were eligible for randomization if they were age 16 to 49 years, uncircumcised, and had access to private text messaging.
Randomization
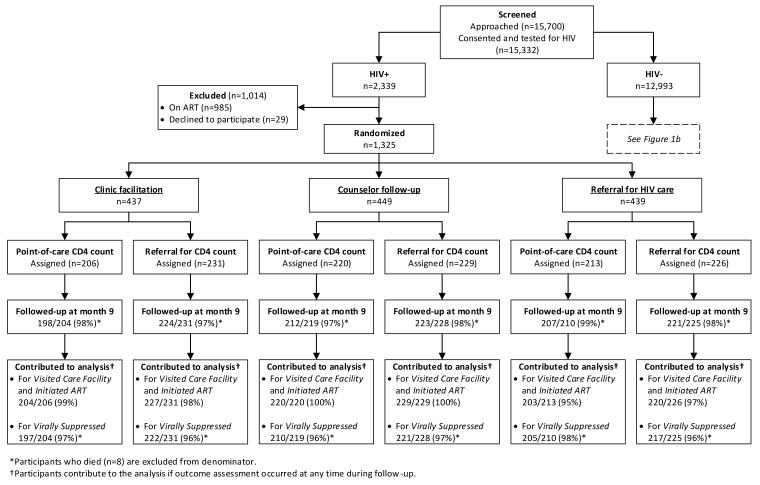
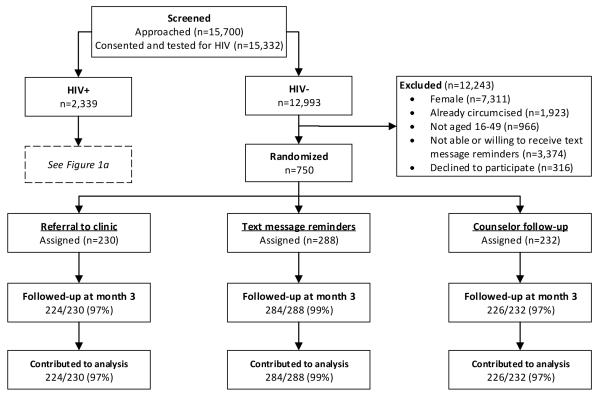
The study biostatistician generated the randomization allocation using varying block sizes and stratified by country. The randomization allocation was automatically assigned by the software to the study participant after obtaining informed consent. Once eligibility was assessed and the participant consented to continuing with the study, the randomization assignment was revealed. The study staff did not have access to the randomization code. Eligible participants in the same household were randomized to the same arm to prevent crossover between study arms. HIV-positive persons not on ART were randomized in a factorial design to 1) either lay counselor follow-up home visits, clinic facilitation, or standard referral; and then to 2) either point-of-care CD4 count testing after post-testing counseling, or referral for CD4 testing (Figure 1a). HIV-negative uncircumcised men were randomized to text message reminders, lay counselor visits, or referral (Figure 1b). After enrolling 448 participants, we discovered that the mobile phone companies were blocking the text messages and participants were not receiving the intervention. The study biostatistician redid the block randomization code to increase the number of participants randomized to the text message arm to ensure at least 80% power to see a 10% effect of the male circumcision linkage strategies.
Figure 1a.
HIV-positive arms CONSORT diagram
Figure 1b.
HIV-negative arms, medical male circumcision promotion CONSORT diagram
Procedures
Participants in the point-of-care CD4 arm received same day point-of-care CD4 testing at enrollment, which was used in counseling about ART eligibility under national guidelines (CD4 ≤350 cells/μL, which changed to CD4 ≤500 cells/μL in January 2015). In the referral for CD4 count arm, participants were referred to local HIV clinics to obtain their CD4 count, as is the standard of care. Study staff provided HIV-positive persons a clinic referral card, their point-of-care CD4 test result if they were in the point-of-care CD4 arm, information about local HIV clinics, and encouraged participants to visit a clinic within a month and collected plasma for HIV viral load testing.
In the lay counselor follow-up arm, participants received visits at home at months one, three and six; home visits stopped once participants reported that they had visited a clinic. At home visits, lay counselors answered questions about HIV care and provided information and support about HIV clinics and ART. In the clinic facilitation arm, a lay counselor met HIV-positive persons at the clinic and explained the steps of engagement in care (e.g., clinic registration, education visits, baseline laboratory tests) and the benefits of ART. Lay counselors facilitated more than one clinic visit for persons who did not complete ART initiation prerequisites at the initial clinic visit. In the standard of care arm, participants visited the clinic and followed clinic procedures for ART initiation, which included three preparatory visits for laboratory testing and ART literacy counseling, without lay counselor support.
All HIV-negative persons were counseled to engage in prevention to remain HIV-negative. HIV-negative men received counseling on male circumcision and a referral card to local male circumcision facilities. HIV-negative men randomized to text message reminders received a non-identifying promotion message (“this could be the best decision you make – act now!”) three weeks after testing with a follow-up phone call one month after testing. If men did not report being circumcised at the month one follow-up call, a second message was sent six to seven weeks after testing with a follow-up phone call two months after testing. Participants in the lay counselor follow-up arm received a home visit one month after testing, and then again at two months if they had not already receive male circumcision services.
As required by local regulatory bodies, participants were compensated for their time with a food parcel in South Africa (approximate value = USD 8) and cash in Uganda (approximate value = USD 2) at the end of the enrollment and follow-up visits regardless of whether they agreed to testing, HIV serostatus, receipt of results, clinic attendance, circumcision uptake or ART initiation. Participants did not receive financial incentives to attend treatment or prevention services.
Outcomes and assessment
The primary outcomes for HIV-positive persons were obtaining a CD4 count, linkage to an HIV clinic, ART initiation, viral suppression and social harms, which were assessed at nine months after enrollment. The primary outcome for uncircumcised, HIV-negative men was uptake of male circumcision at three months. Secondary outcomes were uptake of male circumcision at nine months and social harms.
HIV-positive persons received an exit visit nine months after testing in all study arms to assess linkages to care, barriers to establishing HIV care and uptake of ART. Point-of-care CD4 testing was done for all participants and the results provided to support continuity of care. Specimens were collected for viral load testing at the exit visit. At each visit, lay counselors administered questionnaires about risk behavior, engagement in care, and social harms. To confirm uptake of HIV care and ART, lay counselors reviewed clinic cards and medications with the participant but clinic attendance and ART dispensing were not confirmed with the clinics.
HIV-negative men in all three study arms received a visit at month three, and for those who had not been circumcised before the three month visit, an exit visit at month nine was conducted to assess whether they had visited a male circumcision provider between months three and nine, had been circumcised and had experienced social harms. The male circumcision referral cards were reviewed with the participants to confirm uptake of circumcision services.
Laboratory methods
HIV testing was conducted using blood obtained by finger-stick and tested using rapid serologic tests according to national guidelines: in Uganda Determine (Abbott Laboratories) followed by Statpak (Chembio Diagnostics) for confirmation of positive results and Unigold (Trinity Biotech) as a tie breaker, and in South Africa, ABON HIV Rapid test (Alere) and First Response HIV Test (Premier Medical Corporation Ltd) with HIV 1/2 Gold Screening Test (G-Ocean) as a tie breaker. Point-of-care CD4 testing (Alere, PIMA™) was conducted using a finger-stick specimen. Plasma was obtained via phlebotomy at the home or in the mobile van and transported to the reference laboratory for HIV viral load testing by polymerase chain reaction (Roche Taqman Ampliprep, with a limit of detection of 20 copies/mL).
Statistical analysis
The target sample sizes of 1,300 HIV-positive persons and 750 HIV-negative uncircumcised men were calculated to provide at least 80% power to see a 10% difference in viral suppression for HIV-positive persons and a 10% difference in uptake of male circumcision for HIV-negative men between the different linkage strategies. All available assessments from participants contributed to assignment of whether the participant linked to HIV care or male circumcision services.
The effects of the randomization arms on each outcome were estimated as relative risks (RR), produced using a Poisson regression model with robust variance estimation, adjusted for country and accounting for within-household correlation. Randomized assignments for both interventions were included in the model so that the effect of each is adjusted for the other. In addition, interaction terms were considered in the model of crossed factors in order to evaluate whether the effect of either depended on the other.
The data were analyzed using R version 3.2.1.
Role of the funding source
The study sponsors had no role in study design; data collection, analysis, and interpretation; writing of the report; or in the decision to submit for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Between June 2013 and February 2015, 15,700 participants (6,942 in South Africa and 8,758 in Uganda) were offered home or mobile HIV testing and counseling and 15,332 (98%) were tested. Of those tested, 8,703 (57%) were tested at home, 6,533 (43%) were tested for the first time and 6,578 (43%) were men. The median age was 30 years (interquartile range (IQR): 22-43 years). HIV prevalence was 15%; 24% (1,648/6,912) in South Africa and 8% (691/8,420) in Uganda. HIV prevalence among women and men in Uganda was 10% and 7%, respectively, and in South Africa was 28% and 16%, respectively. Almost half (1,013/2,339, 43%) of HIV-positive persons were newly identified. Overall, 985/2,339 (42%) HIV-positive persons reported currently taking ART and were not eligible for randomization (Figure 1a). Among HIV-negative uncircumcised males below age 49, 1,855/2,926 (63%) reported that they did not have secure access to text message reminders and were not eligible for randomization.
Notably, there were no reported cases of study-related social harm during the study, which included probing about partnership separation, unintended disclosure, gender-based violence and stigma.
Baseline characteristics of HIV-positive participants
Of the 1,325 HIV-positive participants randomized to linkage strategies, the median age was 31 years (IQR: 26-38 years), 641 (48%) were 30 years or younger, 29% were male, and 733 (55%) were identified through home testing (Table 1). Of the participants randomized, 333 (25%) were previously aware of their HIV-positive status, of whom 205 (16%) were aware of their status for more than 12 months, 256 (19%) had previously visited an HIV clinic, and 238 (18%) reported having their CD4 count tested prior to the study. Among persons randomized to the point-of-care CD4 arm, the median CD4 count was 486 cells/μL (IQR: 344-653 cells/μL). Among persons randomized to the clinic referral CD4 arm, 501/626 (80%) obtained a CD4 count. The median CD4 count among the 380/501 (76%) persons who could recall their result was 512 cells/μL (IQR: 384-670 cells/μL). The median viral load at enrollment was 12,170 copies/mL and 311/1,318 (24%) participants had a viral load <50 copies/mL.
Table 1.
Baseline characteristics of participants
| HIV-positive participants N = 1,325 |
HIV-negative male participants N = 750 |
|||||
|---|---|---|---|---|---|---|
| Characateristic | n | (%) | Median (IQR) | n | (%) | Median (IQR) |
| Age (years) | 31 (26 - 38) | 23 (19 - 29) | ||||
| Age group ≤ 30 | 641 | (48.4) | 588 | (78.4) | ||
| Male | 379 | (28.6) | 750 | (100.0) | ||
| Home HIV testing and counseling (vs. mobile) | 733 | (55.3) | 342 | (45.6) | ||
| Ever tested for HIV | - | - | - | 303 | (40.4) | |
| Newly identified | 992 | (74.9) | - | - | - | |
| Previously aware of HIV-infected status | 333 | (25.1) | - | - | - | |
| Previously visited an HIV clinic, (of % aware of status) |
256 | (76.9) | - | - | - | |
| CD4 count previously tested, (of % aware of status) |
238 | (72.8) | - | - | - | |
| Previous CD4 count ≤ 500 cells/μL, (of % remembered result) |
52 | (12.2) | - | - | - | |
| Cohabiting | 125 | (9.4) | 69 | (9.2) | ||
| Sexually active | 1149 | (87.4) | 635 | (86.3) | ||
| Number of current sex partners | ||||||
| 0 | 165 | (12.6) | 101 | (13.7) | ||
| 1 | 1027 | (78.2) | 512 | (69.6) | ||
| > 1 | 122 | (9.3) | 123 | (16.7) | ||
| Condom use with last sex act | 445 | (33.6) | 222 | (29.6) | ||
| Number of children in home * | ||||||
| 0 | 299 | (31.6) | - | - | - | |
| 1-3 | 600 | (63.4) | - | - | - | |
| > 3 | 47 | (5.0) | - | - | - | |
| CD4 count (cells/μL)† | 486 (344 - 653) | - | - | - | ||
| Viral load category (copies/mL) | ||||||
| < 50 | 311 | (23.5) | - | - | - | |
| 50-999 | 119 | (9.0) | - | - | - | |
| 1,000-9,999 | 203 | (15.3) | - | - | - | |
| > 9,999 | 685 | (51.7) | - | - | - | |
| Texting frequency | ||||||
| Never/rarely | - | - | - | 76 | (10.3) | |
| Weekly | - | - | - | 210 | (28.3) | |
| Daily | - | - | - | 455 | (61.4) | |
| Knows someone who has been circumcised | - | - | - | 655 | (87.8) | |
| Believes circumcision benefits female partner | ||||||
| Yes | - | - | - | 615 | (82.2) | |
| No | - | - | - | 22 | (2.9) | |
| Don’t know | - | - | - | 111 | (14.8) | |
| Willingness to undergo circumcision | ||||||
| Yes, at a clinic | - | - | - | 571 | (76.1) | |
| Yes, at a mobile camp | - | - | - | 59 | (7.9) | |
| Yes, at a clinic or mobile camp | - | - | - | 117 | (15.6) | |
| No | - | - | - | 2 | (0.3) | |
IQR = Interquartile range
Female participants only
CD4 count for participants not on ART in the point-of-care CD4 arm only (n=639)
Most (88%) of the HIV-positive participants reported being currently sexually active, with a median number of current partners of 1 (min: 0, max: 7), and 34% reported condom use with the last sex act.
Baseline characteristics of HIV-negative men
Of the 750 HIV-negative men randomized to male circumcision linkage strategies, the median age was 23 years (IQR: 19-29 years), 48% were ≤30 years old, 342 (46%) were identified through home testing, and 303 (40%) reported ever testing for HIV previously (Table 1). Most (85%) of the HIV-negative men reported being sexually active, with a median number of current partners of 1 (min: 0, max: 15), and 222/750 (30%) reported condom use with the last sex act. At baseline, 747 (99%) of participants were willing to undergo male circumcision.
Changes in linkage to care, ART initiation and viral suppression by 9 months
Among the 1,325 HIV-positive persons randomized to linkage strategies, study retention was 96% (1,273/1,325) at month nine. During follow-up, 8 participants died, 31 moved, and 14 withdrew. By month nine, 501/626 participants (80%) in the CD4 testing referral arm and 639/639 (100%) in the point-of-care CD4 count arm obtained a CD4 count (RR=1.25, 95% CI: 1.20, 1.30), with no difference in linkage to clinic, ART initiation or viral suppression by CD4 count testing strategy (Table 2).
Table 2.
Impact of linkage-to-care strategies among HIV-positive participants
| Visited HIV care facility |
Initiated ART |
Viral load < 50 copies/mL |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | RR | (95% CI) | p-value | n | % | RR | (95% CI) | p-value | n | % | RR | (95% CI) | p-value | |
| CD4 COUNT STRATEGY * | ||||||||||||||||
| Referral for CD4 count | 686 | 626/676 | 92.6 | — | reference | — | 243/676 | 35.9 | — | reference | — | 330/660 | 50.0 | — | reference | — |
| Point-of-care CD4 count | 639 | 592/627 | 94.4 | 1.02 | (0.99, 1.05) | 0.177 | 245/627 | 39.1 | 1.08 | (0.94, 1.26) | 0.281 | 305/612 | 49.8 | 1.00 | (0.89, 1.12) | 0.986 |
| LINKAGE STRATEGY † | ||||||||||||||||
| Clinic referral | 439 | 378/423 | 89.4 | — | reference | — | 142/423 | 33.6 | — | reference | — | 214/422 | 50.7 | — | reference | — |
| Clinic facilitation | 437 | 421/431 | 97.7 | 1.09 | (1.05, 1.13) | < 0.001 | 161/431 | 37.4 | 1.11 | (0.92, 1.34) | 0.260 | 219/419 | 52.3 | 1.03 | (0.90, 1.18) | 0.668 |
| Lay counselor follow-up | 449 | 419/449 | 93.3 | 1.04 | (1.00, 1.09) | 0.044 | 185/449 | 41.2 | 1.23 | (1.02, 1.47) | 0.028 | 202/431 | 46.9 | 0.92 | (0.80, 1.06) | 0.273 |
| TESTS FOR INTERACTION | ||||||||||||||||
| Point-of-care CD4 count × Clinic facilitation |
0.176 | 0.447 | 0.315 | |||||||||||||
| Point-of-care CD4 count × Lay counselor follow-up |
0.953 | 0.795 | 0.341 | |||||||||||||
N = number enrolled (and in subset if applicable)
n = proportion with outcome among those ever assessed for outcome
RR = relative risk; CI = confidence interval
Adjusted for linkage strategy and country;
adjusted for CD4 count strategy and country
Clinic visit uptake was high across the six arms (93%). Clinic facilitation increased engagement with HIV clinics with 421/431 (98%) participants visiting a clinic compared to 378/423 (89%) in the referral arm (RR=1.09, 95% CI 1.05, 1.13), which was similar to clinic linkage 419/449 (93.3%) in the lay counselor follow-up arm compared to the referral arm (RR=1.04, 95% CI 1.00, 1.09).
ART initiation was higher in the lay counselor follow-up arm (185/449, 41%) than in the referral arm (142/423, 34%) (RR=1.23, 95% CI 1.02, 1.47). ART initiation in the clinic facilitation arm was not clearly higher (161/431, 37%) compared to the referral arm (RR=1.11, 95% CI 0.92, 1.34). Among HIV infected persons who met national ART eligibility guidelines (CD4 count, pregnancy and active tuberculosis) and who were not virally suppressed at baseline, 74% of participants (131/177) had initiated ART by nine months in the lay counselor arm compared to 57% (85/149) in the referral arm (RR=1.32, 95% CI 1.12, 1.56), and 66% (110/166) in the clinic facilitation arm (RR=1.17, 95% CI 0.98, 1.40; compared to referral arm). The median time to ART initiation, among those eligible for ART, was 22 weeks.
Overall, viral suppression at nine months was 50% (635/1,272), without significant differences by study arm (Table 2). There were no significant interactions between point-of-care CD4 testing and either clinic facilitation or lay counselor follow-up. Overall, 83% of persons initiating ART achieved viral suppression by nine months after enrollment without significant difference between study arms.
The most common reasons reported by participants for not initiating ART, despite being eligible by national guidelines, were “I was told I was not eligible” when assessed at the HIV clinic (58%), clinic barriers such as needing multiple visits for ART assessment (18%), and personal reasons such as not feeling sick (13%).
Changes in male circumcision uptake
Study retention at nine months in the male circumcision arms was 98% (734/750). Overall, uptake of visits to a male circumcision facility was high (523/750, 70%), without significant differences between arms (Table 3). However, by month three, uptake of male circumcision was significantly higher in the text message promotion arm (137/284, 48%) compared to the referral arm (62/224, 28%) (RR=1.72, 95% CI: 1.36, 2.17), as was uptake of male circumcision uptake in the lay counselor follow-up arm (106/226, 47%) compared to the referral arm (RR=1.67, 95% CI: 1.29, 2.14). This effect of increased male circumcision uptake seen with text messaging and lay counselor visits was similar and sustained at the month nine exit visit, and did not change when we excluded participants prior to confirmation of text message delivery.
Table 3.
Impact of linkage strategies on medical male circumcision uptake among HIV uninfected, uncircumcised males
| Visited circumcision facility |
Obtained circumcision by month 3 |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | RR | (95% CI) | p-value | n | % | RR | (95% CI) | p-value | |
| LINKAGE STRATEGY * | |||||||||||
| Circumcision promotion | 230 | 151/224 | 67.4 | — | reference | — | 62/224 | 27.7 | — | reference | — |
| Text message encouragement | 288 | 210/284 | 73.9 | 1.09 | (0.97, 1.21) | 0.134 | 137/284 | 48.2 | 1.72 | (1.36, 2.17) | < 0.001 |
| Lay counselor follow-up | 232 | 162/226 | 71.7 | 1.05 | (0.93, 1.19) | 0.403 | 106/226 | 46.9 | 1.67 | (1.29, 2.14) | < 0.001 |
N = number enrolled (and in subset if applicable)
n = proportion with outcome amouuung those ever assessed for outcome
RR = relative risk; CI = confidence interval
Models adjusted for country
Discussion
This study evaluated community-based home and mobile HIV testing and linkage strategies to HIV care and male circumcision in six rural, medium and high HIV prevalence areas in Uganda and South Africa. Uptake of HIV testing was nearly universal, the rate of linkage to an HIV clinic among HIV-positive persons was over 90% and uptake of male circumcision among uncircumcised men in the intervention arms was 50%. However, despite the high overall uptake of linkage to HIV clinics, only 37% of all HIV-positive persons initiated ART by nine months. Lay counselor facilitation of the initial HIV clinic visit modestly increased clinic linkage and lay counselor follow-up home visits modestly increased ART uptake. For male circumcision uptake, simple strategies of encouraging text message reminders and lay counselor visits increased uptake of facility visits and male circumcision, successfully increasing demand where supply was adequate. Importantly, the rate of HIV disclosure was high and no social harms were reported.
For HIV-positive persons, although point-of-care CD4 testing at the initial HIV testing visit increased the proportion of individuals who received a CD4 count by 25%, this effect was not sustained through the continuum of HIV care, which is similar to previous studies.17 As guidelines move to ART at all CD4 counts, the utility of CD4 testing at the time of HIV testing decreases in terms of guiding opportunistic infection prophylaxis for severely immunocompromised persons. Although the high uptake of linkage to care in the standard of care arm highlights the acceptability and effectiveness of community-based HTC in encouraging linkage to care, clinic facilitation and lay counselor follow-up visits only modestly increased linkage to clinic and ART initiation, which we hypothesized would be more substantial.18,23,24 A bottleneck in achieving viral suppression in all arms was the high proportion of ART-eligible participants (58%) not starting ART who were told at HIV clinics that they were not eligible for ART. Thus, community-based testing with lay counselor strategies for linkage are successful in increasing demand for ART but the impact is limited by process of repeat CD4 testing at the clinic, ART adherence counseling requirements and other barriers to ART initiation at the clinics.
Among HIV-negative, uncircumcised men who had access to secure text messaging, text message reminders and lay counselor follow-up visits were equally effective in significantly increasing uptake of male circumcision services (47%-48% at month three) compared to counseling at the point of testing (28%). Thus, simple and scalable linkage strategies can increase the uptake of male circumcision, given sufficient supply. There were fewer clinic barriers to accessing male circumcision services compared to ART initiation, increasing the impact of simple strategies such as text messages that get patients to the clinic.
The main limitation of the study was that health care facility visits, ART initiation and male circumcision uptake were confirmed by examination of clinic cards and ART medication bottles, because clinic electronic health records were not available to verify clinic attendance or pharmacy dispensing. Also, a substantial proportion (311/1,325, 24%) of HIV-positive persons enrolled in the study had a suppressed viral load at enrollment, despite reporting that they were not on ART (an inclusion criterion for the study), possibly to access viral load testing through the study, which was not routinely provided in HIV clinics during the study period. Samples were not stored, so we were not able to measure antiretrovirals in the plasma of persons who were virally suppressed but reported not being on ART.
In summary, community-based HIV testing and lay counselor led linkage strategies in rural South Africa and Uganda achieved extremely high coverage of HIV testing, and served as a platform for combination HIV prevention. These strategies have the potential to cost-effectively avert incident HIV infections,25,26 and may generate economic benefits for persons receiving ART.27 To build on the near universal reach of community-based HIV testing, decentralized ART delivery services have the potential to overcome bottlenecks in care at overburdened clinics.28 Current ART regimens are often once-daily, safe and well-tolerated,29 thus, moving ART initiation and refill supply into the community, in addition to testing, would overcome barriers to care for HIV-positive persons who do not need clinic services.19 To reach the UNAIDS goal of 73% of HIV-positive persons virally suppressed11 and 80% of HIV-negative men accessing male circumcision,9 requires highly effective combination HIV prevention. The utilization of community-based approaches and trained lay persons in communities most affected by HIV are key components of such as approach.
Research in Context
Evidence before this study
We searched PubMed, EMBASE and conference abstracts for community-based HIV testing and linkage studies published between January 1st, 2000, and January 31st 2016, with the terms “HIV infections/diagnosis” AND “Africa South of the Sahara” AND (“mass screening” OR test OR tests OR testing OR screen* OR diagnosis OR “counseling”). We identified 156 abstracts for review, including three systematic reviews. A recent review by Sharma and colleagues reported that linkage to care, defined as visiting a clinic after community testing, was reported for eighteen studies; ten home, six mobile, and two campaign testing studies. Using random effects meta-analysis, home testing achieved high linkage (95%, 95% CI: 87-98%) when paired with enhanced linkage to care interventions (i.e. lay counselor follow-up to encourage clinic visit) compared to home testing interventions without facilitated linkage to care (26% linkage, 95% CI 18-36%). Similarly, the mobile testing strategies that did not include facilitated linkage strategies achieved 37% linkage (95% CI 24-51%) and the one campaign testing strategy, with enhanced linkage, achieved linkage rates of 81% (95% CI 76-85%). Four home testing studies reported ART initiation among those eligible, with higher linkage rates for interventions with enhanced linkage to care vs. those without (76%, 95% CI 68-82% vs. 16%, 95% CI 12-20%). A review by Wynberg and colleagues found that point-of-care CD4 testing decreases time to ART eligibility assessment, but did not change ART adherence. In a recent meta-analysis of text message interventions to promote ART adherence, improved viral suppression and/or CD4 outcomes was associated with two-way, less frequent than daily, and personalized text messages. Lastly, a review of community support groups found peer- or lay counselor-delivered ART can overcome barriers to retention in care and decongest health services in sub-Saharan Africa.
Added value of this study
This study adds to the evidence on the effectiveness of community-based testing with 98% of the population approached agreeing to testing, and the role of linkage strategies to deliver combination HIV prevention. Specifically, all three strategies – lay counselor-delivered strategies, i.e. clinic facilitation and lay counselor home visits for HIV-positive persons –, achieved over 90% rate of linkage to clinic but only one-third of all HIV positive persons initiated ART, and no strategy was more effective in the proportion of HIV-positive persons achieving viral suppression after nine months, probably due to limits of ART supply. Encouragingly, uptake of HIV testing and HIV clinic follow-up was very high in the standard referral arm as well as the intervention arms, indicating that community-based HTC achieves an effect in the early part of the HIV testing and care cascade, but that strategies to simplify and expedite ART initiation are needed. For HIV-negative, uncircumcised men, text message support and lay counselor visits increased the uptake of male circumcision almost two fold.
Implications of all the available evidence
The intervention was successful in modestly increasing ART uptake and linkage to male circumcision in two countries, South Africa and Uganda, supporting the generalizability of this approach in high and medium HIV prevalence settings in Africa. These coordinated, decentralized community-based HIV testing and linkage strategies that involve lay counselors have the potential to cost-effectively achieve high population coverage for combination HIV prevention. Evaluation of the effectiveness and cost of implementation will add to the evidence to guide HIV prevention.
Acknowledgements
We are grateful to the study volunteers for their participation in this study. We acknowledge the outstanding work of the ICOBI, HSRC and UW study teams.
Funding: The authors acknowledge funding from National Institute of Allergy and Infectious Diseases (NIAID) of the US National Institutes of Health (NIH, RC4 AI092552). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Contributors: RVB, CC, HvR and ET oversaw the implementation of the study. RVB wrote the first draft of the paper, which was revised by all authors. All authors contributed to design and execution of the study, as well as to the interpretation of findings. JB and TS did the statistical analysis with input from KKT, RB, JMB, JH and CC. All the authors approved the final version of the paper for submission.
Declaration of interests: We declare that we have no conflicts of interest.
Regulatory: All participants provided written informed consent. The University of Washington Institutional Review Board, the Ugandan National HIV/AIDS Research Committee, and the Human Sciences Research Council Research Ethics Committee approved this study.
Meetings at which preliminary data were presented: 8th IAS Conference on HIV Pathogenesis, Treatment and Prevention (IAS 2015). 19-22 July 2015. Vancouver, Canada. Community-based HIV testing and linkage effectively delivers combination HIV prevention: results from a multisite randomized trial. Abstract number: A-729-0249-03531
References
- 1.Geldsetzer P, Bloom D, Humair S, Bärnighausen T. Copenhagen Consensus Perspective Paper Health - HIV/AIDS: Benefits and costs of the HIV/AIDS targets for the post-2015 development agenda. Copenhagen Consensus Center; Frederiksberg, Denmark: 2015. [Google Scholar]
- 2.Anderson S, Cherutich P, Kilonzo N, et al. Maximising the Impact of Combination HIV Prevention through Prioritising the People and Places in Greatest Need. Lancet. 2014 doi: 10.1016/S0140-6736(14)61053-9. [DOI] [PubMed] [Google Scholar]
- 3.Weiss HA, Dickson KE, Agot K, Hankins CA. Male circumcision for HIV prevention: current research and programmatic issues. Aids. 2010;24(Suppl 4):S61–9. doi: 10.1097/01.aids.0000390708.66136.f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS medicine. 2005;2(11):e298. doi: 10.1371/journal.pmed.0020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369(9562):643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 6.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369(9562):657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 7.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. The New England journal of medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donnell D, Baeten JM, Kiarie J, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375(9731):2092–8. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sgaier SK, Reed JB, Thomas A, Njeuhmeli E. Achieving the HIV prevention impact of voluntary medical male circumcision: lessons and challenges for managing programs. PLoS medicine. 2014;11(5):e1001641. doi: 10.1371/journal.pmed.1001641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tanser F, Barnighausen T, Grapsa E, Zaidi J, Newell ML. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science. 2013;339(6122):966–71. doi: 10.1126/science.1228160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.UNAIDS Fast-Track: Ending the AIDS Epidemic by 2030. 2014 http://www.unaids.org/sites/default/files/media_asset/JC2686_WAD2014report_en.pdf.
- 12.Alsallaq RA, Baeten JM, Celum CL, et al. Understanding the potential impact of a combination HIV prevention intervention in a hyper-endemic community. PloS one. 2013;8(1):e54575. doi: 10.1371/journal.pone.0054575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sabapathy K, Van den Bergh R, Fidler S, Hayes R, Ford N. Uptake of home-based voluntary HIV testing in sub-Saharan Africa: a systematic review and meta-analysis. PLoS medicine. 2012;9(12):e1001351. doi: 10.1371/journal.pmed.1001351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma M, Ying R, Tarr G, Barnabas R. Systematic review and meta-analysis of community and facility-based HIV testing to address linkage to care gaps in sub-Saharan Africa. Nature. 2015;528(7580):S77–85. doi: 10.1038/nature16044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suthar AB, Ford N, Bachanas PJ, et al. Towards universal voluntary HIV testing and counselling: a systematic review and meta-analysis of community-based approaches. PLoS medicine. 2013;10(8):e1001496. doi: 10.1371/journal.pmed.1001496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wynberg E, Cooke G, Shroufi A, Reid SD, Ford N. Impact of point-of-care CD4 testing on linkage to HIV care: a systematic review. Journal of the International AIDS Society. 2014;17:18809. doi: 10.7448/IAS.17.1.18809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jani IV, Sitoe NE, Alfai ER, et al. Effect of point-of-care CD4 cell count tests on retention of patients and rates of antiretroviral therapy initiation in primary health clinics: an observational cohort study. Lancet. 2011;378(9802):1572–9. doi: 10.1016/S0140-6736(11)61052-0. [DOI] [PubMed] [Google Scholar]
- 18.van Rooyen H, Barnabas RV, Baeten JM, et al. High HIV testing uptake and linkage to care in a novel program of home-based HIV counseling and testing with facilitated referral in KwaZulu-Natal, South Africa. Journal of acquired immune deficiency syndromes. 2013;64(1):e1–8. doi: 10.1097/QAI.0b013e31829b567d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Decroo T, Rasschaert F, Telfer B, Remartinez D, Laga M, Ford N. Community-based antiretroviral therapy programs can overcome barriers to retention of patients and decongest health services in sub-Saharan Africa: a systematic review. International health. 2013;5(3):169–79. doi: 10.1093/inthealth/iht016. [DOI] [PubMed] [Google Scholar]
- 20.Chamie G, Kwarisiima D, Clark TD, et al. Uptake of community-based HIV testing during a multi-disease health campaign in rural Uganda. PloS one. 2014;9(1):e84317. doi: 10.1371/journal.pone.0084317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Finitsis DJ, Pellowski JA, Johnson BT. Text message intervention designs to promote adherence to antiretroviral therapy (ART): a meta-analysis of randomized controlled trials. PloS one. 2014;9(2):e88166. doi: 10.1371/journal.pone.0088166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2011;376(9755):1838–45. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 23.Barnabas RV, Van Rooyen H, Tumwesigye E, et al. Initiation of antiretroviral therapy and viral suppression after home HIV testing and counselling in KwaZulu-Natal, South Africa, and Mbarara district, Uganda: a prospective, observational intervention study. Lancet HIV. 2014:70024–4. doi: 10.1016/S2352-3018(14)70024-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tumwebaze H, Tumwesigye E, Baeten JM, et al. Household-based HIV counseling and testing as a platform for referral to HIV care and medical male circumcision in Uganda: a pilot evaluation. PloS one. 2012;7(12):e51620. doi: 10.1371/journal.pone.0051620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith J, Sharma M, Levin C, et al. Community-based strategies to strengthen the continuum of HIV care are cost-effective in rural South Africa: a health economic modelling analysis. Lancet HIV. 2015 doi: 10.1016/S2352-3018(15)00016-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eaton JW, Menzies NA, Stover J, et al. Health benefits, costs, and cost-effectiveness of earlier eligibility for adult antiretroviral therapy and expanded treatment coverage: a combined analysis of 12 mathematical models. The Lancet Global health. 2014;2(1):e23–34. doi: 10.1016/S2214-109X(13)70172-4. [DOI] [PubMed] [Google Scholar]
- 27.Thirumurthy H, Chamie G, Jain V, et al. Improved employment and education outcomes in households of HIV-infected adults with high CD4 cell counts: evidence from a community health campaign in Uganda. Aids. 2013;27(4):627–34. doi: 10.1097/QAD.0b013e32835c54d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.MacPherson P, Lalloo DG, Webb EL, et al. Effect of optional home initiation of HIV care following HIV self-testing on antiretroviral therapy initiation among adults in Malawi: a randomized clinical trial. JAMA. 2014;312(4):372–9. doi: 10.1001/jama.2014.6493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delaugerre C, Ghosn J, Lacombe J, et al. Significant Reduction in HIV Virologic Failure During a 15-Year Period in a Setting With Free Healthcare Access. Clinical Infectious Diseases. 2015;60:463–72. doi: 10.1093/cid/ciu834. [DOI] [PubMed] [Google Scholar]