Abstract
BACKGROUND
The Child Health Initiative for Lifelong Eating and Exercise is a multi-component obesity-prevention intervention, which was evaluated among Head Start (HS) centers in American Indian and predominantly Hispanic communities in rural New Mexico. This study examines the intervention’s foodservice outcomes: fruits, vegetables, whole grains, discretionary fats, added sugars, and fat from milk served in meals and snacks.
METHODS
Sixteen HS centers were randomized to intervention/comparison groups, following stratification by ethnicity and pre-intervention median body mass index of enrolled children. The foodservice component included quarterly trainings for foodservice staff about food purchasing and preparation. Foods served were evaluated before and after the 2-year intervention, in the fall 2008 and spring 2010.
RESULTS
The intervention significantly decreased fat provided through milk and had no significant effect on fruit, vegetables and whole-grain servings, discretionary fats, and added sugar served in HS meals and snacks. When effect modification by site ethnicity was examined, the effect on fat provided through milk was only found in American Indian sites.
CONCLUSIONS
Foodservice interventions can reduce the amount of fat provided through milk served in HS. More research is needed regarding the implementation of foodservice interventions to improve the composition of foods served in early education settings.
Keywords: child, preschool, American Indians, Hispanic Americans, school foodservice, obesity prevention
Obesity among preschool-age children is a serious public health problem that may lead to long-term, negative health consequences persisting into adulthood.1–7 Rural, low-income and minority children experience a disproportionate obesity burden.2,8,9 Children’s dietary intake is a direct, modifiable cause of childhood obesity and is influenced by a myriad of social, environmental and policy contexts.10 Evidence among adults suggests that reduction in dietary fat intake, replacement of refined carbohydrates with high-fiber foods, increase in fruits and vegetable intake, consumption of low-fat dairy and reduction in intake of sugar-sweetened beverages, among other factors, play a role in obesity prevention.11 The evidence is less conclusive for children, though the relationship tends in the same direction.11 There is consistent evidence for a relationship between sugar-sweetened beverage and overall energy-dense food consumption and children’s body weight.12–14 Early childhood in particular presents a window of opportunity for prevention of obesity, and it is a crucial period for development of children’s food preferences and eating patterns.15,16
Early education and childcare settings can play a significant role in the development of children’s eating patterns.17–20 Several reviews have summarized research in the past two decades describing the quality of foods provided in these settings, most of which enrolled centers participating in the Child and Adult Care Food Program (CACFP) administered by U.S. Department of Agriculture (USDA).18,21,22 These studies suggest that meals offered in these settings are inconsistent with the Dietary Guidelines for Americans in that they exceed maximum recommended intakes for saturated fat and sodium and do not meet recommended fruit and vegetable servings.23,24
In a national study, Butte et al found that preschool children do not consume enough fiber and consume too much saturated fat and sodium compared to what is recommended by the Dietary Guidelines for Americans.25,26 When examining the foods consumed by preschool-age children, 3 years of age, Fox et al found that whereas most consume more servings of fruit as whole fruit than as 100 percent juice, they do not consume a sufficient variety of vegetables, they consume 2% and whole milk instead of 1% and fat-free milk, and a majority consume one or more sweetened beverages, desserts or snack foods per day.27 Although childcare centers are not shown to contribute disproportionately to children’s intake of saturated fat and sodium compared to intake outside of care, improvement in food provided in early education and childcare settings has the potential to improve the quality of children’s overall diet.28
Head Start (HS) has been identified as a model for other child-service programs and presents a unique opportunity to reach children who are at increased risk for obesity, because it serves low-income children.29 HS program standards require nutrition services to provide one-third to two-thirds of children’s daily nutritional needs, depending on length of daily enrollment, and to provide a variety of foods high in nutrients and low in fat, sugar and salt.30 In addition, foods provided by HS centers are regulated by CACFP, which specifies daily food patterns eligible for reimbursement.31 These standards require provision of several food groups throughout the day and specify that: (1) only 100 percent fruit or vegetable juice can be used; (2) breads and grains be made from whole or enriched meal or flour; and (3) cereals be whole-grain, enriched or fortified. These standards lay the basis for the provision of nutritious meals at HS centers, but they do not specifically require that meals align with the Dietary Guidelines for Americans.26 Although HS centers often report exceeding these federal standards,32 there is room for improvement.
To date, few interventions in the preschool setting have included a foodservice component, addressing the quality and nutrient content of meals and snacks provided at the preschool.18,33–37 Of the interventions that did,34–37 fewer still evaluated the component’s impact on foodservice practices and composition of meals.34,36,37 To the authors’ knowledge, no preschool foodservice interventions have been evaluated in American Indian communities.
The Child Health Initiative for Lifelong Eating and Exercise (CHILE) was a 5-year study that developed and evaluated a multi-level obesity-prevention intervention among preschool children enrolled in rural New Mexico HS centers located in American Indian and predominantly Hispanic communities. The theoretical framework for the intervention is based on the socio-ecological trans-community model, in which several levels of influence contribute to children’s health, including individual, interpersonal, organizational, community, and public policy.38 The CHILE intervention focuses on HS children, their families, HS centers, and local communities.38 The main outcome of the CHILE study was body mass index (BMI) and will be reported elsewhere. Results of other measurements including formative assessment,39 dietary intake, physical activity and screen time, family eating behaviors, retail food environment and process evaluation are or will be reported separately as well.
This paper identifies the impact of the CHILE intervention on foods served in enrolled HS centers. Specifically, it describes the intervention effect on fruit, vegetable, and whole-grain servings; amount of discretionary fat; amount of added sugars; and amount of fat from milk provided in HS meals.
METHODS
Study Design
The CHILE study was a controlled trial with a stratified, group-randomized design at the site level, with 16 participating HS centers in American Indian and predominantly Hispanic communities in rural New Mexico. Potential HS centers were identified for participation in the study based on the following criteria: (1) HS center enrolled predominantly Hispanic or American Indian children; (2) HS center enrolled a minimum of 20 3-year-old children; and (3) HS center retained at least 80% of its students for 2 years. HS centers in metropolitan areas were not eligible for inclusion, and HS centers within 150 miles of Albuquerque were prioritized to minimize travel expense. Distance to participating communities averaged 82 miles and ranged from 17 to 176 miles one way. The engagement, recruitment and retention processes are further described elsewhere.40
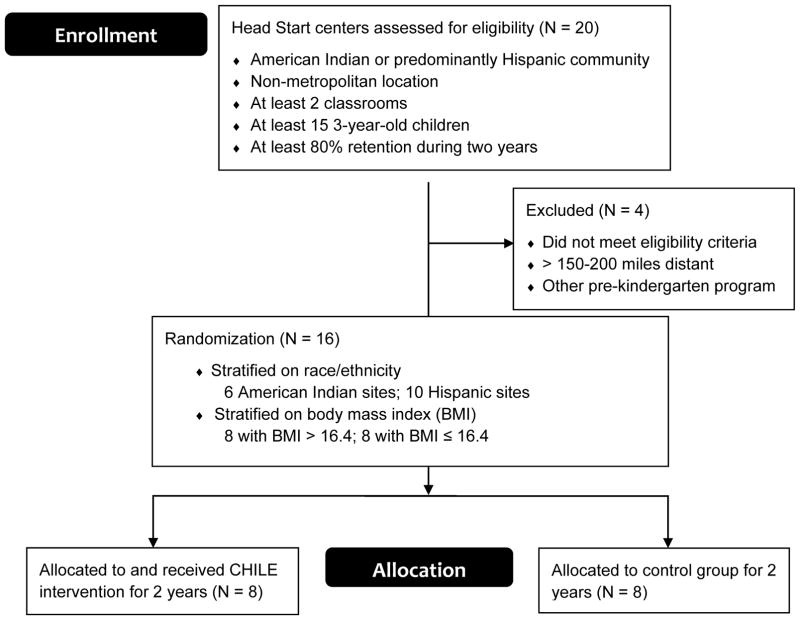
Randomization to intervention and comparison groups occurred at the HS center level (Figure 1). Centers were assigned to intervention (N = 8) or comparison (N = 8) group after being stratified by ethnicity (American Indian N = 6, Hispanic N = 10) and HS BMI (lower-BMI≤16.4 N = 8, higher-BMI>16.4 N = 8). The BMI cut-off point of 16.4, chosen on the basis of a pre-randomization sample of 3-year-old children measured by center staff, was close to the median and allowed a balanced distribution of HS centers within each racial/ethnic group. Among American Indian centers, 3 were in each BMI group. Among Hispanic centers, 5 were in each BMI group. Within each of the 4 categories of median BMI and site ethnicity, centers were randomly assigned to intervention and comparison groups.
Figure 1.
CONSORT Diagram for the CHILE Study.
The intervention and data collection occurred over a 2-year period. The baseline measures were collected in fall 2008. They were immediately followed by implementation of the CHILE intervention among the intervention sites while comparison sites followed classroom activities and foodservice as usual. The 2-year intervention spanned the 2008–2009 and 2009–2010 school years. Immediately after the conclusion of the intervention, follow-up measures were collected in spring 2010.
CHILE Intervention
The design and content of the entire CHILE intervention have been described elsewhere.38,40 Briefly, the intervention includes 6 components: (1) CHILE nutrition and physical activity curriculum; (2) professional development for HS staff; (3) foodservice; (4) family engagement; (5) community grocery store; and (6) healthcare provider. Table 1 details the objectives and content of the intervention by intervention component. The CHILE curriculum component forms the core of the intervention and consists of nutrition and physical activity lessons delivered to children in classrooms. The nutrition lessons are closely related to and supported by the foodservice component, and center on providing young children with repeated tasting opportunities to overcome their unwillingness to try new foods and to develop a preference for them.15,41–43 The CHILE nutrition curriculum is divided into 8 modules intended for implementation over 2 school years, and during each module, children complete 8 classroom tasting lessons focused on either a target fruit or vegetable.
Table 1.
Components of the CHILE Intervention
| Component | Objectives | Content |
|---|---|---|
| Nutrition and physical activity curriculum | Increase structured PA by 30 minutes/day Provide repeated opportunities to try new FVs |
Activities to increase structured PA Nutrition modules with repeated opportunities to taste target FVs |
| Professional development | Support HS teaching and food- service staff in implementing CHILE | Quarterly training modules Instructions and strategies for curriculum implementation Nutrition and PA education |
| Food service | Increase the variety of FVs served Increase the amount of whole- grain foods and low-fat dairy products served Improve food-preparation methods |
Servings of target FVs at least 4 times/quarter Recommendations to replace refined-grain foods with whole- grain foods when possible Recommendations to replace higher-fat with lower-fat dairy products when possible Recommendations to drain and rinse ground beef before serving |
| Family | Increase consumption of FVs and whole grains Decrease consumption of SSBs and high-fat foods Increase PA Decrease sedentary time |
Curriculum-linked take-home materials with information, activities, recipes, and ideas for increasing PA and improving dietary behavior Family events |
| Grocery stores | Increase availability and visibility of healthier foods Provide nutrition information and recipes to HS families |
Shelf labels identifying target CHILE foods Nutrition information brochures Six module-specific recipes/quarter |
| Health care providers | Reinforce CHILE messages during clinic visits and at HS family events | Participation of health care providers in CHILE family events CHILE messages incorporated into clinic visits with HS families |
CHILE, Child Health Initiative for Lifelong Eating and Exercise; FVs, fruits and vegetables; HS, Head Start; PA, physical activity; SSBs, sugar-sweetened beverages.
As part of the foodservice intervention component, the foodservice staff received quarterly training aimed at making policy and behavioral changes to food purchasing and menus. The number of foodservice staff directly implementing CHILE ranged from 1 to 4 per HS. All training sessions had at least the head cook in attendance, other cooks and, on occasion, foodservice directors. The CHILE project provided technical assistance but no monetary resources to HS foodservice programs to implement this component of the intervention.
Foodservice staff members are asked to include target fruits and vegetables 4 times each in meals and snacks at the same time that CHILE nutrition lessons are done in classrooms with the same fruits and vegetables. This combination of classroom lessons and foodservice provides children with a total of 8 exposures to each fruit and vegetable during every module. In addition, foodservice staff are asked to implement the following practices: (1) using fruits and vegetables that are fresh, frozen, or canned without added sugars or high-fat sauce, and if fruits canned in syrup were unavoidable, foodservice staff are asked to rinse off the syrup; (2) switching to whole-grain bread, pasta, and tortillas; (3) switching to low-fat dairy products (1% milk and low-fat cheese [≤6g fat per serving]); (4) switching to brown rice; (5) using whole-grain, low-sugar (≤7g per serving) ready-to-eat cereals; and (6) rinsing and draining ground beef after cooking to reduce fat content. The training also included the recommendation of the American Academy of Pediatrics that consumption of fruit juice among preschool-age children be limited to no more than 4 to 6 ounces per day, given that fruit juice is not equivalent to whole fruits in nutritional content.45 The content of the foodservice component was developed in accordance with the 2005 Dietary Guidelines for Americans, with emphasis on limiting excess calories from fat and sugar and addressing the inadequate intake of fruits, vegetables and whole grains.24
Outcome Measures
Foodservice measures were collected through direct observations of foodservice staff during announced visits to HS sites. These data were collected in each HS center during 5 weekdays immediately before implementation of the 2-year intervention and immediately afterwards, in fall 2008 and spring 2010. Every effort was made to collect foodservice data on 5 consecutive days within the same week. However, when logistical issues prevented data collection on one day in a designated week, the day was made up during an alternate week in the data collection period. Trained and certified CHILE data collection personnel observed foodservice staff during all meals and snacks prepared on each data collection day using the CHILE Food Service Data Collection protocol and forms. For every meal and snack prepared, the portion per child of each food was recorded and weighed. For processed foods, information from the packaging was recorded, and food labels and nutrition fact panels were retained. For recipes, descriptions and amounts of each ingredient were recorded.
Foodservice data were analyzed by 2 registered dietitians from UNM General Clinical Research Center and one registered dietitian from UNM Prevention Research Center using the Food Intake Analysis System Millennium 1.0 Version to calculate food group servings and nutrients offered per child based on the Pyramid Servings Database for USDA Survey Codes 1.0.45 The following outcome variables were retained for analysis: total daily vegetable and whole grain servings; grams of discretionary fat, which is fat in a food above the amount that would be found in a lean, low-fat, or fat-free form of the food; and teaspoons of added sugar provided, which are sugars added to foods during processing or preparation, not including naturally occurring sugars. The discretionary fat and added sugar variables, rather than total fat or sugar, were selected for analysis as they captured the choice in selecting and cooking healthful foods that was part of the foodservice training. A variable for grams of fat contributed daily by milk was calculated to measure changes in the fat content of milk. A daily fruit servings variable was created, which excluded fruit juice from the fruit servings calculation, to accurately represent the changes recommended in the intervention, as foodservice staff were asked to modify their inclusion of whole fruits in meals and snacks.
The resulting foodservice measures pertain to the average serving per child of food provided by HS centers for each day of the week. Daily values were retained so that effects of foodservice practices that varied by day; for example, provision of breakfast or snacks and day of week could be investigated. No observations of food consumed or plate waste measurements were conducted.
Other Study Measures
Categorical variables were created to describe the site ethnicity (American Indian, Hispanic), data collection day (Monday through Friday), whether breakfast was provided on the data collection day (yes, no), and whether snack was provided on the data collection day (yes, no). HS site size was expressed as a continuous variable measuring the average number of students enrolled at the site during the follow-up period. Change in HS size during the follow-up period was expressed as the difference in the average number of students enrolled in each HS between year 1 and year 2 of follow-up.
Data Analysis
Characteristics of sites were compared using the Wilcoxon-rank sum test for continuous variables and the chi-square test or Fisher’s exact test for categorical variables. Variables that differed between intervention and comparison sites were retained as possible confounders or covariates.
The effect of the intervention on the number of fruit, vegetable and whole grain servings, grams of discretionary fat, teaspoons of added sugar, and grams of fat from milk provided in HS meals and snacks was examined using multi-level modeling.46 The outcome variables were natural-log-transformed to improve normality and to stabilize variance. The mixed linear model (MIXED procedure) was used with the intervention variable, time variable, intervention x time interaction, day of the week, snack variable and breakfast variable as fixed factors, and site variable as a random factor to control for the clustering effect of the repeated measures within each study site. The difference in change over time between the intervention and control sites was tested using the intervention x time interaction. As the outcome variables were log-transformed before analyses, when the effect size estimates are back-transformed this contrast can be interpreted as the ratio of the change over time for the intervention sites to the change over time for control sites: (Intervention Group in 2010 / Intervention Group in 2008) / (Control Group in 2010 / Control Group in 2008).
As a secondary analysis, not originally planned as part of the CHILE study, results were also examined for effect modification by community type (predominantly Hispanic or American Indian). Interaction between the intervention effect over time and community type was examined for significance, and where significant (p < .05), the results are reported separately by community type.
Variables for HS size and change in HS size during follow-up were hypothesized to influence the foods served at the HS, but were not included because they did not differ between intervention and comparison sites and model effect sizes did not substantially change after adjustment with these variables. Data analysis was conducted using Statistical Analysis Systems statistical software package version 9.2 (SAS Institute, Cary, NC, USA).
RESULTS
Intervention and control sites were similar with no differences in HS size, change in HS size, or days with breakfast or snacks (Table 2). The intervention sites experienced a statistically significant decrease in daily grams of fat from milk over time, compared to the comparison sites (Table 3). There were no statistically significant differences between the groups over time in daily fruit, vegetable and whole-grain servings, grams of discretionary fat, and teaspoons of added sugar (Table 3). Intervention sites reduced their daily provision of fat from milk 18% more than comparison sites. The variance component estimates from the main analysis models are the following: σsite=0.004 and σresidual=0.059 for fruit; σsite=0.002 and σresidual=0.064 for vegetables; σsite=0.001 and σresidual=0.076 for whole-grains; σsite=0.037 and σresidual =0.114 for discretionary fat; σsite=0.043 and σresidual=0.357 for added sugar; and, σsite=0.069 and σresidual=0.119 for fat from milk.
Table 2.
Descriptive Variables for Head Start Sites in the Child Health Initiative for Lifelong Eating and Exercise (CHILE) Study
| Control Sites | Intervention Sites | |||
|---|---|---|---|---|
| Descriptive Variables | N | Mean (SD) | N | Mean (SD) |
| Head Start size (number of students) | 8 | 87.9 (26.9) | 8 | 80.9 (46.2) |
| Change in Head Start size during intervention period (number of students)a | 8 | 0.5 (3.6) | 8 | 0.8 (18.3) |
| Nc | % | Nc | % | |
| Snack was served (%)b | 80 | 66.3 | 80 | 60.0 |
| Breakfast was served (%)b | 80 | 98.8 | 80 | 100.0 |
As the variable change in Head Start size is not normally distributed, a median is presented instead of a mean.
Variables ‘snack was served’ and ‘breakfast was served’ refer to the percentage of data collection days on which breakfast or snack was served, with 10 data collection days per each Head Start site.
The sample size for these variables at baseline refers to 5 data collection days per each Head Start site.
Table 3.
Effect of the Intervention on Total Daily Fruit, Vegetable and Whole-Grain Servings, Grams of Discretionary Fats and Fat from Milk, and Teaspoons of Added Sugar Provided in Head Start Meals in the Child Health Initiative for Lifelong Eating and Exercise (CHILE) Studya,b
| Fall 2008 | Spring 2010 | Intervention vs. Control | |||
|---|---|---|---|---|---|
| Outcome Measure | Mean(SE)c | Mean(SE)c | Change | Change Intervention / Change Controld | (95% CI) |
| Fruit (servings)e | |||||
| Intervention | 1.37(0.05) | 1.28(0.05) | −0.09 | 1.02 | (0.88, 1.19) |
| Control | 1.40(0.05) | 1.25(0.05) | −0.15 | ||
| Vegetables (servings) | |||||
| Intervention | 0.67(0.04) | 0.89(0.04) | 0.22 | 1.07 | (0.91, 1.25) |
| Control | 0.81(0.04) | 0.92(0.04) | 0.11 | ||
| Whole grains (servings) | |||||
| Intervention | 0.31(0.04) | 0.33(0.04) | 0.02 | 1.09 | (0.92, 1.30) |
| Control | 0.31(0.05) | 0.22(0.04) | −0.09 | ||
| Discretionary fat (grams) | |||||
| Intervention | 20.10(0.09) | 19.77(0.09) | −0.32 | 1.00 | (0.81, 1.24) |
| Control | 19.35(0.09) | 18.98(0.09) | −0.37 | ||
| Added sugar (teaspoons) | |||||
| Intervention | 2.58(0.13) | 2.23(0.13) | −0.35 | 0.94 | (0.65, 1.37) |
| Control | 3.21(0.13) | 3.03(0.13) | −0.18 | ||
| Milk fat (grams) | |||||
| Intervention | 7.07(0.10) | 5.50(0.10) | −1.57 | 0.82 | (0.71, 0.94)* |
| Control | 6.38(0.10) | 6.26(0.10) | −0.13 | ||
The analysis models consist of the intervention variable, time variable, intervention x time interaction term, day of the week, snack variable and breakfast variable as fixed factors, and site variable as a random factor.
The sample size per analysis group (N = 40) is based on 5 measurements in each Head Start site.
Adjusted geometric mean. SE refers to standard error of the estimate.
As outcome variables were log-transformed, a relative change estimate is calculated to compare the changes in outcome variables over follow-up period between intervention and comparison groups, with the comparison group as the reference group.
The fruit outcome measure includes whole fruits only, not fruit juice.
Statistically significant at p < .05.
Effect modification by site ethnicity was examined using the interaction between intervention group, time and site ethnicity. The interaction term was found to be statistically significant for daily servings of vegetables (p=.042), teaspoons of added sugar (p=.024) and grams of fat from milk (p=.014), but was similar for fruit servings (p=.677), whole-grain servings (p=.631) and discretionary fats (p=.579).
The analyses of servings of vegetables, added sugar and fat from milk were separated by site ethnicity (Table 4) as the presence of significant interaction for these outcomes indicated that the intervention effect over time was modified by site ethnicity. Following stratification, the intervention effect over time was only significant for the fat from milk outcome and only in American Indian sites. American Indian intervention sites had a 34% greater change in fat from milk compared with comparison sites. The CHILE intervention did not significantly affect fat from milk in Hispanic sites. No statistically significant differences were observed between the intervention groups over time in daily vegetable servings and teaspoons of added sugar in either type of site.
Table 4.
Effect of the Intervention on Total Daily Vegetable Servings, Teaspoons of Added Sugar and Grams of Fat from Milk Provided in Head Start Meals by Site Ethnicity in the Child Health Initiative for Lifelong Eating and Exercise (CHILE) Studya,b
| Fall 2008 | Spring 2010 | Intervention vs. Control | |||
|---|---|---|---|---|---|
| Outcome Measure | Mean (SE)c | Mean (SE)c | Change | Change Intervention / Change Controld | (95% CI) |
| American Indian Sites | |||||
| Vegetables (servings) | |||||
| Intervention | 0.76 (0.08) | 0.91 (0.07) | 0.15 | 0.86 | (0.67, 1.11) |
| Control | 0.70 (0.08) | 1.13 (0.07) | 0.43 | ||
| Added sugar (teaspoons) | |||||
| Intervention | 1.16 (0.21) | 1.63 (0.21) | 0.47 | 1.61 | (0.84, 3.09) |
| Control | 2.75 (0.21) | 1.83 (0.21) | −0.92 | ||
| Milk fat (grams) | |||||
| Intervention | 6.17 (0.08) | 3.76 (0.08) | −2.41 | 0.66 | (0.54, 0.81) * |
| Control | 6.07 (0.08) | 6.10 (0.08) | 0.03 | ||
| Hispanic Sites | |||||
| Vegetables (servings) | |||||
| Intervention | 0.63 (0.05) | 0.89 (0.05) | 0.26 | 1.21 | (1.00, 1.48) |
| Control | 0.88 (0.05) | 0.80 (0.05) | −0.08 | ||
| Added sugar (teaspoons) | |||||
| Intervention | 3.74 (0.14) | 2.59 (0.14) | −1.15 | 0.65 | (0.41, 1.04) |
| Control | 3.49 (0.14) | 4.19 (0.14) | 0.71 | ||
| Milk fat (grams) | |||||
| Intervention | 7.73 (0.16) | 6.92 (0.16) | −0.81 | 0.96 | (0.80, 1.15) |
| Control | 6.58 (0.16) | 6.18 (0.16) | −0.40 | ||
The analysis models consist of the intervention variable, time variable, intervention x time interaction term, day of the week, snack variable and breakfast variable as fixed factors, and site variable as a random factor.
The sample size per analysis group (N = 15 for American Indian sites, N = 25 for Hispanic sites) is based on 5 measurements in each Head Start site. Of the total 16 Head Start sites, 10 were in predominantly Hispanic communities and 6 in American Indian communities.
Adjusted geometric mean. SE refers to standard error of the estimate.
As outcome variables were log-transformed, a relative change estimate is calculated to compare the changes in outcome variables over follow-up period between intervention and comparison groups, with the comparison group as the reference group.
Statistically significant at p < .05.
DISCUSSION
The purpose of this study was to describe the impact of the CHILE intervention on foods served in the enrolled HS centers that have the potential to prevent obesity: fruits, vegetables, whole-grains, discretionary fats, added sugars, and fat from milk. Intervention sites were significantly different from comparison sites in reduction of fat provided through milk over the follow-up period. While decreases in fat from milk were observed in all intervention sites compared to comparison sites, the difference only remained significant in American Indian sites when the intervention effect over time was examined for effect modification by site ethnicity. Preschool children currently consume on average 2 to 4 grams of saturated fat per day in excess of the recommended saturated fat limit, assuming an average daily intake of 1300 kcal.25,26,47 Though incremental, a daily 2.41 g reduction in fat from milk in preschool meals has the potential to bring preschool children’s consumption of saturated fat within the recommended limits.
These results are consistent with previous research in terms of the significant impact on total and saturated fat provided in meals and snacks.33,34,48 However, other studies in preschool and school settings documented significant changes in provision of fruits and vegetables, whereas the present study did not.33,36 In the preschool setting, Williams et al34 documented a significant impact on total and saturated fats provided in preschool meals, and Gosliner et al36 showed positive changes in the provision of fruits and vegetables. In a review of elementary and secondary school-based studies, Jaime and Lock33 concluded that the majority of studies showed a decreased total of saturated fat and increased fruit and vegetable availability following interventions targeting guidelines for school food preparation. Notably, one study that was conducted in American Indian communities, the Pathways study, was effective in reducing total and saturated fat content of elementary school meals, without negatively impacting the overall nutrient profile, by using a multi-component intervention that included a targeted foodservice component.48
The results from this study indicate that it is possible to reduce the amount of fat provided in HS meals and snacks by changing the type of milk served. For other foodservice changes that involve substituting or altering foods within the same food group, such as substituting whole grains, a more intensive intervention, such as described by Williams et al,34 may have strengthened the results. In that study, foodservice staff received a focused intervention that included monthly visits to monitor progress, and motivational and financial incentives, which may have contributed to the intervention’s success.34 Considering that the baseline provision of whole grains in the present study was low at 0.31 whole grain servings compared to up to 1.5 total grain servings specified by CACFP, a more intensive intervention may have had a significant impact.31 On the other hand, the low baseline levels of daily added sugars in preschool meals, 2.58 to 3.21 teaspoons, would most likely have improved little even with a more intensive intervention.
Effecting absolute change in servings of food groups, such as an increase in fruits and vegetables, is difficult without a national policy change governing HS foodservice. CACFP reimbursable meal patterns regulate the amount of fruits and vegetables to be served in each meal; in a day, HS centers are to serve one cup of fruits and vegetables at breakfast and lunch, and may add half of a cup of fruits and vegetables as snack.31 As HS centers only receive reimbursement for the meal pattern mandated by CACFP, change in fruit and vegetable servings following the CHILE intervention would be difficult without additional subsidy or reimbursement.49,50 The Institute of Medicine recently published its recommendations for improvements to the CACFP requirements that seek to better align the CACFP meals with the current dietary guidelines, and these recommendations are expected to be implemented in 2014.51 These recommendations include better control of calories provided, greater number and variety of fruits and vegetables, more whole-grain-rich foods, limiting milk choices to nonfat and low-fat, and further limiting foods high in solid fats and added sugars.
In a secondary analysis not originally planned in the CHILE study, this study found that the intervention effect on fat provided through milk was only statistically significant in American Indian sites. These results should be interpreted with caution because the CHILE study was not designed and powered to examine differences by community type. One hypothesis to explain the observed difference is that differences in HS administration structures affected the uptake of the CHILE intervention in the 2 types of sites. HS sites in predominantly Hispanic communities were often administered as part of a cluster of HS centers, where a parent organization administers several HS centers in a geographic area. In contrast, the American Indian HS sites were all individual HS grantees with more autonomy to make administrative decisions at the individual HS center level. Whereas, in the predominantly Hispanic HS sites proposed foodservice changes had to be reviewed by 2 or more administrative levels prior to implementation, administrators in American Indian sites were directly involved in the intervention and were able to make foodservice changes independently. This unplanned finding should be examined through further research.
Limitations
Although the group-randomized controlled design is a strength of the CHILE study, a limitation is posed by the sample size for evaluation of the foodservice component of the intervention (N = 16). The study sample size was originally calculated based on the number of sites and children necessary to detect changes in BMI, the main outcome of the overall study; the lack of a sample size calculation specific to the foodservice component may have resulted in inadequate power for this component of the study. HS centers also varied in terms of authority of head cooks and kitchen managers to make changes to purchasing patterns and HS administration support for foodservice changes,38 and variation could have occurred between sites in terms of foodservice staff turnover.40 Although the randomized design should have minimized the impact of these possible limitations, as HS variability and differences in food choice between data collection points are expected to be non-differential between intervention and comparison sites, some bias could have been introduced given the cluster design and small sample size.
Repeated observations of foods served to account for within-week variation is in line with similar studies, and avoids reliance on what is reported on HS menus.34,48,52–54 However, data collection points at the beginning and end of the school year may have attenuated the results, and this may have been improved by intermediate measures during the implementation period. The research team noted that at the end of the school year, some HS centers began using up remaining food stock in lieu of purchasing new products, which may have impacted food choices. Food choice may have been further limited by seasonal effects on availability and price of fruits and vegetables.
Conclusions
The CHILE foodservice intervention was effective in reducing the amount of fat provided in HS meals by changing the type of dairy products served, but had no significant effect on fruits, vegetables, whole-grains, discretionary fats and added sugars. More research is needed on the impact of foodservice interventions on food environments in preschool settings, as most of the evidence to date pertains to school settings.
IMPLICATIONS FOR SCHOOL HEALTH.
Early education settings have been identified as important venues for obesity prevention. This study demonstrates the challenge multi-level trans-community interventions experience in impacting foods served in preschool settings like HS. CHILE and other similar interventions succeeded in creating some changes in food preparation and service with potential to prevent obesity in preschool-age children, but effectiveness is often constrained by the national policy environment that governs reimbursement of foods. New CACFP nutrition standards that are to be implemented in 2014 will provide key supports for trans-community efforts to address complex problems like childhood obesity. Further research is necessary regarding the process of implementation of foodservice interventions in early education settings, particularly in communities underrepresented in obesity prevention research.
Acknowledgments
The authors thank the CHILE Head Start centers (especially the foodservice staff), colleagues on the CHILE team, and Rosemary Wold, formerly from the UNM Clinical and Translational Sciences Center. This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (#1-R01DK72958-1) and is registered at Clinicaltrials.gov (NCT00428805).
Footnotes
Human Subjects Approval Statement
The CHILE study was approved by the University of New Mexico (UNM) Health Sciences Center Human Research Review Committee (#06-040).
Contributor Information
Alexandra B. Morshed, Email: a.b.morshed@wustl.edu, Doctoral Student, The Brown School, Washington University in St. Louis, Campus Box 1196, One Brookings Drive, St. Louis, MO 63130-4899, Phone: (314) 824-8408, Fax: (314) 935-8511.
Sally M. Davis, Email: sdavis@salud.unm.edu, Professor, Department of Pediatrics, Director, Prevention Research Center, University of New Mexico, MSC 11 6145, Albuquerque, NM 87131. Phone: (505) 272-4462, Fax: (505) 272-4857.
Patricia C. Keane, Email: pkeane@salud.unm.edu, Associate Scientist III, Department of Pediatrics, University of New Mexico Prevention Research Center, MSC 11 6145, Albuquerque, NM 87131.
Orrin B. Myers, Email: omyers@salud.unm.edu, Research Associate Professor, Department of Internal Medicine, University of New Mexico, MSC 10 5550, Albuquerque, NM 87131.
Shiraz I. Mishra, Email: smishra@salud.unm.edu, Professor, Department of Pediatrics, University of New Mexico, Albuquerque, NM 87131.
References
- 1.New Mexico Department of Health, Healthy Kids New Mexico. [Accessed September 29, 2015];New Mexico BMI surveillance report. 2010 Available at: https://www.nmms.org/files/uploaded/files/2010BMISurveillanceReport.pdf.
- 2.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 4.Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DR, Byers T. Do obese children become obese adults? A review of the literature. Prev Med. 1993;22(2):167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- 5.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: the Bogalusa Heart Study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]
- 6.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes (Lond) 2010;35(7):891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 7.Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006;16(1):47–67. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. [Accessed September 29, 2015];Obesity among low-income preschool children. Available at: http://www.cdc.gov/obesity/downloads/pednssfactsheet.pdf.
- 9.Lutfiyya MN, Lipsky MS, Wisdom–Behounek J, Inpanbutr-Martinkus M. Is rural residency a risk factor for overweight and obesity for U.S. children? Obesity (Silver Spring) 2007;15(9):2348–2356. doi: 10.1038/oby.2007.278. [DOI] [PubMed] [Google Scholar]
- 10.Koplan JP, Liverman CT, Kraak VI Committee on Prevention of Obesity in Children and Youth. Preventing childhood obesity: health in the balance. J Am Diet Assoc. 2005;105(1):131–138. doi: 10.1016/j.jada.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 11.Woodward-Lopez G, Davis Ritchie L, Gerstein DE, Crawford PB, editors. Obesity: Dietary and Developmental Influences. Boca Raton, FL: CRC Press; 2006. [Google Scholar]
- 12.Must A, Barish EE, Bandini LG. Modifiable risk factors in relation to changes in BMI and fatness: what have we learned from prospective studies of school-aged children? Int J Obes (Lond) 2009;33(7):705–715. doi: 10.1038/ijo.2009.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newby PK. Are dietary intakes and eating behaviors related to childhood obesity? A comprehensive review of the evidence. J Law Med Ethics. 2007;35(1):35–60. doi: 10.1111/j.1748-720X.2007.00112.x. [DOI] [PubMed] [Google Scholar]
- 14.Pérez-Escamilla R, Obbagy JE, Altman JM, Essery EV, McGrane MM, Wong YP, et al. Dietary energy density and body weight in adults and children: a systematic review. J Acad Nutr Diet. 2012;112(5):671–684. doi: 10.1016/j.jand.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 15.Cooke L. The importance of exposure for healthy eating in childhood: a review. J Hum Nutr Diet. 2007;20(4):294–301. doi: 10.1111/j.1365-277X.2007.00804.x. [DOI] [PubMed] [Google Scholar]
- 16.Birch LL, Fisher JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(3 pt 2):539–549. [PubMed] [Google Scholar]
- 17.Mulligan GM, Brimhall D, West J US Department of Education. [Accessed September 29, 2015];Child care and early education arrangements of infants, toddlers, and preschoolers. 2001 Available at: http://nces.ed.gov/pubs2006/2006039.pdf.
- 18.Story M, Kaphingst KM, French S. The role of child care settings in obesity prevention. Future Child. 2006;16(1):143–168. doi: 10.1353/foc.2006.0010. [DOI] [PubMed] [Google Scholar]
- 19.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–272. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 20.Kaphingst KM, Story M. Child care as an untapped setting for obesity prevention: state child care licensing regulations related to nutrition, physical activity, and media use for preschool-aged children in the United States. Prev Chronic Dis. 2009;6(1):A11. [PMC free article] [PubMed] [Google Scholar]
- 21.Glanz F. Child and Adult Care Food Program. In: Fox MK, Hamilton W, Lin BH, editors. Effects of Food Assistance and Nutrition Programs on Nutrition and Health: Volume 3, Literature Review. Washington, DC: US Department of Agriculture; 2004. [Accessed September 30, 2015]. pp. 236–249. Available at: http://www.ers.usda.gov/media/873018/fanrr19-3_002.pdf. [Google Scholar]
- 22.Larson N, Ward DS, Neelon SB, Story M. What role can child-care settings play in obesity prevention? A review of the evidence and call for research efforts. J Am Diet Assoc. 2011;111(9):1343–1362. doi: 10.1016/j.jada.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 23.US Department of Agriculture, US Department of Health and Human Services. [Accessed September 29, 2015];Nutrition and Your Health: Dietary Guidelines for Americans. (5). 2000 Available at: http://health.gov/dietaryguidelines/dga2000/dietgd.pdf.
- 24.US Department of Agriculture, US Department of Health and Human Services. [Accessed September 29, 2015];Dietary Guidelines for Americans. (6). 2005 Available at: http://health.gov/dietaryguidelines/dga2005/document/pdf/DGA2005.pdf.
- 25.Butte NF, Fox MK, Briefel RR, Siega-Riz AM, Dwyer JT, Deming DM, et al. Nutrient intakes of US infants, toddlers, and preschoolers meet or exceed dietary reference intakes. J Am Diet Assoc. 2010;110(12 suppl):S27–S37. doi: 10.1016/j.jada.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 26.US Department of Agriculture, US Department of Health and Human Services. [Accessed September 29, 2015];Dietary Guidelines for Americans. (7). 2010 Available at: http://www.cnpp.usda.gov/sites/default/files/dietary_guidelines_for_americans/PolicyDoc.pdf.
- 27.Fox MK, Condon E, Briefel RR, Reidy KC, Deming DM. Food consumption patterns of young preschoolers: are they starting off on the right path? J Am Diet Assoc. 2010;110(12 suppl):S52–S59. doi: 10.1016/j.jada.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 28.Crepinsek MK, Burstein NR, Ghelfi LM. Maternal Employment and Children’s Nutrition: Volume I, Diet Quality and the Role of the CACFP. Washington, DC: US Department of Agriculture; 2004. [Accessed September 30, 2015]. Available at: http://www.ers.usda.gov/publications/efan-electronic-publications-from-the-food-assistance-nutrition-research-program/efan04006-1.aspx. [Google Scholar]
- 29.Gomby DS, Larner MB, Stevenson CS, Lewit EM, Behrman RE. Long-term outcomes of early childhood programs: analysis and recommendations. Future Child. 1995;5(3):6–24. [PubMed] [Google Scholar]
- 30.Code of Federal Regulations. Program performance standards for the operation of Head Start programs by grantee and delegate agencies. 1996 45 CFR §1304. [Google Scholar]
- 31.Code of Federal Regulations. Child and adult care food program. 1990 7 CFR §226. [Google Scholar]
- 32.Whitaker RC, Gooze RA, Hughes CC, Finkelstein DM. A national survey of obesity prevention practices in Head Start. Arch Pediatr Adolesc Med. 2009;163(12):1144–1150. doi: 10.1001/archpediatrics.2009.209. [DOI] [PubMed] [Google Scholar]
- 33.Jaime PC, Lock K. Do school based food and nutrition policies improve diet and reduce obesity? Prev Med. 2009;48(1):45–53. doi: 10.1016/j.ypmed.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 34.Williams CL, Bollella MC, Strobino BA, Spark A, Nicklas TA, Tolosi LB, et al. “Healthy-start”: outcome of an intervention to promote a heart healthy diet in preschool children. J Am Coll Nutr. 2002;21(1):62–71. doi: 10.1080/07315724.2002.10719195. [DOI] [PubMed] [Google Scholar]
- 35.Endres J, Barter S, Theodora P, Welch P. Soy-enhanced lunch acceptance by preschoolers. J Am Diet Assoc. 2003;103(3):346–351. doi: 10.1053/jada.2003.50046. [DOI] [PubMed] [Google Scholar]
- 36.Gosliner WA, James P, Yancey AK, Ritchie L, Studer N, Crawford PB. Impact of a worksite wellness program on the nutrition and physical activity environment of child care centers. Am J Health Promot. 2010;24(3):186–189. doi: 10.4278/ajhp.08022719. [DOI] [PubMed] [Google Scholar]
- 37.Ward DS, Benjamin SE, Ammerman AS, Ball SC, Neelon BH, Bangdiwala SI. Nutrition and physical activity in child care: results from an environmental intervention. Am J Prev Med. 2008;35(4):352–356. doi: 10.1016/j.amepre.2008.06.030. [DOI] [PubMed] [Google Scholar]
- 38.Davis SM, Sanders SG, FitzGerald CA, Keane PC, Canaca GF, Volker-Rector R. CHILE: an evidence-based preschool intervention for obesity prevention in Head Start. J Sch Health. 2013;83(3):223–229. doi: 10.1111/josh.12018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sussman AL, Davis SM. Integrating formative assessment and participatory research: building healthier communities in the CHILE project. Am J Health Educ. 2010;41(4):244–249. doi: 10.1080/19325037.2010.10599150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cruz TH, Davis SM, FitzGerald CA, Canaca GF, Keane PC. Engagement, recruitment, and retention in a trans-community, randomized controlled trial for the prevention of obesity in American Indian and Hispanic children. J Prim Prev. 2014;35(3):135–149. doi: 10.1007/s10935-014-0340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Birch LL. The role of experience in children’s food acceptance patterns. J Am Diet Assoc. 1987;87(9 suppl):S36–S40. [PubMed] [Google Scholar]
- 42.Birch LL, Marlin DW. I don’t like it; I never tried it: effects of exposure on two-year-old children”s food preferences. Appetite. 1982;3(4):353–360. doi: 10.1016/s0195-6663(82)80053-6. [DOI] [PubMed] [Google Scholar]
- 43.Russell CG, Worsley A. A population-based study of preschoolers’ food neophobia and its associations with food preferences. J Nutr Educ Behav. 2008;40(1):11–19. doi: 10.1016/j.jneb.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 44.Committee on Nutrition, American Academy of Pediatrics. The use and misuse of fruit juice in pediatrics. Pediatrics. 2001;107(5):1210–1213. doi: 10.1542/peds.107.5.1210. [DOI] [PubMed] [Google Scholar]
- 45.Friday JE, Bowman SA. MyPyramid equivalents database for USDA survey food odes, 1994–2002, version 1.0. Beltsville, MD: US Department of Agriculture; 2006. [Accessed September 29, 2015]. http://www.ars.usda.gov/Services/docs.htm?docid=8503. [Google Scholar]
- 46.Snijders TA, Bokser RJ. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Thousand Oaks, CA: Sage Publications; 1999. [Google Scholar]
- 47.National Cancer Institute. [Accessed September 29, 2015];Selected intakes as ratios of energy intake, US population. 2001–04 Available at: http://epi.grants.cancer.gov/diet/usualintakes/energy/
- 48.Story M, Snyder MP, Anliker J, Weber JL, Cunningham-Sabo L, Stone EJ, et al. Changes in the nutrient content of school lunches: results from the Pathways study. Prev Med. 2003;37(6, pt 2):S35–S45. doi: 10.1016/j.ypmed.2003.08.009. [DOI] [PubMed] [Google Scholar]
- 49.Monsivais P, Kirkpatrick S, Johnson DB. More nutritious food is served in child-care homes receiving higher federal food subsidies. J Am Diet Assoc. 2011;111(5):721–726. doi: 10.1016/j.jada.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 50.Monsivais P, Johnson DB. Improving nutrition in home child care: are food costs a barrier? Public Health Nutr. 2012;15(2):370–376. doi: 10.1017/S1368980011002382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Institute of Medicine. Child and Adult Care Food Program:Aligning Dietary Guidance for All. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 52.Oakley CB, Bomba AK, Knight KB, Byrd SH. Evaluation of menus planned in Mississippi child-care centers participating in the Child and Adult Care Food Program. J Am Diet Assoc. 1995;95(7):765–768. doi: 10.1016/S0002-8223(95)00213-8. [DOI] [PubMed] [Google Scholar]
- 53.Fleischhacker S, Cason KL, Achterberg C. “You had peas today?”: a pilot study comparing a Head Start child-care center’s menu with the actual food served. J Am Diet Assoc. 2006;106(2):277–280. doi: 10.1016/j.jada.2005.10.038. [DOI] [PubMed] [Google Scholar]
- 54.Benjamin Neelon SE, Copeland KA, Ball SC, Bradley L, Ward DS. Comparison of menus to actual foods and beverages served in North Carolina child-care centers. J Am Diet Assoc. 2010;110(12):1890–1895. doi: 10.1016/j.jada.2010.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]