Abstract
Higher mortality in Blacks than Whites has been consistently reported in the US, but previous investigations have not accounted for poverty at the individual level. The health of its population is an important part of the capital of a nation. We examined the association between individual level poverty and disability and racial mortality differences in a 5% Medicare beneficiary random sample from 2004 to 2010. Cox regression models examined associations of race with all-cause mortality, adjusted for demographics, comorbidities, disability, neighborhood income, and Medicare “Buy-in” status (a proxy for individual level poverty) in 1,190,510 Black and White beneficiaries between 65 and 99 years old as of January 1, 2014, who had full and primary Medicare Part A and B coverage in 2004, and lived in one of the 50 states or Washington, DC.
Overall, black beneficiaries had higher sex-and-age adjusted mortality than Whites (hazard ratio [HR] 1.18). Controlling for health-related measures and disability reduced the HR for Black beneficiaries to 1.03. Adding “Buy-in” as an individual level covariate lowered the HR for Black beneficiaries to 0.92. Neither of the residential measures added to the predictive model. We conclude that poorer health status, excess disability, and most importantly, greater poverty among Black beneficiaries accounts for racial mortality differences in the aged US Medicare population. Poverty fosters social and health inequalities, including mortality disparities, notwithstanding national health insurance for the US elderly. Controlling for individual level poverty, in contrast to the common use of area level poverty in previous analyses, accounts for the White survival advantage in Medicare beneficiaries, and should be a covariate in analyses of administrative databases.
Keywords: USA, Poverty, Socioeconomic status, Mortality, Race, Neighborhood, Disability, Disparities, Buy-in, Dual-eligible, Medicare, Medicaid, USRDS
Highlights
-
•
Socioeconomic disparities have important consequences for patient outcomes.
-
•
Including poverty in analyses mitigates racial mortality disparities in the elderly.
-
•
Poverty is an essential factor associated with Medicare racial mortality disparities.
Introduction
Black people have higher mortality than Whites in the US (Isaacs and Schroeder, 2004, Sautter et al., 2012). Excess mortality in older Blacks has been attributed to poorer health status, more widespread adverse health behaviors, more limited access to care, and lower socioeconomic status (SES) among Black Americans. These factors explain a substantial proportion of racial mortality differences, but a sizable unexplained residual remains (Isaacs and Schroeder, 2004, Thorpe et al., 2012, Williams et al., 2010). The unexplained portion may be attributed to limitations such as inadequate or imprecise measurement of contributing factors, insufficient adjustment for unmeasured factors, small samples, or unrepresentative populations. Ideally, SES measures should be individual level, but large population databases usually lack such measures (Adler, Bush, & Pantell, 2012). Smaller databases containing individual level SES measures are often not generalizable, and lack power to detect differences from which definitive conclusions may be made (Adler et al., 2012, Isaacs and Schroeder, 2004).
We recently used ecologic variables to assess relationships among health outcomes and income, income inequality, and residential segregation in Black and White end-stage renal disease (ESRD) patients. Black patients who lived in areas characterized by segregation and lower income had higher mortality (Kimmel, Fwu, & Eggers, 2013).
The mortality disadvantage for Blacks in the US elderly population is substantial. The disparity varies with age, decreasing from a mortality disadvantage of 49% in those 65–69, to 12% in those 80–84. The racial mortality disadvantage reverses after age 85. The reason for crossover at 85 is unknown, but the finding is well-documented (Liu and Witten, 1995, Sautter et al., 2012). Therefore, the etiology of Black disadvantage is undoubtedly complex, reflecting many confounding factors.
Poverty is an important factor underlying US racial mortality differences, given the strong link between higher mortality and adverse economic conditions (Isaacs & Schroeder, 2004) and the well-documented differences in poverty rates across racial groups (DeNavas-Walt, Proctor, & Smith, 2013). Poverty and poor health can reinforce each other, a notion increasingly recognized as an impediment to economic advances in both developed and low-income nations (Mirvis, Chang, & Cosby, 2008).
Residential or ecologic characteristics such as neighborhood median household income and racial segregation may also contribute to racial mortality disparities (Kimmel et al., 2013, Nuru-Jeter and LaVeist, 2011). Residence in a socioeconomically disadvantaged community is associated with poorer health and higher mortality (Ludwig et al., 2011, Nuru-Jeter and LaVeist, 2011). Poor neighborhoods can provide unhealthy environments and offer residents little chance to engage in healthy behaviors (Nuru-Jeter & LaVeist, 2011). Residential segregation perpetuates poor housing, unhealthy neighborhood environments (Kramer and Hogue, 2009, Nuru-Jeter and LaVeist, 2011) and limited health care access (Rodriguez et al., 2007).
Typical analytic approaches evaluating SES factors in US studies include linking large databases, such as Medicare enrollment files, with Census level SES measures. Analyses using area level approaches usually show modest associations of SES and outcomes, but are subject to ecological biases (Kimmel et al., 2013, Rodriguez et al., 2007). Relying solely on area-wide poverty or income measures to account for individual variation in health outcomes may result in misleading or inadequate assessment of income effects on health (Hanley & Morgan, 2008). Individual level information regarding income and wealth as socioeconomic indicators is largely missing from US administrative health registries (Isaacs & Schroeder, 2004). Direct individual level income or poverty measures are much preferred for such analyses since even race-specific ecologic analyses may subject the evaluation of certain characteristics, such as income, to misclassification (Hanley & Morgan, 2008).
Medicare data, however, include both individual level disability and poverty measures, not widely used in outcome analyses (Lovald et al., 2013). First, Social Security offers Medicare coverage to those unable to work because of medically determined physical or mental impairment before age 65. This lack of participation in the legal workforce, acknowledged by disability status, in combination with relatively low levels of monetary reimbursement, puts even recipients of disability benefits at economic disadvantage. Compared to elderly beneficiaries, disabled Medicare beneficiaries are much more likely to be of a minority group (Iezzoni, 2006). Disability also is associated with increased mortality (Lubitz & Pine, 1986). Therefore, Medicare disability eligibility is a marker of economic and health disadvantage during beneficiaries’ early lives that may have enduring effects, which could contribute to racial mortality disparities.
Second, Medicare also has a proxy poverty measure. Many Medicare beneficiaries qualify for benefits from Medicaid, a Federal-State program for certain low-income individuals. In addition, Medicare “Buy-in” benefits were created to help low-income Medicare beneficiaries pay Medicare premiums, and in some instances, deductibles and copayments. Medicare Buy-in Programs are administered by States to pay all or part of Medicare health insurance co-pay expenses for eligible low-income Medicare recipients. All Medicare beneficiaries qualifying for either Medicaid or State Buy-in programs meet designated low-income standards, usually no higher than 135% of Federal poverty levels (Eichner and Vladeck, 2005, Ryan and Super, 2003). In 2013, $15,510 annual income was the poverty level for a US family of two (US HHS, 2013). Average income for households headed by someone≥65 years at that time was $53,000. Consequently, anyone receiving a Buy-in subsidy (dual eligibility) had an income less than one-third the average for elderly persons.
In addition to direct SES and disability measures, Medicare beneficiary data are linkable to claims data, permitting calculation of health status based on hospitalizations (Waxman, Greenberg, Ridgely, Kellermann, & Heaton, 2014).
We hypothesized mortality disparities between US Black and White aged persons can be largely accounted for by health status, poverty, and disability, and that these individual level measures are more powerful predictors of mortality than residential characteristics.
Methods
Data resources and study population
We obtained a 5% Medicare beneficiary random sample, using 2004–2010 Denominator files and 2004 Part A Institutional Claims files from Centers for Medicare & Medicaid Services (CMS) in this retrospective cohort study. We identified 1,461,071 Black and White beneficiaries 65–99 years old as of January 1, 2004 (and 66–100 years old at study start on January 1, 2005), who had full Medicare Part A and B coverage in 2004, were not in hospice care, and resided in the 50 States or Washington, DC. Data from 2004 (the 1-year observation period before study start) were used to establish baseline health status. To ensure complete Medicare claims data for baseline health status, we excluded 231,110 beneficiaries enrolled in health maintenance organizations in all or part of 2004.
We assigned two residential measures for each beneficiary, linking individual level data from Medicare files with 2000 Census Bureau data, as previously (Kimmel et al., 2013), using residential ZIP code (for race-specific neighborhood median household income) and county code (for Dissimilarity Index scores to measure residential racial segregation) (Nuru-Jeter & LaVeist, 2011). We excluded 39,451 beneficiaries with unavailable ZIP and county code data. The final study cohort included 1,190,510 beneficiaries (Supplemental Fig. 1).
Baseline characteristics
Demographic factors included race, age (as of January 1, 2005) and gender. Two health-related measures were considered: hospitalizations with Charlson Comorbidity Index (Charlson) scores, and ESRD therapy. Beneficiaries were designated hospitalized if they had one or more Part A institutional inpatient care claims in 2004. Based on diagnoses in the Medicare Part A Institutional Claim files, we used standardized coding algorithms (Quan et al., 2005) to calculate Charlson scores for beneficiaries hospitalized in 2004. Charlson score is a widely-used composite value based on number and seriousness of comorbid medical illnesses that alter mortality risk (Charlson, Pompei, Ales, & MacKenzie, 1987). We treated beneficiaries having no hospitalization as one category and grouped other beneficiaries into another six categories (based on calculated Charlson scores 0, 1 through 4, or ≥5) to represent beneficiaries’ baseline hospitalization and Charlson score. The other baseline health-related measure, ESRD status, was indicated in 2004 Denominator files. The Medicare program covers virtually all elderly US ESRD patients.
Disability before 65 was identified in 2004 Denominator files based on the original reason for Medicare entitlement. “Disabled” status-indicating inability to work for any medically determinable physical or mental impairment before age 65—is determined by the Social Security Administration at the time of disability benefit application (Social Security Administration, 2011). Previous studies show disability before 65 is associated with increased mortality risk after age 65 (Lubitz & Pine, 1986).
We assigned beneficiaries a state Buy-in status (dual eligibility) if enrolled in Medicaid or the state Buy-in program for Medicare Parts A and B for at least 1 month in 2004. (88% of beneficiaries assigned Buy-in status had the full 12 months’ assistance during the year.) Hereafter we refer to Buy-in status as “dual eligibility,” or “poverty,” an individual level administrative marker of poverty.
Two residential measures were used to represent characteristics of each beneficiary’s neighborhood, as previously (Kimmel et al., 2013). First was race-specific neighborhood median household income. Beneficiaries were assigned to annual income categories (<$20,000, $20,000–$29,999, $30,000–$39,999, $40,000–$49,999, $50,000–$59,999, $60,000–$69,999, and ≥$70,000) based on 2000 Census Bureau race and residential ZIP code data. The other residential measure, the Dissimilarity Index, is a county-level variable widely used as a residential racial segregation measure (Kimmel et al., 2013, Kramer and Hogue, 2009, Nuru-Jeter and LaVeist, 2011). We categorized counties into residential segregation quartiles. The first quartile represents counties with the least, and the fourth quartile counties with the most racial residential segregation. We assigned each beneficiary to a quartile based on county residence.
Outcomes
Date of death is included in Medicare Denominator files. Beneficiaries were followed for all-cause death for 6 years, from January 1, 2005 through December 31, 2010.
Statistical analysis
Descriptive statistics depicted baseline characteristics for the study cohort as a whole and by race. We calculated means and standard deviations (SD) for age, median and interquartile neighborhood household income ranges, and percentage distributions for categorical variables. We used t-test for age, Wilcoxon–Mann–Whitney test for income, and chi-square tests for categorical variables to compare distributions between Black and White beneficiaries.
Race-specific all-cause mortality rates were calculated for all beneficiaries and for each 5-year age group (66–70, 71–75, 76–80, 81–85 and ≥86 years). Cox proportional hazards regression models were specified to examine associations of race with all-cause mortality. The “base” model was adjusted for gender and age. Subsequent models were created in step-wise fashion based on prior causal assumptions. The order of the additions was health-related measures, disability, dual eligibility, and ecologic SES measures. Because of the well-known mortality crossover in older Americans (Sautter et al., 2012), we repeated analyses separately for each 5-year age group to assess the findings’ robustness. Secondary analyses examined individual effects of predictor variables on all-cause mortality, by adding each variable to the base model separately.
Proportional hazards models were fit using sandwich estimates for variance calculation to account for potentially unaccounted factors when clustering by county, as previously (Kimmel et al., 2013). Proportional hazards assumptions were examined by graphing log (−log[survival function]) curves. No violation was observed. Statistical significance was defined as p<0.05 using two-tailed tests. Means are reported±SD. Analyses were conducted using SAS version 9.2.
Results
Baseline characteristics
Among 1,190,510 Medicare beneficiaries alive January 1, 2005, 7.9% were Black, 41.1% male, 21.5% were hospitalized in 2004, 0.4% had ESRD, 7.6% received disability benefits before age 65, 10.7% met income definitions qualifying for Medicaid or state Buy-in programs, 13.6% lived in neighborhoods with median household income<$30,000 and 15.4% in areas with average income≥$60,000 (Table 1). 12.1% lived in the least and 43.9% in the most racially segregated areas. Mean age was 76.5±7.3 years.
Table 1.
Baseline characteristics of study cohort, by race.
| Characteristics | All (n=1,190,510) | Black (n=94,541) | White (n=1,095,969) | p-value⁎ |
|---|---|---|---|---|
| Demographic features | ||||
| Black (%) | 7.9 | – | – | |
| Male (%) | 41.1 | 37.3 | 41.4 | <0.001 |
| Age in years (mean±SD) | 76.5±7.3 | 75.7±7.3 | 76.6±7.3 | <0.001 |
| Age group | <0.001 | |||
| 66–70 years (%) | 25.4 | 29.9 | 25.0 | |
| 71–75 years (%) | 24.2 | 25.4 | 24.1 | |
| 76–80 years (%) | 21.4 | 19.8 | 21.6 | |
| 81–85 years (%) | 16.1 | 13.8 | 16.3 | |
| ≥86 years (%) | 12.9 | 11.2 | 13.0 | |
| Health-related measures | ||||
| Hospitalization/Charlson score | <0.001 | |||
| No hospitalization | 78.5 | 75.4 | 78.8 | |
| Charlson score=0 | 6.0 | 5.0 | 6.1 | |
| Charlson score=1 | 6.0 | 6.5 | 5.9 | |
| Charlson score=2 | 4.2 | 5.0 | 4.2 | |
| Charlson score=3 | 2.4 | 3.2 | 2.3 | |
| Charlson score=4 | 1.2 | 1.9 | 1.2 | |
| Charlson score=5 or more | 1.7 | 3.1 | 1.6 | |
| ESRD status (%) | 0.4 | 1.7 | 0.3 | <0.001 |
| Disabilitya (%) | 7.6 | 15.0 | 7.0 | <0.001 |
| State Medicaid/Buy-In Status (%) | 10.7 | 31.9 | 8.9 | <0.001 |
| Residential measures | ||||
| Median household income (median, interquartile range) | $40,881 | $26,371 | $41,773 | <0.001 |
| $33,668–$52,146 | $20,423-$35,523 | $34,936-$53,100 | ||
| Median household income group | <0.001 | |||
| $2500 –<$20,000 (%) | 2.2 | 22.7 | 0.5 | |
| $20,000– <$30,000 (%) | 11.4 | 39.4 | 8.9 | |
| $30,000– <$40,000 (%) | 33.0 | 20.5 | 34.1 | |
| $40,000–<$50,000 (%) | 24.0 | 9.3 | 25.3 | |
| $50,000– <$60,000 (%) | 14.0 | 4.4 | 14.8 | |
| $60,000– <$70,000 (%) | 7.4 | 1.8 | 7.9 | |
| ≥$70,000 (%) | 8.0 | 2.0 | 8.5 | |
| Racial segregationb | <0.001 | |||
| 1st quartile (%) | 12.1 | 11.4 | 12.2 | |
| 2nd quartile (%) | 19.7 | 11.4 | 20.5 | |
| 3rd quartile (%) | 24.2 | 19.4 | 24.6 | |
| 4th quartile (%) | 43.9 | 57.9 | 42.7 |
ESRD: end-stage renal disease.
Note: Values expressed as mean, standard deviation; median, interquartile range; or percent.
T-test for continuous variables, chi-square test for categorical variables, and Wilcoxon–Mann–Whitney test for median comparison.
Based on original eligibility categories of Medicare enrollment.
Quartile definitions for racial segregation: <39.50, 39.50–<49.00, 49.00–<58.50, and ≥58.50.
Significant differences existed between Black and White beneficiaries (Table 1). Black beneficiaries were younger (75.7±7.3 vs. 76.6±7.3 years), more likely female (62.7% vs. 58.6%), more likely hospitalized in 2004 (24.6% vs. 21.2%), and had poorer health (Charlson score≥3, 8.2% vs. 5.1%) (all p<0.001). Black beneficiaries were almost six times more likely to have ESRD (1.7% vs. 0.3%, p<0.001). Black beneficiaries received disability benefits before age 65 more than twice as frequently (15.0% vs. 7.0%), and were more than three times as likely to be in poverty (31.9% vs. 8.9%) (both p<0.001), as assessed by dual eligibility status. Black beneficiaries typically lived in neighborhoods with less than two-thirds the median annual household income of Whites, characterized by higher levels of racial residential segregation.
Model results showed, in addition to expected demographic associations, higher mortality for higher comorbid illness burden (hazard ratio [HR] ranging from 1.16 for Charlson score 0 to 4.81 for Charlson score≥5), ESRD (2.56), prior disability (1.51), and individual level poverty (1.57), adjusting for all listed characteristics in the total population (Table 2). Beneficiaries residing in higher income areas had lower mortality than comparison groups.
Table 2.
Effects of race and contributing factors on all-cause mortality (n=1,190,510).
| Characteristics | Hazard ratio | (95% confidence interval) | p-value |
|---|---|---|---|
| Race | |||
| White | 1.00 | ||
| Black | 0.91 | (0.89–0.93) | <0.001 |
| Sex | |||
| Female | 1.00 | ||
| Male | 1.37 | (1.36–1.39) | <0.001 |
| Age | |||
| 66–70 years | 1.00 | ||
| 71–75 years | 1.53 | (1.51–1.55) | <0.001 |
| 76–80 years | 2.48 | (2.45–2.51) | <0.001 |
| 81–85 years | 4.10 | (4.04–4.15) | <0.001 |
| ≥86 years | 8.26 | (8.14–8.38) | <0.001 |
| Hospitalization/Charlson score | |||
| No hospitalization | 1.00 | ||
| Charlson score=0 | 1.16 | (1.15–1.18) | <0.001 |
| Charlson score=1 | 1.69 | (1.66–1.71) | <0.001 |
| Charlson score=2 | 2.24 | (2.21–2.27) | <0.001 |
| Charlson score=3 | 2.79 | (2.75–2.84) | <0.001 |
| Charlson score=4 | 3.36 | (3.28–3.44) | <0.001 |
| Charlson score=5 or more | 4.81 | (4.71–4.92) | <0.001 |
| End stage renal disease | |||
| No | 1.00 | ||
| Yes | 2.56 | (2.46–2.66) | <0.001 |
| Disabilitya | |||
| No | 1.00 | ||
| Yes | 1.51 | (1.49–1.53) | <0.001 |
| State Medicaid/Buy-In status | |||
| No | 1.00 | ||
| Yes | 1.57 | (1.53–1.61) | <0.001 |
| Median household income group | |||
| $ 2500–<$20,000 | 0.96 | (0.93–0.99) | 0.01 |
| $20,000–<$30,000 | 1.01 | (0.99–1.02) | 0.53 |
| $30,000–<$40,000 | 1.00 | ||
| $40,000–<$50,000 | 0.99 | (0.98–1.00) | 0.01 |
| $50,000–<$60,000 | 0.96 | (0.95–0.97) | <0.001 |
| $60,000–<$70,000 | 0.96 | (0.94–0.97) | <0.001 |
| ≥$70,000 | 0.90 | (0.88–0.92) | <0.001 |
| Racial segregationb | |||
| 1st quartile | 1.00 | ||
| 2nd quartile | 0.98 | (0.97–1.00) | 0.07 |
| 3rd quartile | 1.00 | (0.98–1.02) | 0.98 |
| 4th quartile | 0.99 | (0.97–1.01) | 0.22 |
Note: Results from Cox regression model after adjusting for all listed characteristics.
Based on original eligibility categories of Medicare enrollment.
Quartile definitions for racial segregation: <39.50, 39.50–<49.00, 49.00–<58.50, and ≥58.50.
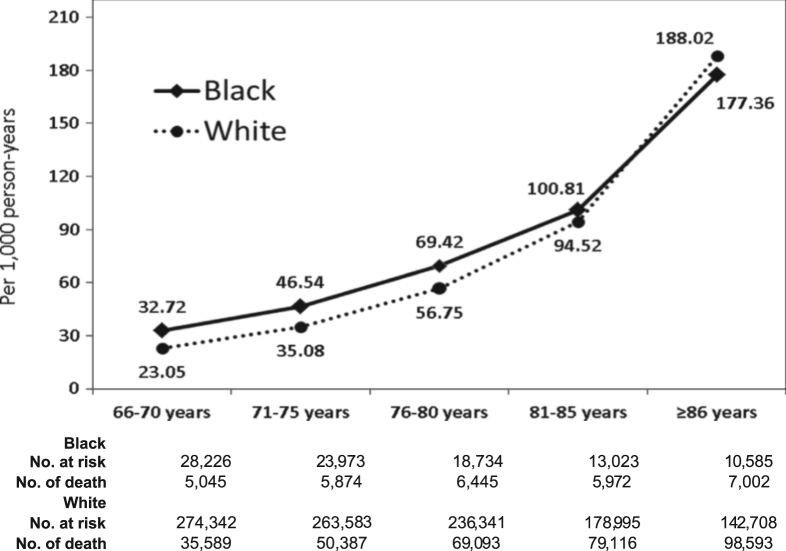
Mortality rates
During the 6-year study period, 363,116 deaths occurred. Overall mortality rate was 60.2 deaths/1000 person-years. Mortality rate was 64.3/1,000 person-years (95% CI: 63.6–65.0) in Black and 59.9/1000 person-years (59.7–60.1) in White beneficiaries. Fig. 1 shows sample size, number of deaths, and mortality rates by race by age group. As expected, mortality crossover occurred for beneficiaries age≥86, consistent with previous reports.
Fig. 1.
Mortality rate (per 1000 person-years), by race and age group.
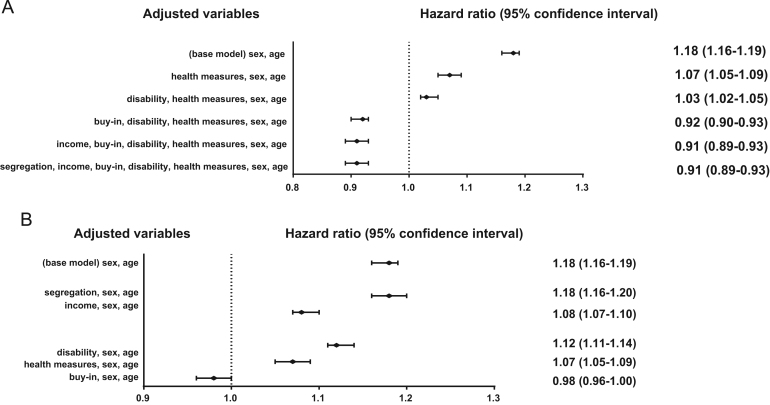
Role of contributing factors
Fig. 2 (Panel A) shows results of sequential Cox models for the overall study cohort, indicating the incremental role of each set of factors associated with racial differences in all-cause mortality. In the base model (adjusting for age and gender only), Blacks had 18% higher mortality than Whites (HR: 1.18; 95% CI: 1.16–1.19). After adjustment for health-related measures, HR for Blacks was attenuated substantially (HR: 1.07; 95% CI: 1.05–1.09). Adding disability to the model reduced the HR for race from 1.07 to 1.03 (95% CI: 1.02–1.05). Further addition of poverty status reduced the HR for race from 1.03 to 0.92 (95% CI: 0.90–0.93). Subsequent adjustment for additional ecologic residential measures did not appreciably change the HR for race.
Fig. 2.
Hazard ratios (95% confidence interval) of all-cause mortality for Blacks from multivariate-adjusted Cox regression models (n=1,190,510). Note: Health measures include hospitalization/Charlson score and end-stage renal disease.
Supplemental Fig. 2 shows the results of mortality analyses by age. The full model accounts entirely for the Black mortality disparity for the youngest three age groups, reverses the HR for persons ages 81–85, and shows increased survival for Blacks≥86 years.
Secondary analyses examined the effects of these additional factors on mortality individually. Fig. 2 (Panel B) shows effects of adjustment for each factor. Among ecological variables, adjustment for segregation had negligible effects. Controlling for median household income reduced the HR for Black beneficiaries from 1.18 to 1.08. Adjustment for prior disability and health measures both reduced the HR, to 1.12 and 1.07, respectively. However, accounting for individual level poverty alone – without additional covariates other than age and gender – reduced the HR for race from 1.18 to 0.98. After adjustment for this poverty measure, no meaningful and statistically significant mortality differences between comparable Black and White beneficiaries remain.
Discussion
Poverty is a critical problem, associated with impaired health and increased mortality, both US and worldwide (Isaacs & Schroeder, 2004). Poverty, ill health and mortality combine to form a vicious cycle harming a substantial proportion of the population. Currently intense debate exists regarding best approaches to alleviating US and worldwide poverty and its deleterious effects on health.
Previous studies demonstrated elderly and younger US Blacks consistently have higher mortality rates than Whites. Reasons suggested to explain this disparity include differences in health status (Hernandez & Pressler, 2014), access to care (Schoenbaum, Schoen, Nicholson, & Cantor, 2011), insurance coverage (Van Der Wees, Zaslavsky, & Ayanian, 2013), and biologic characteristics including prevalence of acute and chronic illnesses, as well as genetic variation (Rosenberg et al., 2010). All these factors may be exacerbated by poverty.
The higher mortality risk among Black Medicare beneficiaries was attenuated by accounting for several variables. Black beneficiaries had demonstrably worse health status, measured by Charlson score and ESRD prevalence. Adjusting for these factors together reduced the racial death rate disparity considerably. Black beneficiaries also had twice the rate of prior disability, accounting for further disparity reduction. However, it was poverty, measured by the State Buy-in indicator for the poor and near-poor, that had the greatest impact on accounting for the disparity between the two groups. The addition of this individual level variable essentially equalized the groups’ adjusted mortality rate. Secondary analyses showed inclusion of individual level poverty alone could account for the age-gender adjusted mortality difference between Black and White aged Americans (Fig. 2, Panel B).
Buy-in in these analyses plays at least two roles. First, it functions as a marker of poverty. Buy-in also describes a benefit, associated with health care access, which may decrease illness and mortality, indicating the marker’s role in partially mitigating mortality disparities.
The “adjusted” mortality advantage for Blacks does not mean elderly Blacks are better off than elderly Whites (Isaacs & Schroeder, 2004). Rather, it emphasizes the tremendous effect of the racial differential in poverty on health disparities. Elderly Blacks are three times as likely as elderly Whites to live in poverty, measured by Buy-in. These findings do however suggest the higher age–gender adjusted mortality rate among Blacks is explained by factors known to affect health, such as disability, comorbid illness, access to advanced care, employment, and primarily the notable extent of poverty in this population (Isaacs & Schroeder, 2004).
Study limitations include retrospective analysis and dependence on administrative data. Therefore the findings reflect associations and not necessarily causation. Neighborhood income and residential segregation data which are at ZIP code or county level, reflect the characteristics of an area, meaning these variables’ associations with mortality may not hold in individual level data. Medicaid or State “Buy-in” status, while an individual level variable, measures beneficiaries’ poverty status imperfectly. For example, the Buy-in variable misses some poor Medicare beneficiaries not enrolled in the program. In addition, the Buy-in variable is binary, and therefore subject to misclassification, as is disability history. However, levels of inference are at the individual level for ascertainment of poverty, which is a unique finding compared to prior publications. In contrast, ascertainment of area-level income is made at the ZIP code level, and inference is ecological for this factor. Medicare files do not indicate cause of disability or death, nor how long disability existed. Charlson scores are based on ICD-9 codes from billing records, and may not fully represent health status.
A key study strength, however, is use of the Medicare 5% sample, a very large, excellent representative sample of the aged US population. Although this study reports findings from a large sample of the US Medicare population, the findings only apply directly to the Medicare population. Differences between the Medicare and non-Medicare population have been reported previously through CMS (Medicare.gov), and are available in customizable detail through the Henry J. Kaiser Foundation (kff.org). In summary, Medicare beneficiaries, compared to members of the US population who do not receive Medicare, are considerably older (primarily due to eligibility at age 65, with a substantially smaller minority of patients eligible for Medicare before that age due to disability), of lower income, and black. Thus, our findings may be less applicable to the working age, non-disabled population. Mortality follow-up in this database is virtually complete, with many administrative and legal elements in place to ascertain death dates.
Poverty, as represented by Buy-in or dual eligibility, clearly explains much of the disparity in mortality rates between Black and White people in Medicare, which represents the universe of US aged persons with health insurance. Reducing poverty, or alleviating its adverse effects, is a daunting challenge. Methods to alleviate poverty include policy approaches such as improving neighborhood characteristics, increasing health care coverage through Medicaid and the Affordable Care Act, supplementing diet and income through the food stamp program, and improving income of the poor and near-poor through the earned income tax credit. Other interventions include consideration of innovative approaches such as housing initiatives and various health interventions (Doran et al., 2013, Ludwig et al., 2011). However, poverty will likely remain a vexing problem, especially in light of increasing income disparities (Granados, 2013, Isaacs and Schroeder, 2004).
We conclude poverty is one of the most important factors associated with racial disparities in all-cause mortality in the US Medicare population. As with all observational studies, we cannot exclude a role for unmeasured cofounders. Mortality consequences exist associated with social and health inequalities due to poverty. Inclusion of individual level poverty as an analytic factor mitigates the Black and White racial mortality disparity in the elderly US population. This factor should be a key individual level element in health outcome and mortality analyses. Reducing poverty would likely result in improved life expectancy for Black and White elderly Medicare beneficiaries, and could serve to diminish health care disparities.
Author contributions
All authors contributed to the study concept and design, had full access to all of the data in the study, and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors were involved in analysis and interpretation of data. P.L.K., P.W.E., and C.W.F. drafted the manuscript, and all authors contributed to the critical revision of the manuscript for important intellectual content.
Funding
C.W.F. is a contractor of the US National Institute of Diabetes, Digestive and Kidney Diseases, National Institute of Health (HHSN 276201200161U). The funding source had no role in study design, data interpretation, or manuscript preparation.
Conflict of interests
All authors declare: no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Disclaimer
The views expressed do not necessarily represent the views of the Department of Health and Human Services, the National Institutes of Health, the National Institute of Diabetes, Digestive and Kidney Diseases, or the United States Government. The data reported here have been supplied by the United States Renal Data System (USRDS). The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as official policy or interpretation of the US government.
Acknowledgments
None.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2016.02.003.
Contributor Information
Paul L. Kimmel, Email: kimmelp@extra.niddk.nih.gov.
Chyng-Wen Fwu, Email: cfwu@s-3.com.
Kevin C. Abbott, Email: kevin.abbott@nih.gov.
Jonathan Ratner, Email: JonRatner@westat.com.
Appendix A. Supplementary material
Supplementary material
References
- Adler N., Bush N.R., Pantell M.S. Rigor, vigor, and the study of health disparities. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(Suppl. 2):17154–17159. doi: 10.1073/pnas.1121399109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson M.E., Pompei P., Ales K.L., MacKenzie C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C., Proctor B.D., Smith J.C. U.S. Government Printing Office; Washington, DC: 2013. Income, poverty, and health insurance coverage in the United States: 2012. [Google Scholar]
- Doran K.M., Misa E.J., Shah N.R. Housing as health care—New York׳s boundary-crossing experiment. New England Journal of Medicine. 2013;369:2374–2377. doi: 10.1056/NEJMp1310121. [DOI] [PubMed] [Google Scholar]
- Eichner J., Vladeck B.C. Medicare as a catalyst for reducing health disparities. Health Affairs (Millwood) 2005;24:365–375. doi: 10.1377/hlthaff.24.2.365. [DOI] [PubMed] [Google Scholar]
- Granados J.A. Health at advanced age: Social inequality and other factors potentially impacting longevity in nine high-income countries. Maturitas. 2013;74:137–147. doi: 10.1016/j.maturitas.2012.11.013. [DOI] [PubMed] [Google Scholar]
- Hanley G.E., Morgan S. On the validity of area-based income measures to proxy household income. BMC Health Services Research. 2008;8:79. doi: 10.1186/1472-6963-8-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez D.C., Pressler E. Accumulation of childhood poverty on young adult overweight or obese status: Race/ethnicity and gender disparities. Journal of Epidemiology and Community Health. 2014;68:478–484. doi: 10.1136/jech-2013-203062. [DOI] [PubMed] [Google Scholar]
- US HHS. (2013). https://aspe.hhs.gov/2013-poverty-guidelines
- Iezzoni L.I. Quality of care for Medicare beneficiaries with disabilities under the age of 65 years. Expert Review Pharmacoeconomics Outcomes Research. 2006;6:261–273. doi: 10.1586/14737167.6.3.261. [DOI] [PubMed] [Google Scholar]
- Isaacs S.L., Schroeder S.A. Class—The ignored determinant of the nation׳s health. New England Journal of Medicine. 2004;351:1137–1142. doi: 10.1056/NEJMsb040329. [DOI] [PubMed] [Google Scholar]
- Kimmel P.L., Fwu C.W., Eggers P.W. Segregation, income disparities, and survival in hemodialysis patients. Journal of the American Society of Nephrology. 2013;24:293–301. doi: 10.1681/ASN.2012070659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramer M.R., Hogue C.R. Is segregation bad for your health? Epidemiologic Reviews. 2009;31:178–194. doi: 10.1093/epirev/mxp001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Witten M. A biologically based explanation for mortality crossover in human populations. Gerontologist. 1995;35:609–615. doi: 10.1093/geront/35.5.609. [DOI] [PubMed] [Google Scholar]
- Lovald S.T., Ong K.L., Lau E.C., Schmier J.K., Bozic K.J., Kurtz S.M. Mortality, cost, and health outcomes of total knee arthroplasty in Medicare patients. Journal of Arthroplasty. 2013;28:449–454. doi: 10.1016/j.arth.2012.06.036. [DOI] [PubMed] [Google Scholar]
- Lubitz J., Pine P. Health care use by Medicare׳s disabled enrollees. Health Care Financing Reviews. 1986;7:19–31. [PMC free article] [PubMed] [Google Scholar]
- Ludwig J., Sanbonmatsu L., Gennetian L., Adam E., Duncan G.J., Katz L.F., Kessler R.C., Kling J.R., Lindau S.T., Whitaker R.C., McDade T.W. Neighborhoods, obesity, and diabetes—A randomized social experiment. New England Journal of Medicine. 2011;365:1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mirvis D.M., Chang C.F., Cosby A. Health as an economic engine: Evidence for the importance of health in economic development. Journal of Health and Services Administration. 2008;31:30–57. [PubMed] [Google Scholar]
- Nuru-Jeter A.M., LaVeist T.A. Racial segregation, income inequality, and mortality in US metropolitan areas. Journal of Urban Health-Bulletin of the New York Academy of Medicine. 2011;88:270–282. doi: 10.1007/s11524-010-9524-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quan H., Sundararajan V., Halfon P., Fong A., Burnand B., Luthi J.C., Saunders L.D., Beck C.A., Feasby T.E., Ghali W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- Rodriguez R.A., Sen S., Mehta K., Moody-Ayers S., Bacchetti P., O׳Hare A.M. Geography matters: Relationships among urban residential segregation, dialysis facilities, and patient outcomes. Annals of Internal Medicine. 2007;146:493–501. doi: 10.7326/0003-4819-146-7-200704030-00005. [DOI] [PubMed] [Google Scholar]
- Rosenberg N.A., Huang L., Jewett E.M., Szpiech Z.A., Jankovic I., Boehnke M. Genome-wide association studies in diverse populations. Nature Reviews Genetics. 2010;11:356–366. doi: 10.1038/nrg2760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan J., Super N. Dually eligible for medicare and medicaid: Two for one or double jeopardy? Issue Briefing National Health Policy Forum. 2003:1–24. [PubMed] [Google Scholar]
- Sautter J.M., Thomas P.A., Dupre M.E., George L.K. Socioeconomic status and the Black–White mortality crossover. American Journal of Public Health. 2012;102:1566–1571. doi: 10.2105/AJPH.2011.300518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenbaum S.C., Schoen C., Nicholson J.L., Cantor J.C. Mortality amenable to health care in the United States: The roles of demographics and health systems performance. Journal of Public Health Policy. 2011;32:407–429. doi: 10.1057/jphp.2011.42. [DOI] [PubMed] [Google Scholar]
- Social Security Administration (2011). Annual statistical report on the social security disability insurance program. Washington, DC.
- Thorpe R.J., Jr., Koster A., Bosma H., Harris T.B., Simonsick E.M., van Eijk J.T., Kempen G.I., Newman A.B., Satterfield S., Rubin S.M., Kritchevsky S.B. Racial differences in mortality in older adults: Factors beyond socioeconomic status. Annals of Behavioral Medicine. 2012;43:29–38. doi: 10.1007/s12160-011-9335-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Wees P.J., Zaslavsky A.M., Ayanian J.Z. Improvements in health status after Massachusetts health care reform. Milbank Quarterly. 2013;91:663–689. doi: 10.1111/1468-0009.12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waxman D.A., Greenberg M.D., Ridgely M.S., Kellermann A.L., Heaton P. The effect of malpractice reform on emergency department care. New England Journal of Medicine. 2014;371:1518–1525. doi: 10.1056/NEJMsa1313308. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A., Leavell J., Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Annals of the New York Academy of Sciences. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material