Abstract
Context:
The first step to identifying factors that increase the risk of recurrent ankle sprains is to identify impairments after a first sprain and compare performance with individuals who have never sustained a sprain. Few researchers have restricted recruitment to a homogeneous group of patients with first sprains, thereby introducing the potential for confounding.
Objective:
To identify impairments that differ in participants with a recent index lateral ankle sprain versus participants with no history of ankle sprain.
Design:
Cross-sectional study.
Patients or Other Participants:
We recruited a sample of convenience from May 2010 to April 2013 that included 70 volunteers (age = 27.4 ± 8.3 years, height = 168.7 ± 9.5 cm, mass = 65.0 ± 12.5 kg) serving as controls and 30 volunteers (age = 31.1 ± 13.3 years, height = 168.3 ± 9.1 cm, mass = 67.3 ± 13.7 kg) with index ankle sprains.
Main Outcome Measure(s):
We collected demographic and physical performance variables, including ankle-joint range of motion, balance (time to balance after perturbation, Star Excursion Balance Test, foot lifts during single-legged stance, demi-pointe balance test), proprioception, motor planning, inversion-eversion peak power, and timed stair tests. Discriminant analysis was conducted to determine the relationship between explanatory variables and sprain status. Sequential discriminant analysis was performed to identify the most relevant variables that explained the greatest variance.
Results:
The average time since the sprain was 3.5 ± 1.5 months. The model, including all variables, correctly predicted a sprain status of 77% (n = 23) of the sprain group and 80% (n = 56) of the control group and explained 40% of the variance between groups (
 = 42.16, P = .03). Backward stepwise discriminant analysis revealed associations between sprain status and only 2 tests: Star Excursion Balance Test in the anterior direction and foot lifts during single-legged stance (
= 42.16, P = .03). Backward stepwise discriminant analysis revealed associations between sprain status and only 2 tests: Star Excursion Balance Test in the anterior direction and foot lifts during single-legged stance (
 = 15.2, P = .001). These 2 tests explained 15% of the between-groups variance and correctly predicted group membership of 63% (n = 19) of the sprain group and 69% (n = 48) of the control group.
= 15.2, P = .001). These 2 tests explained 15% of the between-groups variance and correctly predicted group membership of 63% (n = 19) of the sprain group and 69% (n = 48) of the control group.
Conclusions:
Balance impairments were associated with a recent first ankle sprain, but proprioception, motor control, power, and function were not.
Key Words: index inversion ankle sprain, proprioception, inversion-eversion peak power
Key Points
The Star Excursion Balance Test in the anterior direction and the number of foot lifts during single-legged stance most strongly discriminated between participants with index ankle sprains and control participants. These deficits should be targeted in treatments.
Decreased range of dorsiflexion may contribute to impairments in balance and postural control.
The combination of measures of balance, proprioception, motor control, and function predicted ankle-sprain status in most participants.
Although a noncatastrophic injury, ankle sprain has a high incidence and a consequent high prevalence of persisting problems that lead to a high burden of chronic health issues in the community. Recent estimates have indicated that presentation of ankle sprains to emergency departments in the United States is 2.15 per 1000 people per year, resulting in a cumulative health care cost of $4.5 billion per annum after adjusting for inflation.1,2 The incidence of ankle sprain is much higher in military settings (58.4 sprains per 1000 people per year)3 and athletic populations (eg, 1000.0 sprains per 1000 people per year for field hockey and 233.4 sprains per 1000 people per year for rugby).4
Ankle sprains are commonly considered benign injuries that resolve quickly.5 However, lifestyle-limiting impairments and recurrent sprains after the index acute sprain are highly prevalent.6 The term index acute sprain refers to the first or initial ankle sprain that was associated with inflammatory symptoms (eg, pain or swelling) and caused at least 1 interrupted day of desired physical activity.7 Researchers8 have suggested that the development of proprioceptive deficits, decreased range of motion (ROM), balance impairments, or muscle weakness after an index ankle sprain is likely to cause ongoing impairments and increase the risk of recurrent sprains. To evaluate this model, many investigators have studied the association between an acute ankle sprain and physical, neuromuscular, or functional impairments. Impairments that have been studied after an acute ankle sprain include balance, motor planning and motor control,9,10 strength or power,11–13 ankle-joint kinematics,14 and proprioception.15,16 Findings of these studies, however, have been inconsistent. Genthon et al9 observed postural-stabilization asymmetry during bipedal stance, but Akbari et al10 reported contrasting results, finding no postural-control asymmetries after an acute ankle sprain. Researchers13,17 have also reported contrasting findings of postural-control impairments during single-legged balance after an acute ankle sprain. Furthermore, Leanderson et al15 and Cornwall and Murrell16 noted increased postural sway after an acute ankle sprain and reported their findings as impaired proprioception at the ankle joint. However, Ledin et al18 showed that postural sway is not an accurate measure of proprioception. When investigating inversion-eversion strength after an acute ankle sprain, Leanderson et al13 found a reduction in eversion strength in the injured ankle, but Holme et al11 did not.
In addition to inconsistent findings, drawing a conclusion from these studies is particularly difficult due to a methodologic limitation. Most researchers have investigated the association between an acute ankle sprain and different impairments in participants with 1 or more ankle sprains. Participants with recent index ankle sprains and no history of previous injuries have been tested in only 2 studies.12,13 Therefore, given the different characteristics of participants, the changes or impairments associated with an index ankle sprain that may increase the risk of recurrent sprains are not understood.
To identify impairments evident after an index ankle sprain that distinguishes this group from individuals who have never sprained their ankles, investigators should recruit participants only after their index ankle sprains. By establishing the association between neuromuscular, physical, or functional deficits and an index ankle sprain, these deficits can be investigated as putative risk factors for recurrent sprain in a prospective study. Therefore, the purpose of our study was to identify deficits in test variables among participants with recent index lateral ankle sprains compared with control participants with no history of ankle sprain. The test variables were postural control, proprioception, inversion-eversion peak power, motor planning and control, and functional performance. Based on previously proposed models,8 we hypothesized that the results of these tests would discriminate sprain from nonsprain status.
METHODS
Study Design
This cross-sectional observational study was the first phase of a prospective study in which participants were followed for 12 months to determine whether the impairments after an index ankle sprain can predict the chance of recurrent sprains.
Participants
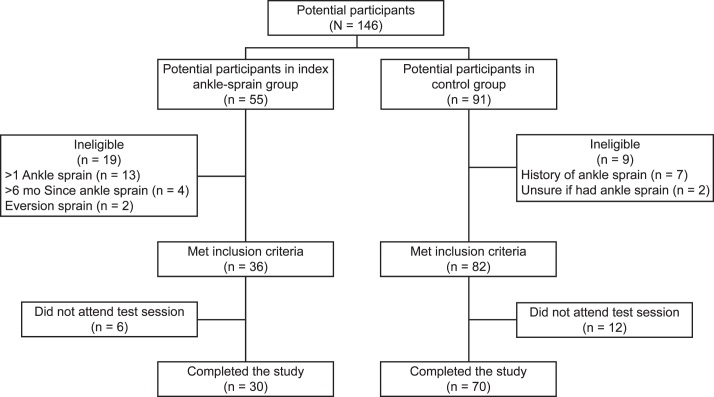
A sample of convenience was recruited by advertising on The University of Sydney bulletin boards and Web-based bulletins. From May 2010 to April 2013, 146 potential recruits contacted the primary investigator (F.P.) to participate in the study: 55 for the index ankle-sprain group and 91 for the control group. After primary screening, 36 participants were eligible for the index ankle-sprain group; 82 participants, for the control group. Eighteen participants did not attend the test session due to travel time or length of the test session (Figure). Therefore, 100 participants (70 in the control group and 30 in the index ankle-sprain group) from 18 to 61 years of age completed the study (Table 1).
Figure. .
Flow chart of participants.
Table 1. .
Demographic and Physical Characteristics of Participants
| Characteristic |
Group |
P Value |
|
| Control (n = 70) |
Index Ankle Sprain (n = 30) |
||
| Sex (No.) | |||
| Male | 24 | 17 | .50 |
| Female | 46 | 13 | |
| Age, y (mean ± SD) | 27.4 ± 8.3 | 31.1 ± 13.3 | .09 |
| Height, cm (mean ± SD) | 168.7 ± 9.5 | 168.3 ± 9.1 | .66 |
| Mass, kg (mean ± SD) | 65.0 ± 12.5 | 67.3 ± 13.7 | .35 |
| Body mass index (mean ± SD) | 22.7 ± 2.9 | 23.6 ± 3.7 | .20 |
| International Physical Activity Questionnaire (No.) | |||
| Low physical activity level | 19 | 9 | .85 |
| Moderate physical activity level | 30 | 11 | |
| Vigorous activity level | 21 | 10 | |
| Foot posture index (mean ± SD) | 4.7 ± 2.7 | 4.2 ± 2.5 | .99 |
| Ligamentous laxitya (No.) | |||
| 0 | 4 | 4 | .09 |
| 1 | 41 | 11 | |
| 2 | 25 | 14 | |
| 3 | 0 | 1 | |
| Cumberland Ankle Instability Tool (mean ± SD) | 28.6 ± 2.2 | 24.0 ± 7.4 | .01b |
Ligamentous laxity scores: 0 = stiff, 1 = normal, 2 = moderately lax, 3 = severely lax.
Indicates difference (P < .05).
Participants were included in the control group (n = 70) if they reported no history of ankle sprain. Participants were included in the index ankle-sprain group (n = 30) if they had experienced a single lateral (inversion) ankle sprain for the first time within the 6 months before the study that required protected weight bearing or immobilization for at least 1 day.7 Exclusion criteria for both groups were history of sprain of the contralateral ankle; history of multiple ankle sprains; eversion ankle sprain; sprain within the 3 weeks before the study; any knee-joint or hip-joint injury; and any neurologic, vestibular, or musculoskeletal disorder that could confound test results. Furthermore, participants were excluded from the index ankle-sprain group if they had pain or any residual symptoms from the sprain that could confound test performance. All participants provided written informed consent, and the study was approved by the Human Research Ethics Committee at the University of Sydney.
Procedures
All assessments were performed in 1 session by the same assessor (F.P.), who was not blinded to the participant's group. Participants completed the Cumberland Ankle Instability Tool (CAIT) and International Physical Activity questionnaires. The CAIT was used to identify and grade perceived instability at the ankle joint.19,20 Scores range from 0 to 30, with scores from 28 to 30 representing stable ankles and scores equal to or less than 27 representing increasingly severe ankle instability.19 We used the International Physical Activity Questionnaire to assess the level of habitual physical activity.21
Selected demographic, physical, neuromuscular, and functional variables were measured. Demographic and physical measures included age, height, mass, lower limb dominance, foot posture index,22 ankle-joint laxity (assessed using the modified anterior drawer test),23 passive inversion and eversion ROM, and dorsiflexion ROM. Passive ankle inversion and eversion ROM were measured while participants were seated with their thighs supported and the shank hanging over the edge of the bed. Range was measured in degrees using a small goniometer (Baseline Goniometre 8; NexGen Ergonomics Inc, Quebec, Canada) placed on the dorsal surface of the foot.24 Passive dorsiflexion ROM was measured using the weight-bearing–lunge test.25
The neuromuscular and functional variables included balance, proprioception, motor planning, limb laterality recognition, inversion and eversion peak power, and function (Table 2) and were measured as detailed in this section. The tests were performed on a randomly chosen side of the control group and the injured side of the index ankle-sprain group. The test ankle of the control group and the order of test performance were randomized using a Web-based randomization program (Research Randomizer version 3.0; Geoffrey C. Urbaniak and Scott Plous, http://www.randomizer.org).
Table 2. .
Description of Tests and Variables Measured
| Test |
Variable |
| Modified ankle-joint anterior drawer test | Anteroposterior ankle-joint ligamentous laxity |
| 0 = Stiff | |
| 1 = Normal | |
| 2 = Moderately lax | |
| 3 = Severely lax | |
| Goniometry | Inversion-eversion range of motion (°) |
| Weight-bearing lunge test | Dorsiflexion range of motion (cm) |
| Cumberland Ankle Instability Tool | Perceived ankle instability |
| 28–30 = stable | |
| ≤27 = unstable | |
| International Physical Activity Questionnaire | Level of physical activity |
| 1 = Low activity level | |
| 2 = Moderate activity level | |
| 3 = High activity level | |
| Response to inversion perturbation | Time to recovery from an inversion perturbation (s) |
| Single-legged stance with eyes closed | No. of foot lifts |
| Star Excursion Balance Test | Distance reached in each direction (cm) |
| Anterior reach/leg length | |
| Posterolateral reach/leg length | |
| Posteromedial reach/leg length | |
| Demi-pointe balance test | The ability to keep balance in demi-pointe position for 5 s (fail or pass) |
| Joint position sense test | Average angular error (°) to match target angles of 5° inversion, maximal inversion −5°, maximal eversion −5° |
| Movement detection sense test | Percentage of correctly recognized inversion or eversion movements imposed at 0.1°/s, 0.5°/s, and 2.5°/s |
| Inversion and eversion peak power | Peak power/body weight [(N·m/s)/kg] at velocities of 30°/s, 60°/s, and 120°/s |
| Choice stepping reaction time test | Average time taken to step on a randomly illuminated footplate with the tested side as fast as possible (s) |
| Limb laterality recognition task | No. of correct left or right recognitions of the foot pictures |
| Average time to recognize the laterality of randomly shown foot pictures on the screen (s) | |
| Timed up-and-down stair test | Time to ascend and descend a flight of 10 stairs (s) |
Balance-Related Activities
Given that performance in different balance tests is weakly correlated,26 we tested both dynamic and static balance using 2 tests for each. We assessed dynamic balance using the response to an inversion perturbation23 and the Star Excursion Balance Test (SEBT)27 and evaluated static balance using the number of foot lifts during single-legged stance with eyes closed28 and demi-pointe balance.28
Response to Perturbation
To assess response to perturbation, we used 3SPACE Fastrak (Polhemus Inc, Colchester, VT). The 3SPACE Fastrak is an electromagnetic motion-tracking system that accurately computes the position and orientation of a sensor relative to a source by using the principle of low-frequency magnetic-field technology. Using this system, we measured the magnitude of mediolateral oscillation at the ankle for 10 seconds during single-legged stance. This measure was considered the baseline measurement. Next, mediolateral oscillation was measured in response to a sudden 15° inversion perturbation of the platform.23 Time to return to baseline oscillation after the perturbation was recorded for a maximum of 10 seconds.23 Participants performed 3 practice trials for familiarization and then 3 trials. A trial was considered a failure if the participant touched down with the contralateral foot or held the bar in front for balance. Participants were allowed 3 attempts. For anyone who failed all 3 attempts, recovery time was imputed as 15 seconds. For those who did not fail but could not return to their baseline balance, the recovery time was imputed as 12 seconds. The best attempt (fastest return to baseline) was analyzed.
Star Excursion Balance Test
We instructed the participants to place their hands on their hips and balance on the test limb while using the other foot to reach as far as they could in 3 directions (anterior, posterolateral, posteromedial).29 After 3 practice trials in each direction, they performed 3 trials in each direction. We instructed them to repeat the test if they lost balance at any point during the test, including if the weight-bearing foot lost contact, they touched down with the nonweight-bearing foot, changed hand positions, or put weight on the test limb while reaching on the tape. The longest distance reached was normalized by limb length for analysis.30
Foot Lifts During Single-Legged Stance With Eyes Closed
Participants were instructed to stand on 1 foot; keep the upper extremities extended by their sides, and when they felt steady, close their eyes and control their balance for 30 seconds. The number of times any part of the foot lost contact with the ground during single-legged stance and the number of touch downs with the nonweight-bearing foot were counted and considered the final score.28 Participants failed the test if they opened their eyes or took a step to avoid falling. They performed the task 3 times, and the best score was recorded for analysis.
Demi-Pointe Balance Test
Participants were required to stand on the ball of the test foot (demi-pointe) for 5 seconds. They held their upper extremities straight in front to assist with balance. We considered the test a failure if they lost balance (ie, touched down with the other foot or held the bar in front of them for balance). The outcome was dichotomous: pass or fail.28
Proprioception
Movement detection and joint position sense in the inversion-eversion plane were tested as measures of proprioception. Participants were seated with the knee comfortably flexed (approximately 60°) and the hip in the middle of its abduction-adduction range and in neutral rotation. The test foot was placed on a custom-made footplate with the ankle in the midrange of inversion-eversion and dorsiflexion-plantar flexion. The axis of rotation of the ankle was aligned with the axis of rotation of the footplate.31 Visual and auditory clues were eliminated using blindfolds and earmuffs.
Movement Detection
Movement-detection acuity was tested at 3 velocities, 0.1°/s, 0.5°/s, and 2.5°/s, in random order.31 The end range for each velocity was based on the threshold of movement detection (ie, 5° for 0.1°/s, 4° for 0.5°/s, and 2° for 2.5°/s). A random mix of 10 inversion and 10 eversion movements was imposed on the test ankle using a Servomotor (Gearing and Watson Electronics, Hailsham, East Sussex, United Kingdom) attached to the side of the footplate. The servomotor is a rotatory actuator that allows for precise control of angular position, velocity, and acceleration via a suitable motor coupled to a sensor for position feedback.
Participants held each movement for 3 seconds before returning to the initial position and were required to report the direction of any perceived movement as soon as they were certain it had occurred. We accepted responses during the movement-and-hold period and measured the score as a percentage of correct responses for each velocity.32
Joint Position Sense
The ability to match 3 target angles (5° less than maximal active inversion, 5° of active inversion, and 5° less than maximal active eversion) was tested. Maximal active inversion and eversion ROM were measured with the foot placed on the footplate. Participants moved the test foot to maximal inversion and eversion, maintaining contact with the footplate throughout the movement. Range of motion was recorded from the footplate position. We recorded the maximal range from 3 repetitions in each direction. The contralateral ankle was moved passively to the test angle with a controlled velocity (approximately 1°/s) and held while participants actively reproduced the angle with the test ankle. For each movement, the assessor instructed participants to match the position immediately after the contralateral foot was in the final position. The rest interval between each movement ranged from 5 to 10 seconds. We presented the 3 target angles randomly 10 times each and calculated the average error in the matched angle.33
Motor Planning
Motor planning was assessed using the choice stepping reaction time and limb laterality recognition tasks.
Choice Stepping Reaction Time Task
This task assesses the ability of participants to interpret sensory information to plan a motor response. It has not been used in participants with musculoskeletal conditions, but its reliability and validity have been established.34 A custom-designed apparatus was used. This device was made of a nonslip 80- × 80-cm platform and contained four 32- × 15-cm, randomly illuminated panels: 1 panel located in front of each foot and 1 panel located at each side of the participant. We illuminated each panel 5 times and required participants to step onto the lit panel as quickly as possible with the right foot for the right panels and the left foot for the left panels. The mean response time for the stepping foot was measured from illumination until stepping on the lit panel via a pressure switch that sent information to a computer. Participants had 1 practice trial with 8 responses, involving the illumination of all 4 panels twice. After the practice trial, participants performed the choice stepping task once with 20 responses. That is, each panel illuminated 5 times in a random order.
Limb Laterality Recognition Task
The test for limb laterality has been used to investigate central changes in people with chronic pain.35 An increased time to recognize the laterality of images is thought to be related to deficiencies in integration of information processing, working body schema, and premotor processes in the cortex.36 The simple computer-based test consists of 40 images of feet in different positions appearing briefly on the screen at regular intervals. A specialized reaction time collection device was developed and used to obtain accurate reaction time. The images in a variety of rotations and a variety of postures appeared briefly on a computer screen at regular 3-second intervals. Participants were familiarized with the test by performing 2 practice trials with 20 pictures, none of which was included in the test trials. We required participants to determine laterality (ie, left or right foot) for each picture. The average response time and the total number of correct responses in left or right judgment were recorded and used for analysis.
Inversion and Eversion Peak Power
We determined peak power in 2 directions (inversion, eversion) and at 3 velocities (60°/s, 90°/s, 120°/s) using isokinetic dynamometry (Multi-Joint System 2; Biodex Medical Systems, Shirley, NY).12 Participants were seated with the knee and hip in 90° of flexion and the foot placed and stabilized on a footplate in a plantigrade position. We instructed them to actively move to their maximal inversion and eversion while the foot was stabilized on the footplate. The range of movement during the test was set based on their maximal active range of inversion-eversion. After familiarization and 3 practices in each direction and for each velocity, participants performed 3 maximal isokinetic and concentric contractions. The order of movements into each direction was randomized. Peak power was derived from the peak torque and angular velocity12 and was normalized by body mass. For each velocity, the maximal peak power out of 3 repetitions was used for analysis.
Functional Test
Timed up and down stairs is a measure of functional performance.37 Participants were required to ascend and descend a flight of 10 stairs as quickly as possible without using the hand rails. The timing began on the signal to start and terminated when they returned with both feet to the ground level. A stopwatch (240 Econosport stopwatch; SportLine, Elmsford, NY) was used to record the time to the nearest 100th of a second. Three trials were performed, and the best trial was used for analysis.
Statistical Analysis
Data were tested for normality using the Kolmogorov-Smirnov Z test. Discriminant analysis was performed to (1) determine whether differences existed between the average score profile on a set of variables for the 2 defined groups (control, index ankle sprain) and (2) determine the strength of the relationship between the tested variables and sprain status, indicating which of the independent variables accounted for the greatest differences in the average score profiles of the 2 groups.
When using discriminant analysis, Spicer38 recommended that the smallest group sample size in the dependent variable categories (ie, control, index ankle sprain) should be at least 20 and be greater than the number of independent variables included in the model. Thus, we recruited 30 participants in the index ankle-sprain group, and to increase power to enable analysis of more variables, we enrolled more than 2 control participants for each participant with an index ankle sprain.39 The sample size, therefore, was estimated as 100 (70 control participants, 30 participants with index ankle sprains).
We tested equality of group means to investigate differences between groups and used the Fisher function coefficient to identify which function coefficient maximized the discrimination between groups. Variables that differed between groups at P < .05 were included in the backward stepwise discriminant analysis to reduce the discriminant function to a minimum of relevant variables that explained the greatest variance in sprain status. The Wilks λ calculations showed the statistical differences for the discriminant-analysis model. Finally, we established the clinical meaningfulness of the discriminant models by calculating positive and negative likelihood ratios for outcomes that successfully discriminated between groups using the method described by Portney and Watkins.40 Whereas not planned before data collection began, we used a post hoc Pearson correlation coefficient to further explore the findings of the discriminant analysis. The α level was set at .05. Statistical analyses were performed using SPSS (version 19; IBM Corporation, Armonk, NY).
RESULTS
Participants
The left lower limb was dominant in 5 participants (control group). We defined lower limb dominance as the limb that participants preferred for at least 2 of the hop, kick, and step tasks. In the index ankle-sprain group, 14 had sprained their dominant ankles (right) and 16 had sprained their nondominant ankles (left). The proportions of right and left ankles and of dominant and nondominant limbs were similar in both groups. Of the 30 participants with index ankle sprains, 20 had sprained their ankles during a sport activity; 10, during normal daily activities. The average time since the sprain was 3.5 ± 1.5 months (range, 3 weeks to 6 months). Participants with an index ankle sprain had lower CAIT scores than controls (Table 1). No other difference was found between groups in any of the demographic or physical measures. No data were missing for any participant.
Physical, Neuromuscular, and Functional Measures
During the response to perturbation, 7 participants (5 in the control group, 2 in the index ankle-sprain group) failed all attempts during the test, and their response times were considered as 15 seconds. In addition, 5 participants (3 in the control group, 2 in the index ankle-sprain group) did not fail but could not reach their baseline balance during 10 seconds, and their response times were considered as 12 seconds.
The discriminant analysis revealed an association between groups and test variables, accounting for 40% of the variance (
 = 42.16, P = .03). The model containing all variables (ie, balance, proprioception, motor control, power, and function) correctly identified sprain status for 77% (n = 23) of the index ankle-sprain group and 80% (n = 56) of the control group. In the discriminant model, we observed between-groups differences for only 6 variables: dorsiflexion ROM, time to balance after the perturbation, SEBT (anterior direction), foot lifts during single-legged stance with eyes closed, timed up and down stairs, and eversion peak power at 30°/s velocity (Table 3). The discriminant model including these 6 variables had a positive likelihood ratio of 2.80 and a negative likelihood ratio of 0.36.
= 42.16, P = .03). The model containing all variables (ie, balance, proprioception, motor control, power, and function) correctly identified sprain status for 77% (n = 23) of the index ankle-sprain group and 80% (n = 56) of the control group. In the discriminant model, we observed between-groups differences for only 6 variables: dorsiflexion ROM, time to balance after the perturbation, SEBT (anterior direction), foot lifts during single-legged stance with eyes closed, timed up and down stairs, and eversion peak power at 30°/s velocity (Table 3). The discriminant model including these 6 variables had a positive likelihood ratio of 2.80 and a negative likelihood ratio of 0.36.
Table 3. .
Variables Measured in Control and Index Ankle-Sprain Groupsa
| Variable |
Group |
Fisher Function Coefficient |
P Value |
|
| Control |
Index Ankle Sprain |
|||
| Inversion range of motion, ° (mean ± SD) | 33.10 ± 8.00 | 30.70 ± 10.10 | 1.70 | .20 |
| Eversion range of motion, ° (mean ± SD) | 14.70 ± 5.10 | 14.60 ± 6.50 | 0.17 | .66 |
| Dorsiflexion range of motion, cm (mean ± SD) | 11.30 ± 3.80 | 9.90 ± 3.40 | 5.90 | .02b |
| Response to inversion perturbation, s (mean ± SD) | 2.80 ± 3.13 | 4.83 ± 5.94 | 3.67 | .03b |
| Star Excursion Balance Test, cm (mean ± SD) | ||||
| Anterior reach/leg length | 67.95 ± 6.97 | 63.35 ± 6.09 | 9.82 | .002b |
| Posterolateral reach/leg length | 69.74 ± 11.96 | 66.75 ± 14.03 | 1.18 | .28 |
| Posteromedial reach/leg length | 74.69 ± 11.96 | 72.78 ± 12.47 | 0.52 | .47 |
| No. of foot lifts during single-legged stance with eyes closed (mean ± SD) | 17.91 ± 9.42 | 25.00 ± 14.00 | 8.74 | .04b |
| Demi-pointe balance test (No.) | 0.71 | .27 | ||
| Fail | 16 | 10 | ||
| Pass | 54 | 20 | ||
| Joint position sense, target angle, ° (mean ± SD) | ||||
| 5° inversion | 4.23 ± 2.51 | 4.85 ± 2.82 | 1.20 | .28 |
| Maximal inversion −5° | 4.25 ± 2.46 | 4.81 ± 2.81 | 0.16 | .32 |
| Maximal eversion −5° | 4.91 ± 3.90 | 3.83 ± 2.18 | 1.50 | .22 |
| Movement detection sense, % (mean ± SD) | ||||
| Inversion speed, °/s | ||||
| 0.1 | 69.00 ± 22.10 | 65.30 ± 20.6 | 0.60 | .44 |
| 0.5 | 70.60 ± 27.30 | 68.30 ± 20.0 | 0.16 | .69 |
| 2.5 | 75.60 ± 30.10 | 63.30 ± 28.7 | 3.57 | .06 |
| Eversion speed, °/s | ||||
| 0.1 | 66.70 ± 22.20 | 73.00 ± 17.80 | 1.91 | .17 |
| 0.5 | 68.60 ± 30.00 | 68.00 ± 24.30 | 0.01 | .93 |
| 2.5 | 71.10 ± 31.70 | 76.30 ± 27.50 | 0.61 | .44 |
| Peak power/body weight, (N·m/s)/kg (mean ± SD) | ||||
| Inversion speed, °/s | ||||
| 30 | 20.09 ± 7.41 | 18.46 ± 8.38 | 0.95 | .34 |
| 60 | 33.25 ± 11.23 | 32.12 ± 11.97 | 0.21 | .65 |
| 120 | 53.10 ± 17.15 | 52.01 ± 19.58 | 0.08 | .78 |
| Eversion speed, °/s | ||||
| 30 | 16.47 ± 5.59 | 13.85 ± 5.24 | 4.76 | .03b |
| 60 | 27.42 ± 10.25 | 23.26 ± 9.87 | 3.54 | .06 |
| 120 | 46.18 ± 20.37 | 39.11 ± 15.86 | 2.87 | .09 |
| Choice stepping reaction time, s (mean ± SD) | 0.43 ± 0.08 | 0.45 ± 0.07 | 1.41 | .09 |
| Limb laterality recognition task (mean ± SD) | ||||
| No. of correct responses | 15.71 ± 1.17 | 15.37 ± 1.19 | 0.35 | .56 |
| Response time, s | 2.49 ± 0.19 | 3.15 ± 0.19 | 0.32 | .57 |
| Timed up and down stairs, s (mean ± SD) | 5.70 ± 0.97 | 6.53 ± 1.93 | 8.00 | .006b |
All the presented variables were analyzed separately.
Indicates between-groups difference (P < .05).
The results of the stepwise discriminant analysis using these 6 variables revealed an association between 2 tests (SEBT anterior direction and foot lifts during single-legged stance) and sprain status (Table 4). These 2 variables explained 15% of the between-groups variance (
 = 15.2, P = .001). The model correctly predicted the sprain status of 63% (n = 19) of the index ankle-sprain group and 69% (n = 48) of the control group and had a positive likelihood ratio of 2.03 and a negative likelihood ratio of 0.54.
= 15.2, P = .001). The model correctly predicted the sprain status of 63% (n = 19) of the index ankle-sprain group and 69% (n = 48) of the control group and had a positive likelihood ratio of 2.03 and a negative likelihood ratio of 0.54.
Table 4. .
Backward Stepwise Discriminant Modela
| Step |
Included Variable |
Fisher Function Coefficient |
r 2 |
% of Correct Prediction |
Wilks λb |
P Value |
|||
| Index Ankle-Sprain Group |
Control Group |
λ |
df 1c |
df 2d |
|||||
| 1 | Response to inversion perturbation | 3.67 | 19.2 | 74 | 73 | 0.817 | 6 | 98 | .004 |
| Eversion peak power (30°/s) | 4.76 | ||||||||
| Dorsiflexion range of motion | 5.90 | ||||||||
| Timed stair test | 8.00 | ||||||||
| No. of foot lifts during single-legged stance with eyes closed | 8.74 | ||||||||
| Star Excursion Balance Test | 9.82 | ||||||||
| 2 | Eversion peak power (30°/s) | 4.76 | 18.4 | 70 | 76 | 0.824 | 5 | 98 | .002 |
| Dorsiflexion range of motion | 5.90 | ||||||||
| Timed stair test | 8.00 | ||||||||
| No. of foot lifts during single-legged stance with eyes closed | 8.74 | ||||||||
| Star Excursion Balance Test | 9.82 | ||||||||
| 3 | Dorsiflexion range of motion | 5.90 | 17.7 | 73 | 73 | 0.832 | 4 | 98 | .001 |
| Timed stair test | 8.00 | ||||||||
| No. of foot lifts during single-legged stance with eyes closed | 8.74 | ||||||||
| Star Excursion Balance Test | 9.82 | ||||||||
| 4 | Timed stair test | 8.00 | 16.9 | 70 | 68 | 0.840 | 3 | 98 | .001 |
| No. of foot lifts during single-legged stance with eyes closed | 8.74 | ||||||||
| Star Excursion Balance Test | 9.82 | ||||||||
| 5 | No. of foot lifts during single-legged stance with eyes closed | 8.74 | 15.2 | 63 | 69 | 0.855 | 2 | 98 | .001 |
| Star Excursion Balance Test | 9.82 | ||||||||
Abbreviation: df, degrees of freedom.
At each step, the variable with the lowest Fisher function coefficient and highest Wilks λ was excluded from the model.
Wilks λ indicates the significance of the discriminant model. The 2 predictors that add discriminative power to the discriminant model are different at P = .01.
The effect degrees of freedom for the given function are based on the number of groups present in the categorical variable and the number of continuous discriminant variables.
The error degrees of freedom for the given function are based on the number of groups present in the categorical variable, the number of continuous discriminant variables, and the number of observations in the analysis.
Through our post hoc analysis, we observed that dorsiflexion ROM was moderately correlated with the anterior-reach distance on the SEBT (r = 0.523, P < .001) but only weakly correlated with posteromedial-reach (r = 0.298, P < .001) and posterolateral-reach (r = 0.362, P < .001) distances on the SEBT.
DISCUSSION
The primary purpose of our study was to determine which factors were the most predictive of membership in 2 groups: control or index ankle sprain. Therefore, we investigated the relationships between variables in different domains and sprain status. We observed that a combination of measures of balance, proprioception, motor control, and function predicted sprain status in most participants, elucidating the multifactorial nature of impairments after an ankle sprain. Whereas all variables predicted the group memberships for more than 75% of participants in both groups, only 6 variables were different between groups. Among the 6 variables, which consisted of 3 measures of balance, the timed stair test, dorsiflexion ROM, and eversion peak power (30°/s), the combination of only 2 balance measures explained most of the differences between groups in the final discriminant model. The anterior-reach distance on the SEBT was less and the number of foot lifts during single-legged stance was greater in the index ankle-sprain group than in the control group. These measures may help researchers or clinicians detect impairments associated with ankle sprains and may have implications for the treatment of these patients.
Investigators41 have found that the anterior-reach distance on the SEBT is reduced in participants with recurrent sprains. These participants demonstrated reduced dorsiflexion ROM, which was moderately correlated with performance in the anterior direction of the SEBT.41 Our index ankle-sprain participants also had less dorsiflexion ROM than those in the control group, and in a post hoc analysis, we found similar results. Dorsiflexion ROM was moderately correlated with the anterior-reach distance on the SEBT but only weakly correlated with posteromedial-reach and posterolateral-reach distances on the SEBT. The number of foot lifts during single-legged stance was also associated with sprain status, which was consistent with the results of Hiller et al.28 They found that participants with a history of ankle sprain had a higher number of foot lifts than control participants.28
Deficits in balance and postural control after the index ankle sprain may be due to several factors, such as changes in postural-control strategies.42 Two discrete postural strategies have been hypothesized to produce adaptable control of the horizontal position of the center of gravity: the ankle strategy and the hip strategy.43 Whereas the ankle strategy repositions the center of gravity by moving the whole body as a single-segment inverted pendulum around the ankle joint, the hip strategy moves the body as a double-segment inverted pendulum with counterphase motions around the hip and ankle.43 Thus, the ankle strategy is useful during static balance, whereas the hip strategy appears more useful during dynamic balance. Participants with ankle injuries shifted from the typical ankle strategy of balance maintenance during single-legged stance to the less efficient hip strategy of balance.42 Therefore, to control their posture, participants logically lift the borders of the foot to counterbalance movements around the hip joint, as we observed. Bullock-Saxton44 suggested that such changes may result from altered proximal muscle activity in response to ankle injury.
Researchers8 have also associated impaired postural control after an ankle sprain with proprioceptive deficits. Even measures of static postural control are sometimes used as assessment tools for a proprioception test.15,16 However, we found no differences in the results of 2 proprioceptive tests between participants with index ankle sprains and control participants. Consistent with our findings, Myers et al45 and Riemann et al46 did not report balance deficits when they reduced proprioceptive input from ligamentous mechanoreceptors at the ankle joint using local anesthesia that simulated deafferentation after an ankle sprain.45
Our results highlight the importance of targeting dynamic and static balance impairments after an acute ankle sprain in treatment strategies. Several researchers found balance training effectively prevented recurrent sprains. Wester et al47 observed that participants with ankle sprains who received balance training for 8 weeks had fewer recurrent sprains (25%) than participants who did not receive balance training (54%) during their 8-month follow-up study. Holme et al11 reported similar findings at 1-year follow-up of participants after acute ankle sprain. Participants who pursued a 6-week balance-training program had fewer resprains (7%) than participants who did not perform such training (29%). Our results will also enable us to investigate prospectively whether balance impairments after a recent index ankle sprain can predict the risk of recurrent sprains.
We observed that inversion and eversion peak power, as well as motor planning and control, did not discriminate sprain status. Wilkerson et al12 found that participants with acute ankle sprains had deficits in invertor and evertor muscle strength or power 3 weeks after the injury. However, at the 6- and 12-week follow-ups, no deficit was detected.12 They suggested that the initial reduction in muscle power probably resulted from a reduction in neuromuscular recruitment due to pain or edema, or both. Therefore, the exclusion of participants with pain likely explains the difference in findings.
We evaluated the clinical meaningfulness of the discriminant models by computing positive and negative likelihood ratios for the 6- and 2-variable discriminant models. Positive and negative likelihood ratios reflect the shift in probability of the condition being present after the clinical test results are obtained. Using the 6-variable discriminant model, the proportions of participants who were allocated correctly to the index ankle-sprain and control groups were 74% (22/30) and 73% (51/70), respectively. These results demonstrate that in participants with impaired balance (indicated by 3 balance tests), reduced dorsiflexion ROM, decreased eversion peak power (30°/s), and increased time during the stair test, the probability of the ankle sprain being truly present was 2.80. However, when using only 2 balance measures (SEBT and number of foot lifts during single-legged stance with eyes closed), the probability of the ankle sprain being truly present in participants with impaired balance was reduced to 2.03, with 63% (19/30) of participants correctly allocated to the index ankle-sprain group and 69% (48/70) correctly allocated to the control group. This shift in probability indicated that the 2-variable discriminant model was at the cutoff point of clinical meaningfulness. This finding suggests that, whereas clinicians may choose to examine only anterior reach on the SEBT test and the number of foot movements during single-legged stance when assessing patients with ankle sprains, it may be better to include the other test variables (ie, timed stair test, dorsiflexion ROM, eversion power, or response to perturbation), depending on equipment availability and time constraints in the clinical setting.
Our study had limitations. One limitation was the different times since the index ankle sprain (3 weeks to 6 months) in the participants. This difference was due to our including recruits when they had no clinical symptoms and had resumed their normal physical activities, leading to most participants in the index ankle-sprain group (n = 23, 77%) being tested between 1 and 4 months after their injuries. In future studies, researchers could enroll participants at a set time or stage after index ankle sprain to confirm our findings. Another potential limitation to this study was that we did not control for participants seeking treatment for their sprains. Seven participants had received rehabilitation before the study. However, when we performed a post hoc analysis, we observed no differences between participants who received rehabilitation and those who did not.
CONCLUSIONS
Impairments in balance and postural control are strongly associated with a history of index ankle sprain. A combination of performance on the SEBT (anterior direction) and the number of foot lifts during single-legged stance with eyes closed most strongly discriminated between participants with index ankle sprains and healthy control participants and, therefore, should be targeted in treatments. Decreased range of dorsiflexion may contribute to these impairments. Furthermore, the combination of measures of balance, proprioception, motor control, and function predicted sprain status in most participants, which confirmed the wider effect of what is generally considered a simple injury.
ACKNOWLEDGMENTS
This research was presented at the World Confederation for Physical Therapy Congress 2015, May 1–4, 2015, Singapore. Portions of the data have also been presented at the Fifth International Ankle Symposium, October 17–20, 2012, Lexington, Kentucky, and the Third Congress of the International Foot and Ankle Biomechanics Community, April 11–13, 2012, Sydney, Australia.
REFERENCES
- 1. Soboroff SH, Pappius EM, Komaroff AL. Benefits, risks, and costs of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop Relat Res. 1984; 183: 160– 168. [PubMed] [Google Scholar]
- 2. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010; 92 13: 2279– 2284. [DOI] [PubMed] [Google Scholar]
- 3. Waterman BR, Belmont PJ, Jr, Cameron KL, Deberardino TM, Owens BD. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010; 38 4: 797– 803. [DOI] [PubMed] [Google Scholar]
- 4. Fong DT, Hong Y, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007; 37 1: 73– 94. [DOI] [PubMed] [Google Scholar]
- 5. Birrer RB, Fani-Salek MH, Totten VY, Herman LM, Politi V. Managing ankle injuries in the emergency department. J Emerg Med. 1999; 17 4: 651– 660. [DOI] [PubMed] [Google Scholar]
- 6. Hiller CE, Nightingale EJ, Raymond J, et al. Prevalence and impact of chronic musculoskeletal ankle disorders in the community. Arch Phys Med Rehabil. 2012; 93 10: 1801– 1807. [DOI] [PubMed] [Google Scholar]
- 7. Gribble PA, Delahunt E, Bleakley C, et al. Selection criteria for patients with chronic ankle instability in controlled research: a position statement of the International Ankle Consortium. Br J Sports Med. 2014; 48 13: 1014– 1018. [DOI] [PubMed] [Google Scholar]
- 8. Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002; 37 4: 364– 375. [PMC free article] [PubMed] [Google Scholar]
- 9. Genthon N, Bouvat E, Banihachemi JJ, Bergeau J, Abdellaoui A, Rougier PR. Lateral ankle sprain alters postural control in bipedal stance: part 1. Restoration over the 30 days following the injury. Scand J Med Sci Sports. 2010; 20 2: 247– 254. [DOI] [PubMed] [Google Scholar]
- 10. Akbari M, Karimi H, Farahini H, Faghihzadeh S. Balance problems after unilateral lateral ankle sprains. J Rehabil Res Dev. 2006; 43 7: 819– 824. [DOI] [PubMed] [Google Scholar]
- 11. Holme E, Magnusson SP, Becher K, Bieler T, Aagaard P, Kjaer M. The effect of supervised rehabilitation on strength, postural sway, position sense and re-injury risk after acute ankle ligament sprain. Scand J Med Sci Sports. 1999; 9 2: 104– 109. [DOI] [PubMed] [Google Scholar]
- 12. Wilkerson GB, Pinerola JJ, Caturano RW. Invertor vs. evertor peak torque and power deficiencies associated with lateral ankle ligament injury. J Orthop Sports Phys Ther. 1997; 26 2: 78– 86. [DOI] [PubMed] [Google Scholar]
- 13. Leanderson J, Bergqvist M, Rolf C, Westblad P, Wigelius-Roovers S, Wredmark T. Early influence of an ankle sprain on objective measures of ankle joint function: a prospective randomised study of ankle brace treatment. Knee Surg Sports Traumatol Arthrosc. 1999; 7 1: 51– 58. [DOI] [PubMed] [Google Scholar]
- 14. Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002; 32 4: 166– 173. [DOI] [PubMed] [Google Scholar]
- 15. Leanderson J, Eriksson E, Nilsson C, Wykman A. Proprioception in classical ballet dancers: a prospective study of the influence of an ankle sprain on proprioception in the ankle joint. Am J Sports Med. 1996; 24 3: 370– 374. [DOI] [PubMed] [Google Scholar]
- 16. Cornwall MW, Murrell P. Postural sway following inversion sprain of the ankle. J Am Podiatr Med Assoc. 1991; 81 5: 243– 247. [DOI] [PubMed] [Google Scholar]
- 17. Tropp H, Ekstrand J, Gillquist J. Factors affecting stabilometry recordings of single limb stance. Am J Sports Med. 1984; 12 3: 185– 188. [DOI] [PubMed] [Google Scholar]
- 18. Ledin T, Hafstrom A, Fransson PA, Magnusson M. Influence of neck proprioception on vibration-induced postural sway. Acta Otolaryngol. 2003; 123 5: 594– 599. [DOI] [PubMed] [Google Scholar]
- 19. Hiller CE, Refshauge KM, Bundy AC, Herbert RD, Kilbreath SL. The Cumberland Ankle Instability Tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006; 87 9: 1235– 1241. [DOI] [PubMed] [Google Scholar]
- 20. Donahue M, Simon J, Docherty CL. Critical review of self-reported functional ankle instability measures. Foot Ankle Int. 2011; 32 12: 1140– 1146. [DOI] [PubMed] [Google Scholar]
- 21. Kurtze N, Rangul V, Hustvedt BE. Reliability and validity of the International Physical Activity Questionnaire in the Nord-Trondelag Health Study (HUNT) population of men. BMC Med Res Methodol. 2008; 8: 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin Biomech (Bristol, Avon). 2006; 21 1: 89– 98. [DOI] [PubMed] [Google Scholar]
- 23. Hiller CE, Refshauge KM, Herbert RD, Kilbreath SL. Intrinsic predictors of lateral ankle sprain in adolescent dancers: a prospective cohort study. Clin J Sport Med. 2008; 18 1: 44– 48. [DOI] [PubMed] [Google Scholar]
- 24. Menadue C, Raymond J, Kilbreath SL, Refshauge KM, Adams R. Reliability of two goniometric methods of measuring active inversion and eversion range of motion at the ankle. BMC Musculoskelet Disord. 2006; 7: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. O'Shea S, Grafton K. The intra and inter-rater reliability of a modified weight-bearing lunge measure of ankle dorsiflexion. Man Ther. 2013; 18 3: 264– 268. [DOI] [PubMed] [Google Scholar]
- 26. Nakagawa L, Hoffman M. Performance in static, dynamic, and clinical tests of postural control in individuals with recurrent ankle sprains. J Sport Rehabil. 2004; 13 3: 255– 268. [Google Scholar]
- 27. Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012; 47 3: 339– 357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hiller CE, Refshauge KM, Herbert RD, Kilbreath SL. Balance and recovery from a perturbation are impaired in people with functional ankle instability. Clin J Sport Med. 2007; 17 4: 269– 275. [DOI] [PubMed] [Google Scholar]
- 29. Hertel J, Miller SJ, Denegar CR. Intratester and intertester reliability during the Star Excursion Balance Tests. J Sport Rehabil. 2000; 9 2: 104– 116. [Google Scholar]
- 30. Gribble PA, Hertel J. Considerations for normalizing measures of the Star Excursion Balance Test. Meas Phys Educ Exerc Sci. 2003; 7 2: 89– 100. [Google Scholar]
- 31. Refshauge KM, Raymond J, Kilbreath SL, Pengel L, Heijnen I. The effect of ankle taping on detection of inversion-eversion movements in participants with recurrent ankle sprain. Am J Sports Med. 2009; 37 2: 371– 375. [DOI] [PubMed] [Google Scholar]
- 32. Refshauge KM, Kilbreath SL, Raymond J. Deficits in detection of inversion and eversion movements among subjects with recurrent ankle sprains. J Orthop Sports Phys Ther. 2003; 33 4: 166– 173. [DOI] [PubMed] [Google Scholar]
- 33. Konradsen L, Magnusson P. Increased inversion angle replication error in functional ankle instability. Knee Surg Sports Traumatol Arthrosc. 2000; 8 4: 246– 251. [DOI] [PubMed] [Google Scholar]
- 34. Lord SR, Ward JA, Williams P, Anstey KJ. Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc. 1994; 42 10: 1110– 1117. [DOI] [PubMed] [Google Scholar]
- 35. Coslett HB, Medina J, Kliot D, Burkey A. Mental motor imagery and chronic pain: the foot laterality task. J Int Neuropsychol Soc. 2010; 16 4: 603– 612. [DOI] [PubMed] [Google Scholar]
- 36. Hudson ML, McCormick K, Zalucki N, Moseley GL. Expectation of pain replicates the effect of pain in a hand laterality recognition task: bias in information processing toward the painful side. Eur J Pain. 2006; 10 3: 219– 224. [DOI] [PubMed] [Google Scholar]
- 37. Zaino CA, Marchese VG, Westcott SL. Timed up and down stairs test: preliminary reliability and validity of a new measure of functional mobility. Pediatr Phys Ther. 2004; 16 2: 90– 98. [DOI] [PubMed] [Google Scholar]
- 38. Spicer J. Making Sense of Multivariate Data Analysis. Thousand Oaks, CA: SAGE Publications, Inc; 2005: 139– 152. [Google Scholar]
- 39. Hennessy S, Bilker WB, Berlin JA, Strom BL. Factors influencing the optimal control-to-case ratio in matched case-control studies. Am J Epidemiol. 1999; 149 2: 195– 197. [DOI] [PubMed] [Google Scholar]
- 40. Portney L, Watkins M. Foundations of Clinical Research: Applications to Practice. 3rd ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2008: 619– 658. [Google Scholar]
- 41. Basnett CR, Hanish MJ, Wheeler TJ, et al. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int J Sports Phys Ther. 2013; 8 2: 121– 128. [PMC free article] [PubMed] [Google Scholar]
- 42. Pintsaar A, Brynhildsen J, Tropp H. Postural corrections after standardised perturbations of single limb stance: effect of training and orthotic devices in patients with ankle instability. Br J Sports Med. 1996; 30 2: 151– 155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Runge CF, Shupert CL, Horak FB, Zajac FE. Ankle and hip postural strategies defined by joint torques. Gait Posture. 1999; 10 2: 161– 170. [DOI] [PubMed] [Google Scholar]
- 44. Bullock-Saxton JE. Local sensation changes and altered hip muscle function following severe ankle sprain. Phys Ther. 1994; 74 1: 17– 28. [DOI] [PubMed] [Google Scholar]
- 45. Myers JB, Riemann BL, Hwang JH, Fu FH, Lephart SM. Effect of peripheral afferent alteration of the lateral ankle ligaments on dynamic stability. Am J Sports Med. 2003; 31 4: 498– 506. [DOI] [PubMed] [Google Scholar]
- 46. Riemann BL, Myers JB, Stone DA, Lephart SM. Effect of lateral ankle ligament anesthesia on single-leg stance stability. Med Sci Sports Exerc. 2004; 36 3: 388– 396. [DOI] [PubMed] [Google Scholar]
- 47. Wester JU, Jespersen SM, Nielsen KD, Neumann L. Wobble board training after partial sprains of the lateral ligaments of the ankle: a prospective randomized study. J Orthop Sports Phys Ther. 1996; 23 5: 332– 336. [DOI] [PubMed] [Google Scholar]