Abstract
Health and immigration researchers often implicate dietary acculturation in explanations of Mexican children of immigrants’ weight gain after moving to the U.S., but rarely explore how diet is shaped by immigrants’ structural incorporation. We used data from the 1999/00–2009/10 National Health and Nutrition Examination Survey to assess how indicators of Mexican-origin children’s acculturation and structural incorporation influence two outcomes: how healthy and how “Americanized” children’s diets are. Indicators of acculturation were strongly associated with more Americanized and less healthy diets. However, structural incorporation indicators were mostly unrelated to diet outcomes net of acculturation. An exception was that parental education was positively associated with consuming a healthy diet. Finally, children of natives consumed more Americanized, unhealthy diets than children of immigrants and these differences were largely explained by differences in the acculturation. Children of natives would have consumed an even less healthy diet were it not for their higher levels of parental education. Overall, the results suggest that the process of adapting to the U.S. life style is associated with the loss of cultural culinary preferences and less healthy eating behaviors despite improvements in socioeconomic status.
Keywords: Mexican-origin, Children, Dietary acculturation, Diet quality, Health assimilation, Socioeconomic status
Introduction
Mexican-origin children are among the heaviest race/ethnic groups in the U.S. (Flegal et al. 2010; Ogden et al. 2012). Although obesity is also high and increasing in Mexico (Rivera et al. 2009), obesity among U.S.-resident Mexican-origin children does not appear to be imported from Mexico. Instead, Mexican children who are the most likely to migrate to the U.S. are among the leanest in Mexico. They appear to gain weight rapidly after arriving in the U.S. (Van Hook et al. 2012).
This is unsurprising given that the U.S. environment is often characterized as unhealthy for all residents due to a “default American lifestyle” where deliberate effort is necessary to “swim upstream” and avoid the adoption of unhealthy behaviors including poor diets (Mirowsky and Ross 2010). In fact, few American children have diets that conform to USDA recommendations (Guenther et al. 2013; Hiza et al. 2013). An apt illustration of this point is how prevalent consumption of sugar-sweetened beverages is among U.S. youth. Soda consumption contributes to the majority of total beverage intake for 12–19-year olds of every U.S. racial/ethnic group (Storey et al. 2006), and on any given day, 70 % of boys and 60 % of girls aged 2–19 consume beverages with added sugar (Ogden et al. 2011).
Absent any effort to resist this normative unhealthy American lifestyle, the acculturation of Mexican children of immigrants should implicitly lead to dietary changes that have been implicated in U.S. Mexican-origin children’s high-obesity prevalence (Gordon-Larsen et al. 2003). This is worrying because children’s eating behaviors will affect their health and well-being across the life course (Birch 1999; Birch and Fischer 1998). However, this depiction of the assimilation process does not fully recognize the extent to which health outcomes are socioeconomically stratified within American society.
Gordon’s (1964) classic work on immigrant assimilation and Portes and Zhou’s (1993) segmented assimilation perspective motivated us to extend beyond prior research. Both frameworks recognize the importance of acculturation (immigrants’ assimilation of American culture, preferences, and norms) and structural incorporation (immigrants’ inclusion in the U.S. system of socioeconomic opportunity and mobility). In this paper, we ask whether one can assume that Mexican-origin children’s dietary outcomes are a function of acculturation alone, or whether they are also shaped by indicators of structural incorporation.
We also contribute to the prior literature by distinguishing between how “Americanized” and how healthy children’s diets are. Prior research on U.S. immigrants’ diets often assumes that declines in diet quality (i.e., how healthy the diet is) are synonymous with how American the diet is. However, not all aspects of adopting an American diet are necessarily unhealthy. Replacing low-fiber bread and high-fat milk for high-fiber bread and low-fat milk have been identified as beneficial changes in the dietary acculturation process of Mexican–Americans (Batis et al. 2011). Thus, we treat diet Americanization and quality as separate constructs.
A third study contribution is that we not only examine how indicators of acculturation and structural incorporation predict individual Mexican-origin children’s diet Americanization and quality, but also use decomposition techniques to investigate how acculturation and structural incorporation explain population-level dietary differences between children of immigrants and children of U.S.-born natives.
Background
Dietary acculturation is a general process of dietary change that often occurs among immigrants. One important aspect of dietary acculturation involves the shift from a diet consisting primarily of foods eaten in immigrants’ country of origin to those of the host society (Satia-Abouta et al. 2002). Diet is an important marker of ethnicity (Waters 1990), and this shift toward eating a more American diet is one of many ways that immigrants begin to assimilate into American culture. A second aspect of dietary acculturation that is often implicitly assumed involves a shift in diet quality. Much evidence supports this assumption. Research has suggested that migration to the U.S. and duration of residence are associated with consuming fewer vegetables, less fiber, more meat, fat, and sugar (Akresh 2007; Ayala et al. 2008; Batis et al. 2011; Brown 2005; Dixon et al. 2000; Duffey et al. 2008; Guendelman and Abrams 1995). That said, other research suggests that the relationship between acculturation and eating a healthy diet is mixed (Batis et al. 2011; Carrera et al. 2007; Edmonds 2005; Liu et al. 2010).
Dietary acculturation is usually understood by public health and epidemiological scholars through a “health acculturation” lens, which argues that health advantages typically enjoyed by newly arrived immigrants decline over time in the U.S. due to the acculturation of U.S. (risky) health behaviors (Abraído-Lanza et al. 2006; e.g., Aldrich and Variyam 2000). However, some scholars criticize the health acculturation perspective for underestimating structural drivers of health disparities, such as discrimination, legal barriers, and low socioeconomic status (Hunt et al. 2004; Viruell-fuentes et al. 2012). It has been argued that immigrant health research needs to more fully recognize segmented assimilation theory’s premise that immigrants may experience one of three assimilation pathways (Acevedo-Garcia and Bates 2008; Portes and Zhou 1993). Those experiencing barriers to economic mobility but rapid acculturation are vulnerable to “downward assimilation.” Others experiencing simultaneous acculturation and structural incorporation should follow a more straightforward assimilation pathway into the American mainstream, or “straight-line assimilation.” Still others may engage in “selective acculturation” where they delay acculturation through ties to ethnic communities while investing in their children’s educational attainments and upward socioeconomic mobility.
This leads us to explore whether and how acculturation and structural incorporation predict diet Americanization and quality for Mexican-origin children, and how the relative balance of acculturation and incorporation contributes to dietary change across generations. For Mexican-origin families, dietary change most likely begins with crossing the U.S.-Mexico border (Batis et al. 2011) or even earlier in anticipation of migration. Following migration, exposure to U.S. foods and eating behaviors is structured by children’s family and neighborhood contexts within the U.S. In the next section, we expand upon family and neighborhood-level indicators of acculturation and incorporation that we expect to be related to diet Americanization and quality.
Acculturation and Structural Incorporation as Predictors of Mexican-Origin Children’s Diets
We expect children with more acculturated families and neighborhoods to eat a more Americanized diet. Many family-level indicators of acculturation, including English language use, generational status, and the percentage of food eaten away from home, are associated with greater intake of commonly consumed American foods among Hispanic children (Van Hook et al. 2015). Children’s community contexts also shape opportunities for dietary change. Living in immigrant communities may slow down Mexican-origin children’s diet Americanization. Co-ethnic social networks create markets for ethnic foods (Portes 1998; Portes and Sensenbrenner 1993) and reduce the desire to fit in by eating American foods (Guendelman et al. 2011).
More acculturated families and neighborhoods will also likely lead Mexican-origin youth to consume less healthy diets, though we are less certain about this supposition because of conflicting evidence about the way that parents’ acculturation is related to children’s eating. Supporting our supposition is evidence of the protective effect that living in an immigrant neighborhood has on the diets of Mexican-origin persons in the U.S. (Dubowitz et al. 2008b; Kimbro and Denney 2013; Osypuk et al. 2009; Park et al. 2008; Reyes-Ortiz et al. 2009; Wen and Maloney 2011) and the deleterious effect of generational status for Hispanic children’s diet quality (Van Hook et al. 2015). However, some studies find that parents’ acculturation is unevenly related to eating specific kinds of healthy and unhealthy foods (e.g., it reduces fruit consumption, increases fast food consumption, but has no association with vegetable consumption) (Kaiser et al. 2015; Erinosho et al. 2012), while yet other research finds that children of more acculturated parents actually consume more fruits and vegetables than children of less acculturated parents (Chaparro et al. 2015).
We expect structural incorporation, like acculturation, to foster diet Americanization. Although empirical evidence on this topic is thin, we suspect that middle-class Mexican-origin families are likely to come into greater contact with non-Hispanic whites in schools, neighborhoods, and workplaces than lower SES families, and may have more opportunities and social pressure to try out U.S. foods in these contexts (Guendelman et al. 2011).
However, unlike acculturation, incorporation should be positively associated with Mexican-origin children’s diet quality. This supposition is consistent with previous research showing that family-level socioeconomic status is associated with healthier eating among Mexican-origin (Martin et al. 2015) and Hispanic children (Balistreri and Van Hook 2009). Neighborhood SES also predicts healthy eating. Living in disadvantaged neighborhoods is associated with poorer diet quality, less fruit and vegetable intake (Dubowitz et al. 2008a), greater fat and sodium consumption (Keita et al. 2009), and childhood obesity (Kimbro and Denney 2013). This reflects the fact that disadvantaged neighborhoods feature more fast food restaurants and convenience stores, and fewer full-service grocery stores and family restaurants, which limits food choices (Drewnowski 2012), especially for lower income, minority, and rural populations (Larson et al. 2009).
We summarize our expectations about the way that acculturation and structural incorporation are related to Mexican-origin’s diets in Table 1. We expect acculturation and structural incorporation to positively predict diet Americanization. Structural incorporation should also increase healthy eating. Conversely, family and neighborhood acculturation could reduce diet quality consistent with some previous research, or it may have no association with diet quality given the limited evidence that it pushes differentially on disparate types of healthy and unhealthy foods.
Table 1.
Expected relationships between acculturation and structural incorporation and Mexican-origin children’s diet Americanization and diet quality
| Diet Americanization | Diet quality | |
|---|---|---|
| Acculturation | Positive | Negative or null |
| Structural incorporation | Positive | Positive |
Do Acculturation and Structural Incorporation Explain Generational Differences in the Diets of Mexican-Origin Children?
While it is important to understand how family and neighborhood-level indicators of acculturation and incorporation predict Mexican-origin children’s individual-level dietary outcomes, it is equally important to understand whether and how population-level compositional differences in acculturation and incorporation translate into group differences in the diets of Mexican-origin children of immigrants and children of natives. Such analyses are imperative for understanding how group-level differences in acculturation and incorporation lead to health disparities between groups.
The compositional differences between Mexican-origin children of immigrants and natives in the U.S. have been described in previous research. As a whole, Mexican-origin children of natives are more integrated into U.S. society than children of immigrants, but there is more variability in their structural incorporation. Mexican-origin children of immigrants have been noted for their exceptionally high levels of poverty and low parental educational attainment (Van Hook et al. 2013). But upward socioeconomic mobility across generations (Myers 2007) leads to higher levels of parental educational attainment, family income (Bean and Stevens 2003), and neighborhood income (South et al. 2005a, b) among Mexican children of natives. In fact, intergenerational mobility between Mexican immigrants and their children is actually higher than the level of mobility between Asian immigrants and their children, at least among immigrants in California (Lee and Zhou 2015). Nevertheless, there is substantial heterogeneity in structural incorporation that results in the Mexican children of natives on average being unable to reach parity with non-Hispanic whites (Telles and Ortiz 2008). It is their partial mobility that largely motivates us to explore how compositional differences between children of immigrants and children of natives produce group differences in diets.
How compositional differences produce diet Americanization is straightforward. The greater acculturation and structural incorporation of Mexican-origin children of natives should lead them to have more Americanized diets than children of immigrants. How compositional differences are related to diet quality is less certain. As discussed in the previous section, the individual-level effects of acculturation and structural incorporation may work against each other, and it is unclear whether enough Mexican-origin children of natives live in households that have experienced enough socioeconomic incorporation to positively impact diet quality at the population level.
Thus, we posit that there are three alternative patterns, illustrated in Fig. 1, of population-level group differences in healthy eating that we could observe. In all three, we hypothesize that children of immigrants have moderately healthy diets. While they do not have many socioeconomic resources to help resist the unhealthy American lifestyle, their lack of acculturation relative to children of natives should protect them because they are unlikely to have shed more traditional food preferences and eating practices.
Fig. 1.
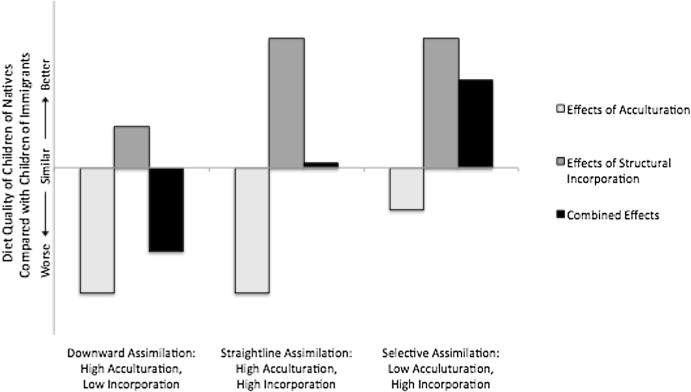
Three alternative expectations of how generational differences in acculturation and structural incorporation produce generational differences in diet quality.
Will the diets of children of natives be less healthy than children of immigrants? This depends on how their stock of acculturation and incorporation is balanced. If children of natives have high levels of acculturation but low levels of structural incorporation, they are likely to have worse diets than children of immigrants. This “downward assimilation” scenario is depicted with the first three bars in Fig. 1. Their high levels of acculturation contribute to much worse diets than children of immigrants (shown by the long light gray bar dipping below the axis). Their modest increases in structural incorporation contribute to slightly better diets (shown by the short dark gray bar). But these effects combine to produce worse diets than children of immigrants (shown by the medium-length black bar dipping below the axis).
Conversely, it is also possible that if enough children of natives have families that are sufficiently upwardly mobile, the diets of children of natives on average may be no worse than the diets of children of immigrants because the group has additional resources. This “straightline assimilation” scenario is depicted by the middle three bars in Fig. 1. The negative effects of acculturation are the same as in the downward assimilation scenario, but they are completely offset by large positive effects of structural incorporation.
Finally, if enough children of natives have families that prevent or delay their children’s acculturation yet experience upward socioeconomic mobility, then group differences in healthy diets may favor children of natives. This third scenario is similar in many ways to the “selective acculturation model” also described by segmented assimilation, and is depicted by the last three bars of Fig. 1.
Methods
Data and Sample
To assess the ideas outlined above, we analyzed data from the 1999/00–2009/10 continuous National Health and Nutrition Examination Survey (NHANES). NHANES is a nationally representative, cross-sectional study conducted by the Centers for Disease Control and Prevention (CDC). We used the restricted-use version of the NHANES, which contains census tract identifiers that we linked to information about the population composition of children’s census tracts. Tract-level data were obtained from the 2000 Census Summary Files (for the 1999/00–2003/04 NHANES) and the 2005–2009 American Community Survey Summary Files (for the 2005/06–2009/10 NHANES). Our sample was restricted to the 6164 Mexican-origin children age 5–19 in the 1999/00–2009/10 NHANES.
Diet Measures
NHANES collects 24-h dietary recall data over two different days by trained interviewers using the U.S. Department of Agriculture (USDA) Automated Multiple-pass Method. Day 1 recalls are conducted in-person and Day 2 recalls are collected by telephone. Half of the children completed both days of dietary recall. For them, we averaged the dietary outcomes across both days. For the remaining children with only one day of dietary recall data, we used only these data.1 Children ages 12 and older completed the dietary recall on their own, while children ages 6–11 were assisted by a proxy. Proxy respondents reported dietary data for children ages 5 and younger and for all children regardless of age who cannot self-report. All recalled foods were coded by NHANES staff using the USDA Food and Nutrient Database for Dietary Studies (Blanton et al. 2006; Conway et al. 2003; Moshfegh et al. 2008).
We analyzed two dimensions of children’s diets. Diet Americanization was measured using the food similarity index (FSI), a measure developed and validated in previous research (Van Hook et al. 2015). The FSI indicates the similarity of the foods consumed by individuals to the foods most commonly consumed by same-aged U.S-born peers. Briefly, we used dietary recall data from U.S.-born children of natives ages 5–9, 10–14, and 15–19 to assign each USDA 5-digit food category rank scores indicating the popularity of each food category for each age group, ranked according to the proportion of these children that consumed the food (1 = most commonly consumed food, 2 = 2nd most commonly consumed food, etc.). We next assigned the children in our sample the age-appropriate mean rank score averaged across all foods they consumed across the two dietary recall days. Finally, we transformed this score for interpretability. It was reverse-scored so that higher values indicated greater food similarity and then converted to a percentile normed against same-aged children of natives. Thus, an FSI value of 50 indicates that a child’s diet was as American as the median among children of natives in his/her age group.
Diet quality was measured using the 2010 healthy eating index (HEI), which is a validated scale ranging from 1 to 100 indicating the degree to which children’s reported intake conforms to the guidelines recommended by the Center for Nutrition Policy and Promotion (CNPP) issued through the Department of Agriculture (USDA) and the Department of Health and Human Services (DHS) (Guenther et al. 2014). We used SAS code provided by the National Cancer Institute through the U.S. National Institutes of Health (http://riskfactor.cancer.gov/tools/hei/tools.html) to construct the HEI-2010 index for dietary recall days for all children in the sample.
Generational Status was measured with a dichotomous variable indicating whether Mexican-origin children have immigrant parents or U.S. native-born parents (=1). In supplementary analyses, we further classified children as immigrant children (1st generation), U.S. born children of immigrants (2nd generation), and U.S. born children of U.S. born parents (3rd + generation), but we included 1st and 2nd generation children in the same category because results were statistically and substantively similar for them.
Acculturation was tapped using several neighborhood-level and family-level variables. At the neighborhood level, we measured the percentage of U.S.-born individuals in the census tract (obtained from the Census/ACS data), and the average food similarity index score (FSI) among persons of all ages in the child’s census tract (aggregated up from the NHANES data). We did not include the respondent in the calculation of the neighborhood average FSI. At the family/household level, the language of the family interview (English = 1) tapped the extent that children and their parents may be able to interact with and are likely to be influenced by U.S. media, entertainment, friends, teachers, co-workers, and neighbors. The proportion of food eaten away from home indicated the extent children were exposed to U.S. eating behaviors and foods outside of the household. Finally, the number of hours per week children spend watching television or on the computer measured the extent children were exposed to U.S. media and advertising.
Structural Incorporation was measured with three indicators of neighborhood-level and family-level socioeconomic status. Neighborhood advantage was a reverse-coded factor score of the percentage of persons in the census tract with family incomes below the poverty threshold, the percentage on public assistance, the percentage of female-headed households, and the percentage unemployed. These variables explained 65 % of the variance in the one underlying factor. Sampson et al.’s (1997) original index included two additional variables—the percentage younger than 18 and the percentage black—but these did not load highly with the underlying factor so we excluded them. At the family level, we used the householder’s educational attainment (less than 9th grade, 9th to 11th grade, high school graduate, some college or more) and family income-to-poverty ratio, the ratio of the child’s family income to the inflation-adjusted national poverty threshold given family’s size and age composition.
Control variables included the child’s age (5–11, 12–15, 16–19), gender (girl = 1), region (northeast, south, midwest, and west), their neighborhood’s average HEI score (aggregated up from all NHANES respondents in the census tract), whether the child completed only one or both days of dietary recall (both days = 1), and whether the two dietary recalls occurred on 0, 1, or 2 school days. We originally included additional controls—the householder’s age and marital status—but dropped them because they were not significantly related to the diet outcomes.
Data Analysis
All analyses were conducted using Stata 14.0. Missing values on analytical variables were multiply imputed.2 The procedure iteratively replaced missing values on all variables with predictions based on random draws from the posterior distributions of parameters observed in the sample, creating multiple complete data sets (Acock 2005). We averaged empirical results across ten imputation samples and account for random variation across samples to calculate standard errors (Royston 2005; Rubin 1987). All estimates were adjusted to account for the clustered and stratified NHANES sample design.
We first produced descriptive statistics. They describe the two groups of Mexican-origin children in the sample and show mean differences in how Americanized their diets are, how healthy their diets are, and indicators of acculturation and structural incorporation (Table 2).
Table 2.
Average diet (HEI and FSI), acculturation, structural incorporation, and other characteristics of Mexican-origin children of immigrants and children of natives (weighted percentage or mean)
| Children of immigrants | Children of natives | Difference | |
|---|---|---|---|
| Diet | |||
| Americanized eating (food similarity index) | 40.3 | 49.4 | 9.1*** |
| Healthy eating (HEI-2010) | 46.9 | 43.7 | −3.2*** |
| Acculturation | |||
| % U.S.-born in census tract | 71.8 | 79.4 | 7.6*** |
| Average FSI in census tract | 39.8 | 44.4 | 4.6*** |
| English interview (%) | 51.0 | 94.7 | 43.7*** |
| Proportion of food eaten away from home | 0.30 | 0.39 | 0.09*** |
| TV/computer hours | 5.1 | 4.4 | −0.6*** |
| Structural incorporation | |||
| Neighborhood advantage | −0.32 | −0.10 | 0.22** |
| Householder’s education (%) | |||
| <9th grade | 46.8 | 6.5 | −40.3*** |
| 9th–11th grade | 24.9 | 24.6 | −0.3 |
| HS graduate | 15.7 | 28.2 | 12.5*** |
| Some college+ | 12.7 | 40.7 | 28.0*** |
| Income-to-poverty ratio | 1.29 | 2.09 | 0.8*** |
| Control variables | |||
| Child’s age (%) | |||
| 5–11 | 50.3 | 51.6 | 1.3 |
| 12–15 | 25.4 | 26.0 | 0.7 |
| 16–19 | 24.3 | 22.4 | −1.9 |
| Female (%) | 47.3 | 50.7 | 3.4* |
| U.S. region (%) | |||
| Northeast | 1.9 | 0.7 | −1.2 |
| Midwest | 9.3 | 9.5 | 0.2 |
| South | 36.9 | 39.0 | 2.2 |
| West | 52.0 | 50.7 | −1.2 |
| Average HEI in census tract | 49.9 | 48.6 | −1.4*** |
| Completed both days of dietary recall (%) | 57.4 | 51.7 | −5.7 |
| School days (range 0–2) | 0.4 | 0.4 | 0.0 |
| N | 3960 | 2204 |
Source NHANES 1999/00–2009/10. Sample Mexican-origin children ages 5–19 (N = 6164), missing data are multiply imputed, and estimates are weighted
p < .001;
p < .01;
p < .05
We next tested our research expectations summarized in Table 1 concerning the individual-level relationships between acculturation, structural incorporation and diet by estimating weighted hierarchical linear models with children (level 1) nested within census tracts (level 2).3 We present two models for each outcome (Table 3). The first shows the bivariate relationships separately estimated between each independent variable and the outcomes. The second includes all of the independent variables together.
Table 3.
Hierarchical linear models of Americanized eating (FSI) and healthy eating (HEI) for Mexican-origin children
| Americanized eating (FSI)
|
Healthy eating (HEI-2010)
|
|||
|---|---|---|---|---|
| Model 1 (Bivariate) |
Model 2 | Model 1 (Bivariate) |
Model 2 | |
| Children of natives | 8.86*** | 6.64*** | −2.94*** | −2.16*** |
| Acculturation | ||||
| % U.S.-born in census tract | 0.19*** | 0.06* | −0.07*** | −0.03* |
| Average FSI in census tract | 0.31*** | 0.24*** | 0.00 | 0.03* |
| English interview | 6.02*** | 3.67** | −3.82*** | −1.42** |
| Food eaten away from home | 7.67*** | 5.68*** | −5.03*** | −4.29*** |
| TV/computer hours | 0.19 | 0.29* | −0.08 | −0.18** |
| Structural incorporation | ||||
| Neighborhood advantage | 1.70** | 0.65 | −0.18 | 0.01 |
| Householder’s education (Ref ≤ 9th grade) | ||||
| 9th–11th grade | 4.08*** | 1.30 | −0.47 | 0.31 |
| HS grad | 4.50*** | 0.72 | −1.08 | 0.15 |
| Some college+ | 6.03*** | 0.75 | −0.25 | 1.10* |
| Income-to-poverty ratio | 0.88* | −0.65 | −0.32* | 0.00 |
| Control variables | ||||
| Child’s age (Ref = 5–11) | ||||
| 12–15 | 5.03*** | 4.90*** | −2.82*** | −2.78*** |
| 16–19 | 2.48** | 1.63 | −3.00*** | −2.96*** |
| Female | −4.57*** | −4.76*** | 1.08*** | 1.01** |
| U.S. region | ||||
| Midwest | 0.49 | −3.28 | −3.36 | −1.65 |
| South | 1.35 | −1.88 | −3.49* | −1.02 |
| West | −1.60 | −3.94 | −1.80 | −0.08 |
| Average HEI in census tract | −0.11 | 0.19* | 0.34*** | 0.26*** |
| Completed both days of dietary recall | 1.62 | 2.70** | 3.62*** | 3.27*** |
| School days | −1.72* | −1.64* | −0.47 | −1.68*** |
| Intercept | 14.06* | 38.12*** | ||
| N | 6164 | 6164 | 6164 | 6164 |
Source NHANES 1999/00–2009/10. Sample Mexican-origin children ages 5–19 (N = 6164), missing data are multiply imputed. Models are weighted
p < .001;
p < .01;
p < .05
We also tested the three alternative hypotheses about how the relative balance of structural incorporation and acculturation among children of Mexican natives may produce more Americanized diets, and higher, lower, or similar quality diets as children of immigrants. To do this, we employed regression decomposition techniques (Jann 2008), which estimated the degree that generational differences in Americanized diet and diet quality can be explained by generational differences in acculturation and structural incorporation. We decomposed differences between the children of immigrants and children of natives in mean FSI and mean HEI-2010. The generational difference in FSI can be expressed as a function of differences in acculturation and structural incorporation as follows:
where the superscripts 1 and 2 indicate children of immigrants and children of natives, respectively, are the coefficients related to acculturation, are the coefficients related to structural incorporation, are all other coefficients, and the are the mean values for each variable by generation. The first term on the right-hand side of the equation is the difference due to mean differences in acculturation, the second is the difference due to mean differences in structural incorporation, and the third is the remaining difference.
There are multiple decomposition methods that differ in how to treat the coefficients (e.g., by using “pooled” coefficients estimated on both groups; by averaging coefficients for the two groups; and by using the coefficients estimated on only one of the groups). We tried all variations and obtained similar results. We ultimately presented the average of the coefficients for simplicity (Table 4).
Table 4.
Decomposition of differences in Americanized and healthy eating between children of immigrants and children of natives
| Americanized eating (FSI) | Healthy eating (HEI-2010) | |
|---|---|---|
| Children of natives (mean) | 49.43 | 43.71 |
| Children of immigrants (mean) | 40.28 | 46.94 |
| Difference | 9.15*** | −3.23*** |
| Difference due to compositional differences in | ||
| Acculturation | 3.40*** | −1.86*** |
| % U.S.-born in census tract | 0.36 | −0.26* |
| Average FSI in census tract | 1.30*** | 0.12 |
| English interview | 1.48* | −1.46*** |
| Food eaten away from home | 0.46*** | −0.37*** |
| TV/computer hours | −0.19+ | 0.12* |
| Structural incorporation | 0.21 | 0.48+ |
| Neighborhood advantage | 0.15 | 0.04 |
| Education | 0.46 | 0.45* |
| Income-to-poverty ratio | −0.41 | −0.01 |
| Controls | −0.51* | −0.52** |
| Age | 0.00 | 0.04 |
| Gender | −0.16* | 0.04+ |
| Region | 0.03 | −0.04 |
| Average HEI in census tract | −0.22 | −0.39*** |
| Completed both days | −0.16 | −0.17+ |
| School days | 0.05 | 0.05 |
| Total explained | 3.14*** | −1.85*** |
Source NHANES 1999/00–2009/10. Sample Mexican-origin children ages 5–19 (N = 6164), missing data are multiply imputed. Estimates are weighted
p < .001;
p < .01;
p < .05;
p < .10
Results
As shown in Table 2, the degree that Mexican-origin children consumed an Americanized diet differed dramatically across generations. The average FSI was nearly 10 points higher among children of natives (49.4) than children of immigrants (40.3). This difference was paralleled by moderately lower diet quality (HEI-2010) among children of natives (43.7) than children of immigrants (46.9).
We also observed large generational differences in acculturation. Consistent with prior research on spatial assimilation, children of natives tended to live in neighborhoods with a higher proportion of U.S.-born residents and where people ate more Americanized diets than children of immigrants. Additionally, nearly all of the family interviews for children of natives were conducted in English (94.7 %) compared with roughly half among children of immigrants. Children of natives also ate more food away from home but spent slightly less time (by about half an hour per week) watching television or on the computer than children of immigrants.
Table 2 also shows large generational differences in structural incorporation. Children of natives lived in more advantaged neighborhoods. Additionally, children of natives had householders with much higher levels of education (e.g., 40.7 % had attended college or more compared with 12.7 % of children of immigrants) and higher family incomes relative to the poverty threshold.
Acculturation, Structural Incorporation, and Mexican-Origin Children’s Diets
We next show results from models estimating how indicators of acculturation and structural incorporation are associated with how Americanized and healthy all Mexican-origin children’s diets are (Table 3). We begin by describing the bivariate associations in the first and third column of results. As expected, nearly all of the acculturation indicators (except television/computer hours) and all of the structural incorporation indicators were positively associated with eating an Americanized diet (FSI). Additionally, three indicators of acculturation—percentage U.S.-born in the census tract, English interview, and food eaten away from home—were negatively associated with healthy eating (HEI). But unexpectedly, parental education was unassociated with children’s HEI, and the income-to-poverty ratio was negatively associated with HEI.
The full multivariate models are shown in Model 2 (columns 2 and 4). The indicators of acculturation remained significant predictors of diet Americanization, while the structural incorporation indicators did not (column 2). Living in a census tract with more U.S.-born residents and where residents have more Americanized diets, an English language interview, eating away from home and more TV/computer time were all positively associated eating an Americanized diet.
Most of the indicators of acculturation—living in a census tract with more U.S.-born residents, an English language interview, eating food away from home, and TV/computer time—also remained significant predictors of unhealthy eating (column 4). One exception was that living in a neighborhood with a higher average FSI was associated with healthier eating, although the coefficient was small in magnitude. This finding is consistent with the mixed findings in the literature about how acculturation is related to healthy eating. Among the structural incorporation indicators, only having a parent with some college education was associated with healthier eating.
In supplementary models (available upon request), we estimated whether the predicted effects of acculturation were moderated by generational status. They were not. They were equally important predictors for all Mexican-origin children.
Explaining Differences in Diet between Children of Immigrants and Children of Natives
The results just presented suggest that acculturation predicts Americanized diets for Mexican-origin children and most indicators of acculturation also predict unhealthy eating. Conversely, structural incorporation is not associated with diet Americanization, but one indicator—parental educational attainment—has a significant effect on healthy eating. However, these findings do not show how generational differences in incorporation and acculturation produce generational differences in diet Americanization and diet quality. For example, a far greater share of children of natives versus immigrants have parents with some college education (40.7 vs. 12.7 %). This could have important implications for group differences in healthy eating.
Thus, in Table 4, we show the results from the decomposition analyses. These findings suggest that generational differences in acculturation explain much of the generational differences in children’s diets, but that structural incorporation slightly offsets this process in the case of diet quality.
Focusing first on the food similarity index (FSI; first column), the overall generational difference in FSI was 9.15 points. Generational differences in the acculturation indicators explained 3.40 points (37 %) of this difference. Of these factors, the spatial assimilation of children of natives to neighborhoods with more U.S.-born residents and residents with a higher average FSI accounted for a large share, a total of 1.66 points (.36 + 1.30) or 18 %. Generational differences in English language of interview also accounted for a large share (1.48 points or 16 %). Generational differences in food eaten away from home accounted for a small share of the difference (.46 points; 5 %).
Generational differences in structural incorporation did not offset the effects of acculturation on group differences in FSI. In fact, this factor was associated with a small and insignificant increase in FSI of about one-fifth of a point (.21). Overall, acculturation alone drives the generational difference in how Americanized children’ diets are.
Turning to diet quality (HEI-2010, 2nd column), children of natives had lower average HEI-2010 scores than children of immigrants (−3.23 points). This difference was largely explained by generational differences in acculturation (−1.86 points, or 57 % of the total difference in HEI-2010). The higher percentage of children of natives that used English (−1.46 points, or 45 %), ate food away from home (−.37 points, or 12 %), and residence in non-immigrant neighborhoods (−.26 points, or 8 %) accounted for much of this. Structural incorporation offset these generational declines in dietary quality by 0.48 points (15 %). This was almost fully due to generational increases in parental educational attainment. This suggests that if Mexican-original children did not become more socially integrated across generations, their diet quality would slightly improve due to rising parental education across generations.
Discussion
Adapting to life in the U.S. has many benefits including increases in social and economic status. Unfortunately, the loss of cultural traditions and practices in everyday life come with costs to health generally (Abraído-Lanza et al. 2006), and to diet that increases their risk of obesity and eventual obesity-related morbidity.
Our analyses estimated how indicators of acculturation and structural incorporation are associated with how Americanized and healthy Mexican-origin children’s diets are. Results from these analyses suggested that generational status was strongly associated with eating American foods and lower diet quality independent of the measures of acculturation, structural incorporation, and confounders. Although our data are cross-sectional and do not track real generational change, the results suggest that dietary acculturation proceeds with time in the U.S., and that this results in the adoption of diets that are consistent with the hard to resist default American lifestyle (Mirowsky and Ross 2010).
Our analysis also indicated that acculturation has a large and important role in Americanizing Mexican-origin children’s diets and in unhealthy eating. Net of controls, nearly every measure of acculturation predicted an Americanized diet and unhealthy eating. In contrast, indicators of structural incorporation were largely unassociated with how Americanized and healthy children’s diets were, net of other variables in the full models. Neighborhood advantage was never a significant predictor of diet net of family socioeconomic status, even in supplementary models where we removed the other neighborhood measures to ensure that this null finding was not a result of collinearity. Only having a parent with some college education predicted diet quality, which is consistent with prior research on education and health (Baker et al. 2011; Freese and Lutfey 2011), and Mexican-origin children’s healthy eating (Martin et al. 2015).
Moreover, the decomposition results underscored the importance of acculturation for understanding population-level differences in diet across generations. The decomposition results show that differences in Americanized diets and diet quality between Mexican-origin children of immigrants and children of natives are driven by acculturation at all levels—individual, family, and neighborhood—and that the generational decline in diet quality is offset only slightly by family-level socioeconomic advantages among the children of natives. In other words, upward mobility is not sufficiently common among Mexican-origin children of natives to outweigh the unhealthy effects of their greater acculturation. This is consistent with the “negative assimilation” pattern depicted in the first three bars in Fig. 1.
In supplementary analyses, we explored whether this general depiction of generational change in diet was equally applicable to children in different age groups. They were, but acculturation played a weaker role in generational differences in diet Americanization among adolescents, perhaps because our models were not able to account for school and peer effects. However, the results on diet quality were consistent with “downward assimilation” regardless of age. Overall, the results suggest that the focus in prior research on acculturation among Mexican-origin children is largely justified for understanding dietary change.
The contrast in findings for the two diet outcomes also confirmed our premise that diet Americanization is not the same as adopting an unhealthy diet. For example, only healthy eating was tied to structural incorporation. Gordon (1964) once observed that the acculturation of some U.S. behaviors (such as English language usage) occurs rapidly and universally, while acculturation along other dimensions takes longer (if at all) because it depends on the group’s treatment as equals in the host society. Adopting an American diet may be as likely as English language acquisition. It may be very difficult for immigrant parents of all socioeconomic statuses to prevent their children from adopting an American diet, especially once they start attending school, because U.S. food is so widespread and becoming increasingly homogenized. However, healthy eating may be different. It may vary more widely across social strata for many of the reasons discussed earlier.
Another example of how diet Americanization is not the same as unhealthy eating is that living in a neighborhood where other residents eat Americanized food was associated with both Americanized and healthier diets among Mexican-origin children. One possible explanation is that, other things equal, having neighbors who eat Americanized food exposes Mexican-origin families to American ways of thinking about nutrition and health. Although the average American diet is not healthy, thinness and restrained eating is a marker of status in the contemporary United States, particularly among white women (Cawley 2004; Flegal et al. 2010; McLaren 2007; Sobal and Stunkard 1989), and one study found that Americans are more likely than their counterparts in Japan, Belgium, and France to believe that food is linked to health (Rozin et al. 1999).
This study has limitations. Although the NHANES data provide greater detail on children’s diets than any other national-level dataset available, and the restricted version of the data permits us to examine the relationship between neighborhood contexts and children’s eating behaviors, the NHANES has important drawbacks. First, children’s dietary recalls are unlikely to be completely accurate (Dhurandhar et al. 2014). However, given that we are more interested in the types of foods children eat and less interested in their quantities or macronutrient components, reporting accuracy may be less problematic. Additionally, although the HEI has been validated (Guenther et al. 2014), it has not been validated specifically for children. Further, the data do not permit us to identify the school district or the school characteristics for children. Our analyses therefore omit an important acculturating context for Mexican-origin children, particularly for the older children in our sample. Finally, because the NHANES does not collect data from all household members and provides very limited information on household composition, we were unable to measure children’s household and family contexts in as much detail as would be ideal. For example, we do not know the ethnic origins or nativity of children’s household members. This is unfortunate given the moderately high rates of intermarriage observed among Hispanics (Lee and Bean 2010). We suspect that children who live in mixed-origin households (e.g., with mixed-ethnic origin parents or grandparents) may be more likely to eat acculturated foods, but we were unable to test this idea.
We conclude with a brief reflection on the study’s policy implications. The results reinforce the notion that acculturation is central for understanding Mexican-origin children’s dietary change. In the current American context, it may be very difficult to prevent children from adopting an American diet. Therefore, in developing interventions, it is probably important to recognize that the Americanization of children’s diet is not synonymous with reductions in diet quality. The fact that parental educational attainment was related to better diet quality but not a less Americanized diet suggests that there may exist a more benign acculturation pathway for Mexican-origin children that could be reinforced among middle- and lower SES children. As some public health advocates have called for (Aldrich and Variyam 2000; Ayala et al. 2008), interventions that help Mexican-origin children improve diet quality while working within their culinary preferences (whether American, Mexican, or some other tradition) may be more effective than attempting to halt dietary acculturation altogether.
Acknowledgments
This research was supported by grants from the National Institutes of Health (R24 HD041025 and P01 HD062498).
Footnotes
Results were consistent when we relied only on day 1 dietary recall measures.
We obtained very similar results when we did not impute missing values.
Prior to this step, we estimated a series of models that included various combinations of the neighborhood characteristics to assess the level of collinearity among them. We tested multiple measures of neighborhood disadvantage (e.g., poverty level, the percentage with less than a high school education, and the composite measure, neighborhood disadvantage), ethnic and immigrant composition (the percentages Hispanic, foreign-born, Mexican foreign-born, foreign-born that arrived after 1990, non-Hispanic white, and non-Hispanic black). Neighborhood ethnic/immigrant composition and neighborhood disadvantage operated independently but the indicators within these clusters of variables were highly correlated, so we selected the indicators with the strongest relationship with the outcomes—the composite measure of neighborhood disadvantage and the percentage foreign-born—for our final models.
References
- Abraído-Lanza AF, Armbrister AN, Flórez KR, Aguirre AN. Toward a theory-driven model of acculturation in public health research. American Journal of Public Health. 2006;96:1342–1346. doi: 10.2105/AJPH.2005.064980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acevedo-Garcia D, Bates LM. Latino health paradoxes: Empirical evidence, explanations, future research, and implications. In: Rodríguez H, Sáenz R, Menjívar C, editors. Latinas/os in the United States: Changing the face of America. New York: Springer; 2008. pp. 101–113. [Google Scholar]
- Acock AC. Working with missing values. Journal of Marriage and Family. 2005;67:1012–1028. [Google Scholar]
- Akresh IR. Dietary assimilation and health among Hispanic immigrants to the United States. Journal of Health and Social Behavior. 2007;48(4):404–417. doi: 10.1177/002214650704800405. [DOI] [PubMed] [Google Scholar]
- Aldrich L, Variyam JN. Acculturation erodes the diet quality of U.S. Hispanics. Diet Quality. 2000;23:51–55. [Google Scholar]
- Ayala GX, Baquero B, Klinger S. A systematic review of the relationship between acculturation and diet among Latinos in the United States: Implications for future research. Journal of the American Dietetic Association. 2008;108:1330–1344. doi: 10.1016/j.jada.2008.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DP, Leon J, Smith Greenaway EG, Collins J, Movit M. The education effect on population health: A reassessment. Population and Development Review. 2011;37(2):307–332. doi: 10.1111/j.1728-4457.2011.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balistreri KS, Van Hook J. Socioeconomic status and body mass index among Hispanic children of immigrants and children of natives. American Journal of Public Health. 2009;99:2238–2246. doi: 10.2105/AJPH.2007.116103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batis C, Hernandez-Barrera L, Barquera S, Rivera JA, Popkin BM. Food acculturation drives dietary differences among Mexicans, Mexican Americans, and non-Hispanic Whites. The Journal of nutrition. 2011;141(10):1–9. doi: 10.3945/jn.111.141473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bean F, Stevens G. America’s newcomers and the dynamics of diversity. New York: Russell Sage Foundation; 2003. [Google Scholar]
- Birch LL. Development of food preferences. Annual Review of Nutrition. 1999;19(1):41–62. doi: 10.1146/annurev.nutr.19.1.41. [DOI] [PubMed] [Google Scholar]
- Birch LL, Fischer JO. Development of eating behaviors among children and adolescents. Pediatrics. 1998;101(3):539–549. [PubMed] [Google Scholar]
- Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA automated multiple-pass method accurately estimates group total energy and nutrient intake. The Journal of nutrition. 2006;136(10):2594–2599. doi: 10.1093/jn/136.10.2594. [DOI] [PubMed] [Google Scholar]
- Brown D. Dietary challenges of new Americans. Journal of the American Dietetic Association. 2005;105(1704):1706. doi: 10.1016/j.jada.2005.09.013. [DOI] [PubMed] [Google Scholar]
- Carrera PM, Gao X, Tucker KL. A study of dietary patterns in the Mexican-American population and their association with obesity. Journal of the American Dietetic Association. 2007;107:1735–1742. doi: 10.1016/j.jada.2007.07.016. [DOI] [PubMed] [Google Scholar]
- Cawley J. The impact of obesity on wages. Journal of Human resources. 2004;39(2):451–474. [Google Scholar]
- Chaparro M, Langellier B, Wang M, Koleilat M, Whaley S. Effects of parental nativity and length of stay in the US on fruit and vegetable intake among WIC-enrolled preschool-aged children. Journal of Immigrant and Minority Health. 2015;17(2):333–338. doi: 10.1007/s10903-014-0097-5. [DOI] [PubMed] [Google Scholar]
- Conway JM, Ingwersen LA, Vinyard BT, Moshfegh AJ. Effectiveness of the US Department of Agriculture 5-step multiple-pass method in assessing food intake in obese and nonobese women. The American Journal of Clinical Nutrition. 2003;77(5):1171–1178. doi: 10.1093/ajcn/77.5.1171. [DOI] [PubMed] [Google Scholar]
- Dhurandhar N, Schoeller D, Brown A, Heymsfield S, Thomas D, Sørensen T, et al. Energy balance measurement: When something is not betterthan nothing. International Journal of Obesity. 2014;2014:1–5. [Google Scholar]
- Dixon LB, Sundquist J, Winkleby M. Differences in energy, nutrient, and food intakes in a US sample of Mexican-American women and men: Findings from the Third National Health and Nutrition Examination Survey, 1988–1994. American Journal of Epidemiology. 2000;152:548–557. doi: 10.1093/aje/152.6.548. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. The economics of food choice behavior: Why poverty and obesity are linked. Nestlé Nutrition Institute workshop series. 2012;73:95–112. doi: 10.1159/000341303. [DOI] [PubMed] [Google Scholar]
- Dubowitz T, Heron M, Bird CE, Lurie N, Finch BK, Basurto-Dávila R, et al. Neighborhood socioeconomic status and fruit and vegetable intake among whites, blacks, and Mexican Americans in the United States. The American journal of clinical nutrition. 2008a;87:1883–1891. doi: 10.1093/ajcn/87.6.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz T, Subramanian SV, Acevedo-Garcia D, Osypuk TL, Peterson KE. Individual and neighborhood differences in diet among low-income foreign and U.S.-born women. Women’s health issues: Official publication of the Jacobs Institute of Women’s Health. 2008b;18:181–190. doi: 10.1016/j.whi.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duffey KJ, Gordon-Larsen P, Ayala GX, Popkin BM. Birthplace is associated with more adverse dietary Profiles for US-born than for foreign-born Latino adults. The Journal of Nutrition. 2008;138:2428–2435. doi: 10.3945/jn.108.097105. [DOI] [PubMed] [Google Scholar]
- Edmonds VM. The nutritional patterns of recently immigrated Honduran women. Journal of Transcultural Nursing: Official Journal of the Transcultural Nursing Society/Transcultural Nursing Society. 2005;16:226–235. doi: 10.1177/1043659605274959. [DOI] [PubMed] [Google Scholar]
- Erinosho TO, Berrigan D, Thompson FE, Moser RP, Nebeling LC, Yaroch AL. Dietary intakes of preschool-aged children in relation to caregivers’ race/ethnicity, acculturation, and demographic characteristics: Results from the 2007 California Health Interview Survey. Maternal and child health journal. 2012;16(9):1844–1853. doi: 10.1007/s10995-011-0931-5. [DOI] [PubMed] [Google Scholar]
- Flegal K, Caroll M, Ogden C. Prevalence and trends in obesity among US adults, 1999–2008. Journal of the American Medical Association. 2010;303(3):235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- Freese J, Lutfey K. Fundamental causality: Challenges of an animating concept for medical sociology. In: Pescosolido B, Martin J, McLeod J, Rogers A, editors. The handbook of the sociology of health, illness, and healing. New York: Springer; 2011. pp. 67–81. [Google Scholar]
- Gordon MM. Assimilation in American life. Oxford University Press; 1964. [Google Scholar]
- Gordon-Larsen P, Harris K, Ward DS, Popkin BM. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: The National Longitudinal Study of Adolescent Health. Social Science and Medicine. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Guendelman S, Abrams B. Dietary intake among Mexican-American women: Generational differences and a comparison with white non-Hispanic women. American Journal of Public Health. 1995;85:20–25. doi: 10.2105/ajph.85.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guendelman MD, Cheryan S, Monin B. Fitting in but getting fat identity threat and dietary choices among us immigrant groups. Psychological Science. 2011;22(7):959–967. doi: 10.1177/0956797611411585. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Casavale KO, Reedy J, Kirkpatrick SI, Hiza HAB, Kuczynski KJ, Krebs-Smith SM. Update of the healthy eating index: HEI-2010. Journal of the Academy of Nutrition and Dietetics. 2013;113(4):569–580. doi: 10.1016/j.jand.2012.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenther PM, Kirkpatrick SI, Reedy J, Krebs-Smith SM, Buckman DW, Dodd KW, et al. The healthy eating index-2010 is a valid and reliable measure of diet quality according to the 2010 dietary guidelines for Americans. The Journal of nutrition. 2014 doi: 10.3945/jn.113.183079. jn. 113.183079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiza HB, Casavale KO, Guenther PM, Davis C. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level. Journal of the Academy of Nutrition and Dietetics. 2013;113(2):297–306. doi: 10.1016/j.jand.2012.08.011. [DOI] [PubMed] [Google Scholar]
- Hunt LM, Schneider S, Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Social Science and Medicine. 2004;59(5):973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Jann B. The Blinder-Oaxaca decomposition for linear regression models. The Stata Journal. 2008;4:453–479. [Google Scholar]
- Kaiser LL, Aguilera AL, Horowitz M, Lamp C, Johns M, Gomez-Camacho R, Ontai L, de la Torre A. Correlates of food patterns in young Latino children at high risk of obesity. Public health nutrition. 2015:1–9. doi: 10.1017/S1368980014003309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keita AD, Casazza K, Thomas O, Fernandez JR. Neighborhood-level disadvantage is associated with reduced dietary quality in children. Journal of the American Dietetic Association. 2009;109:1612–1616. doi: 10.1016/j.jada.2009.06.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbro RT, Denney JT. Neighborhood context and racial/ethnic differences in young children’s obesity: Structural barriers to interventions. Social Science and Medicine (1982) 2013;95:97–105. doi: 10.1016/j.socscimed.2012.09.032. [DOI] [PubMed] [Google Scholar]
- Larson NI, Story MT, Nelson MC. Neighborhood environments: Disparities in access to healthy foods in the U.S. American Journal of Preventive Medicine. 2009;36:74–81. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- Lee J, Bean FD. The diversity paradox: Immigration and the color line in twenty-first century america. New York: Russell Sage Foundation; 2010. [Google Scholar]
- Lee J, Zhou M. The Asian American achievement paradox. New York: Russell Sage Foundation; 2015. [Google Scholar]
- Liu A, Berhane Z, Tseng M. Improved dietary variety and adequacy but lower dietary moderation with acculturation in Chinese women in the United States. Journal of the American Dietetic Association. 2010;110:457–462. doi: 10.1016/j.jada.2009.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin MA, Van Hook J, Quiros S. Is socioeconomic incorporation associated with a healthier diet? Dietary patterns among Mexican-origin children in the United States. Social Science and Medicine. 2015;147:20–29. doi: 10.1016/j.socscimed.2015.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiologic Reviews. 2007;28(1):29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Self-direction toward health: Overriding the default American lifestyle. In: Suls JM, Davidson KW, Kaplan RM, editors. Handbook of health psychology and behavioral medicine. New York: The Guilford Press; 2010. pp. 235–250. [Google Scholar]
- Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, et al. The US Department of Agriculture automated multiple-pass method reduces bias in the collection of energy intakes. The American Journal of Clinical Nutrition. 2008;88(2):324–332. doi: 10.1093/ajcn/88.2.324. [DOI] [PubMed] [Google Scholar]
- Myers D. Immigrants and boomers: Forging a new social contract for the future of America. New York: Russell Sage Foundation; 2007. [Google Scholar]
- Ogden CL, Caroll MD, Flegal KM, Kit B. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Kit BK, Carroll MD, Park S. Consumption of sugar drinks in the United States, 2005–2008. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2011. [Google Scholar]
- Osypuk TL, Diez Roux AV, Hadley C, Kandula NR. Are immigrant enclaves healthy places to live? The multi-ethnic study of atherosclerosis. Social Science and Medicine. 2009;69:110–120. doi: 10.1016/j.socscimed.2009.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park Y, Neckerman KM, Quinn J, Weiss C, Rundle A. Place of birth, duration of residence, neighborhood immigrant composition and body mass index in New York City. The International Journal of Behavioral Nutrition and Physical Activity. 2008;5:19. doi: 10.1186/1479-5868-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portes A. Social capital: Its origins and applications in modern sociology. Annual Review of Sociology. 1998;24:1–24. [Google Scholar]
- Portes A, Sensenbrenner J. Embeddedness and immigration: Notes on the social determinants of economic action. American Journal of Sociology. 1993;98(6):1320–1350. [Google Scholar]
- Portes A, Zhou M. The new second generation: Segmented assimilation and its variants. The Annals of the American Academy of Political and Social Science. 1993;530:74–96. [Google Scholar]
- Reyes-Ortiz CA, Ju H, Eschbach K, Kuo YF, Goodwin JS. Neighbourhood ethnic composition and diet among Mexican-Americans. Public Health Nutrition. 2009;12:2293–2301. doi: 10.1017/S1368980009005047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivera JA, Irizarry LM, González-de Cossío T. Overview of the nutritional status of the Mexican population in the last two decades. Salud pública de México. 2009;51(Suppl 4):S645–S656. doi: 10.1590/s0036-36342009001000020. [DOI] [PubMed] [Google Scholar]
- Royston P. Multiple imputation of missing values: Update. The Stata Journal. 2005;5(2):1–14. [Google Scholar]
- Rozin P, Fischler C, Imada S, Sarubin A, Wrzesniewski A. Attitudes to food and the role of food in life in the U.S.A., Japan, Flemish Belgium and France: Possible implications for the diet-health debate. Appetite. 1999;33(2):163–180. doi: 10.1006/appe.1999.0244. [DOI] [PubMed] [Google Scholar]
- Rubin D. Multiple imputation for non-response in surveys. New York, NY: Wiley; 1987. [Google Scholar]
- Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. Science. 1997;277(5328):918–924. doi: 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- Satia-Abouta J, Patterson RE, Neuhouser ML, Elder J. Dietary acculturation: Applications to nutrition research and dietetics. Journal of the American Dietetic Association. 2002;102:1105–1118. doi: 10.1016/s0002-8223(02)90247-6. [DOI] [PubMed] [Google Scholar]
- Sobal J, Stunkard AJ. Socioeconomic status and obesity: A review of the literature. Psychological Bulletin. 1989;105:260–275. doi: 10.1037/0033-2909.105.2.260. [DOI] [PubMed] [Google Scholar]
- South S, Crowder K, Chavez E. Migration and spatial assimilation among U.S. Latinos: Classical versus segmented trajectories. Demography. 2005a;42(3):497–521. doi: 10.1353/dem.2005.0025. [DOI] [PubMed] [Google Scholar]
- South SJ, Crowder K, Chavez E. Geographic mobility and spatial assimilation among U.S. Latino immigrants. International Migration Review. 2005b;39(3):577–607. [Google Scholar]
- Storey ML, Forshee RA, Anderson PA. Beverage consumption in the US population. Journal of the American Dietetic Association. 2006;106(12):1992–2000. doi: 10.1016/j.jada.2006.09.009. [DOI] [PubMed] [Google Scholar]
- Telles EE, Ortiz V. Generations of exclusion. New York: Russell Sage Foundation; 2008. [Google Scholar]
- Van Hook J, Baker E, Altman CE, Frisco M. Canaries in a coalmine: Immigration and overweight among Mexican-origin children in the US and Mexico. Social Science & Medicine. 2012;74:125–134. doi: 10.1016/j.socscimed.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hook J, Landale NS, Hillemeier MM. Is the United States bad for children’s health? In: Institute MP, editor. Risk and resiliance among young children of immigrants. Washington, D.C: Migration Policy Institute; 2013. [Google Scholar]
- Van Hook J, Quiros S, Frisco ML. The food similarity index: A new measure of dietary acculturation based on dietary recall data. Journal of Immigrant and Minority Health. 2015;17(2):441–449. doi: 10.1007/s10903-014-0107-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viruell-fuentes EA, Miranda PY, Abdulrahim S. Social science & medicine More than culture: Structural racism, intersectionality theory, and immigrant health. Social Science and Medicine. 2012;75:2099–2106. doi: 10.1016/j.socscimed.2011.12.037. [DOI] [PubMed] [Google Scholar]
- Waters MC. Ethnic options: Choosing ethnic identities in America. University of California Press; 1990. [Google Scholar]
- Wen M, Maloney TN. Latino residential isolation and the risk of obesity in Utah: The role of neighborhood socioeconomic, built-environmental, and subcultural context. Journal of Immigrant and Minority Health. 2011;13(6):1134–1141. doi: 10.1007/s10903-011-9439-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


