Abstract
Background
As an alternative to spinal fusion, non-fusion dynamic stabilization surgery has been developed, showing good clinical outcomes. In the present study, we introduce our surgical series, which involves non-fusion dynamic stabilization surgery for adjacent segment pathology (ASP) after lumbar fusion surgery.
Methods
Fifteen patients (13 female and 2 male, mean age of 62.1 years) who underwent dynamic stabilization surgery for symptomatic ASP were included and medical records, magnetic resonance images (MRI), and plain radiographs were retrospectively evaluated.
Results
Twelve of the 15 patients had the fusion segment at L4-5, and the most common segment affected by ASP was L3-4. The time interval between prior fusion and later non-fusion surgery was mean 67.0 months. The Visual Analog Scale and Oswestry Disability Index showed values of 7.4 and 58.5% before the non-fusion surgery and these values respectively declined to 4.2 and 41.3% postoperatively at 36 months (p=0.027 and p=0.018, respectively). During the mean 44.8 months of follow-up, medication of analgesics was also significantly reduced. The MRI grade for disc and central stenosis identified significant degeneration at L3-4, and similar disc degeneration from lateral radiographs was determined at L3-4 between before the prior fusion surgery and the later non-fusion surgery. After the non-fusion surgery, the L3-4 segment and the proximal segment of L2-3 were preserved in the disc, stenosis and facet joint whereas L1-2 showed disc degeneration on the last MRI (p=0.032). Five instances of radiologic ASP were identified, showing characteristic disc-space narrowing at the proximal segments of L1-2 and L2-3. However, no patient underwent additional surgery for ASP after non-fusion dynamic stabilization surgery.
Conclusion
The proposed non-fusion dynamic stabilization system could be an effective surgical treatment for elderly patients with symptomatic ASP after lumbar fusion.
Keywords: lumbar spine, Non-fusion, Dynamic stabilization system, Dynesys, NFlex, Adjacent segment pathology
Introduction
Since spinal fusion was introduced 100 years ago for the treatment of Pott's disease, fusion technologies have dramatically advanced, and indications for fusion surgery have expanded to the areas of the cervical, thoracic, and lumbosacral spine.1 Fusion rates have exceeded 95% with the recent developments in fusion techniques; however, a large discrepancy is noted between radiologically successful fusion and clinical success rates. As an undesirable effect of fusion, adjacent segment pathology (ASP) has been well described. Referred formerly adjacent segment degeneration and adjacent segment disease (ASD) as well as adjacent segment pathology (ASP) were recently proposed as terms with which to refer to clinical and/or radiological changes at adjacent segments subsequent to a previous spinal surgery.2 The incidence and reoperation rates of ASP after fusion surgery have ranged from 25% to 35% within a 10-year follow-up period.3 Due to the concern over the longevity of fusion constructs and the relatively high development of ASP, alternatives to spinal fusion have been developed with motion-preservation technology.
In 1994, Dubois et al. introduced the first pedicle-based dynamic stabilization system, Dynesys (Zimmer Spine, Minneapolis, USA). Several studies report that this system is an effective option in the treatment of lumbar degenerative disc disease, and indications for this system are expended with reference to spinal stenosis, spondylolisthesis and degenerative lumbar scoliosis.4–8 Currently, various types of dynamic stabilization systems are available.9
To date, there is no research on the application of a non-fusion pedicle-based dynamic stabilization system for ASP after lumbar fusion surgery. With regard to this application, degenerative changes between an earlier fusion surgery and a later non-fusion dynamic stabilization surgery and degeneration after non-fusion surgery should all be assessed. Hence, this study compared degenerative changes arising on the intervertebral disc, central canal, and facet joint in cases of prior fusion surgery, prior non-fusion surgery, and upon the last follow-up. The clinical outcomes and radiologic ASP findings were evaluated to determine the effectiveness of the application of non-fusion surgery for ASP.
Material and methods
Patient population
After the non-fusion dynamic stabilization system was procured by our institute in 2003, 108 patients underwent this type of surgery by a single surgeon as of the end of 2011. Of them, fifteen patients with symptomatic aggravation and radiologic confirmation of ASP after previous lumbar fusion surgery who had undergone the non-fusion dynamic stabilization surgery were included in the present study. Symptomatic patients with pseudarthrosis after fusion surgery, severe osteoporosis under medical treatment (<-2.5 T-score on the DEXA bone densitometry) were excluded.
Description of the dynamic stabilization system
Two types of pedicle-based dynamic stabilization systems were applied: the Dynesys system and the NFlex system (Synthes Spine, Inc.).
The Dynesys system is composed of titanium alloy pedicle screws, polyester cords, and polycarbonateurethane (PCU) spacers. It is fixed in place using standard pedicle screws made of a titanium alloy, and the entire system is stabilized by polyester cords that connect the screw heads through a hollow spacer and hold the screws in place.10
The NFlex system consists of polyaxial titanium alloy pedicle screws that are fixed to a semi-rigid polycarbonate urethane-sleeved rod. The integrated PCU spacer is surrounded by a central titanium ring, to which a pedicle screw is locked. The rod may be attached to pedicle screws in the standard fashion. The PCU spacer is not bonded to the titanium components of the rod. Therefore, when the pedicle-to-pedicle distances increases and decreases during the flexion and extension, the rod is able to elongate and compress to accommodate this change. It can also toggle to accommodate angulation.9
Surgical procedure
Reoperations were performed using previous midline incisions in a neutral prone position. After exposure of the previous fusion segment and index segment, manual distraction was undertaken to determine pseudarthrosis of the fusion segment. If gross motion was not observed, existing rods and screws from the fusion segment were removed, after which adjacent segments which were symptomatic were decompressed via hemilaminectomy or total laminectomy. Additional foraminal decompression also was performed in cases of foraminal stenosis. But additional discectomy was not performed even in combined with degenerative disc disease (DDD). During decompression, the integrity of the facet joint was carefully maintained for the non-fusion dynamic stabilization system. After adequate decompression, dynamic stabilization with Dynesys or NFlex was applied.
Clinical evaluation
Through patients’ medical records, pain was measured by the Visual Analog Scale (VAS, 0-10) and functional outcome was assessed by the Korean version of Oswestry Disability Index (ODI, 0-100%) excluding the item on sexual activity. Clinical parameters were measured before the non-fusion dynamic stabilization surgery and during every postoperative year. Clinical ASP was defined as a condition in which a patient was relieved of symptoms for at least six months after the non-fusion surgery, with newly developed symptoms later, which were compatible with the lesions in adjacent segments demonstrated in radiological images.11 In addition, medication via pain analgesics such as non-steroid anti-inflammatory drugs (NSAIDs) or Gabapentin was evaluated before the operation and upon the last follow-up.
Radiologic evaluation
Disc degeneration, central canal stenosis, and facet joint degeneration were graded on magnetic resonance images (MRI) before the initial fusion surgery, before the non-fusion dynamic stabilization surgery and in the last evaluated images. They were evaluated using the Pfirrmann disc degeneration grade system (grade, I-V), a new MRI grade for central canal stenosis (grade, 0-3) and in terms of the Weishaupt facet joint degeneration grade (grade, 0-3, Table 1).12–14 In addition, instances of disc degeneration from L1-2 to L5-S1 were sequentially evaluated on lateral radiographs (Table 2).15 The range of motion (ROM) calculated the difference between the flexion-extension dynamic radiographs at T12-S1 segments before and after non-fusion dynamic stabilization surgery. Radiologic ASP included disc space narrowing (>2mm loss of the posterior disc height), spur formation, spondylolisthesis (anterior or posterior slip of the vertebra by>2mm), and vacuum phenomenon, comparing each radiographs.16 Radiologic abnormalities such as a radiolucent line around the pedicle screw of the dynamic stabilization system and instrument failure such as a fracture of a screw or a rod were evaluated at each follow-up on plain radiographs. Radiologic data was investigated using a picture archiving and communication system (PACS, M-view, version 5.483, Infinitt Healthcare, Seoul, Korea).
Table 1.
MRI evaluation for disc degeneration, central stenosis, and facet joint degeneration.
| Classification of disc degeneration | |||
|---|---|---|---|
| Grade | Signal intensity | Structure | Distinction of nucleus and anulus |
| I | Hyperintense, isointense to CSF | Homogeneous, bright white | Clear |
| II | Hyperintense, isointense to CSF | Inhomogeneous with or without horizontal bands | Clear |
| III | Intermediate | Inhomogenous, gray | Unclear |
| IV | Intermediate to hypointense | Inhomogenous, gray to black | Lost |
| V | Hypointense | Inhomogenous, black | Lost |
| Classification of central canal stenosis | |||
| Grade | Definition | ||
| 0 | No lumbar stenosis without obliteration of anterior CSF space | ||
| 1 | Mild stenosis with separation of all cauda equina | ||
| 2 | Moderate stenosis with some cauda equine aggregated | ||
| 3 | Severe stenosis with none of the cauda equine separated | ||
| Classification of facet joint degeneration | |||
| Grade | Criteria | ||
| 0 | Normal facet joint space (2-4mm width) | ||
| 1 | Narrowing of the facet joint space (< 2mm) and/or small osteophyte and/or mild hypertrophy of the articular process | ||
| 2 | Narrowing of the facet joint space and/or moderate osteophyte and/or moderate hypertrophy of the articular process and/or mild subarticular bone erosions | ||
| 3 | Narrowing of the facet joint space and/or large osteophytes and/or severe hypertrophy of the articular process and/or severe subarticular bone erosions and/or subchondral cysts | ||
CSF: cerebrospinal fluid.
Table 2.
Grading of disc degeneration on plain radiograph
| Grade | Disc space narrowing | Osteophyte | Endplate sclerosis |
|---|---|---|---|
| I | - | - | - |
| II | + | - | - |
| III | ± | + | - |
| IV | ± | ± | + |
‘+’ indicates present; ‘-’, absence; ‘±’, either present or absent.
Statistical analysis
The Mann-Whitney test and Wilcoxon signed rank tests were used for continuous variables, and Fisher's exact test was used for categorical variables. Statistical significance was defined as a p-value of less than 0.05. Analyses were performed using SPSS version 19.0 software (IBM, Armonk, New York, USA).
Results
Fifteen patients who had previously undergone lumbar fusion surgery and then later underwent non-fusion dynamic stabilization surgery participated in this study. The gender distribution was thirteen females and two males, the mean age was 56.2 ± 6.9 years (range, 43-67) upon the prior fusion surgery, 62.1 ± 6.4 years (range, 46-70) upon the non-fusion surgery, and 68.5 ± 6.8 years (range, 52-77) at the final follow-up (Table 3). The previous fusion segment was mostly the L4-5-S1 (6, 40.0%) followed by L4-5 segment (5, 33.3%), L3-4 (2, 12.5%), L3-4-5 (1, 6.6%) and L2-3 (1, 6.6%). Primary pathology was lumbar spinal stenosis in all cases and it associated with DDD in six patients (40.0%) and degenerative spondylolisthesis in three patients (20.0%). The fusion technique was posterior lumbar interbody fusion (PLIF) with pedicle screw fixation (PSF) in nine patients (60.0%), PLIF without PSF in 4 (26.6%), PSF with posterolateral fusion (PLF) in 1 (6.6%), and anterior lumbar interbody fusion (ALIF) without PSF in 1 (6.6%). The mean pain-free period after fusion was 43.4 ± 30.3 months (range, 0-96), and the mean symptomatic period before non-fusion surgery was 38.1 ± 23.7 months (range, 2-84). Five patients complained about persistent symptoms after fusion surgery, and all patients had continued with their medical treatment, using on average 2.2 types of analgesics. Consequently, the time interval between the prior fusion surgery and the later non-fusion surgery was 67.0 ± 36.9 months (range, 6-120). As ten of the 15 patients showed ASP at L3-4, it was indicated as the most common proximal adjacent segment from previous fusion. The pathology of ASP was spinal stenosis in all cases, and it was associated with DDD (8, 53.3%) and spondylolisthesis (2, 13.3%). Non-fusion dynamic stabilization surgery was applied at L3-4 (7, 46.6%), L4-5 (3, 20.0%), L1-2-3 (1, 6.6%), L2-3-4 (1, 6.6%), L3-4-5 (1, 6.6%), L2-3-4-5 (1, 6.6%) and L2-3 (1, 6.6%). The Dynesys system (Figure 1) was used on eleven patients while the NFlex system (Figure 2) was used on four patients. Mean T-score at L1-4 on the DEXA bone densitometry was -0.5 ± 1.3 (range,-2.1 – 2.1).
Table 3.
Patient characteristics.
| No. | Gender | Age at fusion surgery (yrs) | Age at non-fusion surgery (yrs) | Previous fusion segment | Pain free period after fusion (m) | Interval between fusion and non-fusion surgery (m) | Feature of ASP | Recent non-fusion segment | Pedicle-based dynamic stabilization system | Clinical ASP after non-fusion surgery | Radiologic ASP after non-fusion surgery |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 49 | 59 | L3-4 | 72 | 120 | Stenosis at L4-5 DDD at L2-3, L4-5 | L4-5 | Dynesys | + | + |
| 2 | F | 60 | 67 | L4-5-S1 | Persistent pain | 84 | Stenosis & DDD at L3-4 | L3-4 | Dynesys | Persistent pain | + |
| 3 | F | 56 | 61 | L4-5-S1 | Persistent pain | 60 | Stenosis & DDD at L3-4 | L3-4 | Dynesys | Persistent pain | + |
| 4 | M | 63 | 68 | L4-5-S1 | 12 | 56 | Stenosis at L3-4 | L3-4 | Dynesys | - | - |
| 5 | F | 49 | 60 | L4-5 | 96 | 120 | Stenosis, DDD & SPL at L2-3-4 | L2-3-4-5 | Dynesys | Persistent pain | - |
| 6 | F | 56 | 61 | L3-4-5 | 36 | 60 | Stenosis at L2-3 | L2-3 | Dynesys | - | - |
| 7 | F | 61 | 63 | L4-5 | Persistent pain | 26 | Stenosis at L3-4-5 SPL at L4-5 | L3-4-5 | Dynesys | + | + |
| 8 | F | 48 | 59 | L4-5 | 48 | 120 | Stenosis & DDD at L3-4 | L3-4 | Dynesys | - | - |
| 9 | F | 62 | 70 | L4-5 | 82 | 94 | Stenosis & DDD at L3-4 | L3-4 | Dynesys | - | - |
| 10 | F | 51 | 57 | L4-5-S1 | 20 | 70 | Stenosis & DDD at L3-4 | L3-4 | Dynesys | - | - |
| 11 | F | 58 | 65 | L4-5-S1 | 36 | 82 | Stenosis at L1-2-3 | L1-2-3 | Dynesys | - | - |
| 12 | F | 67 | 69 | L4-5 | 20 | 22 | Stenosis & DDD at L2-3-4 | L2-3-4 | NFlex | - | + |
| 13 | F | 64 | 70 | L4-5-S1 | 12 | 60 | Stenosis at L3-4 | L3-4 | NFlex | + | - |
| 14 | F | 43 | 46 | L3-4 | Persistent pain | 25 | Stenosis & DDD at L4-5 | L4-5 | NFlex | + | - |
| 15 | F | 56 | 57 | L2-3 | Persistent pain | 6 | Stenosis at L4-5 | L4-5 | NFlex | - | - |
DDD: degenerative disc disease; SPL: spondylolisthesis; ‘+’: developed, ‘-’: absent.
Fig. 1.
The application of Dynesys system (case No. 9). A 70-year-old female patient was diagnosed with spinal stenosis and spondylolisthesis (A) and underwent fusion surgery at L4-5 previously 8 years prior to her visit (B). She developed back pain with intermittent claudication recently in the past year. Spinal stenosis was revealed at L3-4, and dynamic stabilization surgery was performed with Dynesys system at L3-4 (C). Postoperatively 3 years later, her symptoms were much improved with stable radiographic findings (D).
Fig. 2.
The application of NFlex system (case No. 14). A 46-year-old female patient underwent fusion surgery at L3-4 previously 2 years prior to her visit (A), but she complained of persistent pain (B). With more progressed spinal stenosis at L4-5, she underwent dynamic stabilization surgery with the NFlex system (C). No significant radiologic findings at adjacent segments were observed (D), but she maintained medical treatment for pain reduction.
Clinical outcomes
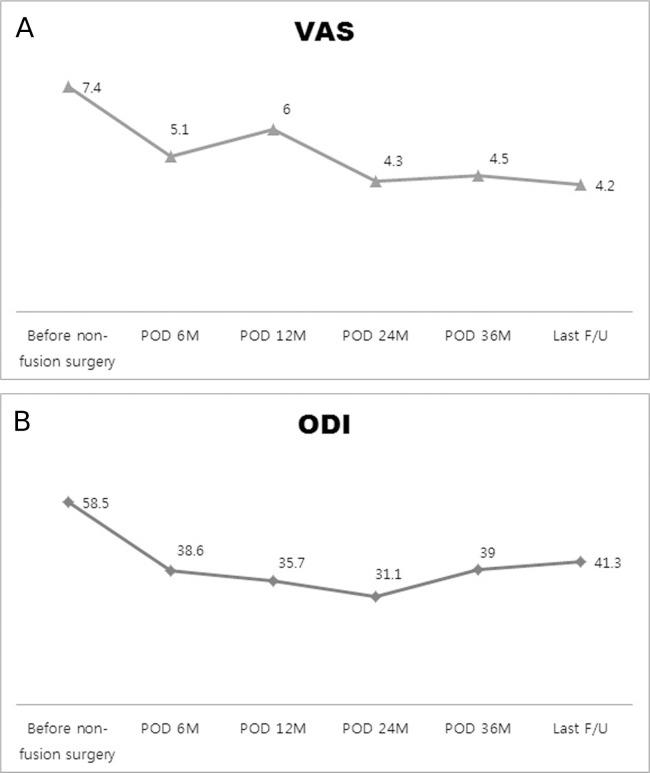
Mean follow-up was conducted for 44.8 ± 25.0 months (range, 12-79). Before the non-fusion surgery, the VAS was checked and was found to be 7.4 ± 1.8 (range, 5-10); it had a tendency to decrease after non-fusion surgery, and it showed a significantly decrease to 4.2 ± 1.1 (range, 3-5) upon the last evaluation (p= 0.027, Figure 3A). ODI was preoperatively 58.5 ± 16.9% (range, 35.5-88.8), and it changed to 41.3 ± 22.8% (range, 11.1-60.0, p=0.018, Figure 3B). However, three patients complained about persistent pain after their non-fusion surgery, and four patients (26.6%) had a relapse of pain in the back and leg after a mean of 30 months after non-fusion surgery (30.0 ± 11.3 months, range, 20-43). Upon the last follow-up, four patients had not taken analgesics, and the remaining eleven patients could reduce the number of their medications to a mean 1.2 analgesics. This was a statistically significant decrease compared to the amount before the non-fusion surgery (p=0.004). Persistent pain after the fusion and non-fusion surgeries, as well as relapsed pain after the non-fusion surgery, did not affect the differences in both the VAS and ODI values (all p>0.05). No patient underwent additional surgery for ASP after undergoing non-fusion dynamic stabilization surgery.
Fig. 3.
Clinical outcomes. A) VAS change. Before non-fusion surgery, VAS was 7.4, and it gradually decreased after non-fusion surgery. VAS was 4.2 at 36 months postoperatively (p= 0.027). B) ODI change. ODI showed a change from 58.5% to 35.0% 36 months postoperatively (p=0.018).
MRI changes according to the surgical procedure
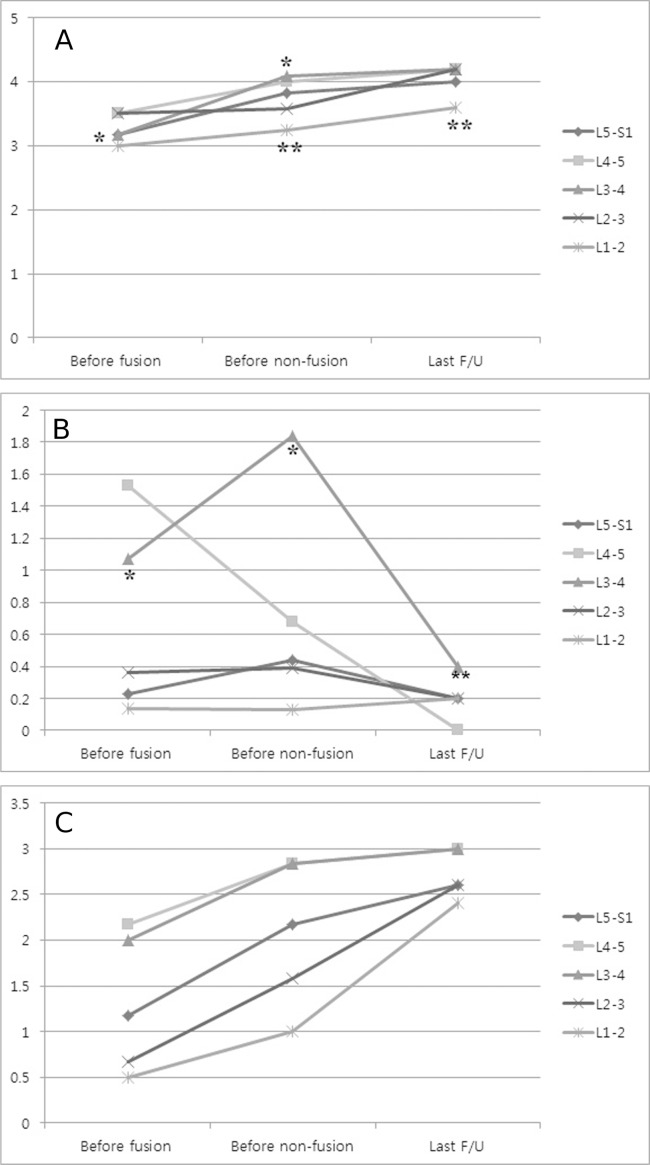
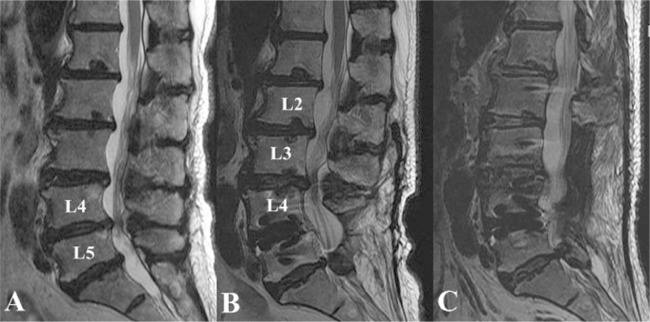
The last MRI was obtained at 36.2 ± 23.8 months (range, 12-72) after non-fusion surgery. The Pfirrmann disc degeneration grades were respectively 3.0, 3.5, 3.2, 3.5 and 3.2 at segments L1-2 to L5-S1 before fusion surgery; these were 3.3, 3.6, 4.1, 4.0 and 3.8 at each respective segment before non-fusion surgery (Figure 4A and Figure 5). Only the intervertebral disc at L3-4 between the fusion and non-fusion surgeries had degenerated to a statistically significant degree (p=0.046). Upon the last MRI, the disc degeneration grades were 4.0, 4.2, 4.2, 4.2 and 4.0 at each respective segment, and the change at L1-2 between non-fusion surgery and the last MRI showed statistical significance (p=0.032), whereas other segments had not changed (all p>0.05). Through central canal stenosis was respectively graded as 0, 0.3, 1.0, 1.1 and 0.2 at segments L1-2 to L5-S1 before fusion surgery, these values were respectively 0.1, 0.7, 1.5, 0.5 and 0.2 before non-fusion surgery (Figure 4B), and central stenosis at L3-4 had significantly worsened (p=0.041). Stenosis at L4-5 was decompressed from the fusion surgery, but this did not show statistical significance (p=0.114). Stenosis at L3-4 was sufficiently decompressed after non-fusion surgery (p=0.041), and the changes in other segmental stenosis conditions upon the last MRI were not significant. Facet joints showed gradual degeneration at points before the fusion to after the non-fusion surgeries, but these changes were not significant at all segments (all P>0.05, Figure 4C).
Fig. 4.
MRI changes. A) Disc degeneration. Each segmental lumbar intervertebral disc gradually degenerated from the time before fusion surgery to after non-fusion surgery. Before non-fusion surgery, disc degeneration at L3-4 (*) showed statistically significant changes compared to that before fusion surgery (p=0.046). Between non-fusion surgery and the last MRI evaluation, the change at L1-2 (**) was statistically significant (p=0.032). B) Central stenosis. In the state between fusion and non-fusion surgery, stenosis at L3-4 (*) demonstrated significant degeneration (p=0.041) despite the fact that the L4-5 segment was decompressed by the fusion surgery. After non-fusion surgery, L3-4 (**) sufficient decompression was accomplished (p=0.041), but other instances of segmental stenosis did not show statistically significant changes. C) Facet joint degeneration. Each segmental facet joint was degenerated as time passed. However, the changes between fusion and non-fusion surgery and between non-fusion surgery and the last follow-up did not show statistical significance.
Fig. 5.
The change of disc degeneration on MRI (case No. 12). A 69-year-old female patient had spinal stenosis at L4-5 with multilevel disc degeneration (A). After a previous fusion surgery at L4-5 two years prior to her visit, spinal stenosis by thickening of the ligamentum flavum and disc degeneration at L2-3-4 had progressed (B). She underwent decompression and dynamic stabilization surgery at L2-3-4. At the postoperative 12-month MRI, segments at L1-2 and L5-S1 showed progression of disc degeneration (C).
Radiologic changes on lateral radiographs
The disc degeneration changes according to lateral radiographs are shown in Figure 6. Before fusion surgery, disc degeneration was observed as follows: 0.9, 1.9, 2.0, 2.4 and 1.6 from L1-2 to L5-S1. Before non-fusion surgery, these values were respectively 1.2, 1.6, 2.8, 2.2 and 1.7, and the degree of disc degeneration at L3-4 showed a significant change (p=0.046). As each disc gradually degenerated, disc degeneration was graded at 3.0, 3.3, 2.6, 3.0 and 1.6 at 36 months after non-fusion surgery. The most frequently involved segment, L3-4, was not changed after non-fusion surgery. Disc degeneration was observed at L1-2 and L2-3, but neither was not statistically significant (p=0.083 and p=0.083, respectively). ROM at T12-S1 was 22.3° ± 22.3 before non-fusion surgery and it was measured 19.1° ± 20.3, 20.4° ± 17.8 and 16.0° ± 7.2 at each annular follow-up period (p=0.180). Based on the definition of radiologic ASP, it was observed in five patients (33.3%) at 30.0 ± 9.5 months (range, 24-40) after the non-fusion surgery. These radiologic features showed disc space narrowing at L1-2 and L2-3 in all cases as a proximal segment. In terms of radiologic abnormalities, screw or NFlex rod fractures were not observed, but a radiolucent line around a screw was identified in five patients (33.3%) with seven screws at the last radiographs.
Fig. 6.
Disc degeneration on lateral radiographs. Upon a comparison of disc degeneration before fusion and before non-fusion surgery and between each postoperative follow-up period, disc degeneration at L3-4 (*) was noted when comparing the state before the fusion surgery and that before the non-fusion surgery. After non-fusion dynamic stabilization surgery, disc degeneration gradually progressed, especially at L1-2 and L2-3.
Discussion
Surgical outcomes of ASP treated with the non-fusion dynamic stabilization system
Many spine surgeons have an interest in managing ASP in patients who undergo fusion surgery and in knowing which surgical method is most effective to prevent ASP. First, additional fusion extension surgery for ASP reportedly shows good clinical outcomes. Five fusion extension studies demonstrated this in patients with a mean age ranging from 52 to 61 years, with males making up 23% to 50% of the study populations.17 The time interval between fusion extension for ASP and the previous fusion surgery ranged from 4.8 to 11.5 years. Although the clinical outcome measurement methods among these five fusion studies varied, satisfactory results were noted in 76.9% - 85% of cases, and postoperative pain relief was identified in 78.6%.18–20 In a recent study about revision lumbar surgery in elderly patients (age >65 years) with symptomatic pseudarthrosis, ASP, or same-level recurrent stenosis, VAS values for back pain and two-year ODI showed significant improvements two years after surgery.21 However, informal outcome measures taking into account pain, medication use, and return to work showed a good outcome in 35.7% of cases.20 Two years postoperatively, only 38% and 40% of patients reached the minimum clinically important difference (MCID) threshold for the ODI and the 36-item short-form health survey (SF-36) physical component scale, respectively.22 Moreover, improvement from the previous surgery was the most predictive factor for subsequent improvement after fusion extension for ASP.22 Additionally, long revision fusion surgery has overall 34.4% of major complications and associated risk factors were age>60 years, medical comorbidities and obesity.23 In two studies of ASP treated with decompression only, patients showed good to excellent results in 57.7% and 64.2% of cases. However, decompression led to increased reoperation and revision rates, and in a meta-analysis, laminectomy alone for the treatment of stenosis with degenerative spondylolisthesis was associated with a 31% incidence of slip progression.26 Instability and recurrence of symptomatic stenosis are both reported complications of laminectomy alone for the treatment of degenerative lumbar scoliosis and stenosis.27 One study reported results of patients with ASP treated with a motion-preserving technique using total disc arthroplasty (TDR).28 Twenty patients in whom symptomatic ASP after lumbar fusion underwent ProDisc lumbar TDR, after which significant improvements in patient satisfaction and disability scores were observed three months postoperatively; these scores were maintained at a two-year follow-up.
Through there is no report on ASP treated with a motion-preserving technique using a pedicle-based dynamic stabilization system, the present study is the first to report the surgical outcome of ASP treated with non-dynamic stabilization system surgery with mid-term follow-ups. As surgical indications for non-fusion dynamic stabilization surgery were extended, the corresponding surgeon attempted to apply this non-fusion dynamic stabilization system to patients who suffered from ASP after fusion surgery. ASP after fusion surgery was identified with disc degeneration and hypertrophy of the ligamentum flavum, causing adjacent segment stenosis, without any significant deformity or instability. Hence, surgery was planned to remove previous inserted rods and screws, to perform sufficient decompression with preservation of integrity of intervertebral disc and facet joints, and to apply the non-fusion dynamic stabilization system to the symptomatic segment. Radiologic changes through MRI and lateral radiographs revealed the progression of disc degeneration and central stenosis at adjacent segments, especially at L3-4 as a proximal segment upon the development of ASP after the fusion procedure. The overall clinical outcome in terms of VAS and ODI showed great improvements after non-fusion surgery, and reductions in the use of pain medication were observed upon the last follow-up. However, five patients complained of persistent pain after the previous fusion surgery, and among them, four patients presented with persistent pain or relapsed pain even after non-fusion surgery. One additional patient presented with persistent pain after non-fusion surgery and two patients experienced pain relapses within 30 months after non-fusion surgery. Although much improvement in terms of pain scores and reductions in pain medication was observed, functional outcomes measured by ODI showed moderate disabilities which were not comparable with our previous clinical experiences with the dynamic stabilization system. In research about poor ODI outcomes among 1054 patients who underwent lumbar spinal fusion, younger men, obese patients, smokers, those with multiple medical comorbidities, those receiving workers compensation, those with psychosocial stressors, and those who had undergone revision lumbar surgery were associated with poor functional outcomes.30–32 And revision surgery for adult deformity surgery also reported significantly lower clinical outcomes in terms of function and pain.33 Similarly, the authors felt that unsatisfactory functional outcomes may be associated with revision surgery.
ASP development after the use of the non-fusion dynamic stabilization system
Through the objective of non-fusion dynamic stabilization is to maintain the normal physiologic range of motion (ROM) and reduce disc and facet joint stress, these theoretically biomechanical properties suggest that this procedure should produce better clinical outcomes, especially regarding ASP prevention.34–37 Successful clinical outcomes in patients who undergo non-fusion dynamic stabilization have been reported, but the long-term effect on ASP after the application of a dynamic stabilization system has not been thoroughly addressed in a clinical series. In the present study, changes in commodities disc, spinal canal and facet joint were in the form of gradual degeneration after non-fusion dynamic surgery at all lumbar segments, and commodities operative segment treated with the non-fusion dynamic stabilization system was preserved without statistical significance. Nonetheless, significant changes were found in the intervertebral disc at L1-2 according to postoperative MRI follow-ups. On lateral radiographs, disc degeneration grades were increased after non-fusion surgery, but these changes were also not statistically significant when comparing grades before non-fusion surgery and 36 months postoperatively. However, radiologic ASP was observed in five patients (33.3%) within 30 months after non-fusion dynamic stabilization surgery. The main characteristic of ASP was disc space narrowing at the segment proximal to the non-fusion instrumented segment; these segments were L1-2 in one patient and L2-3 in four patients. Although the changes at the L1-2 and L2-3 segments were not statistically significant, degeneration in the disc and in the facet joint leading to central stenosis at the corresponding segments was identified by means of MRI and plain radiographs.
Much debate regarding ASP has centered on how much of the degeneration is actually related to the fused segment and how much is related to the natural history of the aging spine.17, 41 According to a recent systemic review about the natural history of the degeneration of the spine, biomechanical effects after fusion may accelerate pathologic changes at adjacent segments, and radiologic ASP may occur at a higher rate relative to the natural history. 42 We observed the sequential development of ASP after fusion surgery followed by ASP after non-fusion surgery. Therefore, the authors agree that there is likely an adverse effect of instrumented surgery on the spine on the development of ASP. Even after non-fusion dynamic stabilization, ASP developed at a rate of 33.3% within 30 months after non-fusion surgery. The mean age at surgery differed by six years between the prior fusion and the later non-fusion surgeries, but ASP developed in a similar period after both surgeries. Considering degeneration caused by the aging process, the author suggests that the non-fusion dynamic stabilization system cannot prevent the development of ASP but that the current system may delay this. Several biomechanical studies of current dynamic stabilization systems have revealed non-physiologic effects, such as insufficient ROM and cases of an abnormal instantaneous center of rotation (COR) compared to an intact spine.34–36 Other authors have reported that the stiffness resulting from the use of the Dynesys system is identical to that resulting from rigid fixation. All of these studies suggest that the Dynesys system is limited when used to simulate the normal spinal motion of an intact spine. The biomechanical discrepancies and design characteristics of the dynamic stabilization system may have a flaw with regard to the prevention of ASP. In addition, several reports reported that screw loosening was not significant problem during dynamic stabilization but that the risk factors and long-term effects should be investigated.
Study limitation
This study reported single surgeon's clinical experiences with a non-fusion dynamic stabilization system for ASP involving a small number of patients. As the mean follow-up period was 44.8 months, this relatively short follow-up time is also a limitation when formulating any conclusion. A comparative study of decompression alone, a non-fusion dynamic stabilization system and fusion extension surgery should be conducted for useful results in patients after they have undergone lumbar fusion, but with a relative small number of patients, we could not plan such a study. While two types of dynamic stabilization systems were used in the present study, four patients in Dynesys system group and one patient in the NFlex system group showed radiologic ASP. A better physiologic dynamic device could not be determined given our small study population, and a prospective randomized study comparing different types of dynamic stabilization systems should be designed. Hence, this study is more of a preliminary report of a series of cases regarding the application of a non-fusion dynamic stabilization system for ASP after lumbar fusion. Although ASP after non-fusion dynamic stabilization surgery was still observed, these devices may be able to delay the development of ASP. Further-more, additional physiologic devices for motion preservation should be devised and tested.
Conclusion
The authors identified that non-fusion dynamic stabilization surgery was a safe procedure corresponding to fusion surgery, even in elderly patients with ASP. ASP after non-fusion dynamic stabilization surgery was still observed, but the clinical outcomes observed significant improvements, and these devices may be able to delay the development of ASP. Radiologic ASP was observed in five patients within 30 months after non-fusion surgery, but no additional surgery for ASP was conducted in all cases. Long-term studies are necessary to determine the effectiveness of these systems on the prevention of ASP after non-fusion dynamic stabilization surgery.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings described in this paper. No benefits in any form have been or will be received from any commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Albee FH. Transplantation of a portion of the tibia into the spine for Pott's disease: a preliminary report 1911. Clin Orthop Relat Res. 2007 Jul;460:14–16. doi: 10.1097/BLO.0b013e3180686a0f. [DOI] [PubMed] [Google Scholar]
- 2.Lawrence BD, Wang J, Arnold PM, Hermsmeyer J, Norvell DC, Brodke DS. Predicting the risk of adjacent segment pathology after lumbar fusion: a systematic review. Spine. 2012 Oct 15;37(22 Suppl):S123–132. doi: 10.1097/BRS.0b013e31826d60d8. [DOI] [PubMed] [Google Scholar]
- 3.Ghiselli G, Wang JC, Bhatia NN, Hsu WK, Dawson EG. Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am. 2004 Jul;86-A(7):1497–1503. doi: 10.2106/00004623-200407000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Lee SE, Park SB, Jahng TA, Chung CK, Kim HJ. Clinical experience of the dynamic stabilization system for the degenerative spine disease. J Korean Neurosurg Soc. 2008 May;43(5):221–226. doi: 10.3340/jkns.2008.43.5.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine (Phila Pa 1976). 2006 Feb 15;31(4):442–449. doi: 10.1097/01.brs.0000200092.49001.6e. [DOI] [PubMed] [Google Scholar]
- 6.Schaeren S, Broger I, Jeanneret B. Minimum four-year follow-up of spinal stenosis with degenerative spondylolisthesis treated with decompression and dynamic stabilization. Spine (Phila Pa 1976). 2008 Aug 15;33(18):E636–642. doi: 10.1097/BRS.0b013e31817d2435. [DOI] [PubMed] [Google Scholar]
- 7.Di Silvestre M, Lolli F, Bakaloudis G, Parisini P. Dynamic stabilization for degenerative lumbar scoliosis in elderly patients. Spine (Phila Pa 1976). 2010 Jan 15;35(2):227–234. doi: 10.1097/BRS.0b013e3181bd3be6. [DOI] [PubMed] [Google Scholar]
- 8.Lee S, Jahng TA, Kim HJ. Decompression and nonfusion dynamic stabilization for spinal stenosis with degenerative lumbar scoliosis. Journal of neurosurgery. Spine. 2014 Aug 1;:1–10. doi: 10.3171/2014.6.SPINE13190. [DOI] [PubMed] [Google Scholar]
- 9.Coe JD, Kitchel SH, Meisel HJ, Wingo CH, Lee SE, Jahng TA. NFlex Dynamic Stabilization System : Two-Year Clinical Outcomes of Multi-Center Study. J Korean Neurosurg Soc. 2012 Jun;51(6):343–349. doi: 10.3340/jkns.2012.51.6.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multicenter study of a novel non-fusion system. Eur Spine J. 2002 Oct;11(Suppl 2):S170–178. doi: 10.1007/s00586-002-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee CS, Hwang CJ, Lee SW, et al. Risk factors for adjacent segment disease after lumbar fusion. Eur Spine J. 2009 Nov;18(11):1637–1643. doi: 10.1007/s00586-009-1060-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001 Sep 1;26(17):1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 13.Lee GY, Lee JW, Choi HS, Oh KJ, Kang HS. A new grading system of lumbar central canal stenosis on MRI: an easy and reliable method. Skeletal Radiol. 2011 Aug;40(8):1033–1039. doi: 10.1007/s00256-011-1102-x. [DOI] [PubMed] [Google Scholar]
- 14.Weishaupt D, Zanetti M, Boos N, Hodler J. MR imaging and CT in osteoarthritis of the lumbar facet joints. Skeletal Radiol. 1999 Apr;28(4):215–219. doi: 10.1007/s002560050503. [DOI] [PubMed] [Google Scholar]
- 15.Kettler A, Wilke HJ. Review of existing grading systems for cervical or lumbar disc and facet joint degeneration. Eur Spine J. 2006 Jun;15(6):705–718. doi: 10.1007/s00586-005-0954-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kanayama M, Hashimoto T, Shigenobu K, et al. Adjacent-segment morbidity after Graf ligamentoplasty compared with posterolateral lumbar fusion. J Neurosurg. 2001 Jul;95(1 Suppl):5–10. doi: 10.3171/spi.2001.95.1.0005. [DOI] [PubMed] [Google Scholar]
- 17.Chou D, Dekutoski M, Hermsmeyer J, Norvell DC. The treatment of lumbar adjacent segment pathology after a previous lumbar surgery: a systematic review. Spine. 2012 Oct 15;37(22 Suppl):S180–188. doi: 10.1097/BRS.0b013e31826d613d. [DOI] [PubMed] [Google Scholar]
- 18.Chen WJ, Lai PL, Niu CC, Chen LH, Fu TS, Wong CB. Surgical treatment of adjacent instability after lumbar spine fusion. Spine. 2001 Nov 15;26(22):E519–524. doi: 10.1097/00007632-200111150-00024. [DOI] [PubMed] [Google Scholar]
- 19.Glassman SD, Pugh K, Johnson JR, Dimar JR., 2nd Surgical management of adjacent level degeneration following lumbar spine fusion. Orthopedics. 2002 Oct;25(10):1051–1055. doi: 10.3928/0147-7447-20021001-16. [DOI] [PubMed] [Google Scholar]
- 20.Whitecloud TS, 3rd, Davis JM, Olive PM. Operative treatment of the degenerated segment adjacent to a lumbar fusion. Spine. 1994 Mar 1;19(5):531–536. doi: 10.1097/00007632-199403000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Adogwa O, Carr RK, Kudyba K, et al. Revision lumbar surgery in elderly patients with symptomatic pseudarthrosis, adjacent-segment disease, or same-level recurrent stenosis. Part 1. Two-year outcomes and clinical efficacy: clinical article. Journal of neurosurgery. Spine. 2013 Feb;18(2):139–146. doi: 10.3171/2012.11.SPINE12224. [DOI] [PubMed] [Google Scholar]
- 22.Djurasovic M, Glassman SD, Howard JM, Copay AG, Carreon LY. Health-related quality of life improvements in patients undergoing lumbar spinal fusion as a revision surgery. Spine. 2011 Feb 15;36(4):269–276. doi: 10.1097/BRS.0b013e3181cf1091. [DOI] [PubMed] [Google Scholar]
- 23.Cho SK, Bridwell KH, Lenke LG, et al. Major complications in revision adult deformity surgery: risk factors and clinical outcomes with 2- to 7-year follow-up. Spine. 2012 Mar 15;37(6):489–500. doi: 10.1097/BRS.0b013e3182217ab5. [DOI] [PubMed] [Google Scholar]
- 24.Schlegel JD, Smith JA, Schleusener RL. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine. 1996 Apr 15;21(8):970–981. doi: 10.1097/00007632-199604150-00013. [DOI] [PubMed] [Google Scholar]
- 25.Phillips FM, Carlson GD, Bohlman HH, Hughes SS. Results of surgery for spinal stenosis adjacent to previous lumbar fusion. J Spinal Disord. 2000 Oct;13(5):432–437. doi: 10.1097/00002517-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Mardjetko SM, Connolly PJ, Shott S. Degenerative lumbar spondylolisthesis. A meta-analysis of literature 1970-1993. Spine. 1994 Oct 15;19(20 Suppl):2256S–2265. [PubMed] [Google Scholar]
- 27.Brodke DS, Annis P, Lawrence BD, Woodbury AM, Daubs MD. Reoperation and revision rates of 3 surgical treatment methods for lumbar stenosis associated with degenerative scoliosis and spondylolisthesis. Spine. 2013 Dec 15;38(26):2287–2294. doi: 10.1097/BRS.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 28.Bertagnoli R, Yue JJ, Fenk-Mayer A, Eerulkar J, Emerson JW. Treatment of symptomatic adjacent-segment degeneration after lumbar fusion with total disc arthroplasty by using the prodisc prosthesis: a prospective study with 2-year minimum follow up. Journal of neurosurgery. Spine. 2006 Feb;4(2):91–97. doi: 10.3171/spi.2006.4.2.91. [DOI] [PubMed] [Google Scholar]
- 29.Moon KY, Lee SE, Kim KJ, Hyun SJ, Kim HJ, Jahng TA. Back muscle changes after pedicle based dynamic stabilization. J Korean Neurosurg Soc. 2013 Mar;53(3):174–179. doi: 10.3340/jkns.2013.53.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Carreon LY, Glassman SD, Djurasovic M, et al. Are preoperative health-related quality of life scores predictive of clinical outcomes after lumbar fusion? Spine. 2009 Apr 1;34(7):725–730. doi: 10.1097/BRS.0b013e318198cae4. [DOI] [PubMed] [Google Scholar]
- 31.DeVine J, Norvell DC, Ecker E, et al. Evaluating the correlation and responsiveness of patient-reported pain with function and quality-of-life outcomes after spine surgery. Spine. 2011 Oct 1;36(21 Suppl):S69–74. doi: 10.1097/BRS.0b013e31822ef6de. [DOI] [PubMed] [Google Scholar]
- 32.Gum JL, Carreon LY, Stimac JD, Glassman SD. Predictors of Oswestry Disability Index worsening after lumbar fusion. Orthopedics. 2013 Apr;36(4):e478–483. doi: 10.3928/01477447-20130327-26. [DOI] [PubMed] [Google Scholar]
- 33.Cho SK, Bridwell KH, Lenke LG, et al. Comparative analysis of clinical outcome and complications in primary versus revision adult scoliosis surgery. Spine. 2012 Mar 1;37(5):393–401. doi: 10.1097/BRS.0b013e31821f0126. [DOI] [PubMed] [Google Scholar]
- 34.Schmoelz W, Huber JF, Nydegger T, Dipl I, Claes L, Wilke HJ. Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech. 2003 Aug;16(4):418–423. doi: 10.1097/00024720-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Niosi CA, Zhu QA, Wilson DC, Keynan O, Wilson DR, Oxland TR. Biomechanical characterization of the three-dimensional kinematic behaviour of the Dynesys dynamic stabilization system: an in vitro study. Eur Spine J. 2006 Jun;15(6):913–922. doi: 10.1007/s00586-005-0948-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zander T, Rohlmann A, Burra NK, Bergmann G. Effect of a posterior dynamic implant adjacent to a rigid spinal fixator. Clin Biomech (Bristol, Avon). 2006 Oct;21(8):767–774. doi: 10.1016/j.clinbiomech.2006.04.001. [DOI] [PubMed] [Google Scholar]
- 37.Cunningham BW, Gordon JD, Dmitriev AE, Hu N, McAfee PC. Biomechanical evaluation of total disc replacement arthroplasty: an in vitro human cadaveric model. Spine. 2003 Oct 15;28(20):S110–117. doi: 10.1097/01.BRS.0000092209.27573.90. [DOI] [PubMed] [Google Scholar]
- 38.Morishita Y, Ohta H, Naito M, et al. Kinematic evaluation of the adjacent segments after lumbar instrumented surgery: a comparison between rigid fusion and dynamic non-fusion stabilization. Eur Spine J. 2011 Sep;20(9):1480–1485. doi: 10.1007/s00586-011-1701-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rohlmann A, Burra NK, Zander T, Bergmann G. Comparison of the effects of bilateral posterior dynamic and rigid fixation devices on the loads in the lumbar spine: a finite element analysis. Eur Spine J. 2007 Aug;16(8):1223–1231. doi: 10.1007/s00586-006-0292-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Niosi CA, Wilson DC, Zhu Q, Keynan O, Wilson DR, Oxland TR. The effect of dynamic posterior stabilization on facet joint contact forces: an in vitro investigation. Spine. 2008 Jan 1;33(1):19–26. doi: 10.1097/BRS.0b013e31815e7f76. [DOI] [PubMed] [Google Scholar]
- 41.Wang JC, Arnold PM, Hermsmeyer JT, Norvell DC. Do lumbar motion preserving devices reduce the risk of adjacent segment pathology compared with fusion surgery? A systematic review. Spine. 2012 Oct 15;37(22 Suppl):S133–143. doi: 10.1097/BRS.0b013e31826cadf2. [DOI] [PubMed] [Google Scholar]
- 42.Lee MJ, Dettori JR, Standaert CJ, Brodt ED, Chapman JR. The natural history of degeneration of the lumbar and cervical spines: a systematic review. Spine. 2012 Oct 15;37(22 Suppl):S18–30. doi: 10.1097/BRS.0b013e31826cac62. [DOI] [PubMed] [Google Scholar]
- 43.Jahng TA, Kim YE, Moon KY. Comparison of the biomechanical effect of pedicle-based dynamic stabilization: a study using finite element analysis. Spine J. 2013 Jan;13(1):85–94. doi: 10.1016/j.spinee.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 44.Kim CH, Chung CK, Jahng TA. Comparisons of outcomes after single or multilevel dynamic stabilization: effects on adjacent segment. J Spinal Disord Tech. 2011 Feb;24(1):60–67. doi: 10.1097/BSD.0b013e3181d4eb44. [DOI] [PubMed] [Google Scholar]
- 45.Ko CC, Tsai HW, Huang WC, et al. Screw loosening in the Dynesys stabilization system: radiographic evidence and effect on outcomes. Neurosurg Focus. 2010 Jun;28(6):E10. doi: 10.3171/2010.3.FOCUS1052. [DOI] [PubMed] [Google Scholar]
- 46.Wu JC, Huang WC, Tsai HW, et al. Pedicle screw loosening in dynamic stabilization: incidence, risk, and outcome in 126 patients. Neurosurg Focus. 2011 Oct;31(4):E9. doi: 10.3171/2011.7.FOCUS11125. [DOI] [PubMed] [Google Scholar]