Abstract
Objective
Although standard method has not been established for the chronic subdural hematoma (CSDH), burr-hole trephination and closed system drainage with or without irrigation has been widely accepted as the treatment of choice. The aim of this study is to analysis the post-operative recurrence rates after burr-hole trephination of the CSDH according to the conduction of irrigation.
Methods
We retrospectively reviewed 184 patients with CSDH who underwent surgical treatment between January 2009 and December 2013. And 152 patients fulfilled the inclusion criteria as follows: 1) CSDH diagnosed on computed tomography (CT), 2) unilateral hematoma, 3) burr-hole trephination with closed system drainage, and 4) follow-up CT for at least 3 months. Those patients were divided into two groups. Group A (n=38) underwent burr-hole trephination without irrigation, and Group B (n=114), burr-hole trephination with saline irrigation.
Results
The overall post-operative recurrence rate was 19.1% (n=29) in this study. The majority of recurrence showed in Group B. Twenty-eight patients (24.6%) of Group B had recurrence and only 1 patient (2.6%) of Group A showed recurrence. The recurrence rate was significantly higher in Group B compared with Group A (p=0.003). Another affecting factor for the recurrence was the amount of postoperative pneumocephalus (p=0.02). No catastrophic complications were found in postoperative course.
Conclusion
Although there was no difference of clinical outcome in both groups, the recurrence rate was higher in saline irrigation group compared with no irrigation group. We suggest that saline irrigation procedure be reserved only for selected cases in CSDH burr-hole surgery.
Keywords: Hematoma subdural chronic, Recurrence, Therapeutic irrigation, Drainage, Pneumocephalus
Introduction
Chronic subdural hematomas (CSDHs) are common pathologic entity in the elderly, especially after minor head trauma.4,6) The prevalence of CSDH seems to be increasing in a rapidly aging society.10) Management of the CSDH is not easy because of the high recurrence rate from 3.1% to 33.3% and several comorbidities in elderly.14,16)
Several surgical techniques have been proposed for the treatment of CSDH, including twist-drill trephination, burr-hole trephination, small or large craniotomy, and membranectomy.2,6,8,10,12,23) Of these methods, burr-hole trephination and closed drainage has been widely accepted as a reasonable option to treat the CSDH.4) However, there are some debates in the efficacy of intraoperative saline irrigation after burr-hole trephination.
The purpose of this study was to evaluate the efficacy of intraoperative saline irrigation after burr-hole trephination by analysis of the recurrence rates in two surgical methods, with or without saline irrigation. Furthermore, the relationship between recurrence rate and volume of postoperative pneumocephalus was investigated.
Materials and Methods
We retrospectively reviewed the medical records of 184 patients with CSDH who underwent surgical treatment in our institute between January 2009 and December 2013. 152 patients fulfilled the inclusion criteria as follows: 1) CSDH diagnosed on computed tomography (CT), 2) unilateral hematoma, 3) burr-hole trephination with closed system drainage, and 4) follow-up CT for at least 3 months. The patients consisted of 113 males and 39 females with a mean age of 66.2 years. The initial symptoms of the CSDH were abnormal behavior, headache, and neurological deficit such as motor weakness, dysarthria, and gait disturbance.
All patients were divided into two groups according to the conduction of intraoperative saline irrigation. Group A (n=38) underwent burr-hole trephination with closed system drainage without intraoperative saline irrigation and Group B (n=114) underwent burr-hole trephination with closed system drainage after intraoperative saline irrigation. In Group A, a drainage catheter was immediately inserted after dura mater incision through burr-hole without saline irrigation. In Group B, intraoperative saline irrigation was conducted through burr-hole and drain catheter repeatedly until the clear fluid gushed out. The closed system drainage catheter was maintained for 2 or 3 days and removed according to the change of drainage volume and radiological findings.
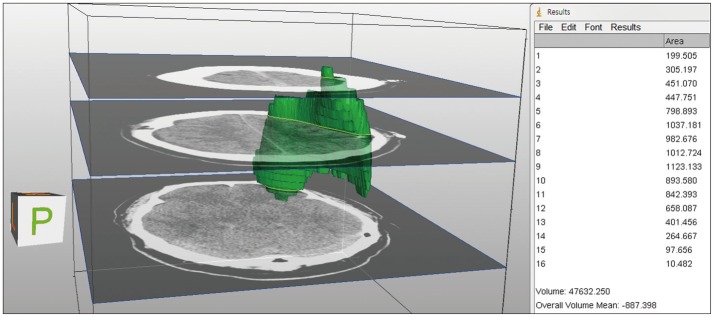
We analyzed the thickness of hematoma, density of hematoma, and membrane formation in subdural space on pre-operative CT. Volumetric analysis of pneumocephalus on operation day was calculated using ImageJ (version 1.48; National Institutes of Health, Washington, DC, USA). Subdural air on axial brain CT was manually outlined in ImageJ and respective region of interest (ROI) of each slice was added to the ROI manager. The area of each ROI was calculated and then multiplied by the slice thickness (5 mm). Finally, all slice volumes were added up to estimate the volume of each three-dimensional structure using Measure-Stack plug-in of ImageJ (Figure 1). Follow-up CT was check-ed on the third and tenth postoperative days. After discharge, the patients were re-evaluated clinically and radiologically by CT scans within 1 month and 3 months to check the thick-ness of subdural space.
FIGURE 1.
Volumetric analysis of pneumocephalus was calculat-ed using ImageJ. The pneumoce-phalus of subdural space on axial brain computed tomography was bounded as region of interest which multiplied by the slice thickness. And all slice volumes were added up to estimate the vo-lume of each 3D structure.
Clinical and radiological findings were reviewed for ev-aluation of the CSDH recurrence. The clinical criteria of recurrence included a mental status change, worsening of the preexisting neurological deficit and new onset or aggravation of headache. The radiological criteria of recurrence defined as increase of subdural fluid collection in the CT scans or further compression of brain parenchyme during the follow-up period. When the maximum width of CSDH was more than 10 mm on the follow-up CT and patients showed new onset or worsening of the symptoms at the same time, we defined as recurrence of CSDH. Each group was compared by the volume of post-operative pneumocephalus, recurrence rate, complications and length of hospital stay.
Statistical analyses were performed using SPSS statistic software (version 12.0 for Windows; SPSS Inc., Chicago, IL, USA). p-values were generated using chi-square, independent t-test. p-values of less than 0.05 was considered statistically significant.
Results
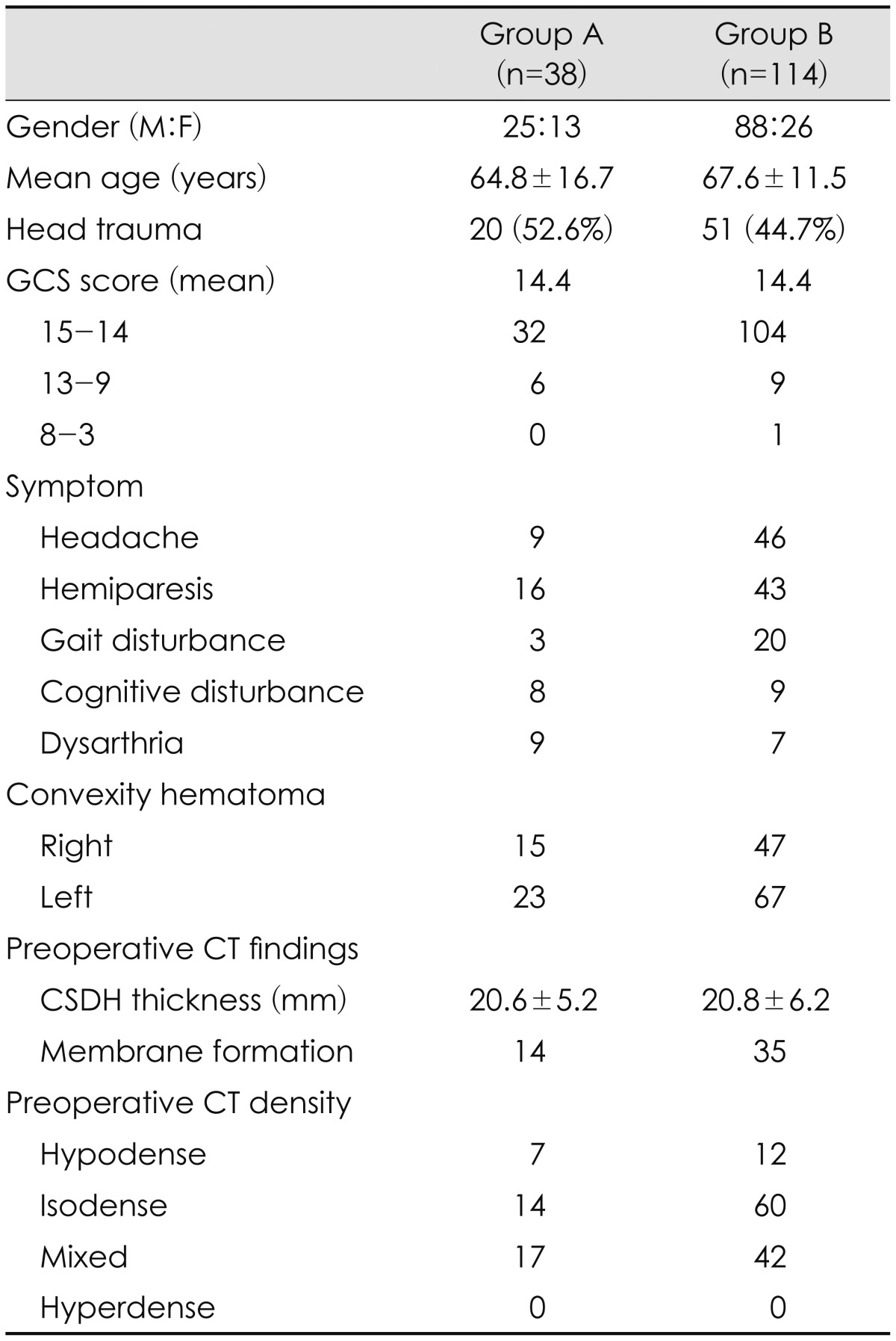
Demographic characteristics are shown in Table 1. There were 25 male and 13 female patients in Group A (n=38) and 88 male and 26 female in Group B (n=114). The average age of each group was 64.8±16.7 and 67.6±11.5 in Group A and B, respectively. A definite history of head injury was identified in 20 (52.6%) of Group A and 51 (44.7%) of Group B. The mean Glasgow coma scale at admission was 14.4 in both groups. The leading symptoms in the Group A were hemiparesis (35%), headache (20%), and dysarthria (20%), whereas the most frequent symptoms in the Group B were headache (37%), hemiparesis (34%), and gait disturbance (16%). On the pre-operative CT, the mean CSDH thickness of Group A was 20.6±5.2 mm and membrane formation was found in 14 patients. And hematomas showed hypodensity in 7 patients, isodensity in 14, and mixed density in 17. In Group B, the mean CSDH thickness was 20.8±6.2 mm and membrane formation was found in 35 patients. Hematomas demonstrated hypodensity in 12 patients, isodensity in 60, and mixed density in 42. There were no significant differences between two groups.
TABLE 1.
Demographic data of patients with chronic subdural hematoma
GCS: Glasgow coma scale, CT: computed tomography, CSDH: chronic subdural hematoma
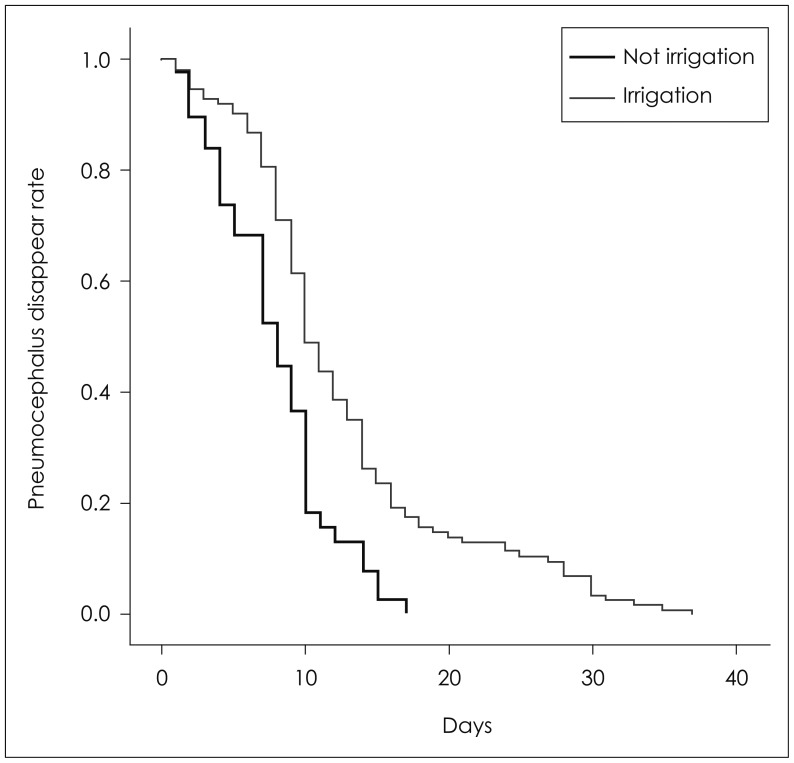
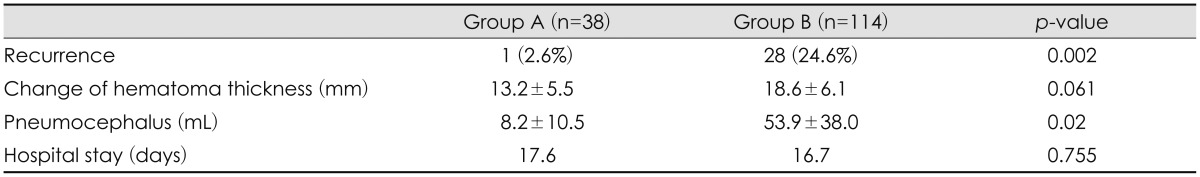
Our results showed the differences in the recurrence rate and radiologic findings according to intraoperative saline irrigation. Postoperative CT scan demonstrated differences in changing of the hematoma thickness and pneumocephalus. In comparison of the preoperative and postoperative state in the two groups, the thickness of CSDH was decreased in Group A more than Group B. The difference of the hematoma showed 13.2±5.5 mm in Group A and 18.6±6.2 in Group B (p=0.061). And the volume of pneumocephalus showed a distinct difference in Group B. The volume of pneumocephalus was 8.2±10.5 mL and 53.9±38.0 mL in Group A and Group B, respectively (p=0.02)(Figure 2).
FIGURE 2.
Kaplan-Meier plot shows difference between the period of post-operative pneumocephalus in subdural space (black: not irrigation, gray: irrigation).
In this study, overall recurrence was reported in 29 patients (19.08%), composed of one patient in Group A and 28 patients in Group B. The majority of recurrence was reported in Group B, intraoperative saline irrigation Group (p=0.002). The recurrence was identified by the clinical symptom and confirmed by follow-up CT. Furthermore, it was found that recurrence of CSDH was strongly related to the volume of pneumocephalus (p=0.003).
There are no significant differences in hospital stay. The average hospital stays were 17.6 days in Group A and 16.7 days in Group B. There was no catastrophic postoperative complication except urinary tract infection, delirium and pulmonary edema. Overall results are shown in Table 2.
TABLE 2.
Overall clinical and radiological results
Discussion
CSDH generally occurs in elderly people by minor head trauma.4,7) It originates in dural border cell layer, placed between dura mater and arachnoid membrane. The dissection of these cell layers makes a subdural cavity which is accumulated by bleeding.19) Because of extensive brain atrophy in elderly, brain is reduced by approximately 200 g, which results in an increased extracerebral volume of up to 11% allowing for greater movement of the brain.1,19,21) This situation makes brain to be vulnerable to developing CSDH. This extra volume can be occupied by the hematoma before a considerable rise in intracranial pressure occurs.1,3)
Surgical evacuation should be needed in CSDH with related symptoms such as headache, hemiparesis, gait disturbance, cognitive disturbance, and abnormal behavior. Various surgical treatments of CSDH have been used, including twist-drill trephination, burr-hole trephination, small or large craniotomy, and membranectomy, with or without irrigation and/or closed system drainage.2,6,8,10,12,23) Recently, several previous literatures suggested the efficacy of the burr-hole trephination. Burr-hole surgery is currently the most common surgical treatment for CSDH. Williams et al.22) concluded that burr hole evacuation was superior to twist drill evacuation of CSDH. And closed system drainage has been widely accepted as reasonable treatment. Many reports speculated the efficacy and lower recurrence rates of the drainage system with burr-hole trephination.11,14,15) One previous report showed significant higher recurrence rate in the patients without drainage, the recurrence rates was 30% without use of drain and 4% with use of drain.15) Some prospective studies showed no beneficial effect, whereas other authors report lower recurrence rates with the use of post-operative drains because of brain expansion.1,5,15) However, closed-system drainage may lead to complications, including hemorrhage, seizure induction, and infection.5,19)
It is unclear whether drainage alone or drainage with irrigation is better treatment for CSDH. Thus, the efficacy of intraoperative saline irrigation has not been well established. Several previous reports showed different results for the saline irrigation. Some studies reported no significant differences in outcome between each surgical techniques.12,23) Ishibashi et al.6) concluded that burr hole drainage with irrigation could be a effective treatment of CSDH with a lower recurrence rate. In contrast, a lower recurrence rate has been reported in patients in whom intra-operative irrigation was not used.9,17)
The current study showed significant lower recurrence rate in the patients managed without intraoperative saline irrigation. The recurrence rate was 2.6% in Group A treated with closed system drainage only, whereas it was 24.6% in Group B treated with irrigation and closed system drainage. And our results showed the large formation of pneumocephalus in irrigation group and its significant relationships with recurrence. Previous reports showed the large pneumocephalus in recurrence cases and the correlation between the volume of air remaining in the subdural cavity and the time required for the disappearance of the subdural cavity.1,13,17,20) Also saline irrigation can lead to brain cortical injury, cortical vessel injury, pneumocephalus, or infection because of high pressure to brain cortex.10,17) Previous studies suggested the risk factors of recurrences in CSDH including age, bleeding tendency, brain atrophy, alcohol abuse, bilateral CSDHs, higher hematoma density, membrane formation, thickness of initial CSDH, drain catheter tip location, postoperative air accumulation, and some technical aspects of surgery.8,18) In current study, intraoperative saline irrigation and postoperative pneumocephalus were regarded as important factors of recurrence in CSDH. And our result showed that amount of postoperative pneumocephalus was remarkable in intraoperative saline irrigation group. Thus, burr-hole trephination and drainage without saline irrigation could be more effective procedure for prevent of recurrence in CSDH.
Limitations of this study were that there was non-randomized study, bias inherent to retrospective chart reviews, and small sample size. Further investigations with larger sample size, quantitative controlled prospective study are required to assess the volume of pneumocephalus as an independent risk factor of CSDH recurrence.
Conclusion
Although there was no difference of clinical outcome in both groups, the recurrence rate was higher in intraoperative saline irrigation group compared with only burr-hole drainage group. We suggest that saline irrigation procedure be reserved only for selected cases in CSDH burr-hole surgery.
Footnotes
This study was supported by clinical research grant (2014), Pusan National University Hospital.
The authors have no financial conflicts of interest.
References
- 1.Aung TH, Wong WK, Mo HP, Tsang CS. Management of chronic subdural haematoma: burr hole drainage, replacement with Hartmann's solution, and closed-system drainage. Hong Kong Med J. 1999;5:383–386. [PubMed] [Google Scholar]
- 2.Camel M. Twist-drill craniostomy for the treatment of chronic subdural hematoma. Neurosurg Clin N Am. 2000;11:515–518. [PubMed] [Google Scholar]
- 3.Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Anderson K, et al. The surgical management of chronic subdural hematoma. Neurosurg Rev. 2012;35:155–169. doi: 10.1007/s10143-011-0349-y. discussion 169. [DOI] [PubMed] [Google Scholar]
- 4.Erol FS, Topsakal C, Faik Ozveren M, Kaplan M, Tiftikci MT. Irrigation vs. closed drainage in the treatment of chronic subdural hematoma. J Clin Neurosci. 2005;12:261–263. doi: 10.1016/j.jocn.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 5.Gurelik M, Aslan A, Gurelik B, Ozum U, Karadag O, Kars HZ. A safe and effective method for treatment of chronic subdural haematoma. Can J Neurol Sci. 2007;34:84–87. doi: 10.1017/s0317167100005849. [DOI] [PubMed] [Google Scholar]
- 6.Ishibashi A, Yokokura Y, Adachi H. A comparative study of treatments for chronic subdural hematoma: burr hole drainage versus burr hole drainage with irrigation. Kurume Med J. 2011;58:35–39. doi: 10.2739/kurumemedj.58.35. [DOI] [PubMed] [Google Scholar]
- 7.Kim HS, Heo W, Cha JH, Song JS, Rhee DY. Factor affecting recurrence of chronic subdural hematoma after burr-hole drainage. Korean J Neurotrauma. 2012;8:73–78. [Google Scholar]
- 8.Kim JH, Kang DS, Kim JH, Kong MH, Song KY. Chronic subdural hematoma treated by small or large craniotomy with membranectomy as the initial treatment. J Korean Neurosurg Soc. 2011;50:103–108. doi: 10.3340/jkns.2011.50.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuroki T, Katsume M, Harada N, Yamazaki T, Aoki K, Takasu N. Strict closed-system drainage for treating chronic subdural haematoma. Acta Neurochir (Wien) 2001;143:1041–1044. doi: 10.1007/s007010170010. [DOI] [PubMed] [Google Scholar]
- 10.Lee JK, Choi JH, Kim CH, Lee HK, Moon JG. Chronic subdural hematomas: a comparative study of three types of operative procedures. J Korean Neurosurg Soc. 2009;46:210–214. doi: 10.3340/jkns.2009.46.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lind CR, Lind CJ, Mee EW. Reduction in the number of repeated operations for the treatment of subacute and chronic subdural hematomas by placement of subdural drains. J Neurosurg. 2003;99:44–46. doi: 10.3171/jns.2003.99.1.0044. [DOI] [PubMed] [Google Scholar]
- 12.Muzii VF, Bistazzoni S, Zalaffi A, Carangelo B, Mariottini A, Pal-ma L. Chronic subdural hematoma: comparison of two surgical techniques. Preliminary results of a prospective randomized study. J Neurosurg Sci. 2005;49:41–46. discussion 46-47. [PubMed] [Google Scholar]
- 13.Nagata K, Asano T, Basugi N, Tango T, Takakura K. [Studies on the operative factors affecting the reduction of chronic subdural hematoma, with special reference to the residual air in the hematoma cavity] No Shinkei Geka. 1989;17:15–20. [PubMed] [Google Scholar]
- 14.Okada Y, Akai T, Okamoto K, Iida T, Takata H, Iizuka H. A comparative study of the treatment of chronic subdural hematoma--burr hole drainage versus burr hole irrigation. Surg Neurol. 2002;57:405–409. doi: 10.1016/s0090-3019(02)00720-6. discussion 410. [DOI] [PubMed] [Google Scholar]
- 15.Ramachandran R, Hegde T. Chronic subdural hematomas--causes of morbidity and mortality. Surg Neurol. 2007;67:367–372. doi: 10.1016/j.surneu.2006.07.022. discussion 372-373. [DOI] [PubMed] [Google Scholar]
- 16.Sambasivan M. An overview of chronic subdural hematoma: experience with 2300 cases. Surg Neurol. 1997;47:418–422. doi: 10.1016/s0090-3019(97)00188-2. [DOI] [PubMed] [Google Scholar]
- 17.Seong HY, Park JB, Kwon SC, Sim HB, Kim Y, Lyo IU. Effect of saline irrigation in the surgical treatment of chronic subdural hematoma. J Korean Neurotraumatol Soc. 2008;4:19–23. [Google Scholar]
- 18.Sim YW, Min KS, Lee MS, Kim YG, Kim DH. Recent changes in risk factors of chronic subdural hematoma. J Korean Neurosurg Soc. 2012;52:234–239. doi: 10.3340/jkns.2012.52.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sousa EB, Brandão LF, Tavares CB, Borges IB, Neto NG, Kessler IM. Epidemiological characteristics of 778 patients who underwent surgical drainage of chronic subdural hematomas in Brasília, Brazil. BMC Surg. 2013;13:5. doi: 10.1186/1471-2482-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stanišić M, Hald J, Rasmussen IA, Pripp AH, Ivanović J, Kolstad F, et al. Volume and densities of chronic subdural haematoma obtained from CT imaging as predictors of postoperative recurrence: a prospective study of 107 operated patients. Acta Neurochir (Wien) 2013;155:323–333. doi: 10.1007/s00701-012-1565-0. discussion 333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tabaddor K, Shulmon K. Definitive treatment of chronic subdural hematoma by twist-drill craniostomy and closed-system drainage. J Neurosurg. 1977;46:220–226. doi: 10.3171/jns.1977.46.2.0220. [DOI] [PubMed] [Google Scholar]
- 22.Williams GR, Baskaya MK, Menendez J, Polin R, Willis B, Nanda A. Burr-hole versus twist-drill drainage for the evacuation of chronic subdural haematoma: a comparison of clinical results. J Clin Neurosci. 2001;8:551–554. doi: 10.1054/jocn.2000.0926. [DOI] [PubMed] [Google Scholar]
- 23.Zakaraia AM, Adnan JS, Haspani MS, Naing NN, Abdullah JM. Outcome of 2 different types of operative techniques practiced for chronic subdural hematoma in Malaysia: an analysis. Surg Neurol. 2008;69:608–615. doi: 10.1016/j.surneu.2007.01.054. discussion 616. [DOI] [PubMed] [Google Scholar]