Abstract
Receptor for advanced glycation end products (RAGE) is a multiligand receptor of S100/calgranulins, high-mobility group box 1, and others, and it is associated with the pathogenesis of various inflammatory and circulatory diseases. The soluble form of RAGE (sRAGE) is a decoy receptor and competitively inhibits membrane-bound RAGE activation. In this study, we measured sRAGE levels in bronchoalveolar lavage fluid (BALF) of 78 patients, including 41 with interstitial pneumonia, 11 with sarcoidosis, 9 with respiratory infection, 7 with ARDS, 5 with lung cancer, and 5 with vasculitis. Among them, sRAGE was detectable in BALF of 73 patients (94%). In patients with ARDS and vasculitis, the sRAGE levels were significantly higher than in the control subjects and those with interstitial pneumonia. The sRAGE levels were positively correlated with total cell counts in BALF and serum levels of surfactant protein-D, lactate dehydrogenase, and C-reactive protein. There was an inverse correlation between PaO2/FIO2 ratio and sRAGE levels. These results indicate that sRAGE in BALF might be considered as a biomarker of lung inflammatory disorders, especially ARDS and vasculitis.
Keywords: RAGE, bronchoalveolar lavage, ARDS, vasculitis, surfactant protein D
Introduction
Receptor for advanced glycation end products (RAGE), a member of the immunoglobulin superfamily, is a multiligand, pattern-recognition receptor, which can bind advanced glycation end products (AGEs), amyloid β-peptide, and S100 proteins.1,2 AGEs are a class of compounds formed by non-enzymatic glycation and oxidation of proteins and lipids. RAGE has also been implicated in mediating the cytokine activity of high-mobility group box 1 (HMGB1), which is a late inflammatory mediator of sepsis or lipopolysaccharide (LPS) lethality.3 RAGE–ligand interaction results in rapid and sustained cellular activation and gene transcription, in most cases culminating in the activation of nuclear factor-κB.4,5 This cellular activation is related to inflammatory processes or tissue injury, such as diabetic microvascular injury or amyloidosis, and immune-inflammatory process.1,6
Structurally, RAGE consists of an extracellular, a transmembrane, and cytosolic domain (mRAGE). In addition, soluble forms exist, which act as decoy receptors since they display similar affinity for ligands and thereby limit their availability to mRAGE.7 Soluble forms are generated by two distinct mechanisms. First, by alternative splicing of the AGER gene, which leads to the formation of endogenous soluble RAGE (esRAGE).7 Second, ectodomain shedding of mRAGE generates soluble form of RAGE (sRAGE), which lacks both the transmembrane and cytosolic domain.8
RAGE is highly expressed in the mature lung by type I pneumocytes when compared with other lung cells and other tissues.9 Both sRAGE and esRAGE have been identified in the human lungs. As a pattern recognition receptor, RAGE has been implicated in the pathogenesis of various lung diseases such as chronic obstructive pulmonary disease (COPD), acute respiratory distress syndrome (ARDS), and lung cancer.10–12
In this study, we aimed to evaluate the levels of sRAGE in the bronchoalveolar lavage fluid (BALF) that was collected from patients with various inflammatory lung disorders, including interstitial pneumonia, sarcoidosis, respiratory infection, and ARDS. We also examined whether the sRAGE levels in BALF are correlated with other clinical parameters, such as oxygenation index, serum marker levels, and imaging scores of high-resolution computed tomography (HRCT).
Methods
The study protocol was approved by the ethical committee of Keio University School of Medicine (2012–332). This study complied with the principles of the Declaration of Helsinki.
Patient selection
We retrospectively evaluated data from 78 consecutive patients who underwent bronchoalveolar lavage (BAL) at Keio University Hospital during the period from May 2011 to December 2012. Forty-seven (60%) of the study subjects were males, and the mean age was 53.9 ± 1.6 years. The clinical diagnosis included interstitial pneumonia (IIP) in 41 patients, sarcoidosis in 11, respiratory infection in 9, ARDS in 7, vasculitis in 5, and lung cancer in 5. The patients who had received oral corticosteroids or immunosuppressive agents by the time of BAL were excluded. No patient with hypersensitivity pneumonia was included in the IIP group. Because no study subjects underwent surgical lung biopsy, more detailed classification of IIP could not be provided. The diagnosis of vasculitis was usually made by the lung pathology obtained with transbronchial lung biopsy. Otherwise, the diagnosis was made with lung imaging and pathology of other involved organs. Four nonsmoking healthy volunteers served as controls.
Data collection
We reviewed the medical records of all the patients evaluated for demographic, radiographic, BAL, and serum data. Radiographic evaluation included the scoring system using HRCT as previously described.13 In sera, the levels of surfactant protein-D (SP-D), lactate dehydrogenase (LDH), KL-6, and C-reactive protein (CRP) were examined.
BAL procedure and fluid processing for analysis
In most cases, BAL was targeted toward affected lung segments as noted on chest CT. In most cases, the procedure was performed by wedging the bronchoscope in a subsegmental bronchus. Usually, three lavages were performed using 50 mL of 0.9% saline solution per lavage. The recovered fluid was placed on ice immediately. The BALF was pooled and filtered through sterile gauze to remove mucous strands. After the cell count was determined, the BALF was centrifuged at 200 ×g for 5 minutes at 4 °C. The cell pellets were used for the differential counts on Wright-Giemsa-stained preparations. The supernatants were aliquotted and frozen at −80 °C until the measurement.
sRAGE measurement
The levels of sRAGE in the BALF were measured using sandwich enzyme-linked immunosorbent assay kits (R&D Systems). The detection limit was 16.14 pg/mL.
HRCT protocol
All HRCTs were performed with 1.0- or 1.5-mm-thick sections taken at 1-cm intervals throughout the entire thorax and were reconstructed using a high-spatial frequency algorithm. No intravenous contrast was administered. Two experienced pulmonologist (TK and ST) independently evaluated all HRCTs that were obtained 1–4 weeks before BAL. The observers scored ground glass opacity (GGO score) and reticular opacity (fibrosis score) on a scale of 0–5. These scores were also summed into a total CT score. For the purpose of analysis, each lobe was scored by the interpreters, and the mean of all lobes was incorporated into a GGO, fibrosis, and total score for each patient.
Statistical analysis
All data were expressed as the mean ± SE. Among the patient groups with different underlying diseases, differences in the sRAGE levels were compared by the Kruskal–Wallis test using SPSS Windows 15.0 statistical analysis software (SPSS Inc.). The relationships between variables were analyzed by the Spearman rank-order correlation test, and Mann–Whitney U test was used for the group comparison. A value of P < 0.05 was considered to be statistically significant.
Results
sRAGE levels in BALF
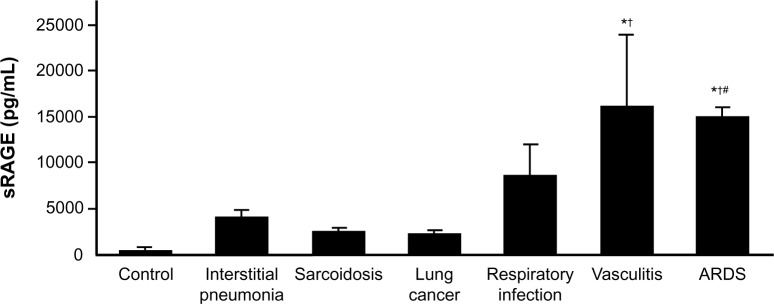
The levels of sRAGE were detected in BALF of 73 patients (94%). The levels of sRAGE and other parameters examined are summarized in Table 1. As shown in Figure 1, the sRAGE levels in BALF were significantly higher in patients with ARDS (P = 0.020) and vasculitis (P = 0.019) when compared with the control subjects. In patients with ARDS, the sRAGE levels in BALF were significantly elevated when compared to those with interstitial pneumonia (P = 0.010) and sarcoidosis (P = 0.014). In patients with vasculitis, the sRAGE concentrations were also increased when compared to those with interstitial pneumonia (P = 0.016). No significant increases in the sRAGE levels in BALF were observed in patients with interstitial pneumonia, sarcoidosis, respiratory infection, and lung cancer when compared with the control subjects.
Table 1.
sRAGE levels and other parameters.
| sRAGE (pg/mL) | 4646.8 ± 579.9 |
| BAL cell | |
| Total cell count (×105/mL) | 7.7 ± 1.0 |
| Differentials | |
| Macrophage (%) | 63.4 ± 2.6 |
| Lymphocyte (%) | 18.6 ± 2.1 |
| Neutrophil (%) | 12.4 ± 1.8 |
| Serum markers | |
| CRP (mg/dL) | 3.4 ± 0.5 |
| LDH (IU/L) | 251.6 ± 11.2 |
| KL-6 (U/mL) | 934.0 ± 88.2 |
| SP-D (ng/mL) | 278.0 ± 29.6 |
| PaO2/FIO2 (Torr) | 395.0 ± 5.8 |
| CT scores | |
| Fibrosis score | 6.4 ± 0.4 |
| GGO score | 2.5 ± 0.5 |
Note: Data expressed as mean ± SE.
Figure 1.
Levels of sRAGE in bronchoalveolar lavage fluid. In patients with ARDS and vasculitis, the sRAGE levels were significantly higher than in the control subjects and those with interstitial pneumonia.
Notes: *P < 0.05 versus control. †P < 0.05 versus interstitial pneumonia. #P < 0.05 versus sarcoidosis.
Correlation between sRAGE and other clinical parameters
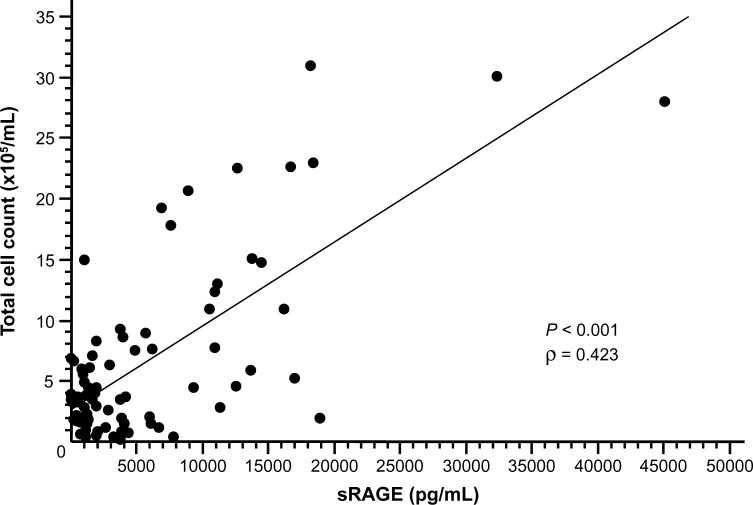
We evaluated the correlation between the sRAGE levels and cell counts in BALF. The sRAGE levels were positively correlated with total cell counts in BALF (P < 0.001, ρ = 0.423; Fig. 2). The levels of sRAGE were correlated with total cell counts in patients with IIP (P < 0.05, ρ = 0.337) and vasculitis (P < 0.05, ρ = 0.468). In contrast, there were no significant correlation between sRAGE level and total cell counts in those with sarcoidosis, lung cancer, respiratory infection, and ARDS. No significant correlation was observed between the sRAGE levels and differential cell counts in BALF (data not shown).
Figure 2.
Correlation between sRAGE levels and total cell counts in bronchoalveolar lavage fluid. The sRAGE levels were positively correlated with total cell counts in BALF (P < 0.001, ρ = 0.423).
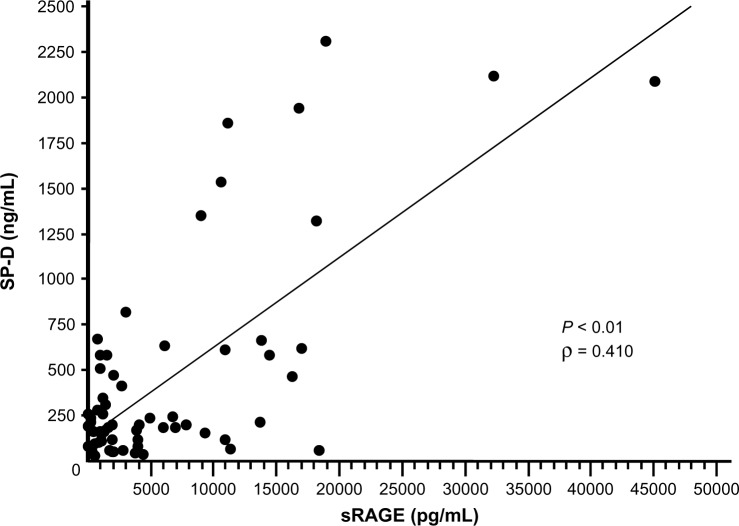
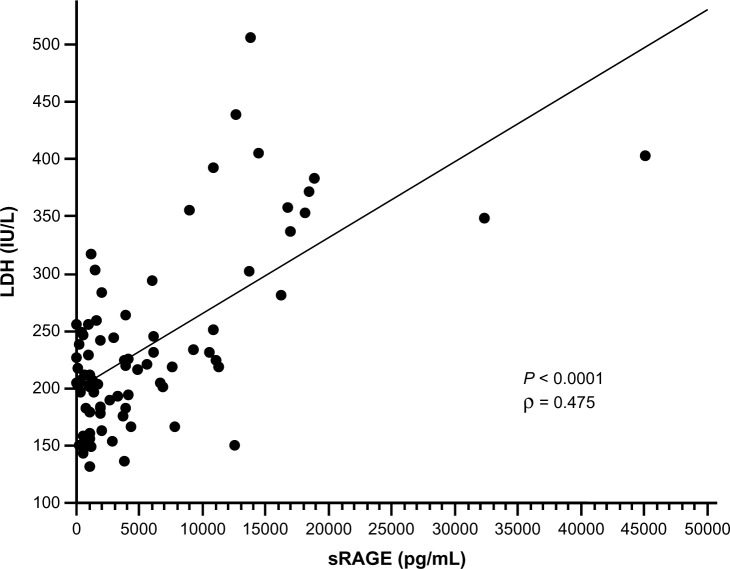
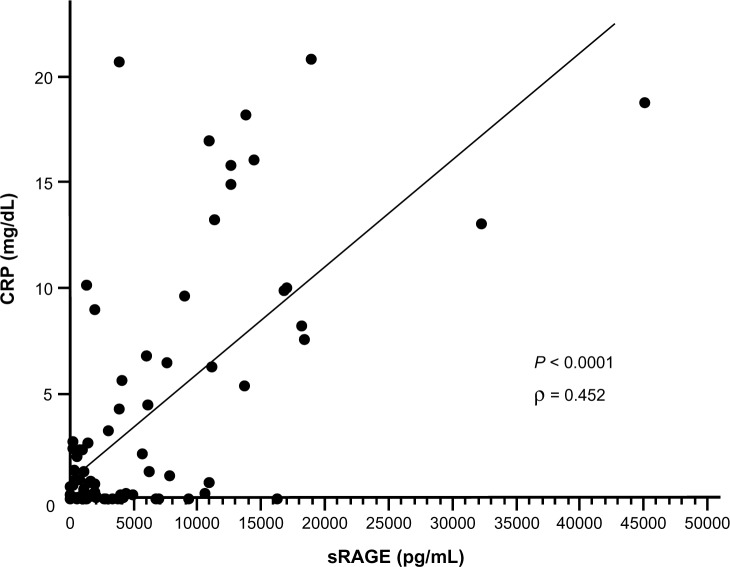
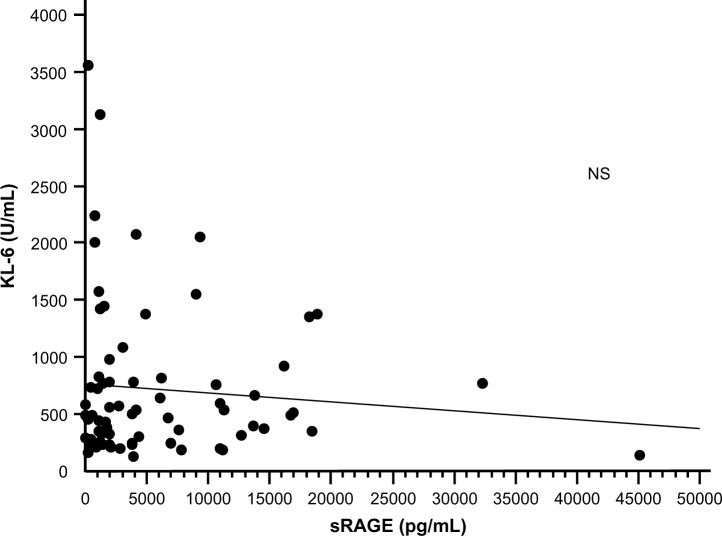
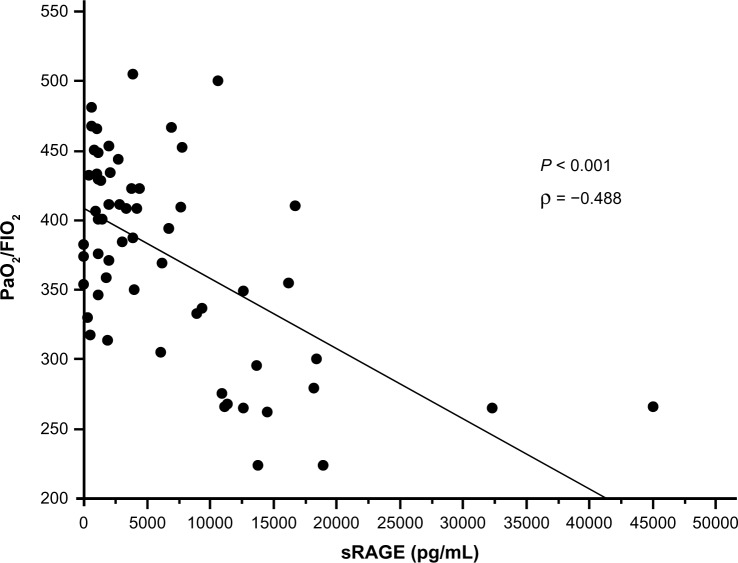
The correlation between the levels of serum markers and the sRAGE levels in BALF was also examined. The sRAGE levels in BALF were positively correlated with the serum levels of SP-D (P < 0.01, ρ = 0.410; Fig. 3). The sRAGE levels in BALF were also correlated with the serum levels of LDH (P < 0.0001, ρ = 0.475; Fig. 4) and CRP (P < 0.0001, ρ = 0.452; Fig. 5). There was no significant correlation between serum KL-6 levels and sRAGE concentrations in BALF (Fig. 6). The oxygenation index, which was determined from the arterial oxygen tension and inspiratory oxygen concentration values, was inversely correlated with the sRAGE levels in BALF (P < 0.001, ρ = −0.488; Fig. 7).
Figure 3.
Correlation between sRAGE levels and serum concentration of SP-D. The sRAGE levels in BALF were positively correlated with the serum levels of SP-D (P < 0.01, ρ = 0.410).
Figure 4.
Correlation between sRAGE levels and serum concentration of LDH. The sRAGE levels in BALF were positively correlated with the serum LDH levels (P < 0.0001, ρ = 0.475).
Figure 5.
Correlation between sRAGE levels and serum concentration of CRP. The sRAGE levels in BALF were positively correlated with the serum CRP levels (P < 0.0001, ρ = 0.452).
Figure 6.
Correlation between sRAGE levels and serum concentration of KL-6. The sRAGE levels in BALF were not significantly correlated with the serum KL-6 levels.
Figure 7.
Correlation between sRAGE levels and oxygenation index. The oxygenation index (PaO2/FIO2) was inversely correlated with the sRAGE levels in BALF (P < 0.001, r = −0.582).
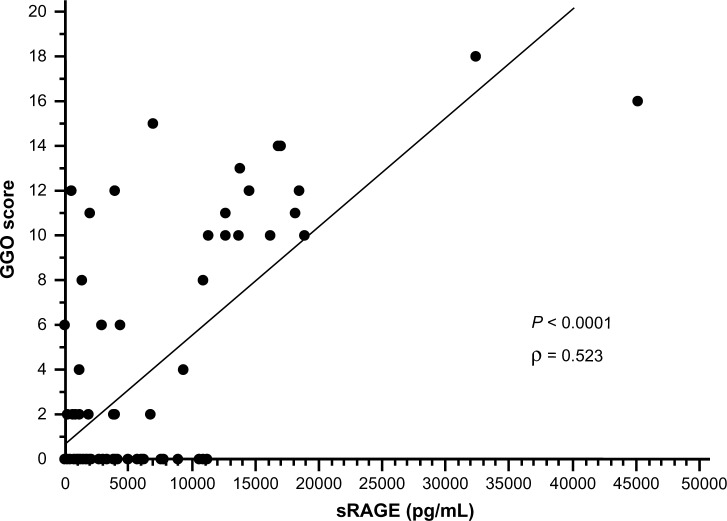
The sRAGE levels in BALF were positively correlated with the GGO scores of HRCT (P < 0.0001, ρ = 0.523; Fig. 8), whereas no significant correlation was observed between the fibrosis scores and sRAGE levels.
Figure 8.
Correlation between sRAGE levels and GGO scores of HRCT. The sRAGE levels in BALF were positively correlated with the GGO scores of HRCT (P < 0.001, r = 0.705).
Although the sRAGE levels were correlated with serum LDH levels in patients with IIP (P < 0.05, ρ = 0.348) and vasculitis (P < 0.05, ρ = 0.539), there were no significant correlation between sRAGE and the clinical parameters in other patient groups.
Discussion
The results of this study have revealed that sRAGE levels are elevated in the alveolar space in patients with ARDS and vasculitis, both of which are characterized with increased permeability of pulmonary vasculature. The levels of sRAGE in BALF were associated with oxygenation impairment and serum markers of lung tissue damage. Although elevated sRAGE levels in injured lungs have been reported, to our knowledge, this is the first study describing the differences in sRAGE levels between the patient groups with various underlying diseases and the association between sRAGE levels and other clinical parameters such as oxygenation index and serum markers.
In this study, the sRAGE levels were correlated with the cell counts in BALF. Besides the role of receptor for AGEs and HMGB-1, RAGE also acts as an endothelial adhesion receptor that mediates interactions with the leukocyte integrin Mac-1 (CD11b/CD18).14 We speculated that sRAGE levels might reflect the expression of RAGE on pulmonary microvascular endothelium, leading to the inflammatory cell accumulation into the alveolar space.
In patients with interstitial pneumonia, the sRAGE levels in BALF were not significantly elevated when compared with those in the control subjects. Kyung et al determined the expression of AGEs and RAGE by the immunofluorescence assay of lung tissues and reported that lungs with idiopathic pulmonary fibrosis (IPF) showed strong expression for both AGEs and RAGE when compared to that in nonspecific interstitial pneumonia and controls.15 Because none of our subjects underwent surgical lung biopsy, no patient had pathologically proven usual interstitial pneumonia (UIP). Among 41 patients with interstitial pneumonia, only 5 showed a UIP pattern on HRCT. The lack of significant elevation of sRAGE levels in those with interstitial pneumonia might be due to the smaller number of patients with IPF.
We observed significant correlation between the sRAGE levels in BALF and SP-D in serum, whereas serum KL-6 levels were not associated with sRAGE levels. Both KL-6 and SP-D are lung-specific proteins secreted primarily by alveolar type II cells, and elevated levels of these markers indicate activation of type II cells in the injured lung.16 It was previously reported that serum levels of KL-6 reflect the overall extent of interstitial lesions on HRCT images, whereas the levels of SP-D mainly reflect the extent of inflammatory lesions.17 In this study, the sRAGE levels were correlated with the GGO score of HRCT, which could reflect the extent of inflammatory lesions. Taken together, sRAGE levels in the alveolar space might be associated with rather inflammatory than fibrotic changes of the lungs.
In this study, we observed that the oxygenation index (PaO2/FIO2) was inversely correlated with the sRAGE levels in BALF (Fig. 4). Calfee et al reported that, in patients with ARDS, higher plasma levels of sRAGE were associated with severity of hypoxemia and increased lung injury scores.18 In experimental lung injury, sRAGE levels in BALF was shown to be much higher than those in plasma, suggesting that the primary source of plasma sRAGE is the alveolar type I cell.12,18 Although we did not measure the plasma sRAGE levels, sRAGE levels in BALF might be a better indicator of alveolar epithelial damage.
RAGE plays a pivotal role, regulating inflammation and epithelial survival in the setting of stress.19 Decreased levels of circulating sRAGE are associated with severity of COPD,20 which might be contradictory to this study. In contrast, there have been several reports describing that higher levels of RAGE are associated with increased severity or poor outcome of lung injury, which is compatible with our findings.12,18 This discrepancy may be owing to the difference in the roles of RAGE in the pathogenesis of various lung disorders.
The major limitation of this study is that sRAGE levels in BALF were measured only at one time point. Although sRAGE levels were correlated with other clinical parameters, its clinical significance remains to be determined in serial measurements. Another limitation is the lack of measurement of sRAGE levels in plasma. Because sRAGE levels were greater in patients with ARDS and vasculitis, both of which are associated with systemic inflammation, it will be a subject of future investigation whether sRAGE levels in BALF correlate with those in plasma. In addition, as the data came from a relatively small number of patients with a variety of underlying diseases, the results could be influenced by possible confounders, such as the age and smoking status of patients.
In summary, the results of the present study indicate that sRAGE levels in BALF were elevated in patients with ARDS and vasculitis and associated with other clinical parameters of inflammatory damage of the lungs. Although further investigation is necessary, sRAGE in BALF might be considered as a biomarker of lung inflammatory disorders, especially ARDS and vasculitis.
Acknowledgments
The authors thank Ms. Miyuki Yamamoto of Keio University School of Medicine for her excellent technical assistance.
Footnotes
ACADEMIC EDITOR: Hussein D. Foda, Editor in Chief
PEER REVIEW: Six peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1,169 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Conceived and designed the experiments: TK, ST. Analyzed the data: TK, ST. Wrote the first draft of the manuscript: TK. Contributed to the writing of the manuscript: ST, YT, SS, TA, KY, HN, MI, NH, TB. Agree with manuscript results and conclusions: TK, ST, YT, SS, TA, KY, HN, MI, NH, TB. Jointly developed the structure and arguments for the paper: TK, ST, YT, SS, TA, KY, HN, MI, NH, TB. Made critical revisions and approved final version: TK, ST, YT, SS, TA, KY, HN, MI, NH, TB. All authors reviewed and approved of the final manuscript.
REFERENCES
- 1.Stern D, Yan SD, Yan SF, Schmidt AM. Receptor for advanced glycation end-products: a multiligand receptor magnifying cell stress in diverse pathologic settings. Adv Drug Deliv Rev. 2002;54:1615–25. doi: 10.1016/s0169-409x(02)00160-6. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt AM, Yan SD, Yan SF, Stern DM. The multiligand receptor RAGE as a progression factor amplifying immune and inflammatory responses. J Clin Invest. 2001;108:949–55. doi: 10.1172/JCI14002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abraham E, Arcaroli J, Carmody A, Wang H, Tracey KJ. HMG-1 as a mediator of acute lung injury. J Immunol. 2000;165:2950–4. doi: 10.4049/jimmunol.165.6.2950. [DOI] [PubMed] [Google Scholar]
- 4.Hofmann MA, Drury S, Fu C, et al. RAGE mediates a novel proinflammatory axis: a central cell surface receptor for S100/calgranulin polypeptides. Cell. 1999;97:889–901. doi: 10.1016/s0092-8674(00)80801-6. [DOI] [PubMed] [Google Scholar]
- 5.Arumugam T, Simeone DM, Schmidt AM, Logsdon CD. S100P stimulates cell proliferation and survival via receptor for activated glycation end products (RAGE) J Biol Chem. 2004;279:5059–65. doi: 10.1074/jbc.M310124200. [DOI] [PubMed] [Google Scholar]
- 6.Bierhaus A, Humpert PM, Morcos M, et al. Understanding RAGE, the receptor for advanced glycation end products. J Mol Med. 2005;83:876–88. doi: 10.1007/s00109-005-0688-7. [DOI] [PubMed] [Google Scholar]
- 7.Raucci A, Cugusi S, Antonelli A, et al. A soluble form of the receptor for advanced glycation endproducts (RAGE) is produced by proteolytic cleavage of the membrane-bound form by the sheddase a disintegrin and metalloprotease 10 (ADAM10) FASEB J. 2008;22:3716–27. doi: 10.1096/fj.08-109033. [DOI] [PubMed] [Google Scholar]
- 8.Yamakawa N, Uchida T, Matthay MA, Makita K. Proteolytic release of the receptor for advanced glycation end products from in vitro and in situ alveolar epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2011;300:L516–25. doi: 10.1152/ajplung.00118.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Demling N, Ehrhardt C, Kasper M, Laue M, Knels L, Rieber EP. Promotion of cell adherence and spreading: a novel function of RAGE, the highly selective differentiation marker of human alveolar epithelial type I cells. Cell Tissue Res. 2006;323:475–88. doi: 10.1007/s00441-005-0069-0. [DOI] [PubMed] [Google Scholar]
- 10.Jing R, Cui M, Wang J, Wang H. Receptor for advanced glycation end products (RAGE) soluble form (sRAGE): a new biomarker for lung cancer. Neoplasma. 2010;57:55–61. doi: 10.4149/neo_2010_01_055. [DOI] [PubMed] [Google Scholar]
- 11.Smith DJ, Yerkovich ST, Towers MA, Carroll ML, Thomas R, Upham JW. Reduced soluble receptor for advanced glycation end-products in COPD. Eur Respir J. 2011;37:516–22. doi: 10.1183/09031936.00029310. [DOI] [PubMed] [Google Scholar]
- 12.Uchida T, Shirasawa M, Ware LB, et al. Receptor for advanced glycation end-products is a marker of type I cell injury in acute lung injury. Am J Respir Crit Care Med. 2006;173:1008–15. doi: 10.1164/rccm.200509-1477OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kazerooni EA, Martinez FJ, Flint A, et al. Thin-section CT obtained at 10 mm increments versus three-level thin-section CT for idiopathic pulmonary fibrosis: correlation with pathologic scoring. AJR Am J Roentgenol. 1997;169:977–83. doi: 10.2214/ajr.169.4.9308447. [DOI] [PubMed] [Google Scholar]
- 14.Pullerits R, Brisslert M, Jonsson IM, Tarkowski A. Soluble receptor for advanced glycation end products triggers a proinflammatory cytokine cascade via β2 integrin Mac-1. Arthritis Rheum. 2006;54:3898–907. doi: 10.1002/art.22217. [DOI] [PubMed] [Google Scholar]
- 15.Kyung SY, Byun KH, Yoon JY, et al. Advanced glycation end-products and receptor for advanced glycation end-products expression in patients with idiopathic pulmonary fibrosis and NSIP. Int J Clin Exp Pathol. 2014;7:221–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Ohnishi H, Yokoyama A, Kondo K, et al. Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. Am J Respir Crit Care Med. 2002;165:378–81. doi: 10.1164/ajrccm.165.3.2107134. [DOI] [PubMed] [Google Scholar]
- 17.Ichiyasu H, Ichikado K, Yamashita A, et al. Pneumocyte biomarkers KL-6 and surfactant protein D reflect the distinct findings of high-resolution computed tomography in nonspecific interstitial pneumonia. Respiration. 2012;83:190–7. doi: 10.1159/000326924. [DOI] [PubMed] [Google Scholar]
- 18.Calfee CS, Ware LB, Eisner MD, et al. NHLBI ARDS Network Plasma receptor for advanced glycation end products and clinical outcomes in acute lung injury. Thorax. 2008;63:1083–9. doi: 10.1136/thx.2008.095588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sparvero LJ, Asafu-Adjei D, Kang R, et al. RAGE (receptor for advanced glycation endproducts), RAGE ligands, and their role in cancer and inflammation. J Transl Med. 2009;7:17. doi: 10.1186/1479-5876-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yonchuk JG, Silverman EK, Bowler RP, et al. Circulating soluble receptor for advanced glycation end products (sRAGE) as a biomarker of emphysema and the RAGE axis in the lung. Am J Respir Crit Care Med. 2015;192:785–92. doi: 10.1164/rccm.201501-0137PP. [DOI] [PubMed] [Google Scholar]