Abstract
Understanding the degree to which eating behaviors, such as disinhibition and restraint, are associated with weight loss and weight loss maintenance could contribute to further refinement of effective weight management intervention strategies. The purpose of this analysis was to examine if these factors mediate weight loss or weight loss maintenance using data from a randomized controlled trial testing a commercial weight loss program that delivered behavioral counseling and structured meal plans including prepackaged foods. Mediation analyses were used to examine whether changes in disinhibition and restraint mediated the relationship between intervention and weight change during initial weight loss (0-6 months), continued weight loss (6-12 months), or weight loss maintenance (12-24 months) phases. Only decreases in disinhibition between baseline and 6 months mediated the intervention effect on initial weight loss. Our results suggest the mediation effects of these eating behaviors are modest and other factors contribute to a larger, more complex long-term weight loss prognosis.
Keywords: Disinhibition, Restraint, Mediation, Commercial Weight Loss Programs, Weight Loss Maintenance, Eating Behavior
Introduction
Successful weight loss and weight loss maintenance remain challenging for many overweight and obese individuals. Behavioral therapy is considered to be a central component of weight loss therapy (Wadden et al., 2012). Behavioral therapy includes counseling participants on techniques such as goal setting and problem solving around moderate energy restriction and increased physical activity. Although participation in behavioral weight loss programs leads to weight loss for many (Butryn et al., 2011) the behavioral mechanisms through which these interventions work are still unclear. Moreover, about half of participants do not achieve a clinically significant weight loss while participating in state-of-the-art programs, and the likelihood of weight regain beyond 12 months remains high (Jeffery et al., 2000; Rock et al., 2010; Unick et al., 2010). Obtaining a better understanding of the behavioral mechanisms underlying successful weight loss and whether such mechanisms vary between the weight loss and weight maintenance phases could support refinement of intervention strategies ultimately leading to improved initial and long-term weight loss outcomes. Among the most compelling behavioral mechanisms are dietary disinhibition and restraint. These dimensions of eating behavior have been associated with weight and weight change in observational studies and weight loss trials (Dalle Grave et al., 2009; Foster et al., 1998). Importantly, these factors have not been fully evaluated as potential mediators of the impact of interventions on weight loss and weight loss maintenance.
Disinhibition, as measured by the commonly used Eating Inventory (EI), has been described as a recurring tendency to overeat in response to one's environment or mood (Stunkard et al., 1985), and is often positively associated with weight status. This includes the lack of ability to control eating when in certain situations, for example, eating too much at social events and the inability to control eating while experiencing certain internal emotions or thoughts wherein eating is a way of coping with emotions or feelings (Niemeier et al., 2007). A number of studies have examined the associations between disinhibition and weight loss or weight loss maintenance. Decreases in total disinhibition have been associated with greater weight loss in overweight and obese treatment-seeking men and women during behavioral weight loss interventions (Dalle Grave et al., 2009; Fogelholm et al., 1999; Foster et al., 1998). Sustained decreases in disinhibition also have been associated with successful weight loss maintenance (Pekkarinen et al., 1996). Conversely, a rise in disinhibition after intervention and successful weight loss has been associated with weight re-gain (Wing et al., 2008). Still, others have found no association between disinhibition and weight loss maintenance after intervention (Vogels et al., 2007). Though not using mediation analysis, one group found that disinhibition decreased after 12 months of intervention and that change in disinhibition during this time also predicted weight loss. This group also measured initials results after only 4 months of intervention and found no effect on disinhibition (Gillison et al., 2015). Only one study has examined disinhibition as a mediator of a behavioral intervention's impact on weight loss and weight loss maintenance (Teixeira et al., 2010). In that study, disinhibition partially mediated 12-month weight change immediately post-intervention and partially mediated weight change at 24 months following a no-intervention phase in a sample of overweight and obese women.
Unlike disinhibition, dietary restraint is thought of as a healthy eating behavior, which is often inversely associated with weight status. Restraint is characterized as concern about or use of strategies to prevent overeating, such as portion control or avoiding unhealthy foods. Restraint has been examined with respect to weight loss and regain. Restraint, as operationalized by the EI, is characterized as adjusting eating behavior after over consuming and being conscious of food choices, but can also include an all-or-nothing approach of strictly following diet plans (Westenhoefer, 1991; Westenhoefer et al., 1999). While disinhibition is most often inversely associated with weight loss, restraint has been shown to be positively associated with weight loss. In fact, higher pre-treatment levels of restraint have been associated with more weight loss over 12 months (Fogelholm et al., 1999). Foster and colleagues showed increases in restraint were associated with greater weight loss over the course of multiple different weight loss interventions in overweight and obese women (Foster et al., 1998). Dalle Grave and colleagues showed that both men and women seeking weight loss treatment demonstrated increased levels of restraint during the weight loss trajectory (Dalle Grave et al., 2009). Increases in total restraint have been associated with improved weight loss maintenance as well. For example, those who had increased dietary restraint during weight loss regained less weight during weight maintenance in studies with overweight or obese participants (Pekkarinen et al., 1996; Vogels et al., 2005, 2007). Others have shown changes in restraint after as little as 4 months of intervention with subsequent changes after 12 months of intervention. However these changes did not predict weight loss outcomes (Gillison et al., 2015). Only one study to date has examined the mediating effect of restraint. In this trial a component of dietary restraint (flexible restraint) did mediate 12-month weight loss immediately post-intervention, an effect that continued through a 24-month weight loss maintenance no-intervention phase that followed the initial active weight loss period (Teixeira et al., 2010).
To build on these findings we examined whether changes in disinhibition or restraint significantly mediate initial weight loss (0 to 6 months), continued weight loss (6-12 months) and/or weight loss maintenance (12-24 months) in a randomized controlled trial testing a commercial weight loss program in women. Examining the degree to which dimensions of eating behaviors, such as disinhibition and restraint, are associated with initial weight loss success and weight loss maintenance could inform further refinement of effective weight management intervention strategies. We hypothesized that decreases in disinhibition and increases in restraint would mediate the intervention's effect on weight loss between baseline and 6 months and between 6 and 12 months. We further hypothesized that maintaining high levels of restraint and low levels of disinhibition between 12 and 24 months would mediate the intervention's effect on weight loss maintenance.
Materials and Methods
Participants and Setting
These analyses were conducted using data from a randomized controlled trial testing the efficacy of a commercial weight loss program (Rock et al., 2010). Overweight and obese adult women from 4 study sites (University of California, San Diego; University of Arizona, Tucson; University of Minnesota, Minneapolis; and Center for Health Research, Kaiser Permanente Center Northwest, Portland, Oregon) were randomized to one of three arms, two of which were intervention arms and one usual care (UC) arm.
Intervention Description
The intervention arms consisted of a multifaceted weight loss program that included in-person or telephone one-to-one counseling, and free-of-charge prepackaged meals during the initial weight loss phase and website and other resources throughout the 2 years. Counseling sessions focused on participants' attitudes and beliefs about weight, food, and physical activity as well as educational advice such as recipes and healthy eating choices at restaurants. Online tools for support were also provided. All prepared foods, counseling and online tools were provided by Jenny Craig Inc. (Carlsbad, California). For the purposes of these analyses, data from the 2 intervention treatment arms were pooled (INT group) given their similar intervention content and the similarity in weight change patterns and change in mediating variables over the 2 years (data not shown). UC participants received print materials, two in-person counseling sessions with a dietetics professional and monthly check-ins. Additional details have been previously published (Rock et al., 2010). Follow-up data were collected in person at 6, 12, and 24 months post randomization. Informed consent was obtained from participants prior to enrollment and all study procedures were approved by the Institutional Review Board at all involved institutions.
Anthropometric Measures
Height and weight were measured by study staff during clinic visits at baseline, 6, 12, and 24 months using standardized protocols. Body mass index (BMI) was calculated as weight in kg divided by height in m2.
Eating Inventory Questionnaire
The 51-item Eating Inventory was administered via self-reported paper survey during regularly scheduled clinic visits at each time point. This measure was designed to assess levels of eating behaviors in three factors, disinhibition (16 items), restraint (21 items), and hunger (14 items). Item responses are summed within each scale. This measure has shown acceptable reliability in previous samples (Stunkard et al., 1985). Only the disinhibition and restraint items are examined in these analyses. In the current sample, raw Cronbach's α were 0.72 and 0.75 respectively for disinhibition and restraint in the full sample at baseline.
Statistical Analyses
First, 2-sample t-tests were used to examine whether there were treatment group differences in the outcome variable (weight) and the potential mediators (disinhibition and restraint) at each time point (baseline, and 6, 12, and 24 months). Three mediation models were conducted to predict (1) initial weight loss (change in weight from baseline to 6 months), (2) continued weight loss (change from 6 to 12 months), and (3) weight loss maintenance or re-gain (change in weight from 12 to 24 months). Change in the mediator variables during these same time frames were tested as potential mediators of the relationship between intervention (yes or no) and weight change. All meditational analyses were conducted following the Baron and Kenny approach which uses a combination of linear regression equations to estimate the effect of the intervention transmitted through the mediators (Baron et al., 1986). In summary, the total impact of the intervention on weight change is first assessed. The indirect effect of the intervention on weight change through the 2 mediation variables is then calculated by summing the product of the intervention effect on each mediator by the relationship between each mediator and weight change. The total effect minus the effect of the intervention on weight change through the mediators leaves the direct effect of the intervention on weight change not transmitted through the intervention. Two-tailed statistical significance of the mediated effects of the intervention on weight change was assessed by calculating 95% confidence intervals using an asymptotic normal distribution method (Preacher et al., 2004). It is important to note that although it is hypothesized that Eating Inventory variables are mediators on the pathway between the intervention and weight change, with mediational analyses, it is also possible that the reverse is true, (that weight change acts as a mediator on the pathway between the intervention and change in Eating Inventory variables.) This limits the inference of causality. All analyses were conducted with SAS statistical software (versions 9.2 and 9.3).
Results
This analysis includes data from 442 participants at baseline, 428 participants at 6 months, 408 participants at 12 months, and 387 participants at 24 months. Dropout rates were similar across groups and ranged from 1% to 9% of the sample. There were no statistically significant differences in baseline characteristics between intervention groups and the usual care group (Table 1). Participant mean (SD) body mass index in kg/m2 was 34 (3) and mean (SD) age in years was 45 (10). Overall, 45% were college graduates, 75% were non-Hispanic white, and 45% had an annual household income of $75,000 or higher. At baseline, there were no significant differences in weight or Eating Inventory factors between the intervention (INT, N=331) or the usual care comparison group (UC, N=111). Mean weight across both groups was 203 ± 24 lbs. Baseline disinhibition score was 9.0 ± 3.4 on a scale of 0-16 and restraint score was 10.0 ± 4.2 on a scale of 0-21, with higher scores indicating higher behavioral responses. The intervention groups had significantly lower average weight at 6 (p<.01), 12 (p<.01), and 24 months (p=.02) as compared to usual care. There were no between group differences in disinhibition at any time point. Restraint was significantly higher in the INT groups at all follow-up time points (6-months, p<.01; 12-months, p=.01; and 24-months, p<.01). There were no significant between-group differences at baseline in any of the disinhibition or restraint subscales. Each of the mediators also showed greater changes between baseline and 6 months (decreases in disinhibition and increases in restraint) in the intervention groups than the comparison group, and these changes were maintained or slightly attenuated over the remaining months (see Table 2).
Table 1. Baseline demographic and Eating Inventory characteristics.
| Overall (N=442) | Intervention (N=331) | Usual Care (N=111) | P-value1 | |
|---|---|---|---|---|
|
|
||||
| Body mass index, M (SD) | 33.9 (3.4) | 33.8 (3.4) | 34.0 (3.2) | 0.66 |
| Age, M (SD) | 44.6 (10.2) | 44.4 (10.1) | 45.3 (10.8) | 0.45 |
| Education, % college graduate | 45 | 44 | 49 | 0.44 |
| Race/Ethnicity, % non-Hispanic white | 74 | 73 | 75 | 0.78 |
| Income, % ≥$75,000 | 45 | 46 | 41 | 0.4114 |
P-values from between groups independent sample t-tests or chi-square testing for baseline differences across groups.
Table 2. Between group differences in primary outcome and hypothesized mediators at baseline, 6-, 12-, and 24-month follow-up measurement points, M (SD).
| Weight, lbs | Disinhibition | Restraint | |
|---|---|---|---|
|
|
|||
| Baseline, N=442 | |||
| INT | 203.6 (23.9) | 9.0 (3.4) | 10.1(4.2) |
| UC | 200.1 (22.9) | 9.1 (3.5) | 9.8 (4.2) |
| p-value | .19 | .85 | .58 |
| 6-Month, N=428 | |||
| INT | 184.1 (24.2) | 7.3(3.4) | 14.7(3.4) |
| UC | 191.9 (23.8) | 8.0 (3.9) | 13.0(4.7) |
| p-value | .005 | .10 | .001 |
| 12-Month, N=408 | |||
| INT | 181.3 (26.6) | 7.9 (3.7) | 14.0(3.7) |
| UC | 192.5 (25.7) | 7.9 (3.9) | 12.2(5.0) |
| p-value | .0003 | .89 | .01 |
| 24-Month, N=387 | |||
| INT | 186.6 (28.7) | 7.8 (3.7) | 13.7(4.3) |
| UC | 194.5 (27.1) | 7.9 (3.8) | 12.2(4.9) |
| p-value | .02 | .83 | .006 |
INT- Intervention groups
UC- Usual care comparison group
Mediation analyses of initial weight loss (baseline to 6 months)
Figure 1 presents the results of the mediation analyses for initial weight loss. As previously reported (Rock et al., 2010), those in the intervention group lost significantly more weight during the first 6 months of the study than those in the usual care group (Pathway C; β=-12.6, p<0.05). During this same time, disinhibition decreased more in the intervention groups (9.0±3.4 to 7.3±3.4) than in the usual care group (9.1±3.5 to 8.0±3.9). The decrease in disinhibition significantly mediated the effect of the intervention on weight change during the initial weight loss phase after controlling for the mediating effect of restraint such that those who had larger decreases in disinhibition demonstrated greater weight loss (Pathway A1B1; β= -0.65, p<0.05). Similarly, greater increases in restraint were observed for those in the intervention groups (10.1±4.2 to 14.7±3.4) compared to the usual care group (9.8±4.2) to 13.0±4.7). However, after controlling for the mediating effects of disinhibition, restraint was not a statistically significant mediator of the interventions effect on weight loss (Pathway A2B2; β= -0.65, p>0.05). Although both disinhibition and restraint combined significantly mediated the intervention's impact on initial weight loss (Pathway A1B1+A2B2; β= -1.81, p<0.05), these variables only partially explained the variation in weight loss during this phase as there was still a significant direct effect of the intervention on weight loss after accounting for changes in disinhibition and restraint (Pathway C′; β=-10.83, p<0.05)
Figure 1. Combined mediated effects of change in disinhibition and change in restraint on the association between the intervention and initial weight change (baseline to 6 months).
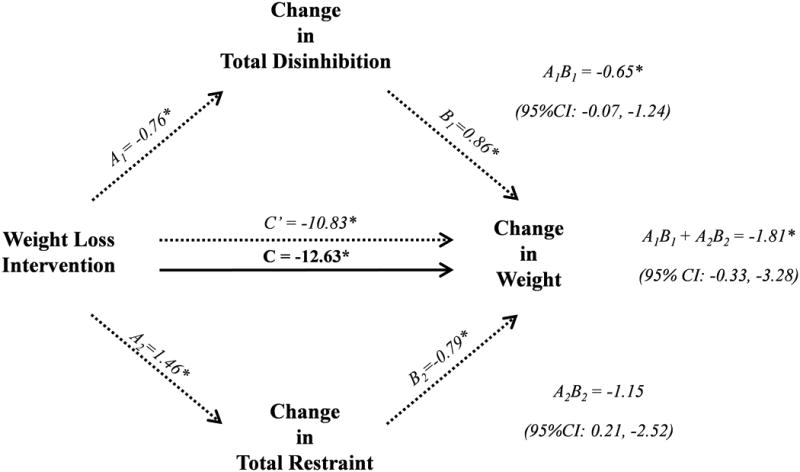
* p < 0.05
Pathway C- the total effect of the intervention on the outcome
Pathway A1 and A2 - the effect of the intervention on the mediator
Pathway B1 and B2 - the relationship of the mediator to the outcome
Pathway C′- the direct effect of the intervention on the outcome not transmitted through the mediators
Mediation analyses of continued weight loss (6 to 12 months)
Between 6 and 12 months of study participation, participants in the intervention groups continued to lose weight while those in the usual care group maintained their weight (Pathway C; β=-2.9, p<0.05). At 12 months, there were no treatment group differences in the disinhibition (Table 2) and disinhibition did not mediate the interventions' effect on continued weight loss after controlling for restraint (Pathway A1B1; β= 0.29, p>0.05). Although the intervention group did have significantly higher restraint scores at 12 months (Table 2), changes in restraint from 6 to 12 months did not mediate continued weight loss during this time after controlling for changes in disinhibition (Pathway A2B2; β= -0.10, p>0.05). Here, the combined mediating effect of restraint and disinhibiton was not statistically significant (Pathway A1B1+A2B2; β= 0.19, p>0.05)
Mediation analyses of weight loss maintenance (12 to 24 months)
Finally, during the weight loss maintenance phase, 12 to 24 months, slight weight regain was observed among intervention group participants, however, intervention group participants continued to weigh significantly less at 24 months compared to usual care group participants (Pathway C; β=-2.9, p<0.05). Between 12 and 24 months, there were no further changes disinhibition (Table 2) and disinhibition did not mediate the intervention's effect on weight regain after controlling for restraint (Pathway A1B1; β= 0.14, p>0.05). Restraint remained stable between 12 and 24 months, and was still higher among intervention group participants relative to usual care group participants (Table 2). Restraint did not mediate the intervention's effect on weight regain after controlling for disinhibition between 12 and 24 months (Pathway A2B2; β= 0.33, p>0.05). Again, the combined mediating effect of restraint and disinhibition was not statistically significant from 12 to 24 months (Pathway A1B1+A2B2; β= 0.47, p>0.05).
Discussion
Developing interventions to support successful weight loss and maintenance in overweight individuals is a public health priority. Understanding the behavioral mechanisms through which weight loss programs work can lead to more efficacious interventions. This study, with ample weight loss, long-term intervention and 24-month follow-up, affords an ideal opportunity to explore such mechanisms (Rock et al., 2010). Both dietary restraint and disinhibition, potentially modifiable behavior mechanisms previously associated with weight loss and maintenance, were evaluated over time in this study. Most importantly, these data provide new insight into the mediating role of these behavioral mechanisms on weight control in a large sample of treatment-seeking women.
Here we show that levels of disinhibition and restraint were associated with intervention randomization and weight at follow-up time points. Similar to previous behavioral weight loss trials, participants in the intervention groups showed greater decreases in measures of disinhibition, greater increases in measures of restraint, and greater weight loss compared to participants in the usual care group during the first 6 months of the study. Because the intervention limited food selections, by way of meal plans and prepackaged foods, it is as expected that dietary restraint was supported in this intervention. Likewise, the provision of meal plans/prepackaged foods is likely to help participants avoid overeating by partially controlling the food environment. This component, paired with the behavioral counseling provided which may have better prepared participants to avoid overeating in other environments, likely explains reductions seen in disinhibition. The magnitude of changes in these behavioral variables during the initial weight loss period (baseline to 6 months) was similar to the magnitude of changes seen by Teixeira and colleagues after 12 months of intervention in women with similar demographic characteristics (Teixeira et al., 2010). In contrast, disinhibition, but not restraint was a mediator of the current intervention's impact on weight loss at 6 months, whereas Teixeira and colleagues found both disinhibiton and components of restraint to be a mediator of 12-month weight loss. The current data suggest that an intervention's ability to diminish the lack of control in overeating in various situations or emotional states may be an important key in initial weight loss. These data also suggest that reducing these “negative” dietary behaviors may be even more important than improving “positive” dietary behaviors. This is the first study to examine disinhibition and restraint as mediators of initial weight loss, as characterized by the first 6 months of intervention.
Between month 6 and 12, participants in the intervention groups continued to lose weight at a slower rate relative to the initial weight loss phase whereas weight stabilized among usual care group participants. In a similar pattern, little additional change in disinhibition or restraint was reported among intervention participants during this time period. These changes in disinhibition and restraint did not act as mediators of the intervention impact on continued weight loss. This finding may have a number of implications. Although the intervention strategies (behavioral counseling and providing prepackaged foods) lead to modified and maintained initial changes in these dietary behaviors, additional or different strategies may be needed to help participants with continued improvements. Similarly, no additional improvements in dietary behaviors or weight loss were seen between 12 and 24 months. In fact, slight weight regain occurred among intervention group participants, although body weight was still lower than usual care participants' weight at 24 months. Also, levels of disinhibiton and restraint began to revert for those in the intervention groups, although still not to baseline levels. This could be in part due to the encouragement of participants to move away from pre-packaged meals later in the intervention and toward their own food choices. These results could also be explained by shifts in participant use of behavioral counseling throughout 24 months. Future work should examine the impact of changes in utilization of intervention components on dietary behaviors. The slight shifts seen in dietary behaviors from 6 to 12 and 12 to 24 months were not significant mediators of weight changes during these same times. This is the first study to examine further change in dietary behavior mediators between 6 and 12 and 12 and 24 months.
Another important aspect of these results is the magnitude of the mediating effects. From baseline to 6 months, the combined mediating effect of changes in disinhibition and restraint, although statistically significant and clinically meaningful, only explained a small portion of the total weight loss. Decreases in disinhibition and increases in restraint together accounted for about 2 pounds of the average 13-pound intervention-induced weight loss between baseline and 6 months (β=-1.81, 95% CI: -0.33 to -3.28). Although the combination of changes in restraint and disinhibition may be a meaningful mediator of initial weight loss, there are clearly other behavioral mechanisms associated with intervention effects on weight. Further exploration to identify additional mediators of successful weight loss and weight loss maintenance interventions is an important next step.
Exploring differences in theoretical frameworks and behavior change techniques used across interventions may give insight into new mediators. But, interestingly, the intervention group changes in disinhibition and restraint shown in the current analyses were similar in magnitude to changes demonstrated in another behavioral weight loss intervention that focused on autonomous decision making with less structure around meals (Teixeira et al., 2010). Additionally, similar amounts of initial weight loss and subsequent weight regain have also been observed across multiple interventions (Teixeira et al., 2010; Westenhoefer et al., 2013). Although these interventions share commonalities in theory, modality, duration, etc. the specific techniques, interventionist training and background, and intensity (weekly, monthly) with which they are delivered can vary a great deal. That similar patterns in restraint, disinhibition, and weight change are seen across these diverse interventions leads to the need for novel theories, techniques, or intervention designs to push the envelope on weight loss research. Identifying mediators of weight loss and weight loss maintenance can facilitate the design of more efficacious weight loss and maintenance intervention strategies.
It is important to note that in these secondary mediation analyses, temporality is not established and it is therefore not possible to determine if changes in the assumed mediators precede and/or cause changes in weight. It is plausible that the reverse is true, changes in weight lead to changes in mediators during a given time period or that another third factor is mediating the intervention impact on both weight change and concurrent change in EI variables. However, these analyses do shed light onto which factors may be important in weight loss and weight loss maintenance and allow us to generate testable hypotheses when designing innovative trials in the future. Furthermore, these findings were from a study of relatively homogeneous (with respects to race, ethnicity and socio-economic status) treatment-seeking women. This limits the generalizability of the findings and provides opportunity to explore potential replication of results findings in more diverse populations. Finally, these analyses were unable to tease apart the effects of specific intervention components (e.g., behavioral counseling or prepackaged foods). Examining the variability in intervention delivery or utilization of these specific components across participants and subsequent changes in dietary behaviors and weight change is an exciting area for future work.
Acknowledgments
This trial was registered at clinicaltrials.gov, NCT00640900. This study was supported by Jenny Craig Inc. (Carlsbad, California), which provided program activities, materials, and prepackaged foods to individuals assigned to the commercial weight loss program. Funding was provided through a clinical trial contract to the coordinating center (School of Medicine, University of California, San Diego), which subsequently disbursed funds to the collaborating clinical sites and the laboratories. Data from the clinical sites and the laboratories were forwarded to the coordinating center where they were pooled for analysis. Jenny Craig Inc. had a minimal role in the design and protocol development. By contractual agreement, scientists at the University of California, San Diego, and the other participating institutions had responsibility and independence regarding data management, analysis, and publication. The funding sponsor had no role in the collection, analysis, or interpretation of the data; or in the preparation, review or approval of the manuscript.
Footnotes
Conflicts of Interest: Authors MMJ, NES, SWF, CRP, CAT, BP, and CLR declare no conflicts of interest. Informed consent was obtained from all patients for being included in the study.
Contributor Information
Meghan M. JaKa, Email: Meghan.M.Senso@HealthPartners.com.
Nancy E. Sherwood, Email: Nancy.E.Sherwood@HealthPartners.com.
Shirley W. Flatt, Email: sflatt@ucsd.edu.
Carly R. Pacanowski, Email: cpacanow@umn.edu.
Bilgé Pakiz, Email: bpakiz@ucsd.edu.
Cynthia A. Thomson, Email: cthomson@email.arizona.edu.
Cheryl L. Rock, Email: clrock@ucsd.edu.
References
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am. 2011;34(4):841–859. doi: 10.1016/j.psc.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalle Grave R, Calugi S, Corica F, Di Domizio S, Marchesini G. Psychological variables associated with weight loss in obese patients seeking treatment at medical centers. J Am Diet Assoc. 2009;109(12):2010–2016. doi: 10.1016/j.jada.2009.09.011. [DOI] [PubMed] [Google Scholar]
- Fogelholm M, Kukkonen-Harjula K, Oja P. Eating control and physical activity as determinants of short-term weight maintenance after a very-low-calorie diet among obese women. Int J Obes Relat Metab Disord. 1999;23(2):203–210. doi: 10.1038/sj.ijo.0800825. [DOI] [PubMed] [Google Scholar]
- Foster GD, Wadden TA, Swain RM, Stunkard AJ, Platte P, Vogt RA. The Eating Inventory in obese women: clinical correlates and relationship to weight loss. Int J Obes Relat Metab Disord. 1998;22(8):778–785. doi: 10.1038/sj.ijo.0800659. [DOI] [PubMed] [Google Scholar]
- Gillison F, Stathi A, Reddy P, Perry R, Taylor G, Bennett P, Greaves C. Processes of behavior change and weight loss in a theory-based weight loss intervention program: a test of the process model for lifestyle behavior change. International Journal of Behavioral Nutrition and Physical Activity. 2015;12(1) doi: 10.1186/s12966-014-0160-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeffery RW, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill DR. Long-term maintenance of weight loss: current status. Health Psychol. 2000;19(1 Suppl):5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- Niemeier HM, Phelan S, Fava JL, Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity (Silver Spring) 2007;15(10):2485–2494. doi: 10.1038/oby.2007.295. [DOI] [PubMed] [Google Scholar]
- Pekkarinen T, Takala I, Mustajoki P. Two year maintenance of weight loss after a VLCD and behavioural therapy for obesity: correlation to the scores of questionnaires measuring eating behaviour. Int J Obes Relat Metab Disord. 1996;20(4):332–337. [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Rock CL, Flatt SW, Sherwood NE, Karanja N, Pakiz B, Thomson CA. Effect of a free prepared meal and incentivized weight loss program on weight loss and weight loss maintenance in obese and overweight women: a randomized controlled trial. JAMA. 2010;304(16):1803–1810. doi: 10.1001/jama.2010.1503. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Silva MN, Coutinho SR, Palmeira AL, Mata J, Vieira PN, Sardinha LB. Mediators of weight loss and weight loss maintenance in middle-aged women. Obesity (Silver Spring) 2010;18(4):725–735. doi: 10.1038/oby.2009.281. [DOI] [PubMed] [Google Scholar]
- Unick JL, Jakicic JM, Marcus BH. Contribution of behavior intervention components to 24-month weight loss. Med Sci Sports Exerc. 2010;42(4):745–753. doi: 10.1249/MSS.0b013e3181bd1a57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogels N, Westerterp-Plantenga MS. Categorical strategies based on subject characteristics of dietary restraint and physical activity, for weight maintenance. Int J Obes (Lond) 2005;29(7):849–857. doi: 10.1038/sj.ijo.0802984. [DOI] [PubMed] [Google Scholar]
- Vogels N, Westerterp-Plantenga MS. Successful long-term weight maintenance: a 2-year follow-up. Obesity (Silver Spring) 2007;15(5):1258–1266. doi: 10.1038/oby.2007.147. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity new developments in diet, physical activity, and behavior therapy. Circulation. 2012;125(9):1157–1170. doi: 10.1161/CIRCULATIONAHA.111.039453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westenhoefer J. Dietary restraint and disinhibition: is restraint a homogeneous construct? Appetite. 1991;16(1):45–55. doi: 10.1016/0195-6663(91)90110-e. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J, Engel D, Holst C, Lorenz J, Peacock M, Stubbs J, Raats M. Cognitive and weight-related correlates of flexible and rigid restrained eating behaviour. Eat Behav. 2013;14(1):69–72. doi: 10.1016/j.eatbeh.2012.10.015. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J, Stunkard AJ, Pudel V. Validation of the flexible and rigid control dimensions of dietary restraint. Int J Eat Disord. 1999;26(1):53–64. doi: 10.1002/(sici)1098-108x(199907)26:1<53::aid-eat7>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Wing RR, Papandonatos G, Fava JL, Gorin AA, Phelan S, McCaffery J, Tate DF. Maintaining large weight losses: the role of behavioral and psychological factors. J Consult Clin Psychol. 2008;76(6):1015–1021. doi: 10.1037/a0014159. [Research Support, N.I.H., Extramural] [DOI] [PMC free article] [PubMed] [Google Scholar]


