Abstract
Background
Hepatic splenosis is rare condition, preceded by splenectomy or spleen trauma, the term refers to nodular implantation of normal splenic tissue in the liver. In patients with history of malignancy in particular, it can be mistaken for metastases and can lead to unnecessary diagnostic procedures or inappropriate treatment.
Case report
Twenty-two-year old male was treated for immature teratoma linked to undescended right testicle after birth. On regular follow-up examinations no signs of disease relapse or long-term consequences were observed. He was presented with incidental finding of mature cystic teratoma after elective surgery for what appeared to be left-sided inguinal hernia. The tumour was most likely a metastasis of childhood teratoma. Origin within remaining left testicle was not found. Upon further imaging diagnostics, several intrahepatic lesions were revealed. Based on radiologic appearance they were suspicious to be metastases. The patient underwent two ultrasound guided fine-needle aspiration biopsies. Cytologic diagnosis was inconclusive. Histology of laparoscopically obtained tissue disclosed presence of normal splenic tissue and led to diagnosis of hepatic splenosis.
Conclusions
Though hepatic splenosis is rare, it needs to be included in differential diagnosis of nodular hepatic lesions. Accurate interpretation of those lesions is crucial for appropriate management of the patient. If diagnosis eludes after cytologic diagnostics alone, laparoscopic excision of nodular lesion is warranted before considering more extensive liver resection.
Key words: hepatic splenosis, teratoma, metastases, laparoscopy
Introduction
Ectopic spleen tissue takes two forms, it is either congenital and presents as accessory spleens or an acquired condition, called splenosis. Splenosis occurs as un-encapsulated splenic tissue localized outside the spleen. It is a benign condition, most commonly linked to splenic trauma or splenectomy. Post traumatic splenosis is believed to be a rare state; however, it is more likely only to be under-recognized. Patients are in fact most often asymptomatic and the majority of cases are diagnosed by coincidence.1
As a rule, there are multiple splenic tissue implants embedded in serous surfaces of abdominal cavity such as mesentery, omentum, surfaces of the colon or diaphragm. After penetrating abdominal trauma, extraperitoneal splenosis has also been reported in subcutaneous tissue, pleural cavity or pericardium.2-5
Rarely, splenic tissue can implant in parenchyma of a visceral organ such as liver. In that case, the condition is defined as hepatic splenosis. Mechanism of splenic tissue spread is not completely understood. One of the hypotheses postulates invagination of splenic implants into sub-capsular area of the liver after spleen trauma. Alternatively, deep-seated hepatic splenic nodules would results from the microembolisation via the splenic vein. Nodular lesions in liver parenchyma are non-specific on imaging and can mimic malignant as well as benign lesions.6 Exploratory laparoscopy is the least invasive method for reaching definitive diagnosis and is the most suitable, especially in patients with history of malignant disease where liver metastases are suspected.
Case report
A 22-year old Caucasian male was presented after operative procedure due to left-sided inguinal hernia, during which a cystic mass inside of hernial sac was revealed. Histology of the tumour disclosed it to be mature cystic teratoma.
The patient was treated for immature teratoma with a prevalence of neuroepithelial components and with high mitotic activity 22 years prior and the tumour most likely originated from retained right testicle. Surgical procedure was performed on day 6 after birth. The tumour had perforated and was macroscopically removed. He received 3 cycles of chemotherapy with vincristine, actinomycin D, cyclophosphamide and cisplatin in the adjuvant setting. On follow-up examinations there were no signs of relapse. At the age of 4 he underwent splenectomy after a motor vehicle accident. For the past year he had been treated for Henoch–Schönlein purpura with renal impairment, he was receiving methylprednisolone.
After the operative procedure for hernia, patient’s alpha-fetoprotein (AFP), Beta unit of human Chorionic Gonadotropin (Beta hCG) and Lactate dehydrogenase (LDH) levels were within normal ranges: AFP 2.2 kU/L (< 5.8), Beta hCG < 0.1 U/L (< 2.0), LDH 2.25 ukat/L (< 4.13). Additional laboratory testing revealed thrombocyte count 491 *109 /L (140–340), neutrophil count 77.7% (40–75%), lymphocyte count 17.3% (20–40%), eosinophil count 0.7% (1–6%), and sedimentation rate 29 mm/h (< 19). Electrolyte concentrations, liver function tests, LDH and thyroid hormones were within normal limits.
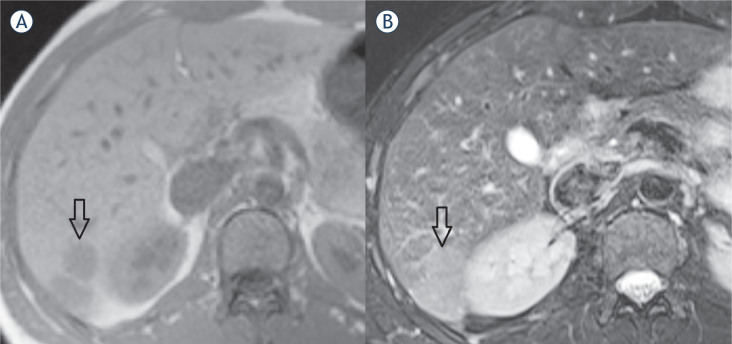
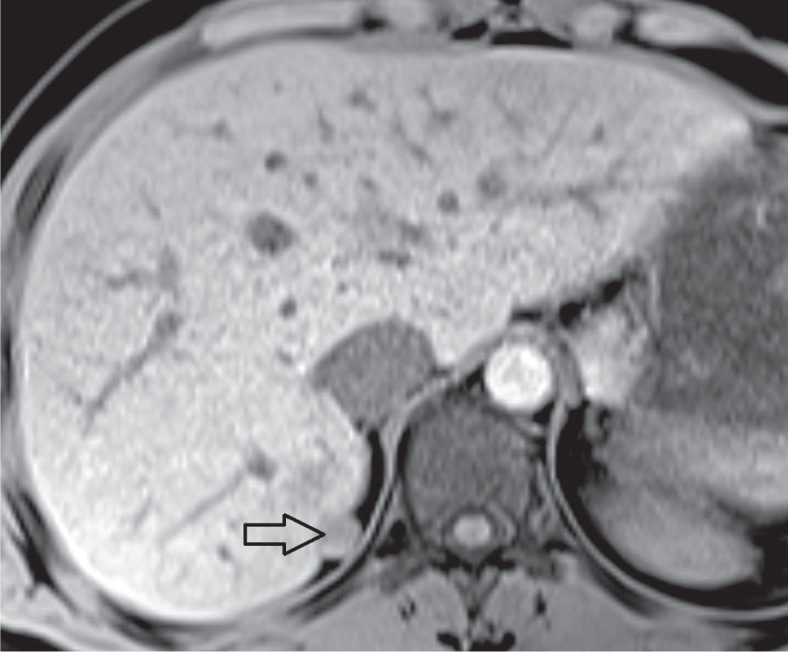
Imaging diagnostics were performed for disease staging. Scrotal ultrasound revealed small left-sided hydrocele, and no suspicious lesions in left testicle. Left epididymis seemed appropriate. Computed tomography (CT) scan of thoracic organs demonstrated no signs of disease progression. However, on abdominal CT scan two poorly demarcated areas in the 6th liver segment and under the capsule were seen in portal phase of contrast enhancement (Figure 1). There was also small perihepatic oval shaped peritoneal solid lesion of same appearance. Liver size was normal.
Figure 1.
CT; portal phase of contrast enhancement - subtle hypodense lesions in 6th liver segment.
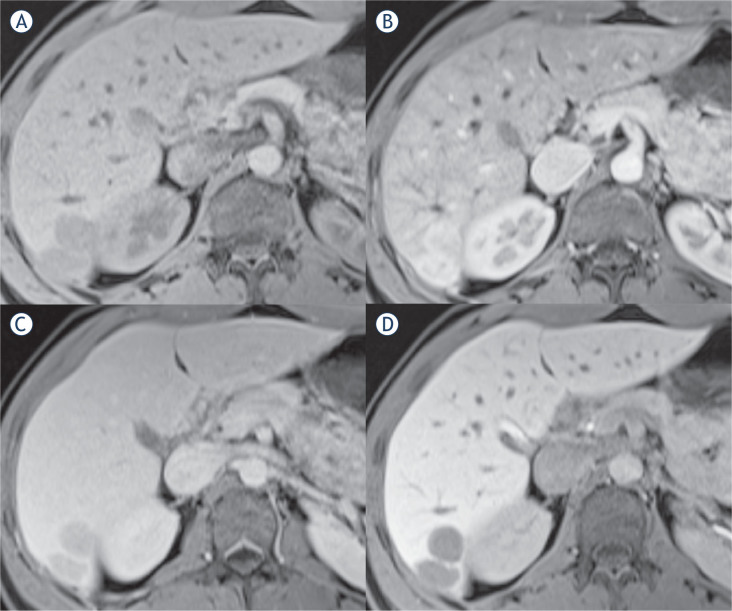
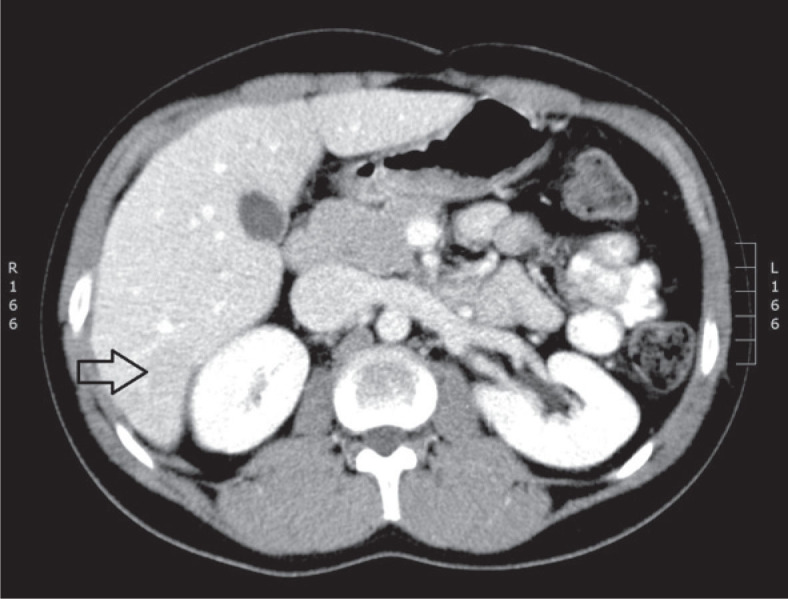
With a view to define perihepatic lesions, magnet resonance imaging (MRI) with hepatospecific contrast medium (Gd-EOB-DTPA disodium, i.e. Primovist, Bayer Pharma AG) was performed. Five round lesions ranging from 0.7 to 2.6 cm in diameter were visible in 2nd, 6th segment and on the border of 6th and 7th segment. They were subcapsularly in liver parenchyma and on the surface of the liver. Lesions were hypointense in T1 weighted images (WI), slightly hyperintense in T2 WI, after administration of hepatospecific contrast medium enhanced during arterial phase, after that they remained hypointense in the late phase images (Figures 2‒4). Lesions were suspected to be metastases.
Figure 2.
MRI; (A)hypointense hepatic lesion in T1 weighted image (WI); (B)T2 fast spin echo (FSE) WI: slightly high signal intensity of hepatic lesion.
Figure 4.
Perihepatic lesion in pre-contrast T1 volume interpolated breathhold examination (VIBE) fat saturated (FS).
Figure 3.
MRI; hepatic lesions in T1 volume interpolated breathhold examination (VIBE) fat saturated (FS); (A) pre-contrast; (B)arterial phase; (C) portal phase; (D) delayed phase (20 minutes) of enhancement.
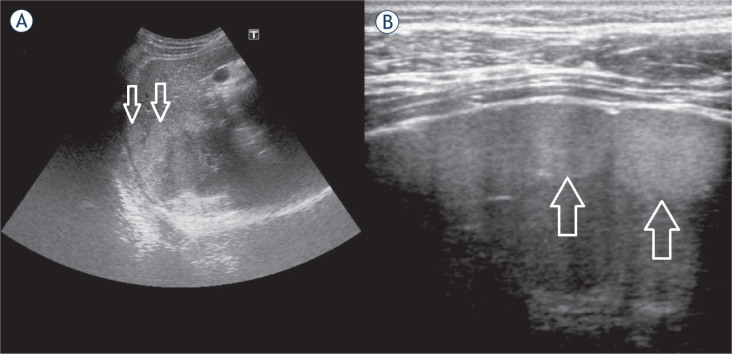
The patient underwent two ultrasound guided fine-needle aspiration biopsies. Sonographically lesions were barely seen, mildly hyperechoic (Figure 5). Obtained samples were unfit to warrant a cytologic diagnosis.
Figure 5.
US; mildly hyperechoic subcapsular hepatic lesions; (A)abdominal probe; (B)high frequency linear probe.
In order to verify suspicious lesions, laparoscopic excision was carried out and intraoperative frozen section analysis evinced spleen tissue. Histology of the obtained sample confirmed hepatic splenosis.
Tumour, a coincidental finding at operative procedure in left inguinal region, was most likely a metastasis of childhood germ cell tumour. There were no signs of disease spread. Treatment of asymptomatic hepatic splenosis was not indicated.
Discussion
Hepatic splenosis is heterotopic autotransplantation of splenic tissue, as a rule it is a consequence of spleen trauma or splenectomy carried out from other reasons. Ectopic splenic tissue in abdominal cavity is present in more than 60% of patients after traumatic splenic rupture; however, isolated hepatic localization is described only in individual cases.6-10 The diagnosis is usually an incidental finding following diagnostics in the scope of another disease, as patients are most often asymptomatic. Mescoli et al. report an average time of 29 years between splenectomy and the liver nodules detection.6 The patient in our report underwent splenectomy 18 years before the hepatic splenosis was established. He was subjected to regular follow- up after the treatment for childhood immature teratoma, and intermittent abdominal sonography revealed no lesions in hepatic parenchyma.
However, none of the imaging techniques is specific enough to identify hepatic splenosis; ultrasound sensitivity is very poor, CT imaging is moderately sensitive and MRI has high sensitivity. Hypervascular nodular hepatic lesions are most commonly haemangioma, hepatic metastases, hepatic adenoma, focal nodular hyperplasia, hepatocellular carcinoma.11 Strictly peripheral lesions in hepatic parenchyma with peritoneal deposits in spleenless patient should warrant differential diagnosis of splenosis. With respect to childhood tumour, hepatic metastases and/or peritoneal dissemination seemed a plausible differential diagnostic option in presented case. The patient was subjected to operative treatment for abdominal tumour few days after birth. Tumour was linked to undescended right testicle and was histologically diagnosed to be immature teratoma. Data shows a link between intraabdominal teratoma and cryptorchidism in children, also, tumour localization at the annulus inguinalis profundus is believed to cause testicular retention.12 Mature teratoma presenting in our patient’s adulthood was considered to be a metastasis of primary childhood tumour and less likely metastatic germ cell tumour originating in left testicle. It is known that contralateral testicular tumour is more often found in patients with history of teratoma and in situ disgenesis is present in 9% of the patients.13 However, clinical examination, biochemistry and imaging excluded left testicle pathology with high probability.
Considering differential diagnosis, nodular hepatic and perihepatic lesions could reflect metastases of immature childhood teratoma as well as mature adulthood teratoma. Immature teratomas are known to metastasize to the solid organs, including liver. Metastatic foci can contain histologically more mature elements than found in primary tumour. One of the reasons is retroconversion of metastases to differentiated mature teratoma under the influence of chemotherapy.14 Mature teratomas are usually asymptomatic and slow growing, 1.8 mm per year on average. That explains the longtime interval between primary tumor management after birth and finding the mature teratoma at the age of 22 in our case. Also, slow growth could explain presence of nodular hepatic lesions, assessed as possible metastases. On the other hand, the origo of metastases could be the adulthood teratoma, as malignant alteration and metastasizing occur in 1 to 2% of mature teratomas.15
Differential diagnosis of hepatic splenosis is wide and indirect diagnostic procedures are unreliable as opposed to histologic evaluation. Hematological evaluation can be useful in assessing any persistence of functioning splenic tissue and the absence of Howell-Jolly bodies, Heinz bodies or pitted cells on blood smears may be helpful in diagnosing splenosis. However, sensitivity of the test is low, especially when there is only small amount of ectopic splenic tissue.
There are no typical radiological features of intrahepatic splenosis. Sonographic appearance is completely unspecific, similar to the current case. Hypoechoic, homogeneous, solid and well circumscribed implants are described in literature, however, in our case lesions were sonographically mildly hyperechoic.10 In contrast-enhanced CT scans, intrahepatic splenosis is generally revealed as round, oval, or lobular, well circumscribed, non-calcified and homogeneously enhancing. Before injection of contrast medium the implants are usually hypodense or isodense to the liver. In the literature, there are few published descriptions of hepatic splenosis on MRI.10,16-21
On MRI, the characteristics of splenosis are limited to anecdotal cases that have found such lesions as homogeneous, of low signal intensity in T1 WI and moderately hyperintense in T2 WI. Sometimes hypointense thin layer of capsule around the lesion is found in T1 and T2 WI. In arterial or/and portal phase of enhancement lesions are mostly hyper-vascular and hypointense in delayed images.17
According to published reports intrahepatic splenosis is most commonly manifested as nodular, solitary lesions, and ranging from 2 to 6 cm in size.6,8,10 Described characteristics are true in our case with the exception of the number of lesions. In contrast with presented case Mescoli et al. reported that solitary splenic nodules were found in 24 out of 27 patients with the hepatic splenosis. In only one patient more than three nodular lesions were found.6 Difference may stem from an underestimation of the results based on radiological investigations. In our case five intrahepatic implants were identified with MRI and two with CT, what is in concordance with multiple studies, which have shown that MRI is superior to CT in sensitivity and accuracy of detecting hepatic lesions.22 Upon ultrasonography the lesions were particularly indistinguishable and mildly hiperechoic. In the literature, all the lesions were described as hypoechoic.
Splenosis is thought to be uncommon, but the incidence is probably underreported since the majority of patients are asymptomatic. Distinguishing the aetiology of hepatic nodular lesions is important because it significantly alters therapeutic procedures. Typical imaging modalities such as US, CT or MRI will not differentiate splenosis from other entities and a histologic specimen needs to be obtained to reach definitive diagnosis. Unfortunately, result of fine-needle aspiration biopsy can be inconclusive as it was in presented case. On the other hand, laparotomy is an excessive operational procedure with potential complications in patients with hepatic splenosis. We presented a case in which hepatic splenosis has been confirmed by explorative laparoscopy. A laparoscopic approach is minimally invasive for the visualization of suspected intrahepatic masses, and allows access for potential liver biopsy or resection. Similar experiences have been described, but in only few published reports.9,23
Conclusions
Due to the significant impact on treatment decisions intrahepatic splenosis must be considered in the diagnostic spectrum of nodular liver lesions, especially in patients with prior splenic trauma or surgery.
Disclosure: No potential conflicts of interest were disclosed.
References
- 1.Fleming CR, Dickson ER, Harrison EG Jr. Splenosis: autotransplantation of splenic tissue. Am J Med 1976; 61: 414-19. [DOI] [PubMed]; Fleming CR, Dickson ER, Harrison EG Jr. Splenosis: autotransplantation of splenic tissue. Am J Med. 1976;61:414–19. doi: 10.1016/0002-9343(76)90380-6. [DOI] [PubMed] [Google Scholar]
- 2.Brewster DC. Splenosis. Report of two cases and review of the literature. Am J Surg 1973; 126: 14-9. [DOI] [PubMed]; Brewster DC. Splenosis. Report of two cases and review of the literature. Am J Surg. 1973;126:14–9. doi: 10.1016/s0002-9610(73)80086-8. [DOI] [PubMed] [Google Scholar]
- 3.Bock DB, King BF, Hezmall HP, Oesterling JE. Splenosis presenting as a left renal mass indistinguishable from renal cell carcinoma. J Urol 1991; 146:152-4. [DOI] [PubMed]; Bock DB, King BF, Hezmall HP, Oesterling JE. Splenosis presenting as a left renal mass indistinguishable from renal cell carcinoma. J Urol. 1991;146:152–4. doi: 10.1016/s0022-5347(17)37737-6. [DOI] [PubMed] [Google Scholar]
- 4.Grantham JR, Clore FC. Subcutaneous splenosis. AJR Am J Roentgenol 1990; 154: 655. [DOI] [PubMed]; Grantham JR, Clore FC. Subcutaneous splenosis. AJR Am J Roentgenol. 1990;154:655. doi: 10.2214/ajr.154.3.2106240. [DOI] [PubMed] [Google Scholar]
- 5.Normand JP, Rioux M, Dumont M, Bouchard G, Letourneau L. Thoracic splenosis after blunt trauma: frequency and imaging findings. AJR Am J Roentgenol 1993; 161: 739-41. [DOI] [PubMed]; Normand JP, Rioux M, Dumont M, Bouchard G, Letourneau L. Thoracic splenosis after blunt trauma: frequency and imaging findings. AJR Am J Roentgenol. 1993;161:739–41. doi: 10.2214/ajr.161.4.8372748. [DOI] [PubMed] [Google Scholar]
- 6.Mescoli C, Castoro C, Sergio A, Ruol A, Farinati F, Rugge M. Hepatic spleen nodules (HSN). Scand J Gastroenterol 2010; 45: 628-32. [DOI] [PubMed]; Mescoli C, Castoro C, Sergio A, Ruol A, Farinati F, Rugge M. Hepatic spleen nodules (HSN) Scand J Gastroenterol. 2010;45:628–32. doi: 10.3109/00365521003587812. [DOI] [PubMed] [Google Scholar]
- 7.Livingston CD, Levine BA, Lecklitner ML, Sirinek KR. Incidence and function of residual splenic tissue following splenectomy for trauma in adults. Arch Surg 1983; 118: 617-20. [DOI] [PubMed]; Livingston CD, Levine BA, Lecklitner ML, Sirinek KR. Incidence and function of residual splenic tissue following splenectomy for trauma in adults. Arch Surg. 1983;118:617–20. doi: 10.1001/archsurg.1983.01390050083016. [DOI] [PubMed] [Google Scholar]
- 8.D’Angelica M, Fong Y, Blumgart LH. Isolated hepatic splenosis: first reported case. HPB Surg 1998; 11: 39-42. [DOI] [PMC free article] [PubMed]; D’Angelica M, Fong Y, Blumgart LH. Isolated hepatic splenosis: first reported case. HPB Surg. 1998;11:39–42. doi: 10.1155/1998/72067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abu Hilal M, Harb A, Zeidan B, Steadman B, Primrose JN, Pearce NW. Hepatic splenosis mimicking HCC in a patient with hepatitis C liver cirrhosis and mildly raised alpha feto protein; the important role of explorative laparoscopy. World J Surg Oncol 2009; 7: 1. [DOI] [PMC free article] [PubMed]; Abu Hilal M, Harb A, Zeidan B, Steadman B, Primrose JN, Pearce NW. Hepatic splenosis mimicking HCC in a patient with hepatitis C liver cirrhosis and mildly raised alpha feto protein; the important role of explorative laparoscopy. World J Surg Oncol. 2009;7:1. doi: 10.1186/1477-7819-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kang KC, Cho GS, Chung GA, Kang GH, Kim YJ, Lee MS, et al. Intrahepatic splenosis mimicking liver metastasis in a patient with gastric cancer. J Gastric Cancer 2011; 11: 64-8. [DOI] [PMC free article] [PubMed]; Kang KC, Cho GS, Chung GA, Kang GH, Kim YJ, Lee MS. et al. Intrahepatic splenosis mimicking liver metastasis in a patient with gastric cancer. J Gastric Cancer. 2011;11:64–8. doi: 10.5230/jgc.2011.11.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toshikuni N, Shiroeda H, Ozaki K, Matsue Y, Minato T, Nomura T, et al. Advanced ultrasonography technologies to assess the effects of radiofrequency ablation on hepatocellular carcinoma. Radiol Oncol 2013; 47: 224-9. [DOI] [PMC free article] [PubMed]; Toshikuni N, Shiroeda H, Ozaki K, Matsue Y, Minato T, Nomura T. et al. Advanced ultrasonography technologies to assess the effects of radiofrequency ablation on hepatocellular carcinoma. Radiol Oncol. 2013;47:224–9. doi: 10.2478/raon-2013-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doi O, Itoh F, Aoyama K. Mature teratoma arising in intraabdominal undescended testis in an infant with previous inguinal exploration: case report and review of intraa bdominal testicular tumors in children. J Pediatr Surg 2002; 37: 1236-8. [DOI] [PubMed]; Doi O, Itoh F, Aoyama K. Mature teratoma arising in intraabdominal undescended testis in an infant with previous inguinal exploration: case report and review of intraa bdominal testicular tumors in children. J Pediatr Surg. 2002;37:1236–8. doi: 10.1053/jpsu.2002.34492. [DOI] [PubMed] [Google Scholar]
- 13.Faure-Conter C, Rocourt N, Sudour-Bonnange H, Vérité C, Martelli H, Patte C, et al. Pediatric germ cell tumours. Bull Cancer 2013; 100: 381-91. [DOI] [PubMed]; Faure-Conter C, Rocourt N, Sudour-Bonnange H, Vérité C, Martelli H, Patte C. et al. Pediatric germ cell tumours. Bull Cancer. 2013;100:381–91. doi: 10.1684/bdc.2013.1729. [DOI] [PubMed] [Google Scholar]
- 14.Kurata A, Hirano K, Nagane M, Fujioka Y. Immature teratoma of the ovary with distant metastases: favorable prognosis and insights into chemotherapeutic retroconversion. Int J Gynecol Pathol 2010; 29: 438-44. [DOI] [PubMed]; Kurata A, Hirano K, Nagane M, Fujioka Y. Immature teratoma of the ovary with distant metastases: favorable prognosis and insights into chemotherapeutic retroconversion. Int J Gynecol Pathol. 2010;29:438–44. doi: 10.1097/PGP.0b013e3181cef16b. [DOI] [PubMed] [Google Scholar]
- 15.Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: tumor types and imaging characteristics. Radiographics 2001; 21: 475-90. [DOI] [PubMed]; Outwater EK, Siegelman ES, Hunt JL. Ovarian teratomas: tumor types and imaging characteristics. Radiographics. 2001;21:475–90. doi: 10.1148/radiographics.21.2.g01mr09475. [DOI] [PubMed] [Google Scholar]
- 16.Gruen DR, Gollub MJ. Intrahepatic splenosis mimicking hepatic adenoma. AJR Am J Roentgenol 1997; 168: 725-6. [DOI] [PubMed]; Gruen DR, Gollub MJ. Intrahepatic splenosis mimicking hepatic adenoma. AJR Am J Roentgenol. 1997;168:725–6. doi: 10.2214/ajr.168.3.9057523. [DOI] [PubMed] [Google Scholar]
- 17.Tsitouridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT and MRI of intraperitoneal splenosis. Diagn Interv Radiol 2010; 16: 145-9. [DOI] [PubMed]; Tsitouridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT and MRI of intraperitoneal splenosis. Diagn Interv Radiol. 2010;16:145–9. doi: 10.4261/1305-3825.DIR.1855-08.1. [DOI] [PubMed] [Google Scholar]
- 18.Menth M, Herrmann K, Haug A, Raziorrouh B, Zachoval R, Jung CM, et al. Intra-hepatic splenosis as an unexpected cause of a focal liver lesion in a patient with hepatitis C and liver cirrhosis: a case report. Cases J 2009; 2: 8335. [DOI] [PMC free article] [PubMed]; Menth M, Herrmann K, Haug A, Raziorrouh B, Zachoval R, Jung CM. et al. Intra-hepatic splenosis as an unexpected cause of a focal liver lesion in a patient with hepatitis C and liver cirrhosis: a case report. Cases J. 2009;2:8335. doi: 10.4076/1757-1626-2-8335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi GH, Ju MK, Kim JY, Kang CM, Kim KS, Choii JS, et al. Hepatic splenosis preoperatively diagnosed as hepatocellular carcinoma in a patient with chronic hepatitis B: a case report. J Korean Med Sci 2008; 23: 336-41. [DOI] [PMC free article] [PubMed]; Choi GH, Ju MK, Kim JY, Kang CM, Kim KS, Choii JS. et al. Hepatic splenosis preoperatively diagnosed as hepatocellular carcinoma in a patient with chronic hepatitis B: a case report. J Korean Med Sci. 2008;23:336–41. doi: 10.3346/jkms.2008.23.2.336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakajima T, Fujiwara A, Yamaguchi M, Makiyama A, Wakae T, Fujita K, et al. Intrahepatic splenosis with severe iron deposition presenting with atypical magnetic resonance images. Intern Med 2008; 47: 743-6. [DOI] [PubMed]; Nakajima T, Fujiwara A, Yamaguchi M, Makiyama A, Wakae T, Fujita K. et al. Intrahepatic splenosis with severe iron deposition presenting with atypical magnetic resonance images. Intern Med. 2008;47:743–6. doi: 10.2169/internalmedicine.47.0689. [DOI] [PubMed] [Google Scholar]
- 21.Imbriaco M, Camera L, Manciuria A, Salvatore M. A case of multiple intra-abdominal splenosis with computed tomography and magnetic resonance imaging correlative findings. World J Gastroenterol 2008; 14: 1453-5. [DOI] [PMC free article] [PubMed]; Imbriaco M, Camera L, Manciuria A, Salvatore M. A case of multiple intra-abdominal splenosis with computed tomography and magnetic resonance imaging correlative findings. World J Gastroenterol. 2008;14:1453–5. doi: 10.3748/wjg.14.1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marcan M, Pavliha D, Music MM, Fuckan I, Magjarevic R, Miklavcic D. Segmentation of hepatic vessels from MRI images for planning of electroporation-based treatments in the liver. Radiol Oncol 2014; 48: 267-81. [DOI] [PMC free article] [PubMed]; Marcan M, Pavliha D, Music MM, Fuckan I, Magjarevic R, Miklavcic D. Segmentation of hepatic vessels from MRI images for planning of electroporation-based treatments in the liver. Radiol Oncol. 2014;48:267–81. doi: 10.2478/raon-2014-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu K, Liang Y, Liang X, Yu H, Wang Y, Cai X. Laparoscopic resection of isolated hepatic splenosis mimicking liver tumors: case report with a literature review. Surg Laparosc Endosc Percutan Tech 2012; 22(5): e307-11. [DOI] [PubMed]; Liu K, Liang Y, Liang X, Yu H, Wang Y, Cai X. Laparoscopic resection of isolated hepatic splenosis mimicking liver tumors: case report with a literature review. Surg Laparosc Endosc Percutan Tech. 2012;22(5):e307–11. doi: 10.1097/SLE.0b013e318263a3f3. [DOI] [PubMed] [Google Scholar]