Abstract
The high burden of exposure to chronic life adversities and trauma is quite prevalent, but assessment of this risk burden is uncommon in primary care settings. This calls for a brief, multiple dimensional mental health risk screening tool in primary care settings. We aimed to develop such a screening tool named the UCLA Life Adversities Screener (LADS). Using pooled data across four studies from the UCLA Center for Culture, Trauma and Mental Health Disparities, five domains of mental health risk including perceived discrimination, sexual abuse histories, family adversity, interpersonal violence, and trauma histories, were identified. Regression models for depression (Centers for Epidemiology Studies-Depression scale (CES-D)) and PTSD (Posttraumatic Diagnostic Scale (PDS)), controlling for demographic factors, were fitted to to develop a weighted continuous scale score for the UCLA LADS. Confirmatory factor analysis supported the five-domain structure, while Item Response Theory (IRT) endorsed the inclusion of each item. Receiver Operating Characteristic (ROC) analysis indicated that the score was predictive for classifying subjects as reaching clinical threshold criteria for either depression (Beck Depression Inventory-II (BDI-II) ≥14 or Patient Health Questionnaire-9 (PHQ-9) ≥ 10) or anxiety (Patient Health Questionnaire-13 (PHQ-13) ≥10). An optimal cut of 0.33 is suggested based on maximizing sensitivity and specificity of the LADS score, identifying patients at high risk for mental health problems. Given its predictive utility and ease of administration, the UCLA LADS could be useful as a screener to identify racial minority individuals in primary care settings who have a high trauma burden, needing more extensive evaluation.
Keywords: Mental health screening, trauma exposure, ethnic-minorities, primary care
INTRODUCTION
Psychological distress is common among American adults (CDC, 2011). Approximately 10% of the general population suffer from symptoms of depression and posttraumatic stress (Prevention, 2011) and up to 20% report having experienced a significant life trauma such as child abuse, interpersonal violence, rape, physical assault, or a life-threatening accident (R.C. Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Prevention, 2010). An estimated 20% to 50% of adult patients in primary care report a history of some type of trauma (Weinreb, Fletcher, Candib, & Bacigalupe, 2007).
For many individuals, life stressors and trauma occur in a chronic and cumulative way, and compromise both physical and mental health over time, often in a comorbid fashion (Jackson, Knight, & Rafferty, 2010; Juster et al., 2011; R.C. Kessler et al., 1995; Myers, 2009). Chronic life stress has been linked to both physical and mental health disorders across the lifespan with differential exposures contributing to health inequities (Benjet, Borges, & Medina-Mora, 2010; Benjet, Borges, Mendez, Fleiz, & Medina-Mora, 2011; Lupien, McEwen, Gunnar, & Heim, 2009; Thoits, 2010). The addition of traumas appears additive, with additional events causing new problems in functioning (Campbell, Dworkin, & Cabral, 2009). Unfortunately, much of the psychological distress stemming from chronic life stress and trauma remains undetected and untreated. Only a small proportion of individuals with psychological distress are identified in health care settings, and a smaller fraction of those ever receive appropriate treatment (Bruce et al., 2001; R. C. Kessler et al., 2001). Untreated psychiatric disorders result in lost productivity, decreased quality of life, and often, poorly managed comorbid physical ailments (Gureje & Jenkins, 2007; Manderscheid, 2007; Organization, 2001). Low income ethnic minority groups and other underserved populations are particularly under-diagnosed and undertreated for mental health disorders, especially when presenting with health problems in primary care settings (Stockdale, Lagomasino, Siddique, McGuire, & Miranda, 2008). They, however, are at great risk of exposure to physical and sexual abuse over the life course (M. Benson, Wooldredge, J., Thistlethwaite, A., Fox, G., 2004a; M. L. Benson, Fox, G.L., 2004b; Bryant-Davis, Chung, Tillman, & Belcourt, 2009; Hampton, 1994; Jenkins, 2004) and to growing up in families that experience significant economic, employment and structural adversities (U.S Department of Health & Human Services, 2001). These experiences are often not assessed and are untreated when they seek health services.
Under the Patient Protection and Affordable Care Act (PPACA), an estimated 16 million people will gain health coverage and enter the healthcare system in 2014 (Congress, 2012). The PPACA provides a unique opportunity to identify those who have not been assessed or treated for mental health needs. Screening and linkage to care can be efficiently accomplished in primary care settings by using a brief assessment to identify significant risk factors for psychiatric disorders. For example, in a large community sample, 22 (4.6%) met criteria for major depression (Boyd, Weissman, Thompson, & Myers, 1982). Up to 35% of patients in primary care have been estimated to have depression (Blacker & Clare, 1987).
Mental health screenings are widely used in many primary care settings and are very useful in identifying patients who meet psychiatric disorder criteria (FORCE., 2002). However, screeners which assess the range of life adversities from multiple dimensions and potentially traumatizing experiences that confer substantial risk for psychiatric disorders are lacking. When working with ethnic minority groups, it may be important to also use a screening tool that assesses experiences and behaviors known to be associated with adverse mental and physical health outcomes. Indeed, several screening measures have been developed to address the under-identification of mental health concerns among minorities (e.g., the Multiculturally Sensitive Mental Health Scale) (Chao & Green, 2011) and to screen for specific experiences known to be risk factors for physical and psychological well-being (e.g., the Jackson Heart Study Discrimination (JHSDIS) Instrument, (Sims, Wyatt, Gutierrez, Taylor, & Williams, 2009) the Sexual Experiences Survey (Koss, 2007)) and brief screening tools for intimate partner violence (Basile, 2007). However, none of these measures were developed to assess the range of challenges that underserved populations commonly experience such as early family adversities and perceived discrimination. Many underserved populations report subtle and overt discrimination over their lifespan, (Myers, 2009; Sue et al., 2007) and such experiences have been linked to negative mental health and poor physical health outcomes (Bogart et al., 2011; Lee & Ahn, 2011; Smedley, 2012). Other more comprehensive mental health screening tools do exist (e.g., Trauma Screener as in Davidson et al., 1997) but they are time-consuming and better suited to psychiatric settings. Given these challenges, measures that are relatively brief, easy to administer, and cover a broad range of lifetime adversities and traumas are needed to help identify ethnically diverse primary care patients with heavy burdens of psychiatric risk.
The purpose of this article is to describe the development and psychometric properties of the UCLA Life Adversities Screener (LADS), a screening tool developed to identify patients being treated in healthcare settings such primary care, especially those from low income, ethnic minority backgrounds who have a history of trauma and serious life stressors and who will likely benefit from mental health services.
METHODS
Sample
A multi-ethnic sample of 550 participants including 230 African American (167 men and 63 women), 270 Latinos/as (50 men and 220 women), and 50 white men who reported histories of childhood sexual abuse (CSA) and/or interpersonal violence (IPV) as adults, were recruited to participate in four studies supported by the National Institute of Mental Health (NIMH)-funded Center for Culture, Trauma and Mental Health Disparities (CCTMHC). Study participants were recruited from a variety of community clinics and agencies, as well as with flyers and word of mouth referrals. Descriptions of the recruitment procedures have been previously published (Glover et al., 2010; Glover, Williams, & Kisler, 2013). This research was approved by the institutional review board at the University of California, Los Angeles (UCLA) and before being enrolled, all study participants provided written informed consent.
Measures
Trained assessors administered a core battery of psychosocial measures to all participants either by interview or on computers equipped with Audio Computer-Assisted Self-Interview (ACASI) software. All participants were compensated for their time and received information on mental and physical health and social services. The key variables of interest included demographic characteristics, early childhood adversities and traumas, adult adversities and traumas, and mental health outcomes (see Table 1).
Table 1.
Description of the Sample
| Demographics* | N (%) | M (SD) | Range |
|---|---|---|---|
|
|
|||
| Age | 36.9 (9.9) | 18–67 | |
| Gender | |||
| Women | 283 (51.5%) | ||
| Men | 267 (48.6%) | ||
| Ethnicity | |||
| African American | 230 (41.8%) | ||
| Latino | 270 (49.1%) | ||
| White | 50 (9.1%) | ||
| Education | |||
| Less than High School | 159 (29.1%) | ||
| High school/GED | 226 (41.3%) | ||
| Vocational/technical degree | 65 (11.9%) | ||
| Associates degree or B.A./B.S. | 91 (16.6%) | ||
| Graduate degree | 6 (1.1%) | ||
| Monthly income | |||
| Less than $1249 | 299 (63.8%) | ||
| $1250 – $2083 | 95 (20.3%) | ||
| $2084 or more | 75 (16.0%) | ||
| Employment | |||
| Unemployed | 365 (67.6%) | ||
| Employed | 175 (32.4%) | ||
| Index risk items | |||
| Penetrative sexual abuse (ever) | 358 (65.1%) | ||
| Discriminated against (last month) | 73 (13.5%) | ||
| Fear injury or death (ever) | 171 (31.3%) | ||
| Family violence (ever) | 262 (47.8%) | ||
| Partner violence (ever) | 219 (40.0%) | ||
|
|
|||
| Mental Health Outcomes | |||
| CESD | 16.5 (12.1) | 0–55 | |
| PHQ13 | 5.4 (4.5) | 0–22 | |
| PTSD | 12.1 (10.8) | 0–46 | |
| BDI (project 4 only) | 6.7 (9.5) | 0–49 | |
| PHQ9 (project 1–3) | 5.9 (5.7) | 0–27 | |
|
|
|||
Sample may not total 550 for all variables as participants were able to skip items.
Demographic characteristics included age, gender, race/ethnicity, education, household income, and employment.
Early childhood adversities and traumas, including: 1) non-sexual, early life adversities (e.g. parental incarceration, illness, disability, severe poverty) were assessed using the family adversity scale; (R. C. Kessler & Magee, 1993) 2) childhood sexual abuse (CSA) was assessed as a composite report of consensual and nonconsensual sexual experiences before the age of 18 using the Wyatt Sexual History Questionnaire (WSHQ-R) (Loeb et al., 2002; Wyatt, Lawrence, Voudounon, & Mickey, 1992) and; 3) other non-sexual traumas such as physical abuse, disasters, accidents, exposure to community violence were assessed using the Trauma History Questionnaire (THQ) (Green, 1996).
Adult life adversities and traumas, including: 1) perceived discrimination (e.g., mistreated because of your race, ethnicity, nationality, gender, sexual orientation or some other characteristic) was assessed with one item from the Chronic Burden Scale; (Gurung RAR, 2004) 2) adult sexual abuse (ASA) assessed attempted or completed rape since the age of 18 with the THQ (Green, 1996); 3) intimate partner violence in the form of psychological and physical abuse was assessed with an item from an abuse screener (McFarlane, Greenberg, Weltge, & Watson, 1995; Soeken K, 1998) and two additional items that assessed if a partner or ex-partner had ever called the participant names, insulted them or ever threatened to hurt their children/or unborn child and; 4) other adult traumas including disasters, accidents, exposure to community violence, etc., was assessed with the THQ (Green, 1996).
Mental health status as the outcome of interest was assessed using five measures of psychiatric symptoms, including depression (Centers for Epidemiology Studies-Depression scale (CES-D), (Radloff, 1977) Patient Health Questionnaire-9 (PHQ-9),(Kroenke, Spitzer, & Williams, 2001) Beck’s Depression Inventory-II (BDI-II) (Beck AT, 1996), PTSD (Posttraumatic Diagnostic Scale (PDS), (Ehring, Kleim, Clark, Foa, & Ehlers, 2007; Foa, 1997) and anxiety (Patient Health Questionnaire-13 (PHQ-13) (Kroenke, Spitzer, & Williams, 2002).
Data Analysis
Five domains of life adversity suggested by previous research, clinical knowledge and expert panel review were first identified and subjected to a confirmatory factor analysis (CFA). Twenty-one items were pooled from data across four studies to represent the five hypothesized domains of life adversities (see Table 2). These domains included: 1) Perceived discrimination; 2) Any penetrative sexual abuse (CSA/ASA); 3) Violence in the family; 4) Intimate partner violence (IPV); and 5) Fear you might be killed or seriously injured. Following CFA, item reduction was performed.
Table 2.
Confirmatory Factor Analysis.
| Factor* | |||||
|---|---|---|---|---|---|
|
| |||||
| Item | 1 | 2 | 3 | 4 | 5 |
| 1. Because of your ethnicity/race, how often have you been treated unfairly by co-workers or classmates? | 0.75 | ||||
| 2. Because of your ethnicity/race, how often have others hinted that you are dishonest or can’t be trusted? | 0.82 | ||||
| 3. Because of your ethnicity/race, how often have others ignored you or not paid attention to you? | 0.74 | ||||
| 4. Because of your ethnicity/race, how often have people not trusted you? | 0.79 | ||||
| † 5. Being discriminated against because of your race, nationality, gender, or sexual orientation. | 0.55 | ||||
| 6. When you were growing up, your family argued and fought a lot. | 0.61 | ||||
| † 7. When you were growing up, people in your family hit each other or threw or broke things when there were arguments or disagreements. | 0.67 | ||||
| 8. When you were growing up, people in your family had problems with alcohol or drugs. | 0.56 | ||||
| 9. Not having enough money to cover the basic needs of life, such as food, clothing, and housing. | 0.41 | ||||
| 10. No reliable source of transportation, such as a car that works or reliable bus service. | 0.38 | ||||
| 11. Losing the help of someone you depend on, such as person moved, got sick, or otherwise was unavailable. | 0.44 | ||||
| 12. Has anyone tried to assault or attack you on the street or in a public space? | 0.71 | ||||
| † 13. Have you ever been in any other situation in which you feared you might be killed or seriously injured? | 0.71 | ||||
| 14. Have you ever seen someone seriously injured or killed? | 0.65 | ||||
| 15. Has your partner or ex-partner ever threatened you or made you feel afraid or unsafe for any reason? | 0.71 | ||||
| † 16. Has your partner or ex-partner ever pushed, hit, slapped, kicked, or otherwise physically hurt you for any reason? | 0.81 | ||||
| 17. Has your partner or ex-partner ever insulted you or called you names (e.g. “stupid”)? | 0.77 | ||||
| 18. Since the age of 18, have you ever been forced to have sex (penetration with a penis or object)? | 0.27 | ||||
| 19. Since the age of 18, has anyone ever attempted to force you to have sex? | 0.28 | ||||
| 20. Did anyone over the age of 18 touch you sexually (score 1) or put an object inside your mouth, vagina, or butt (score 2) before you were 18 years old? (score 0 if none) | 0.89 | ||||
| 21. Before you were 18 years old, did one (score 2) or more (score 3) people over the age of 18 penetrate you sexually? (score 0 if none) | 0.90 | ||||
Factors referred to 1) Perceived discrimination, 2) Violence in the family, 3) Fear you might be killed or seriously injured, 4) Intimate partner violence (IPV), and 5) Any sexual abuse (ASA/CSA);
Item selected for screener. Note that some factors were represented by composite questions, so not every factor has a selected item noted.
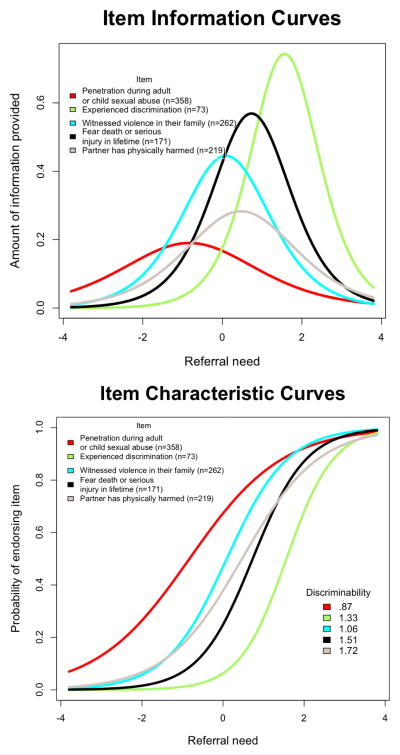
Items were selected from the CFA to best represent each of the five domains. Each item was then evaluated using Item Response Theory (IRT) to ensure its discriminating utility in describing an individual’s need for referral. Need for referral was operationalized as a single latent construct underlying and characterizing the covariance of these items. These five items were then entered into a regression predicting scores on measures of mental health (depression and PTSD) both to create weights to calculate a weighted total scale score across the five domains and to evaluate their predictive ability on mental health outcomes. Finally, the calculated total scale score was used in a Receiver Operating Characteristic (ROC) curve analysis to evaluate its predictive ability for clinically significant levels of mental health (depression or anxiety) symptoms.
IRT analysis was conducted to provide information about the ability of each item to discriminate between someone who would benefit from a referral versus those unlikely to benefit from a referral. Some have suggested discrimination could be interpreted as very low if discrimination is less than 0.2 up to very high if discrimination is 1 (Baker, 1985). Data in this study were modeled in R (v 2.14) using the Latent Trait Models (v .9-7) (Rizopoulos, 2006). The model assumed one underlying latent trait.
Multiple linear regressions predicting the mental health outcomes of PTSD (PDS) (Ehring et al., 2007; Foa, 1997) and depression (CES-D) (Radloff, 1977) were fitted to create item weights. To increase the likelihood that the UCLA Life Adversities Screener (LADS) developed in this sample will generalize to other samples, several demographic characteristics were controlled in the regression. Specifically, age, education, ethnicity (coded as White, Latino, or African-American) and study (n=4) for which the participants were recruited were entered first. Beta coefficients from the regression were used to create a weighted, composite referral need index. The total scale score was calculated as:
| (1) |
where x(i) is the ith item and ω(i) is the rescaled coefficient from formula (2) below. Beta coefficients w(i) of the regression model (see Table 3) were re-scaled to sum to 1 to ease calculation and interpretation:
| (2) |
Table 3.
Regression Coefficients Predicting Mental Health (Depression and PTSD) Difficulties.
| Variable | Coefficient | SE | t value | p value |
|---|---|---|---|---|
|
Controls
| ||||
| Education | −4.55 | 1.98 | −2.29 | 0.02 |
| Age | −0.18 | 0.10 | −1.88 | 0.06 |
| Ethnic (Caucasian) | ||||
| African-American | 6.03 | 3.38 | 1.79 | 0.08 |
| Latino | 0.67 | 2.79 | 0.24 | 0.81 |
| Project (Study 1) | ||||
| Study 2 | 3.45 | 3.40 | 1.01 | 0.31 |
| Study 3 | −2.25 | 3.14 | −0.72 | 0.47 |
| Study 4 | 0.68 | 3.88 | 0.18 | 0.86 |
|
| ||||
|
Screener items
| ||||
| Any penetrative sexual abuse | 5.24 | 2.42 | 2.16 | 0.03 |
| Perceived discrimination | 12.45 | 2.49 | 5.00 | < 0.001 |
| Feared you might be killed or seriously injured | 9.18 | 1.90 | 4.83 | < 0.001 |
| Violence in the family | 7.18 | 1.82 | 3.93 | < 0.001 |
| Intimate partner violence | 7.28 | 1.88 | 3.87 | < 0.001 |
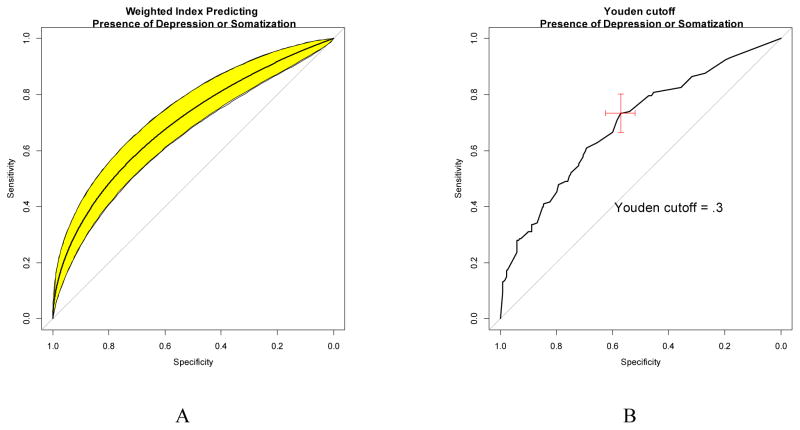
Using the scaled score, a ROC curve was calculated to evaluate its predictive ability for clinically meaningful levels of either depression or anxiety. Specifically, the scaled screener score was used to predict the presence of clinically significant levels of either depression ((PHQ-9≥10) (Kroenke et al., 2001) or (BDI-II≥14) (Beck AT, 1996)) or anxiety (PHQ-13≥10) (Kroenke et al., 2002). The pROC library (Robin et al., 2011) of R was used. The curve was smoothed binormally calculated with 2000 stratified bootstrap replicates, and reported with 95% CI.
Future research will directly test the clinical utility of the index, but empirically optimal cut-points could be suggested from the existing data. Youden’s (1950) statistic, which identifies a point that balances false negatives and positives without regard for actual relative costs, was used to suggest a cut-point.
In analyses, we assume that missingness is random and set type I error at α = 0.05.
RESULTS
Characteristics of the sample
Demographic information of the sample is summarized in Table 1. The mean age of the sample was 36.9 years, almost equally represented by men and women, and composed of primarily African Americans and Latinos. Only 17.7% of the sample had more than a high school or equivalent general education degree (GED) or vocational/technical degree. The majority of the sample was unemployed (67.6%) and 63.8% earned less than $15,000 per year, which is below the 2013 Federal Poverty Guidelines of $15,510 for a family/household of 2 (Services, 2013). A significant portion of the sample reported trauma experiences and stressors in the form of penetrative sexual abuse (65.1%), discrimination based on race, ethnicity, nationality, gender or sexual orientation (13.5%), fear that they might be killed or seriously injured (31.3%), family violence (47.8%), and IPV (40.0%). The majority of participants reported more than one type of trauma experiences and stressors (N=332, 60.36%), while 87 (15.82%) reported no such experiences, and 131 (23.82%) reported only one type. The mean (SD) of depression (CES-D), anxiety (PHQ-13) and PTSD (PDS) scores were 16.5 (12.1), 5.4 (4.5), and 12.1(10.8), respectively. The mean BDI and PHQ-9 scores were 6.7 (9.5), and 5.9 (5.7), respectively, and were collected in a subset of studies only.
Factor Analysis
Confirmatory, principal factor analyses (unrotated solution) suggested the presence of five, independent factors within the 21 items (see Table 2; df = 180, GFI = 0.84, RMSEA = 0.10). The items that loaded most heavily on each factor were selected for inclusion in an index with two exceptions. First, the discrimination items that loaded most highly on the first factor were simple variants focused solely on race/ethnicity discrimination, while the lowest-loading item included “nationality, gender, and sexual orientation”. A clinical decision was made to use this more inclusive item, which would help generalize the screener in sample with, for example, more gender variability. Second, the sexual assault items could be easily combined into a single, inclusive item, because each item included sexual penetration without consent (or ability to consent due to age). These five selected/combined, recoded items (see Appendix I) were then characterized by IRT.
Index psychometrics
Item Response Theory was used to investigate the properties of the five items selected. The fit to a single latent construct appeared reasonable (AIC = 3843.89). The item that best discriminated on the latent variable “referral need” which was thought to underlie these items was “experienced discrimination” (see Figure 1). The item that discriminated the least was a history of penetrative sexual assault as either an adult or child. The probability of any person in this sample endorsing these items was relatively high for sexual assault (0.71) and low for discrimination (0.07). In general, the items provided more information about those high on referral need (60.7%) than those low on referral need (37%). Specifically, the item that provided the most information for those low on referral need was the sexual assault item (61.4%). The item that provided the most information about those high on referral need was the discrimination item (92.2%).
Figure 1.
Item characteristics curve and item information curves
Predictive utility
Multiple regression
Using the items as predictors, multiple regression was used to predict scores on depression (CES-D) and PTSD (PDS) measures after controlling for education, age, ethnicity (African America, Latino, White), and the study (of four studies) from which they participated. The regression model was significant (F(11,439) = 29.66, p <0.001, R2 = 0.43) for each of the five predictor variables (see Table 3).
One of the items concerning experiencing a life-threatening event was strongly predictive of PTSD, t (307) = −8.54, p < 0.001, which could also be viewed as criterion contamination given the similarity of this item to items in the PTSD measure. When the model was run predicting depression scores alone, this item remained significant, as did each of the other screening items. Thus, the item concerning experiencing a life-threatening event was retained.
The coefficients were rescaled (described above) for scoring that was both simple and more likely to generalize to other samples with different education, age, ethnicity, and trauma history. Scoring (detailed in Appendix I) basically adds the weight for each item that a person endorses for a score that ranges from 0 (no life adversity or trauma) to 1 (all life adversities and traumas).
Receiver Operator Characteristic Curve
The ROC for the index score predicting the presence of depression or anxiety was well above chance (AUC =0.7, CI = 0.64–0.74; see Figure 2). The optimal cutoff according to the Youden criteria was 0.33 (see Figure 3).
Figure 2.
Receiver operating characteristic curves showing (smoothed) prediction (A) and Youden’s optimal cut-off +/− 95% CI (B) predicting presence of either depression or somatization
DISCUSSION
The UCLA LADS is a brief (five domains) screener developed to assess experiences that may predict symptoms of depression, PTSD and anxiety. It is brief, which may make it easy to administer in primary care or other non-psychiatric settings, and captures adversity and trauma-related experiences of populations that may not be captured with current screening approaches. This could optimize Affordable Care as it strives to improve prevention efforts. Specifically, populations with high frequencies of life traumas and adversities may not present with mental health symptoms in the same way as other populations, or may not have yet developed clinically significant levels of mental health symptoms, but may most benefit from early interventions.
The UCLA LADS is a unique contribution to the extant body of mental health screeners for several reasons. First, it was developed primarily on African American and Latino male and female participants whose demographics represented populations who are marginal consumers of health and mental health services. Second, while current screeners for depression and PTSD include only items that describe the symptoms themselves, the LADS assesses background experiences, such as childhood traumas and adversities, that predict the development of these symptoms. Thus, it has the advantage of identifying stressors and traumas that contribute to psychological distress further “upstream” from their negative consequences (i.e., symptoms of mental disorders) and provides the opportunity to intervene earlier. Moreover, in a primary care setting, individuals may be more able or willing to affirm whether or not a certain experience has happened to them than to identify, acknowledge or understand the extent to which they have experienced certain psychological symptoms. Third, the UCLA LADS allows health providers to better understand how life adversities account for co-morbid health and mental health problems rather than to assess for only one of these experiences. Studies have shown that trauma-related experiences do not often occur in isolation from others (Edwards, Holden, Felitti, & Anda, 2003; Noll & Grych, 2011). To address one and not the cluster of problems, all of which can predict psychological distress, would only partially address a problem that could worsen over time.
The UCLA LADS was developed because individuals with serious stress and trauma histories might exhibit significant depression, PTSD, or anxiety symptoms that are not currently being recognized by health providers. The items on the screener were selected to represent five constructs: perceived discrimination, sexual abuse histories, family adversity, intimate partner violence, and trauma histories. A series of analyses were used to characterize the type of information provided by each item and to demonstrate that the screener effectively identified individuals at risk for exceeding clinical cut-off criteria for PTSD, depression, and anxiety. The ROC analyses suggested an optimal cutoff for maximizing sensitivity and specificity of 0.33, resulting in 67% sensitivity and 66% specificity. The screener could be a regular part of new patient screening conducted by a first-contact health care provider. In the ideal setting, behavioral health care would be an integrated part of care and would be available for immediate further screening if the screener was positive. At least, a positive screening could start a conversation with providers about the possible need for additional screening in the form of referrals to behavioral health care.
While we used the Youden’s (1950) statistic, an alternative would have been to try to quantify the costs of different errors specific to this context, such as considering the base rates of depression and the cost for not treating an affected individual over five years (Zweig & Campbell, 1993). This more context-specific approach was not used at this time, despite limited published information about the costs of various aspects of treatment for depression and anxiety (Lave, Frank, Schulberg, & Kamlet, 1998) due to the complexities in instantiating assumptions about treatments and given the rapidly changing cost of care in the United States in 2013. Also, given that the motivation of the screener is to identify people who might otherwise miss needed mental health care, a case could be made for minimizing false negatives preferentially. The entire index of cut-scores is provided (see Appendix) to allow users to follow this strategy as appropriate for their setting. Using lower cut-off scores will reduce the number of false negatives, but must always be considered at the expense of false positives. Also, the items differed in the time frame identified. The discrimination item might have performed well because it queried recent events, whereas items like childhood sexual abuse might have occurred only in the distant past. Current investigation will include explicit questions regarding how much the item is currently experienced as distressing to examine how differences in framing might impact endorsement of items.
Developing a screener that is useful during brief clinic visits required some trade-offs. For example, discrimination by race and gender were collapsed, although gender discrimination may be experienced more often by the women in the study. This study focused on identification of the best general predictors for the diverse people that appear in primary care, while future studies will work to provide normative ranges sensitive to gender, ethnicity, etc. as needed for scale interpretation.
While the findings are encouraging, there are limitations to consider. The UCLA LADS was developed using a non-random sample selected for inclusion into the four studies with male and female participants with histories of trauma and HIV infection. Thus, it is likely that the sample represented a segment of the population suffering more from the sequel of trauma and stress than the norm. The UCLA LADS needs to be tested with a more representative community sample and it must be determined if a different cutoff point may be used to yield similar sensitivity and specificity rates. Additionally, the suggested cut-off of 0.33 should be adjusted according to the base rates in the settings used. For those settings with a similar sample to the one tested, the full sensitivity and specificity table (see Appendix II) is provided to allow providers to adjust the current scores as desired for their setting.
Given the predictive utility and ease of administration, the UCLA LADS promises to be a useful tool for identifying individuals with mental health issues in primary care settings. This screener addresses the critical challenge of balancing time and resource constraints with providing adequate screening and care. Future directions include implementing the LADS in primary care settings and testing its effectiveness in clinical settings.
Acknowledgments
Special thanks to Jennifer Carmona, Ph.D., Michael Rodriguez, M.D., Frank Galvan, Ph.D., and Dorie A. Glover, Ph.D., for their contributions to the studies on which these analyses are based and to Ms. Whitney Cale for her editorial assistance. Support for this research was provided by the National Institute of Mental Health (grants 5P50MH073453 and 1 R34 MH077550).
Appendix I. UCLA Life Adversities Screener
Instructions: Please answer “yes” or “no” to each item below as honestly and accurately as you are able.
| Yes | No | Ω | |
|---|---|---|---|
|
|
|||
| 1. Have you ever had a penis or object inserted into your vagina, butt, or mouth when you did not want it as a child or adult? | 0.13 | ||
|
|
|||
| 2. In the last month, have you been discriminated against because of your race, nationality, gender or sexual orientation? | 0.30 | ||
|
|
|||
| 3. Have you ever been in any situation in which you feared you might be killed or seriously injured? | 0.22 | ||
|
|
|||
| 4. Did people in your family ever hit each other or throw or break things when there were arguments or disagreements? | 0.17 | ||
|
|
|||
| 5. Has your partner or ex-partner ever pushed, hit, slapped, kicked or otherwise physically hurt you for any reason? | 0.18 | ||
|
|
|||
| Score* | |||
Each “yes” add the weight of that item from the “ω” column to the score. Score range = 0 to 1. Initial suggested cut-off = 0.33
Appendix II. Sensitivity and specificity (with confidence intervals) for each possible score on the Index
| Score | Specificity | Sensitivity | ||||
|---|---|---|---|---|---|---|
| 2.5% | 50% | 97.5% | 2.5% | 50% | 97.5% | |
|
| ||||||
| Inf | 0 | 0 | 0 | 1 | 1 | 1 |
| 0.04 | 0.14 | 0.18 | 0.22 | 0.89 | 0.93 | 0.97 |
| 0.09 | 0.16 | 0.20 | 0.24 | 0.88 | 0.93 | 0.96 |
| 0.13 | 0.23 | 0.27 | 0.32 | 0.83 | 0.88 | 0.93 |
| 0.16 | 0.27 | 0.32 | 0.36 | 0.81 | 0.86 | 0.91 |
| 0.17 | 0.31 | 0.36 | 0.40 | 0.76 | 0.83 | 0.88 |
| 0.20 | 0.41 | 0.45 | 0.50 | 0.75 | 0.81 | 0.86 |
| 0.23 | 0.41 | 0.46 | 0.51 | 0.73 | 0.80 | 0.85 |
| 0.24 | 0.42 | 0.47 | 0.52 | 0.73 | 0.80 | 0.85 |
| 0.25 | 0.42 | 0.47 | 0.52 | 0.73 | 0.80 | 0.85 |
| 0.26 | 0.49 | 0.54 | 0.59 | 0.67 | 0.74 | 0.81 |
| 0.28 | 0.52 | 0.57 | 0.62 | 0.66 | 0.73 | 0.80 |
| 0.30 | 0.52 | 0.57 | 0.62 | 0.66 | 0.73 | 0.80 |
| 0.32 | 0.54 | 0.58 | 0.64 | 0.63 | 0.71 | 0.77 |
| 0.33* | 0.55 | 0.60 | 0.65 | 0.59 | 0.66 | 0.73 |
| 0.34 | 0.61 | 0.65 | 0.70 | 0.55 | 0.63 | 0.70 |
| 0.36 | 0.65 | 0.69 | 0.74 | 0.53 | 0.61 | 0.68 |
| 0.38 | 0.65 | 0.70 | 0.74 | 0.52 | 0.60 | 0.66 |
| 0.38 | 0.66 | 0.71 | 0.75 | 0.51 | 0.58 | 0.65 |
| 0.39 | 0.66 | 0.71 | 0.75 | 0.50 | 0.58 | 0.65 |
| 0.39 | 0.68 | 0.72 | 0.76 | 0.47 | 0.55 | 0.63 |
| 0.41 | 0.68 | 0.72 | 0.76 | 0.47 | 0.55 | 0.62 |
| 0.44 | 0.71 | 0.75 | 0.79 | 0.44 | 0.52 | 0.60 |
| 0.45 | 0.71 | 0.75 | 0.79 | 0.43 | 0.52 | 0.58 |
| 0.45 | 0.71 | 0.75 | 0.79 | 0.43 | 0.51 | 0.58 |
| 0.45 | 0.71 | 0.76 | 0.80 | 0.42 | 0.50 | 0.58 |
| 0.46 | 0.72 | 0.76 | 0.80 | 0.41 | 0.49 | 0.57 |
| 0.47 | 0.72 | 0.77 | 0.81 | 0.41 | 0.49 | 0.57 |
| 0.48 | 0.75 | 0.79 | 0.83 | 0.40 | 0.48 | 0.55 |
| 0.49 | 0.76 | 0.80 | 0.84 | 0.37 | 0.45 | 0.53 |
| 0.50 | 0.79 | 0.82 | 0.86 | 0.34 | 0.42 | 0.48 |
| 0.52 | 0.79 | 0.83 | 0.86 | 0.34 | 0.42 | 0.48 |
| 0.55 | 0.81 | 0.84 | 0.88 | 0.34 | 0.41 | 0.48 |
| 0.55 | 0.81 | 0.85 | 0.88 | 0.32 | 0.40 | 0.47 |
| 0.55 | 0.81 | 0.85 | 0.88 | 0.32 | 0.40 | 0.47 |
| 0.55 | 0.83 | 0.87 | 0.90 | 0.27 | 0.34 | 0.42 |
| 0.58 | 0.85 | 0.88 | 0.91 | 0.26 | 0.34 | 0.40 |
| 0.61 | 0.86 | 0.89 | 0.92 | 0.26 | 0.34 | 0.40 |
| 0.62 | 0.86 | 0.89 | 0.92 | 0.24 | 0.31 | 0.38 |
| 0.62 | 0.87 | 0.90 | 0.93 | 0.24 | 0.31 | 0.38 |
| 0.63 | 0.88 | 0.91 | 0.94 | 0.24 | 0.30 | 0.37 |
| 0.65 | 0.90 | 0.93 | 0.95 | 0.22 | 0.29 | 0.35 |
| 0.67 | 0.90 | 0.93 | 0.96 | 0.22 | 0.29 | 0.35 |
| 0.68 | 0.91 | 0.94 | 0.96 | 0.21 | 0.28 | 0.35 |
| 0.70 | 0.92 | 0.94 | 0.97 | 0.21 | 0.28 | 0.35 |
| 0.71 | 0.92 | 0.94 | 0.97 | 0.17 | 0.24 | 0.30 |
| 0.74 | 0.95 | 0.97 | 0.99 | 0.12 | 0.17 | 0.23 |
| 0.77 | 0.96 | 0.98 | 0.99 | 0.12 | 0.17 | 0.23 |
| 0.81 | 0.96 | 0.98 | 0.99 | 0.12 | 0.17 | 0.22 |
| 0.83 | 0.96 | 0.98 | 0.99 | 0.10 | 0.15 | 0.20 |
| 0.84 | 0.97 | 0.98 | 0.99 | 0.09 | 0.14 | 0.19 |
| 0.87 | 0.98 | 0.99 | 1.00 | 0.08 | 0.13 | 0.18 |
| 0.91 | 0.98 | 0.99 | 1.00 | 0.08 | 0.13 | 0.18 |
| 0.96 | 0.98 | 0.99 | 1.00 | 0.05 | 0.09 | 0.14 |
| Inf | 1 | 1 | 1 | 0 | 0 | 0 |
Optimal cut-off by Youden criteria.
Footnotes
Note: Our index was developed using pooled data across 4 studies. One of these studies included a biobehavioral intervention and its NIH ClinicalTrials.gov ID is NCT01641146.
References
- Baker FB. The basics of item response theory. Portsmouth, NH: Heineman; 1985. [Google Scholar]
- Basile KC, Hertz MF, Back SE. Intimate partner violence and sexual violence victimization assessment instruments for use in healthcare settings: Version 1. Atlanta, GA: Centers for Disease Control and Prevention. National Center for Injury Prevention and Control; 2007. [Google Scholar]
- Beck AT, Steers RA, Brown GK. BDI-II, Beck Depression Inventory: Manual. Boston, MA: Harcourt; 1996. [Google Scholar]
- Benjet C, Borges G, Medina-Mora ME. Chronic childhood adversity and onset of psychopathology during three life stages: childhood, adolescence and adulthood. J Psychiatr Res. 2010;44(11):732–740. doi: 10.1016/j.jpsychires.2010.01.004. [DOI] [PubMed] [Google Scholar]
- Benjet C, Borges G, Mendez E, Fleiz C, Medina-Mora ME. The association of chronic adversity with psychiatric disorder and disorder severity in adolescents. Eur Child Adolesc Psychiatry. 2011;20(9):459–468. doi: 10.1007/s00787-011-0199-8. [DOI] [PubMed] [Google Scholar]
- Benson M, Wooldredge J, Thistlethwaite A, Fox G. The correlations between race and domestic violence is confounded with community context. Social Problems. 2004a;51:326–342. [Google Scholar]
- Benson ML, Fox GL. When violence hits home: How economics and neighborhood play a role. Washington D.C: U.S. Department of Justice, Office of Justice Programs; 2004b. [Google Scholar]
- Blacker CV, Clare AW. Depressive disorder in primary care. The British Journal of Psychiatry. 1987;150(6):737–751. doi: 10.1192/bjp.150.6.737. [DOI] [PubMed] [Google Scholar]
- Bogart LM, Wagner GJ, Galvan FH, Landrine H, Klein DJ, Sticklor LA. Perceived discrimination and mental health symptoms among Black men with HIV. Cultur Divers Ethnic Minor Psychol. 2011;17(3):295–302. doi: 10.1037/a0024056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd JH, Weissman MM, Thompson W, Myers JK. Screening for depression in a community sample: Understanding the discrepancies between depression symptom and diagnostic scales. Archives of General Psychiatry. 1982;39(10):1195–1200. doi: 10.1001/archpsyc.1982.04290100059010. [DOI] [PubMed] [Google Scholar]
- Bruce SE, Weisberg RB, Dolan RT, Machan JT, Kessler RC, Manchester G, Keller MB. Trauma and Posttraumatic Stress Disorder in Primary Care Patients. Prim Care Companion J Clin Psychiatry. 2001;3(5):211–217. doi: 10.4088/pcc.v03n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant-Davis T, Chung H, Tillman S, Belcourt A. From the margins to the center: ethnic minority women and the mental health effects of sexual assault. Trauma Violence Abuse. 2009;10(4):330–357. doi: 10.1177/1524838009339755. [DOI] [PubMed] [Google Scholar]
- Campbell Rebecca, Dworkin Emily, Cabral Giannina. An Ecological Model of the Impact of Sexual Assault On Women’s Mental Health. Trauma, Violence, & Abuse. 2009;10(3):225–246. doi: 10.1177/1524838009334456. [DOI] [PubMed] [Google Scholar]
- CDC. Mental Illness Surveillance among adults in the United States. Atlanta, GA: 2011. [PubMed] [Google Scholar]
- Chao RC, Green KE. Multiculturally Sensitive Mental Health Scale (MSMHS): development, factor analysis, reliability, and validity. Psychol Assess. 2011;23(4):876–887. doi: 10.1037/a0023710. [DOI] [PubMed] [Google Scholar]
- Congress, U.S; C. B. Office, editor. Estimates for the insurance coverage provisions of the Affordable Care Act updated for the recent Supreme Court decision. Washington D.C: 2012. [Google Scholar]
- Davidson JR, Book SW, Colket JT, Tupler LA, Roth S, David D, Feldman ME. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med. 1997;27(1):153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Ehring T, Kleim B, Clark DM, Foa EB, Ehlers A. Screening for posttraumatic stress disorder: what combination of symptoms predicts best? J Nerv Ment Dis. 2007;195(12):1004–1012. doi: 10.1097/NMD.0b013e31815c1999. [DOI] [PubMed] [Google Scholar]
- Foa E, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of PTSD: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9:445–451. [Google Scholar]
- U.S. PREVENTIVE SERVICES TASK FORCE. Screening for Depression: Recommendations and Rationale. Am Fam Physician. 2002;66(4):647–650. [PubMed] [Google Scholar]
- Glover DA, Loeb TB, Carmona JV, Sciolla A, Zhang M, Myers HF, Wyatt GE. Childhood sexual abuse severity and disclosure predict posttraumatic stress symptoms and biomarkers in ethnic minority women. J Trauma Dissociation. 2010;11(2):152–173. doi: 10.1080/15299730903502920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glover DA, Williams JK, Kisler KA. Using novel methods to examine stress among HIV-positive African American men who have sex with men and women. J Behav Med. 2013;36(3):283–294. doi: 10.1007/s10865-012-9421-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green B. Trauma History Questionnaire. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996. [Google Scholar]
- Gureje O, Jenkins R. Mental health in development: re-emphasising the link. Lancet. 2007;369(9560):447–449. doi: 10.1016/s0140-6736(07)60211-6. [DOI] [PubMed] [Google Scholar]
- Gurung RAR, Taylor SE, Kemeny M, Myers H. HIV Is Not My Biggest Problem”: The Impact of HIV And Chronic Burden On Depression In Women At Risk For AIDS. Journal of Social & Clinical Psychology. 2004;23(4):490–511. [Google Scholar]
- Hampton RL, Gelles RJ. Violence toward black women in a nationally representative sample of black families. Journal of Comparative Family Studies. 1994;25:105–119. [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100(5):933–939. doi: 10.2105/ajph.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins, Block, Campbell Risk of death and serious injury for abused African American women. Paper presented at the 2004 Homicide Research Working Group Annual symposium; Chicago. 2004. [Google Scholar]
- Juster RP, Marin MF, Sindi S, Nair NP, Ng YK, Pruessner JC, Lupien SJ. Allostatic load associations to acute, 3-year and 6-year prospective depressive symptoms in healthy older adults. Physiol Behav. 2011;104(2):360–364. doi: 10.1016/j.physbeh.2011.02.027. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Bruce ML, Koch JR, Laska EM, Leaf PJ, Wang PS. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36(6 Pt 1):987–1007. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Magee WJ. Childhood adversities and adult depression: basic patterns of association in a US national survey. Psychol Med. 1993;23(3):679–690. doi: 10.1017/s0033291700025460. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Koss MP, Abbey A, Campbell R, Cook S, Norris J, Testa M, Ullman S, West C, White J. Revising the SES: A collaborative process to improve assessment of sexual aggression and victimization. Psychology of Women Quarterly. 2007;31:357–370. [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic medicine. 2002;64(2):258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- Lave JR, Frank RG, Schulberg HC, Kamlet MS. Cost-effectiveness of treatments for major depression in primary care practice. Arch Gen Psychiatry. 1998;55(7):645–651. doi: 10.1001/archpsyc.55.7.645. [DOI] [PubMed] [Google Scholar]
- Lee DL, Ahn SU. Racial discrimination and Asian mental health: A meta-analysis. The Counseling Psychologist. 2011;39(3):463–489. [Google Scholar]
- Loeb TB, Williams JK, Carmona JV, Rivkin I, Wyatt GE, Chin D, Asuan-O’Brien A. Child sexual abuse: associations with the sexual functioning of adolescents and adults. Annu Rev Sex Res. 2002;13:307–345. [PubMed] [Google Scholar]
- Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10(6):434–445. doi: 10.1038/nrn2639. [DOI] [PubMed] [Google Scholar]
- Manderscheid R, Druss B, Freeman E. Data to manage the mortality crisis: Recommendations to the substance abuse and mental health services administration. Washington D.C: SAMHSA; 2007. [Google Scholar]
- McFarlane J, Greenberg L, Weltge A, Watson M. Identification of abuse in emergency departments: effectiveness of a two-question screening tool. J Emerg Nurs. 1995;21(5):391–394. doi: 10.1016/s0099-1767(05)80103-5. [DOI] [PubMed] [Google Scholar]
- Myers HF. Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. J Behav Med. 2009;32(1):9–19. doi: 10.1007/s10865-008-9181-4. [DOI] [PubMed] [Google Scholar]
- Noll Jennie G, Grych John H. Read-react-respond: An integrative model for understanding sexual revictimization. Psychology of Violence. 2011;1(3):202–215. doi: 10.1037/a0023962. [DOI] [Google Scholar]
- Organization, World Health. The world health report 2001. World Health Organization; 2001. Mental health: New understanding, new hope. [Google Scholar]
- Prevention, Centers for Disease Control and. Adverse childhood experiences reported by adults – five states. Atlanta, GA: 2010. [Google Scholar]
- Prevention, Centers for Disease Control and. Mental illness surveillance among adults in the United States. Atlanta, GA: 2011. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/su6003a1.htm. [Google Scholar]
- Radloff LS. The CES-D Scale A Self-Report Depression Scale for Research in the General Population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Rizopoulos D. ltm: An R Package for Latent Variable Modeling and Item Response Analysis. Journal of Statistical Software. 2006;17(5):1–25. [Google Scholar]
- Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, Muller M. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77. doi: 10.1186/1471-2105-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Services, U.S. Department of Health & Human. Federal Register, Document No. 2013-01422. Washington DC: 2013. Annual update of the HHS poverty guidelines. Retrieved from https://federalregister.gov/a/2013-01422. [Google Scholar]
- Sims M, Wyatt SB, Gutierrez ML, Taylor HA, Williams DR. Development and psychometric testing of a multidimensional instrument of perceived discrimination among African Americans in the Jackson Heart Study. Ethn Dis. 2009;19(1):56–64. [PMC free article] [PubMed] [Google Scholar]
- Smedley BD. The lived experience of race and its health consequences. Am J Public Health. 2012;102(5):933–935. doi: 10.2105/ajph.2011.300643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soeken K, McFarlane J, Parker B, Lominack MC. The Abuse Assessment Screen: A clinical instrument to measure frequency, severity, and perpetrator of abuse against women. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Stockdale SE, Lagomasino IT, Siddique J, McGuire T, Miranda J. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995–2005. Med Care. 2008;46(7):668–677. doi: 10.1097/MLR.0b013e3181789496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sue DW, Capodilupo CM, Torino GC, Bucceri JM, Holder AM, Nadal KL, Esquilin M. Racial microaggressions in everyday life: implications for clinical practice. Am Psychol. 2007;62(4):271–286. doi: 10.1037/0003-066x.62.4.271. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Stress and health: major findings and policy implications. J Health Soc Behav. 2010;51(Suppl):S41–53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Weinreb L, Fletcher K, Candib L, Bacigalupe G. Physicians’ perceptions of adult patients’ history of child abuse in family medicine settings. J Am Board Fam Med. 2007;20(4):417–419. doi: 10.3122/jabfm.2007.04.060208. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Lawrence J, Voudounon A, Mickey MR. Wyatt Sex History Questionnaire: A structured inerview for female sexual history taking. Journal of Child Sexual Abuse. 1992;1(4):51–68. [Google Scholar]
- Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. 1993;39(4):561–577. [PubMed] [Google Scholar]