Abstract
OBJECTIVES
While much is known about EMS care in urban, suburban and rural settings, only limited national data describe EMS care in isolated and sparsely populated frontier regions. We sought to describe the national characteristics and outcomes of EMS care provided in frontier and remote (FAR) areas in the continental United States (US).
METHODS
We performed a cross-sectional analysis of the 2012 National Emergency Medical Services Information System (NEMSIS) data set, encompassing EMS response data from 40 States. We linked the NEMSIS dataset with Economic Research Service-identified FAR areas, defined as a ZIP Code >60 minutes driving time to an urban center with >50,000 persons. We excluded EMS responses resulting in intercepts, standbys, inter-facility transports, and medical transports. Using odds ratios, t-tests and the Wilcoxon rank-sum test, we compared patient demographics, response characteristics (location type, level of care), clinical impressions and on-scene death between EMS responses in FAR and non-FAR areas.
RESULTS
There were 15,005,588 EMS responses, including 983,286 (7.0%) in FAR and 14,025,302 (93.0%) in non-FAR areas. FAR and non-FAR EMS events exhibited similar median response 5 [IQR 3–10] vs. 5 [3–8] min), scene (14 [10–20] vs 14 [10–20] min) and transport times (11 [5–24] vs 12 [7–19] min). Air medical (1.51% vs 0.42%; OR 4.15 [95% CI: 4.03–4.27]) and Advanced Life Support care (62.4% vs 57.9%; OR 1.25 [1.24–1.26]) were more common in FAR responses. FAR responses were more likely to be of American Indian or Alaska Native race (3.99% vs 0.70%; OR 5.04, 95% CI: 4.97–5.11). Age, ethnicity, location type, and clinical impressions were similar between FAR and Non-FAR responses. On-scene death was more likely in FAR than non-FAR responses (12.2 vs. 9.6 deaths/1,000 responses; OR 1.28, 95% CI: 1.25–1.30).
CONCLUSIONS
Approximately 1 in 15 EMS responses in the continental US occur in FAR areas. FAR EMS responses are more likely to involve air medical or ALS care as well as on-scene death. These data highlight the unique characteristics of FAR EMS responses in the continental US.
Keywords: Emergency Medical Services, allied health personnel, health services, rural
INTRODUCTION
Since its inception in the 1960s, Emergency Medical Service (EMS) care has expanded its geographic reach to encompass the entire United States (US).1 EMS agencies now provide care to patients in a range of population settings, stretching from dense urban locations to isolated regions. EMS care in the latter setting is particularly challenging because of the extended distances, sparse populations, increased costs, and dearth of healthcare resources.2,3 Numerous studies characterize isolated communities as “rural” regions. However, the conventional definition of rural – all population, housing, and geography territory not included within an urban area – has important inconsistencies and may fail to fully capture the remote and isolated nature of the region. For example, while rural usually connotes isolated regions with low population density, the traditional definitions of rural allow for the presence of nearby urban centers. Furthermore, rural regions on the outskirts of a major city may have more in common with the metropolitan area than with other isolated regions.4
More contemporary terms used to characterize isolated regions include “frontier” and “remote.” The Office of Rural Health Policy (ORHP) denotes frontier as “territory characterized by some combination of relatively low population density and high geographic remoteness.”3 An estimated 18 million Americans lived in frontier and remote (FAR) areas in the year 2000.3 While there have been prior descriptions of rural EMS care, no studies have examined EMS care delivered on a national scale in more isolated FAR areas. An understanding of the epidemiology of EMS responses in these regions could be useful for tailoring care for these communities and patients.
Rural areas demonstrate increased rates of mortality, morbidity, and risk factors compared to urban and suburban areas. The age-adjusted death rate is higher in rural areas for all ages. Unintentional injuries, suicides, and chronic obstructive pulmonary disease (COPD) all have higher death rates in rural areas.5 Rural residents demonstrate more risk factors for various diseases including increased rates of tobacco use, obesity, and physical inactivity6. We believe that because of even further isolation, these disparities may be even greater between FAR areas and non-FAR area. There are no national studies examining FAR EMS care. We sought to describe the national characteristics of EMS care response in FAR areas in the continental United States.
METHODS
Study Design
We analyzed data from the 2012 National Emergency Medical Services Information System (NEMSIS) public-release research dataset. The Institutional Review Board of the University of Alabama at Birmingham approved the study. We sought to determine the differences in patient and EMS response characteristics between FAR and non-FAR regions.
Study Setting and Data Source
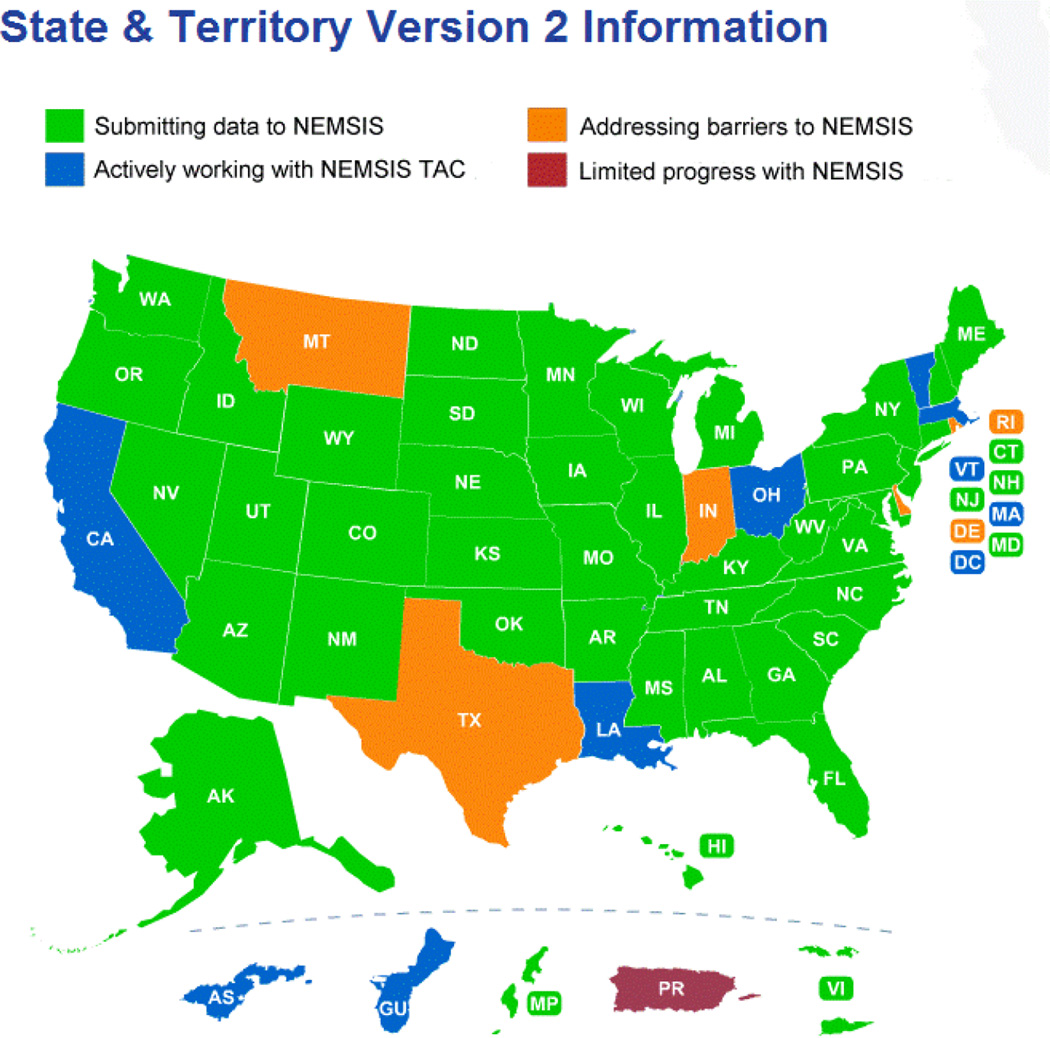
The NEMSIS project has been described previously.7 Maintained by the NEMSIS Technical Assistance Center (University of Utah School of Medicine, Salt Lake City, UT) and supported by the Office of Emergency Medical Services of the National Highway Traffic Safety Administration, NEMSIS seeks to provide a national, standardized EMS database with information collected by EMS personnel. Lead EMS offices in each state aggregate data from local EMS agencies, and submit statewide data to the national database. NEMSIS promotes the use of 75 elements required in the national dataset (available at www.nemsis.org). For this analysis, we used data from the 2012 NEMSIS Public-Release Research Data Set version 2.2.1. The 2012 research dataset contains 19,831,189 EMS activations submitted by 42 states and territories. (Figure 1)
FIGURE 1.
US States and Territories Contributing Data to the 2012 NEMSIS Dataset
Selection of Responses
NEMSIS includes all EMS requests for service (i.e., activations), regardless of outcome or actual service provided. As such, NEMSIS collects data for each 9-1-1 initiated EMS activation rather than for each patient receiving care. We excluded intercepts, mutual aid, and standby responses. We also excluded medical transports and interfacility transports. Remaining responses were classified as 9-1-1 responses. We also excluded medical transports and interfacility transports, excepting those with a Centers for Medicare and Medicaid Services (CMS) level of service code of “Specialty Care Transport to remove non-emergency (convenience) transports.” For the scene mortality analysis, we excluded events that had dispositions of “call cancelled” or “no patient found.”
Identification of Frontier and Remote Areas
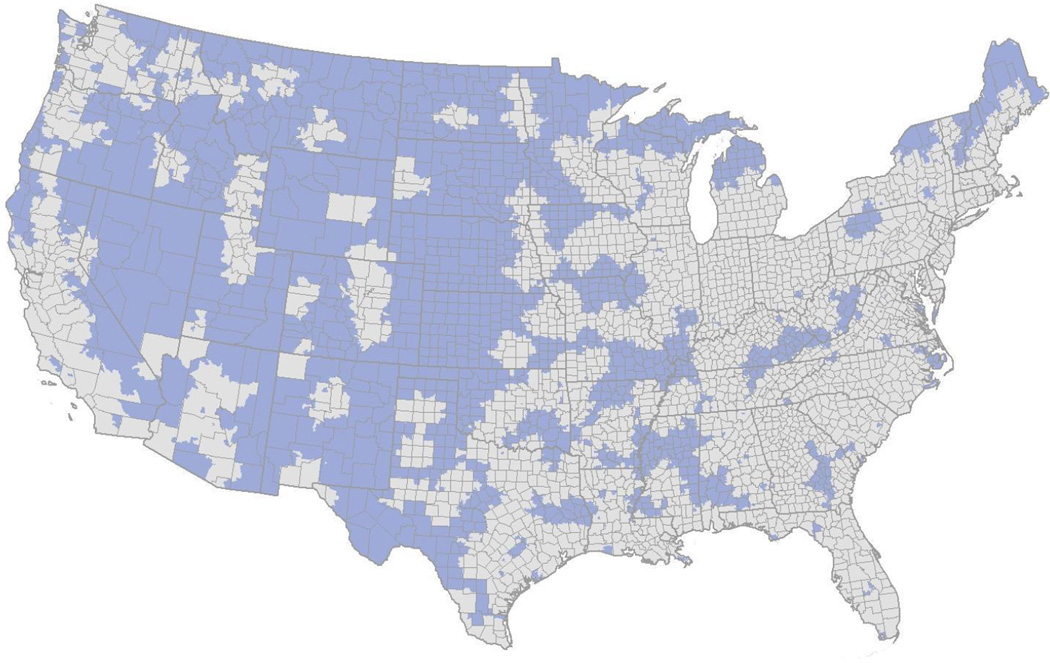
The Department of Health and Human Services’ Office of Rural Health Policy (OHRP), in collaboration with the United State Department of Agriculture’s Economic Research Service (ERS), defines a Frontier and Remote (FAR) area as a Zone Improvement Plan Code Tabulation Area (ZIP code) in which the majority of the population must drive ≥60 minutes to reach an urban area. Urban areas are defined by the Bureau of the Census as regions of census tracts with a combined total >50,000 people. Various criteria are used to formulate the urban areas, including population density and distance between census tracts.8 For each of 11.9 million 1x1 km2 area cells in the continental US, the OHRP and ERS identifies FAR zones based upon drive time routing algorithms, using Federal, State, and county paved roads, but not municipal streets. To facilitate linkage with other data sources, the OHRP/ERS further aggregates FAR cells based upon 2010 US ZIP Codes (Figure 2).3 FAR ZIP codes consisted of zones where the majority of the population lives in FAR-designated cells. Most ZIP codes were entirely FAR or entirely Non-FAR.
FIGURE 2.
United States ZIP Codes Designated as Frontier and Remote (FAR) Areas. Dark Blue – FAR areas Gray – non-FAR areas
Source: Economic Research Service, U.S. Department of Agriculture, using data from the U.S. Census Bureau, the Center for International Earth Science Information Network, and Environmental Systems Research Institute.
The NEMSIS Technical Assistance Center linked the 2012 NEMSIS research dataset with FAR codes, assigning FAR designation according to the ZIP code where the EMS response took place. We excluded EMS responses without ZIP code information.
Outcomes and Covariates
We compared characteristics between EMS responses in FAR areas and Non-FAR areas, including patient demographics, EMS response characteristics, the primary clinical impression indicated by EMS personnel, the procedures utilized, and the on-scene mortality of patients. Patient demographics included age, sex, race, ethnicity, primary payer, and alcohol and drug use indicators. Characteristics of the EMS response included the location type where the 9-1-1 event occurred (home residence, road, etc.), the level of care provided (Advanced Life Support (ALS), Basic Life Support (BLS), air medical, specialty care transport), response, scene, and transport times, any delays that occurred, and the US Census Region where the event occurred. ALS care was indicated by the NEMSIS element “Centers for Medicare and Medicaid Services (CMS) Service Level.” NEMSIS recorded the encounter as ALS if the unit reported providing CMS ALS-level care.
We divided the 24 hour clock into three eight hour periods (7AM – 2:59PM, 3PM-10:59PM, 11PM-6:59AM), and examined the number of dispatches occurring during those time periods. We also compared EMS personnel recorded clinical impressions. We categorized procedures by function and the level of care associated with the procedure. We categorized injuries according to the Centers for Disease Control and Prevention’s matrix of ICD-9 E-Codes.9 Patients who were classified as “dead at scene” were either dead on EMS arrival or dead after arrival with unsuccessful field resuscitation and no transportation.
Data Analysis
We analyzed patient demographics, EMS characteristics, clinical impression, procedures, and injuries using descriptive statistics and bivariate logistic regression (t-tests, Wilcoxon rank-sum tests, and odds ratios), stratifying by FAR and Non-FAR areas. We also compared unadjusted on-scene mortality, using events with dispositions of “dead at scene.” A subgroup analysis was performed for mortality based on responses with primary clinical impressions of stroke, cardiac arrest, and trauma. We analyzed all data using Stata 13.1 (Stata, Inc., College Station,TX).
RESULTS
There were a total of 15,008,588 EMS responses during the study period meeting inclusion criteria, including 983,286 FAR (7.0%) and 14,025,302 non-FAR (93.0%). FAR patients were slightly older than Non-FAR patients (56.3 vs 54.1 years) (Table 1). FAR areas contained more responses to American Indian or Alaskan Native patients (3.99% vs 0.70%; OR 5.04; 95% CI: 4.97–5.11), but contained fewer responses of other minority groups (black 13.3% vs 22.3%; Asian 0.17% vs 0.66%; Native Hawaiian or Other Pacific 0.08% vs 0.19%). FAR patients were more likely than non-FAR patients to have Medicare (44.1% vs 32.1%; OR 1.91; CI: 1.89–1.93) and other government health insurances (1.93% vs 0.88%; OR 3.06; CI: 2.97–3.15). The proportion of responses related to alcohol or drugs was similar between FAR and Non-FAR areas (Table 1).
TABLE 1.
Demographics of Patients for Frontier and Remote (FAR) and Non-FAR EMS responses.
| Not FAR | FAR | Odds Ratio | 95% CI | |||
|---|---|---|---|---|---|---|
| (n=14,025,302) | (n=983,286 ) | |||||
| Demographic | n | Col % | n | Col % | ||
| Age (y) (mean, SD)* | 54.1 | ±24.6 | 56.3 | ±24.4 | ||
| Sex | ||||||
| Male | 5,538,097 | 45.8 | 433,289 | 47.2 | Reference | |
| Female | 6,564,609 | 54.2 | 484,912 | 52.8 | 0.94 | (0.94–0.95) |
| Not available | 1,922,596 | -- | 65,085 | -- | -- | |
| Race | ||||||
| White | 6,922,371 | 69.9 | 600,963 | 79.0 | Reference | |
| Black/African American | 2,202,971 | 22.3 | 101,171 | 13.3 | 0.53 | (0.53–0.53) |
| Asian | 65,494 | 0.66 | 1,283 | 0.17 | 0.23 | (0.21–0.24) |
| American Indian or Alaska Native | 69,301 | 0.70 | 30,339 | 3.99 | 5.04 | (4.97–5.11) |
| Native Hawaiian or Other Pacific | 18,500 | 0.19 | 635 | 0.08 | 0.40 | (0.37–0.43) |
| Other | 620,898 | 6.27 | 26,008 | 3.42 | 0.48 | (0.48–0.49) |
| Not available | 4,125,767 | -- | 222,887 | -- | -- | |
| Ethnicity | ||||||
| Hispanic or Latino | 534,819 | 6.3 | 30,979 | 4.92 | 0.77 | (0.76–0.78) |
| Not Hispanic or Latino | 7,958,950 | 93.7 | 598,465 | 95.1 | Reference | |
| Not available | 5,531,533 | -- | 353,842 | -- | -- | |
| Primary Payer | ||||||
| Private Insurance | 956,520 | 25.3 | 57,894 | 18.2 | Reference | |
| Medicare | 1,213,994 | 32.1 | 140,635 | 44.1 | 1.91 | (1.89–1.93) |
| Medicaid | 542,641 | 14.3 | 46,928 | 14.7 | 1.43 | (1.41–1.45) |
| Other government | 33,316 | 0.88 | 6,167 | 1.93 | 3.06 | (2.97–3.15) |
| Workers compensation | 17,928 | 0.47 | 1,463 | 0.46 | 1.35 | (1.28–1.42) |
| Self-Pay | 674,614 | 17.8 | 43,404 | 13.6 | 1.06 | (1.05–1.08) |
| Not billed (for any reason) | 349,281 | 9.2 | 22,491 | 7.1 | 1.06 | (1.05–1.08) |
| Not available | 10,237,008 | -- | 664,304 | -- | -- | |
| Alcohol & Drug Indicators (n, rate/1000 calls) |
||||||
| Smell of alcohol on breath | 256,469 | 18.3 | 19,149 | 19.5 | 1.07 | (1.05–1.08) |
| Pt admits to alcohol use | 426,072 | 30.4 | 33,880 | 34.5 | 1.14 | (1.13–1.15) |
| Pt admits to drug use | 115,486 | 8.2 | 8,408 | 8.6 | 1.04 | (1.02–1.06) |
| Alcohol/drugs at scene | 80,169 | 5.7 | 6,683 | 6.8 | 1.19 | (1.16–1.22) |
| None | 3,030,084 | 216 | 324,673 | 330 | 1.79 | (1.78–1.80) |
| Not available | 10,365,516 | -- | 603,804 | -- | -- | |
EMS responses in FAR and non-FAR areas occurred at similar times of day and in similar locations (Table 2). ALS care (62.4% vs 57.9%; OR 1.25; CI: 1.24–1.26) and use of air medical transport (1.51% vs 0.42%; OR 4.15; CI: 4.03–4.27) were more common in FAR than non-FAR areas. The use of specialty care transport was similar between FAR and Non-FAR areas (Table 2). FAR and Non-FAR areas exhibited similar median elapsed response (5 [IQR 3–10] vs. 5 [3–8] min, p<0.001), on-scene (14 [10–20] vs 14 [10–20] min, p<0.001) and transport times (11 [5–24] vs 12 [7–19] min, p<0.001). Ninety percent fractile times in FAR areas were longer for response (17 min vs 13 min) and transport (42 min vs 28 min), but similar for scene times (28 min vs 27 min). FAR responses were most common in the Midwest census region (38.5%), followed by the South (37.0%), the West (17.9%), and the Northeast (6.51%). Delays, including response (69 vs 37.7 delays/1000 events), on-scene (68.9 vs 42.8 delays/1000 events), and transport (57.4 vs 20.8 delays/1000 events), were more common in non-FAR areas.
TABLE 2.
Characteristics of Frontier and Remote (FAR) and Non-FAR EMS responses.
| Not FAR | FAR | Odds Ratio | 95% CI | |||
|---|---|---|---|---|---|---|
| (n=14,025,302) | (n=983,286) | |||||
| Characteristic | n | Col % | n | Col | ||
| Event Dispatch Time | ||||||
| 7:00 AM - 2:59 PM | 4,744,373 | 33.8 | 362,536 | 36.87 | 1.12 | (1.12–1.13) |
| 3:00 PM - 10:59 PM | 5,830,736 | 41.6 | 396,405 | 40.31 | Reference | |
| 11:00 PM - 6:59 PM | 3,450,193 | 24.6 | 224,345 | 22.82 | 0.96 | (0.95–0.96) |
| Not Available | -- | -- | -- | |||
| Location Type | ||||||
| Home/residence | 6,970,821 | 55.6 | 524,244 | 56.0 | Reference | |
| Farm, mine/quarry, or industrial place | 82,214 | 0.66 | 9,282 | 0.99 | 1.5 | (1.47–1.53) |
| Recreation, port, lake, river, ocean | 127,391 | 1.02 | 14,646 | 1.56 | 1.53 | (1.50–1.56) |
| Street or highway | 1,738,023 | 13.9 | 119,365 | 12.7 | 0.91 | (0.91–0.92) |
| Public building (schools, gov. offices) | 518,186 | 4.13 | 28,213 | 3.01 | 0.72 | (0.72–0.73) |
| Trade or service (business, bars, restaurants, etc) | 619,867 | 4.94 | 37,345 | 3.99 | 0.8 | (0.79–0.81) |
| Health care facility (clinic, hospital) | 1,406,034 | 11.2 | 142,820 | 15.3 | 1.35 | (1.34–1.36) |
| Residential institution (nursing home, jail/prison) | 594,782 | 4.74 | 39,553 | 4.22 | 0.88 | (0.88–0.89) |
| Other location | 488,387 | 3.89 | 21,102 | 2.25 | 0.57 | (0.57–0.58) |
| Not available | 1,479,597 | -- | 46,716 | -- | -- | |
| Level of Care | ||||||
| BLS | 3,209,115 | 41.6 | 135,226 | 35.9 | Reference | |
| ALS | 4472,014 | 57.9 | 234,893 | 62.4 | 1.25 | (1.24–1.26) |
| Air Medical | 32,411 | 0.42 | 5,671 | 1.51 | 4.15 | (4.03–4.27) |
| Specialty Care Transport | 10,365 | 0.13 | 461 | 0.12 | 1.06 | (0.96–1.16) |
| Not available | 6,301,397 | -- | 607,035 | -- | -- | |
| US Census Region | ||||||
| Midwest | 2,382,562 | 17.0 | 378,853 | 38.5 | 9 | (8.93–9.08) |
| Northeast | 3,624,261 | 25.8 | 64,000 | 6.51 | Reference | |
| South | 6,995,873 | 49.9 | 364,150 | 37.0 | 2.95 | (2.92–2.97) |
| West | 1,022,606 | 7.29 | 176,283 | 17.9 | 9.76 | (9.67–9.85) |
| Time Intervals (min) (median, IQR) | ||||||
| Response time (Unit en route to arrival on scene | 5 | 3–8 | 5 | 3–10 | ||
| Scene time (on scene to depart scene) | 14 | 10–20 | 14 | 10–20 | ||
| Transport time (depart scene to hospital arrival) | 12 | 7–19 | 11 | 5–24 | ||
| 90% Fractile Time (min) | ||||||
| Response time (Unit en route to arrival on scene | 13 | 17 | ||||
| Scene time (on scene to depart scene) | 27 | 28 | ||||
| Transport time (depart scene to hospital arrival) | 28 | 42 | ||||
| Delays (n, rates/1000 calls) | ||||||
| Response delay | 598,222 | 69 | 22,133 | 37.7 | 0.53 | (0.52–0.54) |
| Scene delay | 600,064 | 68.9 | 24,120 | 42.8 | 0.61 | (0.60–0.61) |
| Transport delay | 444,367 | 57.4 | 11,287 | 20.8 | 0.35 | (0.34–0.36) |
| Barriers | 462,676 | 56.3 | 33,040 | 55.8 | 0.99 | (0.98–1.00) |
The clinical impressions of patients were similar between EMS responses in FAR and non-FAR areas (Table 3). Injuries to patients were more commonly reported among responses in FAR areas (26.5% vs 22.3%; OR 1.25; CI 1.24–1.26), although specific causes of injury were similar between FAR and Non-FAR patients. Among FAR responses, patients were more likely to undergo a procedure (596 events per 1000 responses vs 428 events per 1000 responses; OR 1.97; CI: 1.97–1.98) (Table 4).
TABLE 3.
Provider clinical impression and injuries for Frontier and Remote (FAR) and Non-FAR EMS responses.
| Not FAR | FAR | Odds Ratio | 95.00% CI |
|||
|---|---|---|---|---|---|---|
| Clinical Impression or Injury | (n=14,025,302) | (n=983,286) | ||||
| n | Col % | n | Col % | |||
| Traumatic Injury | 1,607,517 | 23.4 | 118,551 | 21.8 | 1.06 | (1.05–1.07) |
| Altered level of consciousness, syncope, seizure, and diabetic emergencies (hypoglycemia) |
1,491,269 | 21.7 | 127,163 | 23.4 | 1.25 | (1.24–1.26) |
| Chest pain and cardiac conditions | 867,540 | 12.6 | 73,567 | 13.6 | 1.23 | (1.22–1.24) |
| Airway obstruction, respiratory distress | 795,483 | 11.6 | 66,613 | 12.3 | 1.21 | (1.20–1.22) |
| Abdominal pain/problems | 748,667 | 10.9 | 57,287 | 10.6 | 1.10 | (1.09–1.11) |
| Behavioral/psychiatric disorder | 485,942 | 7.1 | 25,223 | 4.7 | 0.73 | (0.72–0.74) |
| Poisonings and environmental emergencies |
426,157 | 6.2 | 30,158 | 5.6 | 1.01 | (1.00–1.02) |
| Stroke/cerebrovascular accident | 151,364 | 2.2 | 14,658 | 2.7 | 1.39 | (1.36–1.41) |
| Cardiac arrest | 111,409 | 1.6 | 9,715 | 1.8 | 1.25 | (1.22–1.27) |
| OB/GYN emergency | 78,762 | 1.1 | 5,342 | 1.0 | 0.97 | (0.94–1.00) |
| Obvious death | 55,691 | 0.8 | 6,340 | 1.2 | 1.63 | (1.59–1.67) |
| Hypovolemia/shock | 58,681 | 0.9 | 7,629 | 1.4 | 1.86 | (1.82–1.91) |
| Sexual Assault/Rape | 4,084 | 0.1 | 726 | 0.1 | 2.54 | (2.34–2.75) |
| Unknown | 7,142,736 | -- | 440,314 | -- | ||
| Injury | ||||||
| No | 8,201,915 | 77.7 | 538,954 | 73.5% | ||
| Yes | 2,355,325 | 22.3 | 194,096 | 26.5% | 1.25 | (1.24–1.26) |
| Not available | 3,468,062 | -- | 250,236 | -- | ||
| Cause of Injury | ||||||
| Motor Vehicle accident (including motorized, motorcycle, non- motorized, bicycle, aircraft, and pedestrian traffic) |
631,733 | 34.6 | 56,565 | 35.0 | 1.04 | (1.02–1.06) |
| Environmental and exposure(temperature, lightning, fire/flames, poisoning, radiation, smoke, electrocution) |
71,345 | 3.9 | 3,647 | 2.25 | 0.59 | (0.57–0.62) |
| Falls | 825,371 | 45.1 | 75,622 | 46.7 | 1.06 | (1.05–1.08) |
| Firearm and stabbing (assault, accident, self-inflicted) |
70,427 | 3.9 | 6,219 | 3.8 | 1.03 | (1.00–1.06) |
| Water transport accident and drowning |
4,922 | 0.3 | 443 | 0.3 | 1.05 | (0.95–1.15) |
| Other | 224,551 | 12.3 | 19,325 | 11.9 | Ref | |
TABLE 4.
Procedures performed in Frontier and Remote (FAR) and Non-FAR EMS responses.
| Not FAR | FAR | Odds Ratio | 95% CI | |||
|---|---|---|---|---|---|---|
| Procedure | (n=14,025,302) | (n=983,286) | ||||
| n | n/1000 | n | n/1000 | |||
| Total | 5,983,185 | 42.8 | 585,956 | 59.6 | 1.97 | (1.97–1.98) |
| Therapeutic Interventions (wound care, splinting, etc) | 867,174 | 61.8 | 87,395 | 88.9 | 1.48 | (1.47–1.49) |
| Monitoring (pulse oximetry, ECG, blood glucose) | 4,483,384 | 319.7 | 470,367 | 478.4 | 1.95 | (1.94–1.96) |
| Critical (venous access, CPR, etc) | 3,260,822 | 232.5 | 335,722 | 341.4 | 1.71 | (1.70–1.72) |
| Airway (intubation, cricothyrotomy, oxygen, etc) | 634,185 | 45.2 | 49,574 | 50.4 | 1.12 | (1.11–1.13) |
| Movement (patient loaded, off-loaded, etc) | 251,344 | 17.9 | 43,007 | 43.7 | 2.51 | (2.48–2.53) |
| Medical Activation (specialty center activation) | 17,214 | 1.2 | 689 | 0.7 | 0.57 | (0.53–0.62) |
| Service Activation (Hazmat, fire, SWAT, etc) | 5,614 | 0.4 | 2,605 | 2.6 | 6.63 | (6.33–6.95) |
| Rescue | 27,859 | 2.0 | 3,108 | 3.2 | 1.59 | (1.54–1.65) |
| Restraint | 26,605 | 1.9 | 1,254 | 1.3 | 0.67 | (0.64–0.71) |
| No Procedure | 7,995,215 | 570.1 | 396,624 | 403.4 | 0.51 | (0.51–0.51) |
Unadjusted scene mortality was higher among FAR than non-FAR EMS responses (12.2 vs 9.6 deaths/1000 events; OR 1.44; CI: 1.25–1.30) (Table 5). On subgroup analysis, unadjusted scene mortality was higher for FAR EMS responses to patients with clinical impressions of stroke (OR 2.29; CI: 1.19–4.40) and trauma (OR 1.47; CI: 1.34–1.62), but not for cardiac arrest (OR 1.04; CI: 1.00–1.07).
TABLE 5.
On-scene death in Frontier and Remote (FAR) and Non-FAR EMS responses. Includes only events with death data available.
| Not FAR | FAR | Unadjusted Odds Ratio |
95% CI | |||
|---|---|---|---|---|---|---|
| EMS Response Type | Deaths (n) | n/1000 | Deaths (n) | n/1000 | ||
| All Responses (n = 13,229,021) | 117,656 | 9.6 | 11,373 | 12.2 | 1.28 | (1.25–1.30) |
| Stroke only (n = 188,260 events) | 49 | 0.3 | 11 | 0.7 | 2.29 | (1.19–4.40) |
| Cardiac arrest only (n = 169,804 events) | 54,822 | 351 | 4,920 | 359 | 1.04 | (1.00–1.07) |
| Trauma only (n = 1,797,365 events) | 4,476 | 2.7 | 490 | 3.9 | 1.47 | (1.34–1.62) |
DISCUSSION
Our study provides national data describing the unique characteristics and importance of EMS events in FAR areas. In the continental US, one of every fifteen EMS emergency responses occurred in a FAR region, collectively comprising almost one million activations in 2012. FAR responses had a greater proportion of Native Americans and Alaska Natives..10 Use of air medical transport and ALS care were more common in FAR than non-FAR areas. EMS responses reporting on-scene death were more common in FAR than non-FAR regions.
EMS responders in FAR areas reported a wide spectrum of patient clinical impressions similar to those for non-FAR EMS responses. Of note, on-scene mortality for poisonings and environmental emergencies were similar between FAR and non-FAR. This contrasts previous studies demonstrating increased morbidity and mortality from drug-related poisoning11, carbon monoxide poisoning12, hypothermia13,14, and acute heat illness15 in rural areas. Additionally, on-scene mortality for firearms and water accident/drowning rates were similar between FAR and non-FAR. These findings are also counter to previous studies demonstrating increased mortality from firearms16,17 and drowning17 in rural areas.
In contrast, response and transport times were similar between FAR and non-FAR responses. While the transport times did not differ, we cannot comment on the actual distance driven to the scene or the distance driven to the hospital. FAR region is determined by drive time to a nearby population center of 50,000 or more people. This does not rule out the possibility that EMS may transport patients to small rural or suburban facilities thereby resulting in shorter than anticipated travel times. Also, FAR calculations do not take into account traffic patterns or posted speed limits which may differ between FAR and non-FAR areas.
The majority of isolated areas are thought to be served by EMS agencies which are heavily dependent on volunteers, with services limited to BLS care.18 However, our data show that compared with non-FAR areas, FAR EMS agencies more frequently perform ALS care. Furthermore, EMS responses in FAR areas more likely result in advanced medical procedures such as intubation and intravenous access. FAR EMS personnel may be more likely to institute more definitive interventions in anticipation of extended transport distances. The converse may also be true; non-FAR responders may perform fewer interventions in anticipation of short transport times. These findings may form the basis for re-examination of EMS clinical policies and additional examination of EMS procedures.
The higher frequency of ALS care in FAR areas may also reflect higher patient acuity, illness severity, and comorbid burden. Compared with urban residents, rural populations are known to exhibit poor health behaviors, having higher rates of smoking, sedentary lifestyles, and impairments due to chronic conditions.19 One potential strategy is to expand the ability of basic level providers to deliver advanced level interventions. For example, the use of automated-external-defibrillation by BLS firefighters has been shown to increase cardiac arrest survival.20 Pilot studies have demonstrated the ability of EMT-Basic providers to perform supraglottic airway insertion and intraosseous access at acceptable success rates.21
We observed that EMS responses in FAR areas were more likely to result in an on-scene death compared to responses in non-FAR areas, despite the similar EMS response times. Furthermore, EMS activations to patients with stroke and trauma were more likely to result in death on-scene, while responses to cardiac arrest patients demonstrated equal rates. While our study does not indicate the causative factors, there are several plausible explanations for these observations. As mentioned above, patients seeking EMS care in FAR areas may present with increased illness severity. Laypersons caring for stroke patients in isolated areas may be less effective at recognizing related symptoms, leading to increased time to provision of appropriate care. Motor vehicle collision (MVC) injury could have contributed to on-scene death. MVC injury rates were similar between FAR and Non-FAR (Table 3), but rural areas demonstrate increased rates of hospitalizations and death from MVCs.22,23 Rural roads are estimated to account for 59% of all motor vehicle deaths.24 Pre-hospital MVC death is greater in non-urban and suburban areas, even after accounting for variables such as seat belt use, vehicle ejection, impact location, and more.22
Another potential explanation is disparities in the capabilities of FAR EMS personnel. Cardiac arrest, stroke and trauma represent unique, time-sensitive conditions where targeted interventions may impact outcomes. While on-scene death differed between FAR and non-FAR for both stroke and trauma, it did not differ for cardiac arrest. We suspect that for these patients, the initial prognosis may be too poor for any meaningful care to affect the outcome. Trauma and stroke represent unique opportunities for improvement in FAR EMS care to help improve the survival of patients in these settings. Volunteer EMS personnel may lack expertise with trauma care, triage and transfer decisions.25 One study found deficiencies in adherence to Advanced Trauma Life Support (ATLS) guidelines during transfer of trauma patients from outlying rural hospitals to a level 1 trauma center.26 Also, insufficient recognition of acute stroke by EMS personnel may lengthen time to CT scan and tPA administration.27,28 Targeted training for rural 911 dispatchers and EMS personnel may be helpful in reducing stroke death.29
Our data highlight the national impact that FAR areas exert on EMS resources and patient care. We have put forth the use of a novel method (i.e. FAR identification) that may more accurately capture isolation and geographic remoteness for EMS activations compared to conventional methods. For comparison, the NEMSIS Technical Assistance Center classifies EMS events using the county-based Urban Influence Code methodology (also developed by the Economic Research Service). Using this county-based categorization, in 2012 there were 1,867,087 rural and wilderness EMS events, and 12,941,942 urban and suburban events. Further work will be required to determine which system provides a more accurate depiction of EMS event isolation. Nevertheless, FAR areas have unique EMS needs, requiring advanced interventions at greater frequencies with limited resources. Improving EMS care may lie in advancing technology and increasing training for EMS personnel currently working in FAR areas. With close to a million EMS responses in 2012, EMS care in FAR areas cannot be ignored.
LIMITATIONS
NEMSIS is a registry of EMS activations or responses, and not a registry of patients receiving care. This is due to the fact that multiple emergency resources may respond to the same 9-1-1 call, care on the same patient may be submitted to the state and national EMS registries by multiple EMS agencies. Methods are currently not in place, at the state or national level, to link different reports to the same patient or emergency event. Also, we do not know the acuity/severity of the response. As such, we are unable to determine whether responses utilizing ALS do so out of availability or necessity.
Our intent was to describe the initial EMS care provided to patients in FAR and non-FAR areas. As such, we did not include EMS activations entered as ‘Medical Transport’, defined as transports that are not between hospitals or that do not require an immediate response (e.g. transportation via wheelchair van to a primary care providers office) or ‘Intercept’, ‘Interfacility Transfer’ or ‘Specialty Care Transfer’ defined as interfacility transportation by a ground ambulance vehicle at a level of service beyond the scope of the EMT-Paramedic.
We do not know the medical capabilities of the receiving hospital or hospitals surround the response. While our data represent the best national estimates of EMS responses to FAR and non-FAR regions, there are missing data. Although previous work has supported the accuracy of the NEMSIS dataset, it is unclear the nature of the missing data (e.g. missing at random).30
An additional limitation is that FAR codes have not been calculated by the ERS for Alaska and Hawaii. The FAR system also utilizes 2000 Census data to determine the location of populations within each ZIP code. Population characteristics may have changed over time, with potential differences in FAR/non-FAR designations for select regions. ZIP codes are also constantly in flux. It is common for postal delivery routes to be realigned, ZIP codes to be split, and ZIP codes to be discontinued, added or expanded, leading to some inaccuracy with the FAR code designations.31 Also, even though the NEMSIS Technical Assistance Center has worked to promote standardization throughout the data collection process, data quality depends upon the documentation practices of EMS personnel. Errors and data incompatibility could have occurred during local, state, and national-level aggregation. Finally, the 2012 NEMSIS dataset does not contain data from select states (e.g., California, Texas, or Montana).
CONCLUSIONS
Approximately 1 in 15 EMS responses in the continental US occur in FAR areas. FAR EMS responses are more likely to involve air medical or ALS care as well as on-scene death. These data highlight the unique characteristics of FAR EMS responses in the continental US.
Footnotes
CONFLICTS OF INTERESTS
The authors declare no conflicts of interest.
Contributor Information
Landon R. Mueller, Department of Emergency Medicine, University of Alabama School of Medicine.
John P. Donnelly, Department of Emergency Medicine, University of Alabama School of Medicine; Division of Preventive Medicine, University of Alabama School of Medicine; Department of Epidemiology, School of Public Health, University of Alabama at Birmingham.
Karen E. Jacobson, Department of Pediatrics, University of Utah School of Medicine.
Jestin N. Carlson, Department of Emergency Medicine, University of Pittsburgh; Department of Emergency Medicine, Stain Vincent Health System.
N. Clay Mann, Department of Pediatrics, University of Utah School of Medicine.
Henry E. Wang, Department of Emergency Medicine, University of Alabama School of Medicine.
REFERENCES
- 1.Wang HE, Mann NC, Jacobson KE, Ms MD, Mears G, Smyrski K, Yealy DM. National characteristics of emergency medical services responses in the United States. Prehospital emergency care. 2013;17(1):8–14. doi: 10.3109/10903127.2012.722178. [DOI] [PubMed] [Google Scholar]
- 2.Hart G. [Accessed 2/18/2014];Frontier/Remote Island, and Rural Literature Review. 2012 http://ruralhealth.und.edu/pdf/frontierreview.pdf.
- 3.Hirsch S. Methodology for Designation of Frontier and Remote Areas. Federal Register. 2012;77 [Google Scholar]
- 4.Hart LG, Larson EH, Lishner DM. Rural definitions for health policy and research. American journal of public health. 2005;95(7):1149–1155. doi: 10.2105/AJPH.2004.042432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meit MKA, Gilbert T, et al. [Accessed 6-15-15];The 2014 Update of the Rural-Urban Chartbook. 2014 https://ruralhealth.und.edu/projects/health-reform-policy-research-center/pdf/2014-rural-urban-chartbook-update.pdf.
- 6.Eberhardt MS, Pamuk ER. The Importance of Place of Residence: Examining Health in Rural and Nonrural Areas. American journal of public health. 2004;94(10):1682–1686. doi: 10.2105/ajph.94.10.1682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dawson DE. National Emergency Medical Services Information System (NEMSIS) Prehospital emergency care. 2006;10(3):314–316. doi: 10.1080/10903120600724200. [DOI] [PubMed] [Google Scholar]
- 8.Urban Area Criteria for Census 2000—Proposed Criteria. Federal Register. 2001;66:17018. [Google Scholar]
- 9.Recommended framework for presenting injury mortality data. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 1997;46(RR-14):1–30. [PubMed] [Google Scholar]
- 10.Norris TVP, Hoeffel E. [Accessed 6-15-15];The American Indian and Alaska Native Population: 2010. 2012 http://www.census.gov/prod/cen2010/briefs/c2010br-10.pdf.
- 11.Xiang Y, Zhao W, Xiang H, Smith GA. ED visits for drug-related poisoning in the United States, 2007. The American journal of emergency medicine. 2012;30(2):293–301. doi: 10.1016/j.ajem.2010.11.031. [DOI] [PubMed] [Google Scholar]
- 12.Iqbal S, Law HZ, Clower JH, Yip FY, Elixhauser A. Hospital burden of unintentional carbon monoxide poisoning in the United States, 2007. The American journal of emergency medicine. 2012;30(5):657–664. doi: 10.1016/j.ajem.2011.03.003. [DOI] [PubMed] [Google Scholar]
- 13.Ingram D. Age-adjusted rates for cold-related deaths, by US census region and metropolitan status of place of occurrence—United States, 2010–2013. MMWR Morb Mortal Wkly Rep. 2015 [Google Scholar]
- 14.Ingram D. Age-adjusted rates for cold-related deaths, by US census region and metropolitan status of place of cccurrence—United States, 2010–2013. MMWR Morb Mortal Wkly Rep. 2015 [Google Scholar]
- 15.Hess JJ, Saha S, Luber G. Summertime acute heat illness in U.S. emergency departments from 2006 through 2010: analysis of a nationally representative sample. Environmental health perspectives. 2014;122(11):1209–1215. doi: 10.1289/ehp.1306796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carr BG, Nance ML, Branas CC, Wolff CS, Kallan MJ, Myers SR, Wiebe DJ. Unintentional firearm death across the urban-rural landscape in the United States. The journal of trauma and acute care surgery. 2012;73(4):1006–1010. doi: 10.1097/TA.0b013e318265d10a. [DOI] [PubMed] [Google Scholar]
- 17.Burrows S, Auger N, Gamache P, Hamel D. Leading causes of unintentional injury and suicide mortality in Canadian adults across the urban-rural continuum. Public Health Rep. 2013;128(6):443–453. doi: 10.1177/003335491312800604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.(FORHP) FOoRHP. [Accessed 2/18/2014];A Service Chief’s Guide to Create Community Support of Excellence in EMS. 2004 https://www.ruralcenter.org/tasc/resources/rural-and-frontier-emergency-medical-services-agenda-future-service-chief%E2%80%99s–guide.
- 19.Health, United States, 2012. [Accessed 8/14/2014];2012 http://www.cdc.gov/nchs/data/hus/hus12.pdf.
- 20.Saner H, Morger C, Eser P, von Planta M. Dual dispatch early defibrillation in out-of-hospital cardiac arrest in a mixed urban-rural population. Resuscitation. 2013;84(9):1197–1202. doi: 10.1016/j.resuscitation.2013.02.023. [DOI] [PubMed] [Google Scholar]
- 21.Pratt JC, Hirshberg AJ. Endotracheal tube placement by EMT-Basics in a rural EMS system. Prehospital emergency care. 2005;9(2):172–175. doi: 10.1080/10903120590924564. [DOI] [PubMed] [Google Scholar]
- 22.Ryb GE, Dischinger PC, McGwin G, Jr, Griffin RL. Degree of urbanization and mortality from motor vehicular crashes. Ann Adv Automot Med. 2012;56:183–190. [PMC free article] [PubMed] [Google Scholar]
- 23.Coben JH, Tiesman HM, Bossarte RM, Furbee PM. Rural-urban differences in injury hospitalizations in the U.S., 2004. American journal of preventive medicine. 2009;36(1):49–55. doi: 10.1016/j.amepre.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Traffic Crashes Take Their Toll on America’s Rural Roads. [Accessed 3/23/2015];2006 http://www.nhtsa.gov/people/injury/airbags/RuralCrashes/
- 25.Peek-Asa C, Zwerling C, Stallones L. Acute traumatic injuries in rural populations. American journal of public health. 2004;94(10):1689–1693. doi: 10.2105/ajph.94.10.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCrum ML, McKee J, Lai M, Staples J, Switzer N, Widder SL. ATLS adherence in the transfer of rural trauma patients to a level I facility. Injury. 2013;44(9):1241–1245. doi: 10.1016/j.injury.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 27.Abdullah AR, Smith EE, Biddinger PD, Kalenderian D, Schwamm LH. Advance hospital notification by EMS in acute stroke is associated with shorter door-to-computed tomography time and increased likelihood of administration of tissue-plasminogen activator. Prehospital emergency care. 2008;12(4):426–431. doi: 10.1080/10903120802290828. [DOI] [PubMed] [Google Scholar]
- 28.Belvis R, Cocho D, Marti-Fabregas J, Pagonabarraga J, Aleu A, Garcia-Bargo MD, Pons J, Coma E, Garcia-Alfranca F, Jimenez-Fabrega X, Marti-Vilalta JL. Benefits of a prehospital stroke code system. Feasibility and efficacy in the first year of clinical practice in Barcelona, Spain. Cerebrovascular diseases. 2005;19(2):96–101. doi: 10.1159/000082786. [DOI] [PubMed] [Google Scholar]
- 29.Leira EC, Hess DC, Torner JC, Adams HP., Jr Rural-urban differences in acute stroke management practices: a modifiable disparity. Archives of neurology. 2008;65(7):887–891. doi: 10.1001/archneur.65.7.887. [DOI] [PubMed] [Google Scholar]
- 30.Mann NC, Kane L, Dai M, Jacobson K. Description of the 2012 NEMSIS public-release research dataset. Prehospital emergency care. 2015;19(2):232–240. doi: 10.3109/10903127.2014.959219. [DOI] [PubMed] [Google Scholar]
- 31.Grubesic TH, Matisziw TC. On the use of ZIP codes and ZIP code tabulation areas (ZCTAs) for the spatial analysis of epidemiological data. International journal of health geographics. 2006;5:58. doi: 10.1186/1476-072X-5-58. [DOI] [PMC free article] [PubMed] [Google Scholar]